Abstract
Endothelial progenitor cells (EPCs) play a critical role in the repair of damaged blood vessels and/or in the growth of new ones in ischemic tissues. Elevated levels of oxygen radicals, which accumulate in the ischemic tissue, could compromise the angiogenic potential of EPCs. To determine if oxidative stress alters the angiogenic response of EPCs and to identify possible cellular targets that protect EPCs from the damaging effects of oxidative stress, we have investigated vascular development in embryonic bodies (EBs) under hyperoxic conditions. Murine EBs at differentiaton day 2 were cultured for 3 days under normoxic (21% O2) or hyperoxic (60% O2) conditions. Hyperoxic EBs showed a moderate reduction in Pecam-1, Vegfr-2, eNOS and Tie2 mRNA levels compared to normoxic EBs. However, immunostaining of hyperoxic EBs with antibodies against PECAM-1 after 1 week recovery at room air revealed a defective vasculature completely deficient in branches, while normoxic EBs developed a normal vascular plexus. Oxygen-induced defective vascular development correlated with a dramatic decrease in soluble guanylyl cyclase, phosphodiesterase (Pde) 4B and Pde4C mRNAs. Oxidative stress did not affect the expression of adenylyl cyclase 6 and Pde5. The abnormal vascular development caused by hyperoxia was reverted by pharmacological treatments that increased cGMP levels, such as 8-bromo-cGMP or 4-{[3′,4′-(methylenedioxy)benzyl]amino}-6-methoxyquinazoline, a specific inhibitor of PDE5. These results indicated that oxidative stress inhibits vascular development from EPCs through its effects on levels of cyclic nucleotides and suggested that therapies that target cyclic nucleotide turnover may be useful in protecting vascular repair under oxidative conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A growing body of evidence suggests that endothelial progenitor cells (EPCs) may play a pivotal role in repairing damaged endothelium in ischemic tissue [1–5]. However, the use of EPCs may be limited by oxidative stresses in these tissues. Ischemic tissue is characterized by excessive production of reactive oxygen species and accumulation of oxidized metabolites that may compromise the angiogenic potential of the EPCs. The effects of oxidative stress on EPCs are controversial. While there is some evidence that oxidants decrease the capacity of both cord and adult peripheral blood-derived EPCs to form vessels in vitro and in vivo, other studies have reported that circulating endothelial progenitors are resistant to oxidative injury and able to repair damaged vessels in microenvironments enriched in oxygen radicals [6–9]. The discrepancy between these studies is likely due to dissimilarities between the cell types used and their stage of differentiation. Given the great therapeutic interest in EPCs for treatment and cure of ischemic diseases, it is important to investigate in more detail the effects of oxidative stress on blood vessel formation from these cells.
Blood vessel formation occurs through two processes: vasculogenesis, the differentiation of endothelial precursor cells into mature endothelial cells (ECs) in combination with the formation of a primordial vascular plexus, and angiogenesis, the formation of new blood vessels by branching and sprouting of pre-existing ones [10]. Both vasculogenesis and angiogenesis require activation of intracellular signaling pathways by soluble factors, as well as specific interactions with surrounding cells and extracellular matrix [10, 11]. Vascular endothelial growth factor-A (VEGF-A) is a critical regulator of both vasculogenesis and angiogenesis [12–14]. VEGF-A-activated angiogenic signals are, at least in part, mediated by nitric oxide (NO), a gaseous molecule that, depending on local concentrations and microenvironment, exerts diverse biological functions [15]. In ECs, NO is synthesized by endothelial nitric oxide synthase (eNOS) [16] and regulates EC growth, apoptosis, migration and angiogenesis [15, 17–21]. Many of the biological functions of NO are mediated through its activation of soluble guanylyl cyclase (sGC), that results in the synthesis of cyclic guanosine 3′,5′-monophosphate (cGMP) [22]. Increases in intracellular cGMP concentrations enhance EC migration, growth and formation of capillary-like structures in vitro and in vivo [23, 24]. In contrast, the pathway initiated by adenylyl cyclase (AC) leading to the production of cyclic adenosine 3′,5′-monophosphate (cAMP) inhibits many EC functions, including migration and network formation [25, 26]. Intracellular levels of cGMP and cAMP are dynamically regulated by the rate of their synthesis by cyclases and their hydrolysis by phosphodiesterases (PDEs) [27–29]. In vascular endothelium, PDE4 is the dominant cAMP-specific hydrolyzing enzyme, while PDE5 represents the major cGMP hydrolyzing activity [30]. Synthesis of cGMP in vascular endothelium is mediated by sGC and AC6 is the predominant endothelial cAMP generating enzyme [31, 32].
In this study we have investigated if hyperoxia alters the angiogenic properties of EPCs and determined the role of sGC in EC differentiation and formation of a primary vascular bed under oxidative conditions. For these experiments we have used murine embryonic stem cell-derived embryonic bodies (EBs), 3-dimensional cell aggregates in which events of early embryogenesis, such as hematopoiesis, neurogenesis, and cardiogenesis, take place in a context of paracrine signals, heterotypic cell–cell interactions and cell-extracellular matrix interactions [33]. Murine EBs recapitulate both vasculogenesis and angiogenesis, thus closely mimic the in vivo development and maturation of blood vessels [34, 35].
Our results indicate that hyperoxia (60% O2) interferes moderately with EC differentiation but dramatically affects the formation of a primary vascular bed in developing EBs. In fact, ECs that differentiated under hyperoxic conditions failed to organize into vessel-like structures and accumulated in clumps. Exposure to high oxygen dramatically decreased the mRNA levels of the two sGC subunits (α1 and β1), Pde4B and Pde4C, but did not affect the expression levels of AC6 and Pde5. The defective vascular development caused by oxygen exposure was reverted by pharmacological treatments that enhanced cGMP levels, such as soluble cGMP or inhibitors of PDE5, or decreased cAMP. Our results demonstrate that EPCs can differentiate and become mature ECs under hyperoxic stress but their angiogenic potential is dramatically compromised. Our findings suggest that sGC/cGMP signaling promotes angiogenesis under oxidative conditions, independently of the levels of VEGF-A. Moreover, our results show that functional cyclases and PDEs are present at very early stages of differentiation of EBs and that their regulated activity is indispensable for proper vascular development under both normoxic and hyperoxic conditions.
Methods
Cell culture
W4 mouse embryonic stem (ES) cells were obtained from the ES facility of the NYU Langone Medical Center. ES cells were plated onto mitomycin-treated mouse embryonic fibroblast feeder layers, and maintained in high glucose Dulbecco’ s Modified Eagle Medium (DMEM, GIBCO) supplemented with penicillin–streptomycin, non essential amino acids, sodium pyruvate, l-glutamine (all from GIBCO), 55 μM β-mercaptoethanol (Sigma), 15% heat-inactivated fetal bovine serum (Hyclone) and 1,000 U/ml leukemia inhibitory factor (LIF, obtained from the ES facility).
