Abstract
Here we review the mechanisms by which Thymosin β4 (Tβ4) regulates angiogenesis, its role in processes, such as wound healing and tumour progression and we discuss in more detail the role of Tβ4 in the cardiovascular system and significant recent findings implicating Tβ4 as a potential therapeutic agent for ischaemic heart disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The β-thymosin family
The β-thymosins, which were first isolated from the thymus in the 1960s [1], comprise a family of structurally related 40–44 amino acid polypeptides with hormone-like properties [2]. They are biochemically and functionally distinct from the α- and γ-thymosins, having in common only their original identification as “thymic hormones”. β-thymosins are potent regulators of actin polymerisation in a range of cells and tissues and are evolutionarily conserved in species from mammals to echinoderms but absent from prokaryotes and yeast [3, 4]. Up to date, 15 β-thymosins have been identified although most mammalian tissues investigated express only two [2]. Thymosin β4 (Tβ4) is the most abundant member in most cell types, present in concentrations, as high as 0.4 mM and representing approximately 70–80% of the total β-thymosin content [5–7]. Mammalian species express either thymosin β10 (Tβ10; human, rat, mouse, rabbit and cat) or thymosin β9 (Tβ9; calf, pig, sheep) as the second β-thymosin [2]; a third peptide, thymosin β15 (Tβ15) has additionally been identified in human and rat cells although, in most cases, from metastatic carcinoma tissues and tumour cell lines [8, 9].
Cell morphogenesis and motility depends on precisely regulating the dynamics of the actin cytoskeleton. Rapid cycles of actin assembly and disassembly require a number of actin binding proteins including the β-thymosins, the actin-binding competitor profilin [10] and the depolymerisation factor cofilin [11, 12]. By sequestering actin monomers, β-thymosins function to maintain a large pool of actin monomers (G-actin), which when required, are de-sequestered by profilin to induce rapid filament (F-actin) polymerisation. This process underlies the formation of filamentous structures such as lamellipodia and filopodia, responsible for mediating cell motility and guidance [13, 14]. Mutation of the actin-binding motif of Tβ4, 17LKKTETQEK25, prevents actin polymerisation leading to the accumulation of monomeric actin and cytoskeletal defects [15]. Over the last 15 years, studies have implicated the β-thymosins in a number of cellular events such as wound healing, apoptosis, inflammatory responses and angiogenesis [2], processes which fundamentally depend upon cell migration.
Regulation of angiogenesis by the β-thymosins
A number of β-thymosins, along with some of the α-thymosins, impact on the process of angiogenesis; intriguingly, despite the high degree of sequence homology between isoforms of each family, some α- and β-thymosins are known to promote angiogenesis and other members inhibit angiogenesis. While a number of studies have described the angiogenic properties of individual thymosins [16, 17], the most comprehensive cross-family comparisons derive from the work of Koutrafouri et al. In an in vivo chick chorioallantoic membrane model, Tβ4, Tβ15, prothymosin α1 (proTα1) and thymosin α1 (Tα1) were found to enhance angiogenesis, almost to the same extent as a positive control, β-PMA [18, 19] (Fig. 1a). In contrast, Tβ10, Tβ9 and parathymosin α (paraTα) inhibited angiogenesis to a level comparable with hydrocortisone, a negative regulator of angiogenesis. Interaction between β-thymosins, with respect to angiogenic function was also assessed since Tβ4 and Tβ10 frequently co-exist in mammalian cells. When a constant concentration of Tβ4 was combined with increasing concentrations of Tβ10, the pro-angiogenic effect of Tβ4 was eventually overridden by the anti-angiogenic effect of Tβ10; conversely, the effect of Tβ10 was reversed by increasing concentrations of Tβ4 to produce a net positive effect of promoting angiogenesis (Fig. 1b). Indeed, Tβ10 was shown to be sufficiently anti-angiogenic to abrogate vascular endothelial growth factor (VEGF)-induced angiogenesis and tumour growth in a mouse orthoptic tumour model [20].
Effect of thymosins on angiogenesis. (a) Various α- and β-thymosins were assessed for their angiogenic capacities in the chick chorioallantoic membrane (CAM) in vivo model and are compared with known positive and negative regulators, β-PMA and hydrocortisone. (b) The combined effect of pro- and anti- angiogenic β-thymosins (Tβ4 and Tβ10, respectively), in varying proportions, on angiogenesis, as assessed in the CAM model. Reproduced from Koutrafouri et al. [18]© 2001, with permission from Elsevier
It is intriguing that both α- and β-thymosins regulate cell migration and angiogenesis when they appear not to share any structural or biochemical properties. Indeed, the α-thymosins do not even possess an actin-binding motif, which was found to be critically required for activation of cell migration by Tβ4 [21]. The balance between positive and negative regulators of angiogenesis is reflected in their distinct expression profiles during embryogenesis and tumorigenesis. For example, in the developing cardiovascular system, high Tβ4 and low Tβ10 levels prevail, consistent with the need for extensive de novo vasculogenesis [22, 23]; Tβ4 levels in these tissues diminish by late embryonic and early neonatal stages ([24] and N. Smart, unpublished data) when the need for vasculogenesis has diminished.
This review will focus primarily on the role of Tβ4 in regulating angiogenesis, with occasional references to other members of the β-thymosin family.
Tβ4 promotes angiogenesis
The first intimation of a role for Tβ4 in angiogenesis came from its identification in a screen for rapidly induced (<4 h) genes following culture of human umbilical vein endothelial cells (HUVECs) on either plastic or Matrigel (basement membrane matrix) [25]. A five-fold induction of Tβ4 was observed during endothelial cell differentiation in vitro and transfection of HUVECs with Tβ4 caused an increase in the rate of attachment and spreading and an accelerated rate of tube formation [25]. Further, insight into the influence of Tβ4 on endothelial cell migration came from migration assays demonstrating that Tβ4 acts as a chemoattractant for endothelial cells, stimulating directional migration (as opposed to random motility or chemokinesis) of HUVECs in Boyden chamber assays (4–6-fold over media alone) [26]. The effect of Tβ4 on migration was proposed to be endothelial cell-specific since HUVECs and human coronary artery endothelial cells migrated in response to Tβ4 but foreskin fibroblasts, aortic smooth muscle cells, neutrophils, monocytes and HT1080 human fibrosarcoma cells showed no significant migration towards Tβ4, yet migrated towards their respective positive controls (bFGF, PDGF-BB, FMLP or laminin). Additionally, Tβ4 significantly accelerated the rate of endothelial cell migration in vivo in a subcutaneous Matrigel plug assay [26]. The first evidence that Tβ4 could directly promote angiogenesis came again from Grant and co-workers; they reported that, in addition to stimulating proliferation, attachment and differentiation of endothelial cells, Tβ4 induced tubule formation on Matrigel, vascular sprouting of coronary artery rings (an assay which assesses all steps of in vivo capillary formation) and angiogenesis (a doubling of vessel area via increased branching) with as little as 0.1 μg/ml Tβ4 [27] (Fig. 2). This study also offered the first mechanistic insight; the angiogenic response appeared to involve the binding of Tβ4 to an unknown cell surface receptor, internalisation of the peptide and rearrangement of the actin cytoskeleton. However, receptor binding appeared not to be mediated through the actin-binding motif, LKKTET. These were the first data postulating the existence of a Tβ4 receptor and the possibility of a paracrine role.
Thymosin β4 promotes angiogenesis. Tβ4 promotes capillary sprouting in a coronary artery ring assay (b) at concentrations, as low as 0.1 μg/ml, compared with control (a). Mean vessel area was quantified with computer assisted image analysis (NIH image) and displayed as relative mean vessel area square pixels (c). Modified from Grant et al. [27]© 2000, with permission from Springer Netherlands
That Tβ4 induces angiogenesis by promoting migration of endothelial and other vasculogenic cells is now clearly established [21, 28, 29] yet the precise mechanism by which Tβ4 directs cell migration is only tenuously defined and the role of actin binding versus other receptor-mediated events is still a matter of debate. Philp et al. tested the angiogenic activity of full length Tβ4, proteolytic fragments and synthetic peptides in HUVEC Boyden chamber migration assays and in vessel sprouting assays using chick aortic arch assays [21]. The authors concluded that the actin-binding motif of Tβ4 was both necessary and sufficient in its own right to promote angiogenesis. However, since endothelial cell migration was reduced but not ablated following deletion of the LKKTET motif, the possibility remains that other regions of the peptide are required for maximal effect. This result raises a curious and unexplained enigma; if the Tβ4 actin-binding motif is sufficient to promote cell migration and angiogenesis, why do other β-thymosins, such as Tβ10, inhibit angiogenesis despite sharing the highly conserved actin-binding motif? Moreover, as described above, there is the issue of α-thymosin-induced angiogenesis in the absence of a recognised actin binding motif. These disparities may be reconciled with further understanding of other sequence elements and also of the signalling pathways and protein complexes with which thymosins interact. If reorganisation of the actin cytoskeleton is indeed required for migration, it is plausible that α-thymosins may bind actin indirectly as part of a multiprotein complex or elicit an effect via another actin binding protein.
AcSDKP, a cleavage product of Tβ4, promotes angiogenesis
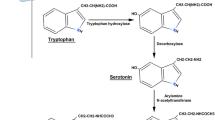
Endoproteinase cleavage of Tβ4 leads to production of N-acetyl-seryl-aspartyl-lysyl-proline (AcSDKP) [7, 30], a potent pro-angiogenic, anti-fibrotic peptide that is degraded exclusively by angiotensin-converting enzyme (ACE) [31]. Tβ4 was identified as the likely precursor for AcSDKP, as it possesses the tetrapeptide sequence at its N-terminus and the enzyme prolyl oligopeptidase has been shown to cleave the Pro-Asp bond to release AcSDKP [32]. Work characterising transgenic Tβ4 knockdown mice has provided further evidence in support of a precursor-peptide relationship between Tβ4 and AcSDKP in a physiological setting.
In addition to inhibiting hematopoietic stem cell proliferation, AcSDKP stimulates endothelial cell migration and differentiation in vitro and secretion of active MMP-1. It promotes a significant in vivo angiogenic response in the chick embryo chorioallantoic model and in matrigel plugs planted subcutaneously into rat muscle [33]. Clearly, there is an extensive overlap of pro-angiogenic properties shared between AcSDKP and its precursor Tβ4 [29, 34].
Wound healing
Formation of new blood vessels is a fundamental component of wound healing. Reports of Tβ4 as a major constituent of ulcer extracts, wound and blister fluids led to speculation that it may play a role in wound repair [35]. Malinda et al. first assessed whether Tβ4 could enhance wound healing in a rat full thickness wounding assay [28]. Topical or intraperitoneal administration of Tβ4 increased epithelialisation, collagen deposition, angiogenesis and wound contraction, identifying Tβ4 as a potent wound healing factor, as had previously been shown for Tα1 [16]. Subsequent studies from the Kleinman laboratory characterised the wound healing capacity of Tβ4 in aged and diabetic rodents [36, 37], since impaired angiogenesis in aged animals results in poor wound healing. Based on these pre-clinical studies, Tβ4 is currently subject to phase 2 clinical trials (RegeneRx, Inc., Bethesda, USA) for treatment of epidermolysis bullosa in infants and pressure ulcers, a common problem for the elderly and infirm.