To form embryonic bodies (EBs), we followed the protocol illustrated in Fig. 1 [35]. Briefly, undifferentiated W4 cells were trypsinized (together with the feeder cells), centrifuged and plated for 20 min in the presence of LIF to remove the feeder cells. The supernatant was then collected and added to new plates for additional 20 min. Cells that did not attach (ES cells) at this step were recovered, centrifuged and resuspended in medium containing 20% heat-inactivated fetal bovine serum. Cells were counted and 30 μl drops containing 400 cells/drop were placed on the lid of tissue culture dishes, over sterile Phosphate Buffer Saline (PBS). The day that feeder cells and LIF were removed and the drops were made was designated differentiation day 0 (d0). After 2 days (d2), the hanging drops were collected and the EBs were either analyzed or transferred into bacterial dishes and grown in suspension for three additional days. At d5, EBs were either collected and analyzed or seeded in 24-well culture dishes and grown for 1 week as adherent colonies. Cells were fed every other day.
Protocol for the preparation of the EBs. ES cells were trypsinized and resuspended in differentiation medium. Time of LIF removal is identified as differentiation day 0 (d0). Drops of 30 μl containing 400 cells were dispersed on the lid of a tissue culture plate and incubated at 37°C for 2 days. During the incubation, the ES cells aggregated and formed the EBs. At d2, EBs were collected and either analyzed by immunofluorescence and RT–PCR, or allowed to further grow and differentiate in suspension for 3 days at 37°C. At this point (d5), EBs were analyzed for gene expression, or cultured as adherent colonies on 24-well tissue culture dishes and analyzed by RT–PCR or immunofluorescence staining at later times of differentiation
Exposure of EBs to hyperoxia
At d2, EBs were collected, transferred into bacterial dishes and cultured in suspension for 3 days. Dishes were placed in plexiglass chambers where either normoxic (21% O2) or hyperoxic (60% ± 5 O2) conditions were established. Oxygen levels inside the chambers were monitored with oxygen-specific sensors (Hudson RCI). If oxygen levels dropped below 55%, additional gas was flushed inside the chamber to reach the desired concentration. As the cultures inside the chambers could not exchange CO2 with the incubator, a hyperoxic medium was designed that maintained the pH of the cultures at 7.4 during the experiment. To prepare the hyperoxic medium, high glucose DMEM powder (GIBCO) was resuspended in 950 ml of sterile water and supplemented with 20 ml of 1 M hepes pH 7.2 and 0.75 ml of 5 N NaOH. Final volume was brought up to 1.01 with sterile water and filtered with a 0.2 μm filter (Nalgene). Penicillin, streptomycin, non essential amino acids, sodium pyruvate, l-glutamine, β-mercaptoethanol (Sigma) and 10% completed regular high glucose medium were added before use. Heat-inactivated fetal bovine serum was added to achieve 20% final concentration.
Treatment of EBs with VEGF-A, cGMP or inhibitors of cyclases and PDEs
EBs were treated with or without VEGF-A (40 ng/ml, R&D), 8-Bromo-cGMP (1 mM, Aldrich), 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one (ODQ, 10 μM, Sigma), SQ22536 (50 μM, Tocris) or 4-{[3′,4′-(methylenedioxy)benzyl]amino}-6-methoxyquinazoline (MMQ, 0.6 μM, Calbiochem). Agents were added just prior oxygen exposure and maintained in the culture medium for the entire duration of oxygen treatment. VEGF-A and soluble cGMP were added again after 48 h of oxygen treatment and cultures were reoxygenated. Cyclase and PDE inhibitors were added only one time, at the beginning of oxygen incubation. At least two plates, containing 50 EBs each, were used for each experimental condition. Three independent experiments were performed for each treatment.
Immunofluorescence
For immunofluorescence analysis, W4 cells and EBs at different differentiation days were rinsed in Ca++/Mn++ PBS (GIBCO) and fixed in 100% ethanol for 10 min at room temperature. Fixed cultures were blocked in staining buffer (2% goat serum [Sigma–Aldrich, St. Louis, MO] in Ca++/Mn++PBS) for 2 h at room temperature, or overnight at 4°C, and then incubated with rat anti mouse-PECAM antibody (1:300, Pharmingen, San Diego, CA) or rabbit polyclonal antibody against VEGFR-2 (1:200, sc-315, Santa Cruz Biotechnology) overnight at 4°C. Cultures were washed three times with staining buffer and incubated with rhodamine-conjugated anti-rat secondary antibodies (1:300, Jackson Laboratories) or DyLight-conjugated donkey anti rabbit secondary antibodies (1:200, Jackson ImmunoResearch Laboratories) for 1 h at room temperature. Cells were rinsed in PBS, mounted and viewed with a Zeiss fluorescent microscope. W4 cells and EBs stained at d2 and d5 were viewed with an EVOS fl Digital Inverted Fluorescence Microscope (AMG).
Reverse transcription-polymerase chain reaction
Total RNA was isolated and purified from EBs at d2 and d5 with TRIzol according to the manufacturer’s directions (Invitrogen) and treated with DNase (Ambion). Equal amount of starting material (1 μg total RNA for each sample) was reverse transcribed with Transcriptor (Roche) and amplified by PCR with Taq polymerase (Roche). The following primers were chosen with the assistance of the computer application Primer 3 [36]: Pecam-1: 5′CACCTCGAAAAGCAGGTCTC3′ (sense), 5′TCCTGATGGGTTCTGACTCC3′ (antisense); Vegfr-2: 5′GTCATGGATCCAGATGAATTGC3′ (sense), 5′CGAAGTCACAGATCTTAACCAC3′ (antisense); Vegf-A: 5′TGCGCTGTGCAGGCTGCTGT3′ (sense), 5′TCACCGCCTCGGCTTGTCAC3′ (antisense); Tie-2: 5′CTCTGTGGAGTCAGCTTGCTC3′ (sense), 5′GAACAATCAGCCTGGTGAAGG3′ (antisense); vWF: 5′ATGATGGAGAGGTTACACATC3′ (sense), 5′GGCAGTTGCAGACCCTCCTTG3′ (antisense); eNOS: 5′GACCCTCACCGCTACAACAT3′ (sense), 5′CTGGCCTTCTGCTCATTTTC3′ (antisense); AC6: 5′GCACACACTACCCTGCTGAA3′ (sense), 5′CGATCATGTCTACCCCCATC3′ (antisense); sGC alpha1 (α): 5′GCACACACTACCCTGCTGAA3′ (sense), 5′CGATCATGTCTACCCCCATC3′ (antisense); SGC beta1 (β): 5′TGCAGATGTTTGGGAAGATG3′ (sense), 5′GACCACTAGGTTCCGGTCAA3′ (antisense); Pde4A: 5′TTCAAGCTGCTGCAAGAAGA3′ (sense), 5′ACAGTGCACCATGTTCCTGA3′ (antisense); Pde4B: 5′GAACAAATGGGGCCTTAACA3′ (sense), 5′GAGGCTCATGTGTTTGGACA3′ (antisense); Pde4C: 5′CATGCTCAACCGTGAGTTGT3′ (sense), 5′TGGAACGTCTTGAGGAGGTC3′ (antisense); Pde4D: 5′AGATGAGTCGGTCTGGCAAC3′ (sense), 5′TCTGCAGCATGGATGTTGTT3′ (antisense); Pde5A: 5′CCGGTTCAATGCAGAAGTTG3′ (sense), 5′TTTATAGGGGTGCAAAGCAAA3′ (antisense). Vegf-A primers identify both Vegf-164 and Vegf-120 isoforms. As the four Pde4 genes generate different splice variants that fall into two major groups, the long and the short isoforms, the PDE4 primers were designed to amplify both short and long forms. PCR results for each gene were normalized to the levels of Gapdh [5′AACTTTGGCATTGTGGAAGG3′ (sense), 5′ACACATTGGGGGTAGGAACA3′ (antisense)], which was found to be a suitable housekeeping gene for differentiating murine ES cells [37].