A further aspect of wound healing which may be amenable to Tβ4 treatment in the future is repair of the cornea [38]. Corneal abrasions are frequently caused by entry of foreign particles such as sand or dust, contact lenses or exposure to ultraviolet radiation and, if untreated, can lead to severe visual impairment. Topical application of Tβ4 was shown to promote corneal repair by inducing conjuctival epithelial cell migration, [39] increasing cell–cell and cell–matrix contacts, inhibiting apoptosis [40] and suppressing the activity of matrix metalloproteinases, MMP-2, MMP-9 and MT6-MMP [41]. Interestingly, however, no increased angiogenesis was observed in the eye, even following prolonged treatment with Tβ4 [41]. Instead, Tβ4-induced corneal repair appears to be largely mediated via suppression of the inflammatory response, notably the NFκB/TNF-α pathway [42].
Tβ4 and tumour progression
The progression of cancers is intrinsically linked with angiogenesis, since tumour growth and metastasis depend upon neovascularisation. Since the first report of Tβ10 up-regulation in renal cell carcinomas in 1991 [24], DNA array methodology has revealed a frequent correlation between dysregulated β-thymosin expression and tumour progression [9, 29, 43–52]. In particular, increased β-thymosin levels were associated with augmented metastatic potential, presumably reflecting the need of these cell types both to migrate [43, 44, 47] and induce vascularisation. Tβ4 overexpression was associated with an increase in the number of blood vessels in solid tumours derived from injected B16-F10 cells and induction of angiogenesis by Tβ4 was associated with up-regulation of VEGF expression [29]. Tβ15, in particular, may prove to be an extremely useful diagnostic marker because, unlike prostate-specific antigen, Tβ15 is not expressed in non-cancerous prostate tissue [9]. Levels of the Tβ4 cleavage product, AcSDKP, were also found to be five-fold higher in malignant thyroid tumours compared with benign lesions [53], an indication that malignancy and metastasis are further common properties shared by AcSDKP and its precursor, Tβ4.
Tβ4 in the cardiovascular system
Even before the angiogenic properties of Tβ4 had been fully appreciated, its expression in the developing cardiovascular system had been reported with the detection of elevated levels of Tβ4 in blood vessels and endocardial cushions of early mouse postimplantation embryos [22].
Subsequent, more detailed studies in the mouse revealed Tβ4 expression at embryonic day (E) 10 in ventricular myocardium, in two distinct regions of the proximal outflow tract, the pericardium and endocardium including the endocardial cushions of the atrio-ventricular canal (cells responsible for invading and separating myocardium from endocardium) and in regions of presumptive migratory cardiac crest, migrating through the pharyngeal arch region [54]. Tβ4 is also expressed in the outer curvature of the right ventricle at E11.5 and by E12.5, expression is expanded throughout the outflow tract and present in the ventricular septum and compact layer [55]. At E14.5, Tβ4 is robustly expressed throughout the myocardium, the epicardium and in endothelial and smooth muscle cells surrounding the great vessels [56].
Based on its prominent expression pattern in blood vessels, Tβ4 similarly appears to play a role in the developing cardiovascular system of the chick [57]. Interestingly, the earliest expression of Tβ4 was detected in the extra-embryonic blood-circulatory system, a lineage which has not yet been investigated, in other species. HH-24 (Hamburger and Hamilton stage 24) embryos displayed strong Tβ4 expression in the capillary network covering the embryonic body and Tβ4-expressing cells were also seen at the surface of the heart anlage, in the developing endocardial cushions and surrounding the oesophagus. The underlying endoderm which plays an important role in heart induction [58] was also strongly Tβ4 positive. Notably, expression was detected in developing coronary vessels in stage HH-24 embryos, but absent in later stage embryos implicating Tβ4 in formation rather than maintenance of vessels.
The profile of Tβ4 was rapidly elevated in 2004 after Srivastava et al. published on the potential for Tβ4 to restore function to the ischemic adult mouse heart [55]. Tβ4 promoted myocardial and endothelial cell migration in the embryonic heart, a property retained in post-natal cardiomyocytes, and significantly enhanced survival and repair of adult cardiomyocytes via activation of the survival kinase, Akt. Following coronary artery ligation in mice, Tβ4 treatment led to increased myocardial preservation and improved cardiac function. The benefits of Tβ4 treatment were attributed to the observed activation of Akt; angiogenic processes and improved vascularisation of the infarcted myocardium were not determined.
Tβ4 is required for coronary vasculogenesis, angiogenesis and arteriogenesis
By selectively knocking down Tβ4 in the developing heart, Smart and co-workers recently characterised an essential role for Tβ4 in regulating all three key stages of cardiac vessel development [56]. Formation of the coronary arteries consists of a precisely orchestrated series of molecular and morphogenetic events which can be divided into three distinct processes: vasculogenesis, angiogenesis and arteriogenesis (Fig. 3; reviewed in [59, 60]). Even subtle perturbations in this process may lead to congenital coronary artery anomalies, as occur in 0.2–1.2% of the general population [61]. Reduced levels of Tβ4 resulted in defects in the overlying epicardium of the developing heart, a lineage which plays a pivotal role in the development of the coronary vasculature (Fig. 4) [62–66] and demonstrated an absolute requirement for Tβ4-induced vasculogenesis in a physiological setting.