Semi-quantitative real-time PCR
Semi-quantitative real-time PCR was performed using the iQ SYBR Green Supermix (Biorad) with the iCycler iQ real-time PCR detection system (Biorad), with 40 cycles of real-time data collection at 95°C for 10 s and 49°C for 30 s. Relative mRNA amounts were normalized to Gapdh expression using the ΔΔCt method [38].
Analysis of tube formation
Vascular density was estimated by counting the number of branches in digital images of 5 different fields from each of at least 12 EBs for each condition. Vessel morphology was analyzed in the same images. The images were acquired using a Zeiss fluorescent microscope equipped with AxioCam and AxioVision imaging system software.
Statistical analysis
The data was analyzed by Student’s t test. Results are presented as the mean ± SD of three experiments performed on independent cultures and were considered significant when P values were <0.05.
Results
Effects of hyperoxia on endothelial cell differentiation
Vascular development in W4-derived EBs was evaluated by RT–PCR analysis at two different times of differentiation, day 2 and day 5 (Fig. 1). Two days after LIF removal (d2), EBs from the hanging drops expressed relatively high levels of Vegf-A and Vegf-receptor-2 (Vegfr-2) mRNA, an early marker of vascular development [39] (Fig. 2a), while markers distinctive of more mature ECs, such as platelet endothelial cell adhesion molecule-1 (Pecam-1), Tie-2, von Willebrand Factor (vWF) and endothelial nitric oxide synthase (eNOS) were present at low levels. At d5, endothelial differentiation was more pronounced as shown by increased levels of vascular markers (Fig. 2a). Developmental regulation of endothelial markers in differentiating EBs was confirmed by real time PCR (Fig. 2b). The kinetics of EC appearance in the developing EBs were also monitored by immunofluorescence staining. Some undifferentiated ES cells (W4), grown in the presence of LIF on a feeder monolayer, showed VEGFR-2 immunostaining, but no staining using antibodies against PECAM-1 (Fig. 2c). At d2, PECAM-1 staining became detectable in areas of developing EBs that were also stained with VEGFR-2 antibodies (Fig. 2c) and by d5 the two proteins colocalized in larger areas of the EBs (Fig. 2c). Thus the appearance of mature ECs in the developing EBs correlated with the kinetics of endothelial gene expression.
Vascular gene expression in developing EBs. Total RNA was extracted from EB cultures at two different days of differentiation, d2 and d5. 1 μg of total RNA was reverse transcribed and amplified by PCR using primers specific for vascular markers. mRNA levels were normalized to the housekeeping gene Gapdh. a Levels of expression of angiogenic markers increased with differentiation time of the EBs. b Changes in expression were confirmed by RT-real time PCR analysis from three independent experiments (*significant increase in expression, P < 0.01). c To identify ECs, EBs were stained with VEGFR-2 and PECAM-1 antibodies at different times of differentiation. Undifferentiated ES cells (W4), grown in the presence of LIF and on a feeder monolayer, showed relatively small amounts of VEGFR-2 protein, localized to specific areas of the cell, but not PECAM-1 (arrows). At d2, PECAM-1 protein could be detected in small areas of the developing EBs and colocalized with VEGFR-2 protein. Black arrow indicates a cell cluster expressing both markers, while arrowheads point to areas that are only VEGFR-2 positive. At d5, the arrow shows costaining with both antibodies covering larger areas of the developing EBs. Scale bar: W4 and d2 = 50 μm; d5 = 200 μm
These results identified the time between d2 and d5 as the period during which major endothelial maturation events occur in differentiating EBs. Thus, to investigate the effects of hyperoxia on EC differentiation, we cultured EBs under hyperoxic conditions (60% O2) from d2 to d5. Control EBs were maintained in normoxia (21% O2) for the entire duration of the experiment. At the end of the exposures, the expression of vascular markers was analyzed by RT–PCR (Fig. 3a, b). Compared to normoxic EBs, hyperoxic EBs showed a moderate, but significant, decrease in Pecam-1, Tie-2, eNOS and vWF mRNAs, as well as mRNAs for Vegf-A and Vegfr-2. Differentiating ECs in hyperoxic EBs were identified by immunostaining. PECAM-1 and VEGFR-2 were found to colocalize in hyperoxic EBs, thus confirming that hyperoxia does not dramatically affect endothelial differentiation (Fig. 3c). Albeit the effects on vascular specification were modest, elevated oxygen concentrations drastically inhibited the total growth of the developing EBs (Fig. 3d).
Effects of hyperoxia on early vascular differentiation. EBs at d2 were incubated in normoxia (21% O2) or hyperoxia (60% O2) for 3 days. At the end of the incubation time, vascular development was analyzed at mRNA and protein levels by RT–PCR and immunofluorescent staining, respectively. a Oxygen exposure caused a decrease in expression of angiogenic markers in the developing EBs. b Changes in expression were confirmed by RT-real time PCR analysis (*significant change, P < 0.02). c Immunostaining with VEGFR-2 and PECAM-1 antibodies showed the presence of maturing ECs in hyperoxic EBs. Arrows indicate colocalization of the two markers. d Hyperoxia inhibited the overall growth of the EBs, as shown by phase contrast microscopy. Scale bar: panel c = 100 μm; panel d = 200 μm
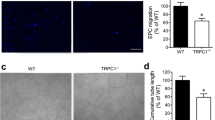
Hyperoxia affects vascular development
We then investigated if exposure of EBs to hyperoxia affected the organization of differentiating ECs into a primary vascular plexus. EBs at d2 were cultured in suspension for 3 days under either normoxic or hyperoxic conditions. At the end of the treatments (d5), normoxic and hyperoxic EBs were seeded in 24 well-dishes and allowed to grow and further differentiate in normal air for 1 week (Fig. 1). Cultures (d12) were then fixed and stained using antibodies to PECAM-1. EBs exposed to normoxia throughout the experiment displayed numerous elongated PECAM+ structures that resembled blood vessels (Fig. 4a). These cultures also contained single mature ECs that were not yet organized into vascular cords (Fig. 4b). In contrast, EBs that were initially treated with hyperoxia formed a defective vasculature, characterized by rounded and compact PECAM+ clusters, deficient in branches (Fig. 4c, d). Only sporadic, thick and short vessels were present in these cultures (Fig. 4e). Staining with antibodies to ICAM-2, a marker expressed by mature ECs, showed a similar vascular defect (online resource 1). Counting branch points confirmed the abnormal vascular development in the hyperoxia-treated cultures (Fig. 4g). Despite the defective vascular organization, the expression of vascular markers, such as Pecam-1 and eNOS, in oxygen-exposed cultures was similar to control cultures (Fig. 4h). Moreover, the deleterious effect of hyperoxia on vascular development was transient, as several normal vascular branches formed when the hyperoxic EBs were cultured in normal air for longer time (d19) (Fig. 4i).
Hyperoxia affects formation of the primary vascular plexus. EBs were cultured under normoxic or hyperoxic conditions between d2 and d5 and then grown for 1 week as adherent colonies in normal air. At the end of the incubation, EBs were stained with antibodies to PECAM-1 to identify ECs. a, b EBs that were cultured under normoxic conditions displayed a normal vascular development with numerous elongated structures (a) and several single ECs (b, arrows). c–e EBs that were treated with hyperoxia during the early phase of differentiation showed a defective vascular development characterized by endothelial clusters and absence of branches. f DAPI staining of the field shown in panel (e). g The number of vascular tubes in the two types of cultures was quantified by counting the elongated structures in digital imges (*significant difference, P < 0.05). h Analysis of vascular expression by RT-real time PCR showed full recovery of Pecam and eNOS expression after 1 week in normoxia (black bars: normoxic EBs; gray bars: hyperoxic EBs after 1 week in normoxia). i The vascular defect caused by oxygen exposure was transient as EBs that were allowed to recover in normal air for 2 weeks formed branches. j DAPI staining of the field shown in panel (i). Scale bar in panels a, c, i and j = 200 μm; scale bar in panels b, d, e and f = 50 μm
Exogenous VEGF-A partially rescues vascular tube formation
We investigated if oxygen-induced downregulation of VEGF-A was responsible for the abnormal vascular development observed in the hyperoxic EBs. EBs that were exposed to hyperoxia in the presence or absence of exogenous VEGF-A (40 ng/ml) showed similar decreased levels of expression of Pecam-1, and Vegfr-2 (online resource 2). However, addition of VEGF-A during oxidative insult rescued later tube formation as shown by increased number of elongated vascular structures in EBs that were co-treated with VEGF-A and oxygen, compared to cultures that were treated with hyperoxia alone (Fig. 5a, b, d). The ability of VEGF-A to rescue vascular development from the effects of hyperoxia was only partial, as several PECAM-1+ clumps still formed in these cultures (Fig. 5b), and the endothelial tubes appeared thin and fragile compared to those in the control dishes (Fig. 5c). Increased doses of VEGF-A (80 ng/ml) protected tube formation but also stimulated the formation of abnormally thick vascular structures (online resource 3). Moreover, addition of VEGF-A to the cultures after oxygen exposure, during the recovery phase in normal air, did not rescue vascular development (Fig. 5e).
Exogenous VEGF-A partially preserves the vascular phenotype in the hyperoxic EBs. EBs were exposed to 60% O2 in the absence or presence of 40 ng/ml of VEGF-A and then allowed to recover in normoxia for 1 week. a EBs that were treated with hyperoxia alone showed abnormal vascular development. b EBs that were treated with VEGF-A during the exposure to hyperoxia showed a partial rescue of vascular development. Arrows indicate the persistence of endothelial clusters in VEGF-hyperoxia-treated EBs. c Normal vascular development in normoxic EBs. Treatment with VEGF during oxidative stress did not completely recover the morphology of the branches to that of cultures maintained in normoxia for the entire duration of the experiment (compare b to c). d Formation of elongated vascular structures was quantified by counting of branches in images from each treatment (*significant difference, P < 0.05). e Addition of VEGF-A during recovery in normoxia did not rescue vascular development from the EBs that were treated with hyperoxia in absence of VEGF. Scale bar = 200 μm
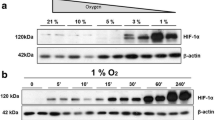
Hyperoxia alters the metabolism of cGMP and cAMP in developing EBs
The eNOS-sGC-cGMP pathway contributes substantially to blood vessel formation as it modulates crucial VEGF-A-mediated angiogenic events, like EC proliferation, migration and sprouting [15–24]. In contrast, the pathway initiated by AC with the formation of cAMP inhibits EC migration and network formation [25, 26]. We found that the expression of α1 and β1 sGC subunits, as well as AC6 and Pde4B were developmentally regulated in EBs, while expression of Pde4A, Pde4C, Pde4D and Pde5A, the major Pde5 isoform in ECs, did not change significantly (Fig. 6a, b). When treated with hyperoxia, EBs showed a dramatic decrease in the expression of both sGC subunits (Fig. 7a, b), but no change in the levels of AC6 mRNA. Moreover, the total Pde4 expression decreased significantly, as the expression levels of Pde4B and Pde4C, two cAMP-specific Pde4 isoforms highly represented in the vascular system, were reduced in the hyperoxic EBs by approximately 60 and 80%, respectively, compared to the normoxic controls (Fig. 7b). The levels of the other two Pde4 isoforms, Pde4A and Pde4D, as well as Pde5A, were not significantly affected by oxidative stress (Fig. 7a, b). Interestingly, the expression of sGC, Pde4B and Pde4C returned to normal levels when the hyperoxic EBs were allowed to recover for 1 week in normal air (online resource 4), suggesting that the defective vascular development observed in these cultures could not be attributed to persistent lack of these enzymes. In addition, the decreased expression of sGC in response to hyperoxia is expected to decrease cGMP levels, whereas the decreased expression of Pde4 is expected to increase cAMP levels, leading to an imbalance in cGMP/cAMP ratios.