Development of the coronary vasculature. Schematic representation of the developing heart and coronary vasculature in the mouse. As the myocardium thickens, trabeculation increases diffusion capacity and oxygen supply until the epicardium forms over the heart to contribute angioblasts for vasculogenesis. The primitive vasculature expands throughout the myocardium by angiogenesis. Following connection to the aorta, the vessels gain support from smooth muscle cells (arteriogenesis). EC: endothelial cell; SMC: smooth muscle cell. Reproduced from Luttun and Carmeliet [60] ©2003 with permission from Elsevier
Epicardium-derived cells are precursors for fibroblasts, endothelial and smooth muscle cells. Following delamination, EPDCs undergo epithelial-mesenchymal transition, migrate into the sub-epicardium and myocardium before differentiating. VEGF and bFGF promote differentiation into endothelial cells while PDGF and TGFβ direct epicardial cells towards a smooth muscle fate. Angioblasts and hemangioblasts form vascular tubes and smooth muscle progenitors form arteries and muscular veins. Modified from Tomanek [59], © 2005 with permission from Springer Netherlands
Embryos with reduced myocardial Tβ4 levels displayed a number of striking cardiac defects at E14.5, including a thin non-compacted myocardium and a detached epicardium which was mottled with abnormal surface nodules, which appeared to represent aberrant vessels [61] (Fig. 5). Disrupted coronary vasculogenesis was apparent after immunostaining of coronary endothelial cells with the endothelial specific receptor, Tie2 [67]. Micro-vessels lined with Tie2 positive cells were seen throughout the dense myocardium of control hearts while the disrupted myocardium of mutant embryos was almost entirely negative for Tie2; the few vessel-like structures present were grossly malformed. In contrast, the epicardial nodules of mutant embryos were intensely stained with Tie2, suggestive of trapping of endothelial cells in nodules at the epicardium. Being also derived from the epicardium, smooth muscle cell recruitment to coronary vessels was also disrupted in Tβ4 knockdown hearts. Smooth muscle cells, labelled for smooth muscle α-actin (SMαA), were evident throughout the control myocardium, specifically surrounding the lumen of micro-vessels. Such expression was lacking in mutant hearts and SMαA positive cells instead persisted in the epicardium and sub-epicardial layer. These data suggest that, as a consequence of reduced Tβ4 signalling from the myocardium, EPDCs, fated to form endothelial and smooth muscle cells, fail to migrate into the myocardium to provide support to the coronary vessels and instead activate their respective differentiation programmes in situ within the epicardium. Interestingly, Tβ4 knockdown embryos also displayed defective recruitment of SMαA-positive smooth muscle cells (arteriogenesis) to the large thoracic vessels which resulted in haemorrhaging; defective angiogenesis resulted in a failure in branching of the aorta and consequent absence of the right subclavian artery.
Tβ4 is required for coronary vasculature formation. Frontal sections through the ventricular myocardium (my) of Tβ4shNk embryos at E14.5; arising from crosses between conditional Tβ4 floxed short hairpin (sh) RNA transgenic mice and heart-specific Nkx2.5Cre (Nk) expressing mice. Embryos are stained with haematoxylin and eosin to visualise epicardial nodules which represent aberrant coronary vessels; black arrowhead (a, b). Smooth muscle α-actin (SMαA) positive cells surround the cannular epicardial nodules (c). Modified from Smart et al. (2007) [56]
The effect of Tβ4 on the developing epicardium in vivo was supported by studies on epicardial explant cultures [56, 68], examining the differentiated cell types formed following outgrowth. Addition of Tβ4 significantly increased the numbers of SMαA positive and Tie2 positive cells and these cell populations were enhanced further still with the addition of VEGF and FGF7 [56] (Fig. 6).
Tβ4 promotes differentiation of EPDCs. EPDCs display maximum potential for differentiation from cultured E10.5 hearts, assessed in culture (other stages not shown). Tβ4 promotes differentiation of smooth muscle (SMαA positive) and endothelial (Tie2 positive) cells, the latter additionally requiring VEGF and FGFs. Modified from Smart et al. (2007) [56]
From these studies it was concluded that Tβ4 signals in a paracrine manner from the myocardium to cells of the epicardium. Cells delaminate from the epicardium, undergo EMT, migrate into the myocardium and differentiate into endothelial cells to form coronary vessels and smooth muscle cells to stabilise vessls. (Fig. 7) In a knockdown situation, there is significantly less Tβ4 to signal to the epicardium. Epicardial cells may undergo EMT but the majority fail to migrate into the myocardium and instead undergo differentiation in the epicardium. As this is a knockdown not knockout system, some cells are able to migrate inwards and a few structures resembling vessels can be seen. However, the lack of smooth muscle cells to support the vessels results in their regression.
Model for the role of Tβ4 in coronary vessel development. During normal heart development (left panel), epicardial derived cells (EPDCs) undergo an epithelial to mesenchyme transition (EMT) in response to BMP, FGF and TGFβ signalling from the myocardium. Secreted myocardial Tβ4 then induces EPDCs to migrate into the myocardium where they respond to angio- (VEGF/bFGF) or arteriogenic (PDGF/TGFβ) factors and differentiate into either endothelial or smooth muscle cells respectively, thus establishing a capillary plexus and stabilisation of coronary vessels. Following knockdown of myocardial Tβ4 (right panel) EPDCs undergo EMT but fail to migrate, becoming trapped in the epicardium where they differentiate into Tie2 and SMαA positive cells. Failure in Tβ4-induced EPDC migration results in significantly impaired vasculogenesis, defective collateral growth and vascular regression which in turn leads to a severe reduction in cardiomyocyte survival manifested as a thin compact layer and disrupted myocardial architecture. Reproduced from Smart et al. (2007) [56]
What is the role of AcSDKP in coronary vasculogenesis?
Both Tβ4 and AcSDKP have recognised angiogenic properties, yet the individual contribution of each peptide had not previously been addressed in a physiological setting. Tβ4 knockdown in the developing heart was accompanied by a significant (40%) reduction in AcSDKP [56]. In order to directly test, whether reduction in myocardial AcSDKP contributed to the vasculogenic defects in Tβ4 knockdown embryos, rescue was attempted by injection of pregnant females with AcSDKP which restored the tetrapeptide to control levels but failed to rescue any aspect of the mutant phenotype. While AcSDKP can stimulate cell migration and angiogenesis, it proved incapable of substituting for Tβ4 in this context, possibly indicating the need for actin binding and filament assembly, consistent with earlier studies in chick aortic arch assays.