Effects of hyperoxia on the expression of sGC, AC6 and Pdes. EBs were exposed to normoxia or hyperoxia between d2 and d5. At the end of the exposure, total RNA was extracted and analyzed by RT–PCR (a) or RT-real time PCR (b). Oxygen exposure significantly inhibited the expression of sGC subunits, Pde4B and PdeC (*significant change, P < 0.02), while it did not affect the level of expression of AC6 and Pde4A. The increase in Pde4D and the decrease in Pde5A were not significant (for Pde4D: P = 0.075, for Pde5A: P = 0.125) but reproducible
cGMP rescues vascular development in hyperoxic EBs
If the impaired vascular development caused by oxidative stress is caused by an imbalance between intracellular levels of cGMP and cAMP, we hypothesized that the defects in vascular development observed under hyperoxic conditions would be attenuated by elevation of intracellular levels of cGMP. A stable analog of cGMP, 8-Br-cGMP, was added into the culture medium of the developing EBs for the duration of the hyperoxic treatment. EBs exposed to hyperoxia with or without 8-Br-cGMP showed similar levels of expression of vascular markers, cyclases and Pdes, suggesting that cGMP treatment during oxidative stress cannot attenuate oxygen-induced downregulation of these genes (online resource 2). However, 8-Br-cGMP preserved the ability of ECs differentiated under hyperoxic conditions to properly assemble and form elongated vascular tubes (Fig. 8). In fact, treatment of developing EBs with 8-Br-cGMP during oxidative stress promoted vessel formation and significantly increased the number of branches and sprouting points once the cultures were allowed to recover for 1 week in normal air, without additional cGMP (Fig. 8a, b, d).
cGMP and inhibition of PDE5 rescue vascular development in EBs treated with hyperoxia. EBs were exposed for 3 days to hyperoxia in the presence or absence of 8-Br-cGMP (1 mM), a stable cell permeable analogue of cGMP, or MMQ (0.6 μM), a specific inhibitor of PDE5, and transferred to normal air for 1 week, without additional treatment. a PECAM-1 staining shows abnormal vascular development in hyperoxic EBs. b EBs that were treated with soluble cGMP during hyperoxic insult showed formation of elongated vascular structures. c DAPI staining of the field shown in panel (b). d Formation of vascular structures was quantified by counting branches in different fields from each of the different culture conditions (*significant difference, P < 0.02). e Treatment with MMQ during oxygen exposure also rescued vascular development in EBs. f When the PDE5 inhibitor was added after oxygen exposure, vascular development was still abnormal. Scale bar = 200 μm
To further examine the vascular protective role of cGMP under hyperoxic conditions, we exposed EBs at d2 to hyperoxia for 3 days in the absence or presence of MMQ, a potent and specific inhibitor of PDE5, the major cGMP specific degrading enzyme. We found that addition of MMQ did not maintain expression of EC marker mRNAs at the normal level (online resource 2), but effectively protected the differentiating ECs from oxygen damage, as they were able to assemble and form elongated vascular structures when allowed to recover in normal air (Fig. 8e). Treatment with the PDE5 inhibitor significantly increased capillary formation in oxygen-exposed EBs (Fig. 8d). Addition of MMQ increased the levels of cGMP in the vascular structures that developed from the hyperoxic EBs (online resource 5). Interestingly, if MMQ was added to the cultures after oxygen exposure, during the recovery in normoxia, it produced aberrant blood vessel formation, with thick and disorganized branches (Fig. 8f).
If balanced concentrations of cGMP and cAMP are requisite for normal vascular development, we hypothesized that reduction of cAMP levels would have effects similar to raising cGMP levels. EBs were incubated for 3 days in hyperoxia in the presence of SQ22636, a drug that inhibits AC6 activity and thus reduces the levels of intracellular cAMP, and then allowed to recover in normoxia for 1 week without inhibitor. We found that lowering the intracellular levels of cAMP with SQ22636 during oxidative stress protected vascular tube formation (Fig. 9a, b). On the other hand, treatment of normoxic EBs between d2 and d5 with ODQ, a potent and selective inhibitor sGC, which is expected to reduce intracellular cGMP levels, caused the formation of an abnormal vascular system that was almost completely devoid of branch points and resembled the defective vasculature observed in EBs treated with oxygen (Fig. 9d, f). Treatment with SQ22636 or ODQ significantly altered capillary formation compared to the untreated counterparts (Fig. 9c, f).
Balanced concentrations of cGMP and cAMP are necessary for normal vascular development. a Abnormal vascular development in hyperoxia-treated EBs. b Co-treatment of oxygen-exposed EBs with SQ22636, a drug that inhibits AC6 activity and thus reduces the levels of intracellular cAMP, rescues tube formation during the recovery in normoxia. d Normal vascular development in normoxic EBs. e Treatment of normoxic EBs with ODQ, a specific inhibitor of sGC, causes defective vascular formation. c, f Formation of vascular structures was quantified by counting branches in different fields from each of the different culture conditions (*significant difference, P < 0.02). Scale bar = 200 μm
Discussion
To study the response of EPCs to oxidative stress, we have employed EBs derived from pluripotent murine ES cells. The EB system recapitulates both vasculogenesis and angiogenesis [34, 35]. In the EB cultures, EPCs differentiate into mature ECs, which assemble into tubular vessel-like structures to form a primordial vascular plexus that gradually increases in density by splitting and sprouting of the formed vessels. Under our experimental conditions, vascular specification in maturing EBs begins as early as d2, as we were able to identify cells expressing vascular markers at both mRNA and protein levels in d2 EBs. In contrast, Vittet et al. [40] have reported that the expression of Vegfr-2 is induced at d3 while Pecam-1 mRNA can be detected at d4. This discrepancy might be due to differences in the ES cell lines or to the different culture conditions used. In the EB system used in this study, we identified the time between d2 and d5 as the period during which major endothelial maturation events occur.
We found that the exposure of EBs to 60% O2 during the time of endothelial commitment interferes with vascular development. Oxidative stress caused a moderate, but reproducible, decrease in the expression of the vascular genes Pecam-1, vWF, eNOS, Vegfr-2 and Tie-2. Since treatment with high oxygen markedly affected the overall EB growth, at this point it is not possible to distinguish if the decreased vascular gene expression is caused by an inhibition of EC proliferation, differentiation, or both. In addition to these early effects on endothelial precursors, we found that exposure to high oxygen levels affected the ability of the differentiating ECs to organize into elongated tubes and caused formation of abnormal vascular structures, which were almost completely devoid of branch points. These results are in agreement with previous studies which reported reduced vessel formation by oxidant-treated cord blood derived EPCs [6, 7, 41]. Importantly, our finding highlights the fact that the damage caused by oxidative stress to the EPCs during their initial stage of differentiation, dramatically compromised later aspects of vascular development. On the basis of these results and taking into account the potential use of EPCs for the treatment of ischemic disorders, it is critical to: (1) understand how oxidative stress affects EPC functional capacities, (2) identify angiogenic modulators that are able to protect the EPCs from the deleterious effects of oxygen radicals and (3) design strategies that enhance their activity during oxidative stress.
VEGF-A is a key modulator of vasculogenesis and angiogenesis, promoting EC migration, proliferation and survival in a dose dependent manner [13, 42], and is a good candidate to promote resistance of EPCs to oxidative stress. Hyperoxic treatment decreased the expression of VEGF-A, suggesting a cause-effect correlation between depletion of VEGF-A and abnormal vascular development of the hyperoxic EBs. However, administration of VEGF-A to EBs during hyperoxic exposure only partially rescued the formation of vessels in these cultures, suggesting that VEGF, although required is not sufficient to completely confer protection from oxygen and that additional factors along the VEGF-A pathway or VEGF-independent angiogenic signals are necessary to protect the angiogenic capacity of the EPCs from oxidative insult.
Increasing evidence indicates that the sGC/cGMP pathway mediates VEGF-NO stimulated EC proliferation, migration and organization into newly forming vessels, while cAMP exerts a negative effect on these properties [17–26]. The intracellular levels of cAMP and cGMP are regulated by the rate of their synthesis by cyclases and degradation by PDEs [27–29]. Therefore, alterations in the levels, or activities, of these enzymes might modify the balance between cGMP and cAMP and consequently affect the angiogenic properties of the ECs.
In this paper we report that hyperoxia-induced changes in EPC angiogenic potential correlated with a dramatic downregulation of sGC mRNA, but not AC6. Total expression of Pde4 (the major cAMP degrading enzymes) in the developing EBs was also affected by oxygen treatment, as Pde4B and Pde4C mRNAs were significantly decreased upon hyperoxic treatment. Although other reports have also shown a reduction in the expression of sGC by reactive oxygen species [43–45], the outcomes of the regulation of the expression of cyclases and phosphodiesterases by oxidative stress on vascular development have not been investigated. Our results suggest that combined inhibition of sGC and Pde4 expressions by hyperoxia generates an intracellular microenvironment in which cGMP production is reduced, while cAMP is synthesized but not hydrolyzed at a normal rate, a setting that is not permissive for vasculogenesis and angiogenesis. Interestingly, the expression of sGC, Pde4B and Pde4C returned to normal levels after recovery in normoxia, although these cultures displayed an abnormally developed vasculature. This result suggests that alterations in the levels of cGMP and cAMP caused by oxidative stress at early time of EC differentiation carry critical consequences for the overall formation of the vascular system.
To understand if targeting the sGC/cGMP system could rescue oxygen-induced endothelial precursor dysfunction, we have evaluated the effects of exogenously applied cGMP on ECs during differentiation under oxidative stress. We found that cGMP, under hyperoxic conditions, functioned as a powerful vascular protectant that, although unable to maintain normal levels of endothelial differentiation/proliferation, effectively rescued the ability of newly differentiated ECs to organize into vessel-like structures and promoted angiogenesis. Similar results were obtained when EBs were co-treated with oxygen and MMQ, a highly specific inhibitor of PDE5, the enzyme responsible for cGMP degradation. This latter result is intriguing because hyperoxia downregulates close to 80% of sGC mRNA but it is in line with the observation that the presence of 5–10% of normal sGC levels is sufficient to elicit maximal vasodilation [46]. Thus, it is possible that PDE5 inhibition by MMQ during oxygen exposure generates physiologically relevant intracellular concentrations of cGMP, despite the low levels of sGC mRNA, and thereby prevents hyperoxic damage of EPC functions. Unfortunately, the effects of oxygen and MMQ on cGMP levels in EBs cannot be determined directly because the intracellular concentration of cGMP is below detectable levels in oxygen–treated EBs (personal observations). Although beneficial effects of sGC-cGMP signaling on developmental angiogenesis [24, 47–49] and angiogenesis in ischemic pathological settings [50, 51] have been described, to the best of our knowledge this is the first direct demonstration that cGMP, or treatments that preserve sufficient cGMP levels, correct the vascular defect induced by oxidative stress in EPCs.
Specific inhibitors of the cyclases or PDE4 provided further support for the role of balanced levels of cGMP and cAMP in vascular development. Disruption of sGC activity with ODQ, a selective inhibitor of sGC, or treatment of developing EBs with rolipram, a specific inhibitor of PDE4 (data not shown), completely abolished the ability of maturing ECs to organize into a vascular plexus under normoxic conditions. This vascular defect occurred in the presence of normal VEGF-A levels, suggesting that cGMP and cAMP function downstream of VEGF-A. Interestingly, both treatments led to the formation of endothelial clumps resembling those observed during the defective vascular development of hyperoxic EBs. In contrast, lowering the levels of cAMP by inhibiting AC6 activity during oxidative stress prevented endothelial defects at later stages of vascular development. These results suggested that cGMP- and cAMP-regulating enzymes are active from the beginning of endothelial differentiation and play a critical role in vascular development. These findings are in agreement with a previous study in which the expression of sGC in early developing EBs was reported [52]. In addition, our results indicated that a proper balance between cGMP and cAMP is crucial for normal blood vessel formation under both normoxic and hyperoxic conditions and that lowering cGMP or increasing cAMP levels at the time of endothelial commitment affect later phases of vascular development.
How balanced levels of cGMP and cAMP protect differentiating ECs from oxidative stress and allow them to form new blood vessels is not clear. Both cyclic nucleotides mediate a wide range of biological effects that allow cells to respond and adapt to different stimuli. Orchestrated activities of the cyclases and Pdes contribute to these diverse physiological responses by regulating the steady-state levels of cyclic nucleotides and their intracellular localization [53]. Proper EC migration, a requisite for new vessel establishment, requires correct cytoskeletal reorganization [54]. It is possible that oxygen-induced unbalance between cGMP and cAMP affects intracellular components of the actinomyosin cytoskeleton, microtubules, or integrins, resulting in impaired EC motility and assemblage into vessels. In addition to the shift in the balance between cGMP and cAMP in the favor of cAMP, oxidative stress could cause a restriction of cAMP to specific subcellular compartments and induce unwanted cAMP-mediated responses [55]. For example hyperoxia could force accumulation of high levels of cAMP at the plasma membrane and cause cAMP-mediated stabilization of cell–cell adhesions and consequently impaired EC migration and vessel formation [56–58].
The precise mechanism underlying oxygen-induced defect in vascular development requires further elucidation. Regardless of the exact mechanism, our data showed high sensitivity of EPCs to oxidative stress and identify regulators of cyclases and PDEs as possible therapeutic strategies to protect EPCs in pathological conditions associated with oxidative stress, such as inflammation, diabetes and retinopathies.