Tβ4 promotes neovasculogenesis via adult epicardium
Translation of a vascular development role for Tβ4 to that of angiogenic therapy for coronary artery disease in the adult heart relies on the release of the adult epicardium from a quiescent state and restoration of pluripotency. In order to investigate the potential for Tβ4 in this context, the ability of Tβ4 to induce outgrowth and differentiation of isolated epicardial explants from adult hearts was assessed (Fig. 8) This was the first successful culture of adult epicardial explants since it was previously perceived that adult epicardium resides in a state of dormancy, having lost all potential for migration, differentiation and signalling during late embryonic stages [68]. Indeed, untreated adult explants displayed virtually no detectable outgrowth (Fig. 8a). In contrast, treatment with Tβ4 stimulated extensive outgrowth of cells (Fig. 8b) which, as they migrated away from the explant, differentiated into a variety of discernable cellular phenotypes. The emerging epithelial cells were positive for the epicardial-specific transcription factor epicardin and these cells differentiated, with migration, into procollagen type I, SMαA and Flk1 positive cells indicative of fibroblasts, smooth muscle and endothelial cells (Fig. 8d–h). As discussed above, these cells represent the definitive progenitors for the coronary microvasculature and the data of Smart et al., therefore, demonstrate that, under the control of Tβ4, vasculogenic potential remains within the adult epicardium, which may be harnessed for use in therapeutic angiogenesis. In support of these observation, Van Tuyn et al. reported that epicardial cells from human adult heart can undergo EMT and obtain characteristics of smooth muscle cells in vitro [69].
Tβ4 promotes migration of adult epicardium derived precursor cells and enables their differentiation into vasculogenic cells. Outgrowth of large colonies of cells from adult heart explants stimulated by Tβ4 (b, c), compared with a minimal degree of migration from untreated explants (a). Emerging cells (d, blue box) identified as epicardial cells (e). Following migration, cells undergo differentiation into smooth muscle cells (b, d green box), fibroblasts (b, d yellow box, f) and endothelial cells (b, d red box, h). Whilst unable to promote significant epicardial outgrowth beyond control levels (i), AcSDKP brought about rapid differentiation of any emerging EPDCs, such that the differentiated cells were almost exclusively Flk1 positive endothelial cells (k, l). Modified from Smart et al (2007) [56]
Whilst unable to significantly promote epicardial outgrowth beyond control levels, AcSDKP brought about rapid differentiation of emerging EPDCs such that cells observed in close proximity to the explant tissue were almost exclusively endothelial (Flk1 positive) with very few smooth muscle cells or fibroblasts (Fig. 8i–l) [56]. This suggests that AcSDKP, cleaved from Tβ4, exclusively promotes EPDC endothelial cell differentiation and may underlie a compound vasculogenic effect of Tβ4.
In considering the epicardium as a source of vascular progenitors, valuable insight may be derived from studies in the zebrafish. Following ventricular resection of the adult fish heart, the epicardium exhibits a rapid and robust response to injury, which includes proliferation and expression of embryonic epicardial markers (Tbx18 and RALDH2), within 1–2 days of resection [70]. The activated epicardium envelopes the cardiac chambers, including the injured apex and a subpopulation of cells invades the sub-epicardial space and myocardium to contribute endothelial and smooth muscle cells to form new coronary vessels; this is highly reminiscent of the processes involving the epicardium during mouse embryonic heart development, for which Tβ4 was required [56]. It is highly significant, therefore that, in a related study, the fish orthologue of Tβ4 was found to be up-regulated in regenerating zebrafish hearts [71]. Taken together, these data, along with the ability of Tβ4 to mobilise murine adult EPDCs, provide strong support for the potential of Tβ4 to induce neovascularisation and possibly other aspects of myocardial regeneration, in the injured adult heart.
Release of quiescent EPDCs represents a viable source of vascular progenitors for continued renewal of regressed vessels at low basal level or sustained neovascularisation following cardiac injury. The feasibility of employing Tβ4 in therapeutic angiogenesis for the injured adult heart has not been assessed in vivo. Although the minimum requirement of Tβ4-induced EPDC migration from adult heart has been realized [56] it remains to be confirmed whether Tβ4 can promote neovascularisation to restore a functional vasculature and maintain cardiomyocyte survival in the injured heart. Certainly, Tβ4 has been shown to improve cardiomyocyte survival and functional recovery post myocardial infarction (MI) [55], but the underlying mechanism has not been defined. Neovascularisation of the ischemic myocardium represents the most likely mechanism for conferring cardioprotection.
Does endogenous Tβ4 stimulate angiogenesis?
The mammalian myocardium responds to stresses, including ischaemia, by activating a multitude of adaptive mechanisms that seek both to limit cellular injury and to prepare for any subsequent insult and is essentially the basis of ischaemic preconditioning. It is highly significant, therefore, that endogenous levels of both Tβ4 and AcSDKP were up-regulated following MI (Fig. 9) [56], implying a possible role for these pro-angiogenic peptides in the intrinsic mechanism of cardioprotection. The minimal degree of protection afforded by endogenous Tβ4 and AcSDKP is clearly insufficient, since it does not significantly salvage the myocardium from ischaemic damage; however, injected Tβ4 has been shown to limit scar volume and improve cardiac function post-MI [55]. This may simply reflect a higher concentration of Tβ4 attained in the myocardium following injection, although the exact levels were not reported. Alternatively, injected Tβ4 may act either on a cell type other than cardiomyocytes or its cardioprotective effects may be initiated extracellularly not intracellularly, possibly via activation of a cell surface receptor, as discussed below. It is unlikely that the endogenous levels of Tβ4, even after MI-induced up-regulation, would be secreted at a level comparable to that achieved by injection. Although inadequate in terms of its protective benefits, endogenous Tβ4 and AcSDKP up-regulation may be pharmacologically manipulated for therapeutic benefit, once the endogenous mechanism is fully understood and when further insight has been gained into the optimal route for delivery of Tβ4.