References
Asahara T, Murohara T, Sullivan A, Silver M, Van Der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM (1997) Isolation of putative progenitor endothelial cells for angiogenesis. Science 275(5302):964–967
Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M, Kearne M, Magner M, Isner JM (1999) Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 85(3):221–228
Takahashi T, Kalka C, Masuda H, Chen D, Silver M, Kearney M, Magner M, Isner JM, Asahara T (1999) Ischemia- and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med 5(4):434–438
Masuda H, Kalka C, Asahara T (2000) Endothelial progenitor cells for regeneration. Hum Cell 13(4):153–160
Tepper OM, Capla JM, Galiano RD, Ceradini DJ, Callaghan MJ, Kleinman ME, Gurtner GC (2005) Adult vasculogenesis occurs through in situ recruitment, proliferation, and tubulization of circulating bone marrow-derived cells. Blood 105(3):1068–1077
Ingram DA, Krier TR, Mead LE, McGuire C, Prater DN, Bhavsar J, Saadatzadeh MR, Bijangi-Vishehsaraei K, Li F, Yoder MC, Haneline LS (2007) Clonogenic endothelial progenitor cells are sensitive to oxidative stress. Stem Cells 25(2):297–304
Fujinaga H, Baker CD, Ryan SL, Markham NE, Seedorf GJ, Balasubramaniam V, Abman SH (2009) Hyperoxia disrupts vascular endothelial growth factor-nitric oxide signaling and decreases growth of endothelial colony-forming cells from preterm infants. Am J Physiol Lung Cell Mol Physiol 297(6):L1160–L1169
Dernbach E, Urbich C, Brandes RP, Hofmann WK, Zeiher AM, Dimmeler S (2004) Antioxidative stress-associated genes in circulating progenitor cells: evidence for enhanced resistance against oxidative stress. Blood 104(12):3591–3597
He T, Peterson TE, Holmuhamedov EL, Terzic A, Caplice NM, Oberley LW, Katusic ZS (2004) Human endothelial progenitor cells tolerate oxidative stress due to intrinsically high expression of manganese superoxide dismutase. Arterioscler Thromb Vasc Biol 24(11):2021–2027
Carmeliet P (2000) Mechanisms of angiogenesis and arteriogenesis. Nat Med 6(4):389–395
Senger DR, Ledbetter SR, Claffey KP, Papadopoulos-Sergiou A, Peruzzi CA, Detmar M (1996) Stimulation of endothelial cell migration by vascular permeability factor/vascular endothelial growth factor through cooperative mechanisms involving the alphavbeta3 integrin, osteopontin, and thrombin. Am J Pathol 149(1):293–305
Carmeliet P, Ferreira V, Breier G, Pollefeyt S, Kieckens L, Gertsenstein M, Fahrig M, Vandenhoeck A, Harpal K, Eberhardt C, Declercq C, Pawling J, Moons L, Collen D, Risau W, Nagy A (1996) Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele. Nature 380(6573):435–439
Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9(6):669–676
Ferrara N (2009) Vascular endothelial growth factor. Arterioscler Thromb Vasc Biol 29(6):789–791
Fukumura D, Gohongi T, Kadambi A, Izumi Y, Ang J, Yun CO, Buerk DG, Huang PL, Jain RK (2001) Predominant role of endothelial nitric oxide synthase in vascular endothelial growth factor-induced angiogenesis and vascular permeability. Proc Natl Acad Sci USA 98(5):2604–2609
Janssens SP, Shimouchi A, Quertermous T, Bloch DB, Bloch KD (1992) Cloning and expression of a cDNA encoding human endothelium-derived relaxing factor/nitric oxide synthase. J Biol Chem 267(21):14519–14522
Gooch KJ, Dangler CA, Frangos JA (1997) Exogenous, basal and flow-induced nitric oxide production and endothelial cell proliferation. J Cell Physiol 171(3):252–258
Dimmeler S, Zeiher AM (1999) Nitric oxide-an endothelial cell survival factor. Cell Death Differ 6(10):964–968
Dimmeler S, Dernbach E, Zeiher AM (2000) Phosphorylation of the endothelial nitric oxide synthase at ser-1177 is required for VEGF-induced endothelial cell migration. FEBS Lett 477(3):258–262
Murohara T, Asahara T, Silver M, Bauters C, Masuda H, Kalka C, Kearney M, Chen D, Symes JF, Fishman MC, Huang PL, Isner JM (1998) Nitric oxide synthase modulates angiogenesis in response to tissue ischemia. J Clin Invest 101(11):2567–2578
Ziche M, Morbidelli L (2000) Nitric oxide and angiogenesis. J Neurooncol 50(1–2):139–148
Parenti A, Morbidelli L, Cui X-L, Douglas JG, Hood JD, Granger HJ, Ledda F, Ziche M (1998) Nitric oxide is an upstream signal of vascular endothelial growth factor-induced extracellular signal-regulated kinase(1/4) activation in postcapillary endothelium. J Biol Chem 273(7):4220–4226
Al-Ani B, Hewett PW, Ahmed S, Cudmore M, Fujisawa T, Ahmad S, Ahmed A (2006) The release of nitric oxide from S-nitrosothiols promotes angiogenesis. PLoS One 1:e25
Pyriochou A, Beis D, Koika V, Potytarchou C, Papadimitriou E, Zhou Z, Papapetropoulos AJ (2006) Soluble guanylyl cyclase activation promotes angiogenesis. J Pharmacol Exp Ther 319(2):663–671
Leitman DC, Fiscus RR, Murad F (1986) Forskolin, phosphodiesterase inhibitors, and cyclic AMP analogs inhibit proliferation of cultured bovine aortic endothelial cells. J Cell Physiol 127(2):237–243
Favot L, Keravis T, Holl V, Le Bec A, Lugnier C (2003) VEGF-induced HUVEC migration and proliferation are decreased by PDE2 and PDE4 inhibitors. Thromb Haemost 90(2):334–343
Pyriochou A, Papapetropoulos A (2005) Soluble guanylyl cyclase: more secrets revealed. Cell Signal 17(4):407–413
Cooper DM (2003) Regulation and organization of adenylyl cyclases and cAMP. Biochem J 375(Pt3):517–529
Lugnier C (2006) Cyclic nucleotide phosphodiesterase (PDE) superfamily: a new target for the development of specific therapeutic agents. Pharmacol Ther 109(3):366–398
Netherton SJ, Maurice DH (2005) Vascular endothelial cell cyclic nucleotide phosphodiesterases and regulated cell migration: implications in angiogenesis. Mol Pharmacol 67(1):263–272
Papapetropoulos A, Cziraki A, Rubin JW, Stone CD, Catravas JD (1996) cGMP accumulation and gene expression of soluble guanylate cyclase in human vascular tissue. J Cell Physiol 167(2):213–221