Tβ4 and AcSDKP are up-regulated following myocardial infarction. Myocardial infarction induces an increase in endogenous Tβ4 (a) and AcSDKP expression levels (b) in the adult heart, determined by Western blot and enzyme immunoassay, respectively. Reproduced from Smart et al. (2007) [56]
The potential for Tβ4-induced neovascularisation via other cardiac progenitor cells
The data illustrating that Tβ4 contributes to coronary vessel development and to mobilisation of adult epicardial progenitors are of real significance in light of the current drive to identify reservoirs of adult cardiac progenitor cells that may regenerate coronary vessels, in addition to replacement cardiomyocytes, valves and the conduction system. Bone marrow derived mesenchymal stem cells (BMSCs) are the most extensively studied of the potential cardiac progenitor cells, although their ability to transdifferentiate is equivocal, controversial and, on the whole, disputed [72, 73]. However, BMSCs may offer potential benefit through their secretion of paracrine factors that are cardioprotective or angiogenic. Significantly, Tβ4 levels were elevated in Akt over-expressing BMSCs [74], particularly under hypoxic conditions; injection of Akt-MSCs or even their conditioned medium considerably reduced infarct size and improved cardiac function. That conditioned medium conferred a comparable degree of cardiac repair suggests that, besides contributing new cardiac or vascular progenitors, secretion of angiogenic factors contributes significantly towards neovascularisation induced by BMSCs.
Until recently, the prevailing dogma was that vessels in the embryo derived from endothelial progenitors, whereas angiogenesis in the adult derived only from division of differentiated endothelial cells. A wealth of evidence has since emerged to indicate that endothelial progenitors can also contribute to vessel growth in ischaemic, malignant and inflamed tissues in the adult and present themselves as a potential vehicle for therapeutic vasculogenesis [75–79]. Clonal embryonic endothelial progenitor cells (eEPCs) home specifically to hypoxic areas in tumour metastases, but spare (normal) organs and well-vascularised tumours [80, 81]. On this basis, Kupatt and co-workers investigated the ability of transplanted eEPCs to induce neovascularisation and tissue rescue in two animal models of vascular disease, myocardial ischaemia in mice and limb ischaemia in rabbits [82]. Local administration of embryonic cells in rabbits or systemic injection in mice led to a measurable increase in neovascularisation and improved tissue recovery. In order to investigate the underlying mechanism of neovasularisation in these models, genome-wide expression profiling of eEPCs were performed. eEPCs are a rich source of secreted proteins that modulate tissue angiogenesis and tissue repair. Alongside recognised angiogenic factors such as VEGFA and VEGFB, Tβ4, proTα and Tβ10 were found to be among the most abundant of factors secreted by eEPCs.
Although much remains to be determined regarding the efficacy of cardiac progenitor cell treatment, it is clear that Tβ4 offers tremendous therapeutic potential for cardiac regeneration, be it via paracrine secretion to mediate the mobilisation and homing of BMSCs or eEPCs or via direct stimulation of resident epicardial cells.
The mechanism of Tβ4-induced angiogenesis
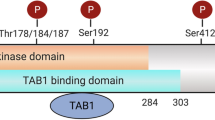
Over the past 15 years, a number of studies have contributed towards our understanding of the mechanism of Tβ4 function and it is now recognised that Tβ4 is involved in a wide range of cellular processes aside from regulating cytoskeletal assembly (Fig. 10). However, it is not entirely clear how some of the functions are mediated or indeed which combination of functions is required for a single process, such as angiogenesis.
Proposed mechanisms of Tβ4 action. Multiple facets of the Tβ4 mechanism may account for its ability to promote angiogenesis. In addition to regulating the dynamics of the actin cytoskeleton, Tβ4 may activate a cell surface receptor to initiate intracellular signal transduction via multiple pathways, thereby increasing the range of its effects. Furthermore, Tβ4 has been shown to enter the nucleus, raising the possibility that it could influence transcription and may explain the reported effects of Tβ4 at the level of gene expression
A number of gene expression changes have been reported following Tβ4 treatment raising speculation that it may, in some way, modify transcription, consistent with its translocation to the nucleus [83]. The most notable of genes from an angiogenic perspective is probably VEGF. An up-regulation of VEGF was first described following overexpression of Tβ4 in B16-F10 lung tumour cells [29]; conversely, a down-regulation of VEGF in situ was observed in Tβ4 knockdown hearts suggesting that appropriate VEGF expression may require Tβ4 [56]. Furthermore, in the study investigating cardioprotective effects of Akt-over expressing BMSCs, both Tβ4 and VEGF were significantly up-regulated in the MSCs during hypoxia, as potential mediators of myocardial protection [74]. However, it has yet to be determined, whether there is a direct interaction between Tβ4 and VEGF, or whether Tβ4 mediates an effect on VEGF expression via intermediaries, such as hypoxia-inducible factor α (HIF1α). In keeping with the fact that pro-angiogenic Tβ4 leads to an increase in VEGF levels, anti-angiogenic Tβ10 down-regulates several factors including VEGF and VEGFR-1, supporting the correlation between β-thymosin expression, VEGF levels and angiogenesis [17].
Among the other genes up-regulated by Tβ4 are cytoskeletal-related proteins, including myosin IIA, α-actinin, tropomyosin, talin, α5-integrin, vinculin [84] and zyxin [85], extracellular matrix (ECM) components such as laminin-5 [86] and matrix metalloproteinases, which degrade components of ECM [41, 87] consistent with a role for Tβ4 in co-ordinating the necessary changes to the cytoskeleton and ECM which are required to effect cell migration.
Contrary to the report of Hannapel and Leibold [88], who suggested that Tβ4 may not be a secretory peptide, the consensus is now that β-thymosins can be secreted from a range of cell types and exert a paracrine effect upon adjacent cells by internalisation and/or receptor activa tion [20, 29, 55, 56, 89, 90]. However, neither a definitive Tβ4 receptor nor, for that matter, the mechanism of secretion have been identified. The identification of the respective receptors for Tβ4 and AcSDKP (which may in fact be the same) is crucial to the understanding of their function and therapeutic potential and should facilitate the elucidation of downstream signalling pathways, further clarifying the mechanisms behind their diverse range of effects. A complete understanding of the mechanisms of Tβ4 action is essential for the evolution of more efficient therapies for wound healing and ischaemic heart disease.
References
Goldstein AL, Slater FD, White A (1966) Preparation, assay, and partial purification of a thymic lymphocytopoietic factor (thymosin). Proc Natl Acad Sci USA 56:1010–1017
Huff T, Muller C, Otto A, Netzker R, Hannappel E (2001) β-thymosins, small acidic peptides with multiple functions. Int J Biochem Cell Biol 33:205–220
Sanders MC, Goldstein AL, Wang Y (1992) Thymosin {beta}4 (Fx Peptide) is a potent regulator of actin polymerization in living cells. PNAS 89:4678–4682
Stanka Stoeva SHWV (1997) A novel β-thymosin from the sea urchin: extending the phylogenetic distribution of β-thymosins from mammals to echinoderms. J Pept Sci 3:282–290
Low TL, Hu SK, Goldstein AL (1981) Complete amino acid sequence of bovine thymosin β4: a thymic hormone that induces terminal deoxynucleotidyl transferase activity in thymocyte populations. Proc Natl Acad Sci USA 78:1162–1166
Low TL, Goldstein AL (1982) Chemical characterization of thymosin beta 4. J Biol Chem 257:1000–1006
Goldstein AL, Hannappel E, Kleinman HK (2005) Thymosin β4: actin-sequestering protein moonlights to repair injured tissues. Trends Mol Med 11:421–429
Lere B, Massimo L, Bruce RZ (1998) Thymosin β15 expression in tumor cell lines with varying metastatic potential. Clin Exp Metastasis 16:227–233
Bao L, Loda M, Janmey PA, Stewart R, nand-Apte B, Zetter BR (1996) Thymosin β 15: a novel regulator of tumor cell motility upregulated in metastatic prostate cancer. Nat Med 2:1322–1328
Sun HQ, Kwiatkowska K, Yin HL (1995) Actin monomer binding proteins. Curr Opin Cell Biol 7:102–110
Ghosh M, Song X, Mouneimne G, Sidani M, Lawrence DS, Condeelis JS (2004) Cofilin promotes actin polymerization and defines the direction of cell motility. Science 304:743–746
Lappalainen P, Drubin D (1997) Cofilin promotes rapid actin filament turnover in vivo. Nature 388:78–82
Faix J, Rottner K (2006) The making of filopodia. Curr Opin Cell Biol 18:18–25
Chen H, Bernstein B, Bamburg J (2000) Regulating actin-filament dynamics in vivo. Trends Biol Sci 25:19–23
Van Troys M, Dewitte D, Goethals M, Carlier MF, Vandekerckhove J, AMpe C (1996) The actin binding site of thymosin beta 4 mapped by mutational analysis. EMBO J 15:201–210
Malinda KM, Sidhu GS, Banaudha KK, Gaddipati JP, Maheshwari RK, Goldstein AL, Kleinman HK (1998) Thymosin {alpha}1 stimulates endothelial cell migration, angiogenesis, and wound healing. J Immunol 160:1001–1006
Mu H, Ohashi R, Yang H, Wang X, Li M, Lin P, Yao Q, Chen C (2006) Thymosin beta10 inhibits cell migration and capillary-like tube formation of human coronary artery endothelial cells. Cell Motil Cytoskeleton 63(4):222–230
Koutrafouri V, Leoniadis L, Avgoustakis K, Livianou E, Czarnecki J, Ithakissios D, Evangelatos G (2001) Effect of thymosin peptides on the chick chorioallantoic membrane angiogenesis model. Biochim Biophys Acta 1568:60–66
Koutrafouri V, Leondiadis L, Ferderigos N, Avgoustakis K, Livaniou E, Evangelatos GP, Ithakissios DS (2003) Synthesis and angiogenetic activity in the chick chorioallantoic membrane model of thymosin β15. Peptides 24:107–115
Lee SH, Son MJ, Oh SH, Rho SB, Park K, Kim YJ, Park MS, Lee JH (2005) Thymosin β10 inhibits angiogenesis and tumor growth by interfering with Ras function. Cancer Res 65:137–148
Philp D, Huff T, Gho YS, Hannappel E, Kleinman HK (2003) The actin binding site on thymosin β4 promotes angiogenesis. FASEB J 17:2103–2105
Gomez-Marquez J, del Amo F, Carpintero P, Anadon R (1996) High levels of mouse thymosin β4 mRNA in differentiating P19 embryonic cells and during development of cardiovascular tissues. Biochim Biophys Acta 1306:187–193