Creighton JR, Masada N, Cooper DM, Stevens T (2003) Coordinate regulation of membrane cAMP by Ca2+-inhibited adenylyl cyclase and phosphodiesterase activities. Am J Physiol Lung Cell Mol Physiol 284(1):L100–L107
Karbanova J, Mokry J (2002) Histological and histochemical analysis of embryoid bodies. Acta Histochem 104(4):361–365
Evans AL, Bryant J, Skepper J, Smith S, Print CG, Charnock-Jones DS (2007) Vascular development in embryoid bodies: quantification of transgenic intervention and antiangiogenic treatment. Angiogenesis 10(3):217–226
Jakobsson L, Kreuger J, Claesson-Welsh L (2007) Building blood vessels-stem cell models in vascular biology. J Cell Biol 177(5):751–755
Rozen S, Skaletsky HJ (2000) Primer3 on the WWW for general users and for biologist programmers. In: Krawetz S, Misener S (eds) Bioinformatics methods and protocols: methods in molecular biology. Humana Press, Totowa, pp 365–386
Murphy CL, Polak JM (2002) Differentiating embryonic stem cells: GAPDH, but neither HPRT nor beta-tubulin is suitable as an internal standard for measuring RNA levels. Tissue Eng 8(4):551–559
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25(4):402–408
Yamaguchi TP, Dumont DJ, Conlon RA, Breitman ML, Rossant J (1993) flk-1, an flt-related receptor tyrosine kinase is an early marker for endothelial cell precursors. Development 118(2):489–498
Vittet D, Prandini MH, Berthier R, Schweitzer A, Martin-Sisteron H, Uzan G, Dejana E (1996) Embryonic stem cells differentiate in vitro to endothelial cells through successive maturation steps. Blood 88(9):3424–3431
Case J, Ingram DA, Haneline LS (2008) Oxidative stress impairs endothelial progenitor cell function. Antioxid Redox Signal 10(11):1895–1907
Bautch VL, Redick SD, Scalia A, Harmaty M, Carmeliet P, Rapoport R (2000) Characterization of the vasculogenic block in the absence of vascular endothelial growth factor-A. Blood 95(6):1979–1987
Gerassimou C, Kotanidou A, Zhou Z, Simoes DC, Roussos C, Papapetropoulos A (2007) Regulation of the expression of soluble guanylyl cyclase by reactive oxygen species. Br J Pharmacol 150(8):1084–1091
Papapetropoulos A, Abou-Mohamed G, Marczin N, Murad F, Caldwell RW, Catravas JD (1996) Downregulation of nitrovasodilator-induced cyclic GMP accumulation in cells exposed to endotoxin or interleukin-1 beta. Br J Pharmacol 118(6):1359–1366
Hoffmann LS, Schmidt PM, Keim Y, Schaefer S, Schmidt HH, Stasch JP (2009) Distinct molecular requirements for activation or stabilization of soluble guanylyl cyclase upon haem oxidation-induced degradation. Br J Pharmacol 157(5):781–795
Mergia E, Friebe A, Dangel O, Russwurm M, Koesling D (2006) Spare guanylyl cyclase NO receptors ensure high NO sensitivity in the vascular system. J Clin Invest 116(6):1731–1737
Krumenacker JS, Murad F (2006) NO-cGMP signaling in development and stem cells. Mol Genet Metab 87(4):311–314
Pyriochou A, Zhou Z, Koika V, Petrou C, Cordopatis P, Sessa WC, Papapetropoulos A (2007) The phosphodiesterase 5 inhibitor sildenafil stimulates angiogenesis through a protein kinase G/MAPK pathway. J Cell Physiol 211(1):197–204
Aicher A, Heeschen C, Feil S, Hofmann F, Mendelsohn ME, Feil R, Dimmeler S (2009) cGMP-dependent protein kinase I is crucial for angiogenesis and postnatal vasculogenesis. PLoS One 4(3):e4879
Senthilkumar A, Smith RD, Khitha J, Arora N, Veerareddy S, Langston W, Chidlow JH Jr, Barlow SC, Teng X, Patel RP, Lefer DJ, Kevil CG (2007) Sildenafil promotes ischemia-induced angiogenesis through a PKG-dependent pathway. Arterioscler Thromb Vasc Biol 27(9):1947–1954
Dussault S, Maingrette F, Ménard C, Michaud SE, Haddad P, Groleau J, Turgeon J, Perez G, Rivard A (2009) Sildenafil increases endothelial progenitor cell function and improves ischemia-induced neovascularization in hypercholesterolemic apolipoprotein E-deficient mice. Hypertension 54(5):1043–1049
Mujoo K, Krumenacker JS, Wada Y, Murad F (2006) Differential expression of nitric oxide signaling components in undifferentiated and differentiated human embryonic stem cells. Stem Cells Dev 15(6):779–787
Cooper DM (2005) Compartmentalization of adenylate cyclase and cAMP signalling. Biochem Soc Trans 33(Pt6):1319–1322
Schmidt A, Brixius K, Bloch W (2007) Endothelial precursor cell migration during vasculogenesis. Circ Res 101(2):125–136
DeFouw LM, DeFouw DO (2001) Differential phosphodiesterase activity contributes to restrictive endothelial barrier function during angiogenesis. Microvasc Res 62(3):263–270
Creighton J, Zhu B, Alexeyev M, Stevens T (2008) Spectrin-anchored phosphodiesterase 4D4 restricts cAMP from disrupting microtubules and inducing endothelial cell gap formation. J Cell Sci 121(Pt1):110–119
Fukuhara S, Sakurai A, Sano H, Yamagishi A, Somekawa S, Takakura N, Saito Y, Kangawa K, Mochizuki N (2005) Cyclic AMP potentiates vascular endothelial cadherin-mediated cell-cell contact to enhance endothelial barrier function through an Epac-Rap1 signaling pathway. Mol Cell Biol 25(1):136–146
Abraham S, Yeo M, Montero-Balaguer M, Paterson H, Dejana E, Marshall CJ, Mavria G (2009) VE-Cadherin-mediated cell-cell interaction suppresses sprouting via signaling to MLC2 phosphorylation. Curr Biol 19(8):668–674
Acknowledgments
This work was supported in part by a donation from the Jack Cary Eichenbaum Foundation. We thank Marian Acevedo, Andrea Zambetti, and Jenifer Lee for their technical help. We thank Dr. David Moscatelli for critical reading of the manuscript. We also thank Dr. Frederick Naftolin for making the EVOS Digital Fluorescence Microscope available to us.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Curatola, A.M., Xu, J. & Hendricks-Munoz, K.D. Cyclic GMP protects endothelial progenitors from oxidative stress. Angiogenesis 14, 267–279 (2011). https://doi.org/10.1007/s10456-011-9211-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-011-9211-7