Carpintero P, Franco dA, Anadon R, Gomez-Marquez J (1996) Thymosin β10 mRNA expression during early postimplantation mouse development. FEBS Lett 394:103–106
Hall AK (1991) Differential expression of thymosin genes in human tumors and in the developing human kidney. Int J Cancer 48:672–677
Grant D, Kinsella J, Kibbey M, LaFlamme S, Burbelo P, Goldstein A, Leinman H (1995) Matrigel induces thymosin(β4 gene in differentiating endothelial cells. J Cell Sci 108:3685–3694
Malinda K, Goldstein A, Kleinman H (1997) Thymosin β4 stimulates directional migration of human umbilical vein endothelial cells. FASEB J 11:474–481
Grant DS, Rose W, Yaen C, Goldstein A, Martinez J, Kleinman H (1999) Thymosin β4 enhances endothelial cell differentiation and angiogenesis. Angiogenesis 3:125–135
Malinda K, Sidhu G, Mani H, Banaudha K, Mashewari R, Goldstein A, Kleinman H (1999) Thymosin β4 accelerates wound healing. J Invest Dermatol 113:364–368
Cha HJ, Jeong MJ, Kleinman HK (2003) Role of thymosin β4 in tumor metastasis and angiogenesis. J Natl Cancer Inst 95:1674–1680
Grillon C, Rieger K, Bakala J, Schott D, Morgat JL, Hannappel E, Voelter W, Lenfant M (1990) Involvement of thymosin β4 and endoproteinase Asp-N in the biosynthesis of the tetrapeptide AcSerAspLysPro a regulator of the hematopoietic system. FEBS Lett 274:30–34
Rieger KJ, Saez-Servent N, Papet MP, Wdzieczak-Bakala J, Morgat JL, Thierry J, Voelter W, Lenfant M (1993) Involvement of human plasma angiotensin I-converting enzyme in the degradation of the haemoregulatory peptide N-acetyl-seryl-aspartyl-lysyl-proline. Biochem J 296(Pt 2):373–378
Cavasin MA, Rhaleb NE, Yang XP, Carretero OA (2004) Prolyl oligopeptidase is involved in release of the antifibrotic peptide Ac-SDKP. Hypertension 43:1140–1145
Liu JM, Lawrence F, Kovacevic M, Bignon J, Papadimitriou E, Lallemand JY, Katsoris P, Potier P, Fromes Y, Wdzieczak-Bakala J (2003) The tetrapeptide AcSDKP, an inhibitor of primitive hematopoietic cell proliferation, induces angiogenesis in vitro and in vivo. Blood 101:3014–3020
Bonnet D, Lemoine FM, Frobert Y, Bonnet ML, Baillou C, Najman A, Guigon M (1996) Thymosin(β4, inhibitor for normal hematopoietic progenitor cells. Exp Hematol 24:776–782
Frohm M, Gunne H, Bergman AC, Agerberth B, Bergman T, Boman A, Liden S, Jornvall H, Boman HG (1996) Biochemical and antibacterial analysis of human wound and blister fluid. Eur J Biochem 237:86–92
Philp D, Badamchian M, Scheremeta B, Nguyen M, Goldstein A, Kleinman H (2003) Thymosin β4 and a synthetic peptide containing its actin-binding domain promote dermal wound repair in db/db diabetic mice and in aged mice. Wound Repair Regen 11:19–24
Philp D, Goldstein AL, Kleinman HK (2004) Thymosin [beta]4 promotes angiogenesis, wound healing, and hair follicle development. Mech Ageing Dev 125:113–115
Sosne G, Chan C, Thai K, Kennedy M, Szliter E, Hazlett L, Kleinman H (2001) Thymosin beta 4 promotes corneal wound healing and modulates inflammatory mediators in vivo. Exp Eye Res 72:605–608
Sosne G, Hafeez S, Greenberry AL, Kurpakus-Wheater M (2002) Thymosin beta4 promotes human conjunctival epithelial cell migration. Curr Eye Res 24:268–273
Sosne G, Siddiqi A, Kurpakus-Wheater M (2004) Thymosin-{beta}4 Inhibits Corneal Epithelial Cell Apoptosis after Ethanol Exposure In vitro. Invest Ophthalmol Vis Sci 45:1095–1100
Sosne G, Christopherson PL, Barrett RP, Fridman R (2005) Thymosin-{beta}4 modulates corneal matrix metalloproteinase levels and polymorphonuclear cell infiltration after alkali injury. Invest Ophthalmol Vis Sci 46:2388–2395
Sosne G, Qiu P, Christopherson PL, Wheater MK (2007) Thymosin beta 4 suppression of corneal NF[kappa]B: a potential anti-inflammatory pathway. Exp Eye Res 84:663–669
Clark E, Golub T, Lander E, Hynes R (2000) Genomic analysis of metastasis reveals an essential role for RhoC. Nature 406:532–535
Ridley A (2000) Molecular switches in metastasis. Nature 406:466–467
Kobayashi T, Okada F, Fujii N, Tomita N, Ito S, Tazawa H, Ayoama T, Choi S, Shibita T, Fujita H, Hosokawa M (2002) Thymosin-β4 regulates motility and metastasis of malignant mouse fibrosarcoma cells. Am J Pathol 160:869–882
Diamond DL, Zhang Y, Gaiger A, Smithgall M, Vedvick TS, Carter D (2003) Use of proteinchip(TM) array surface enhanced laser desorption/ionization time-of-flight mass spectrometry (seldi-tof ms) to identify thymosin [beta]-4, a differentially secreted protein from lymphoblastoid cell lines. J Am Soc Mass Spectrom 14:760–765
Wang W-S, Chen P-M, Hsiao H-L, Ju S-Y, Su Y (2003) Overexpression of the thymosin b-4 gene is associated with malignant progression of SW480 colon cancer cells. Oncogene 22:3297–3306
Yamamoto T, Gotoh M, Kitajima M, Hirohashi S (1993) Thymosin [beta]-4 expression is correlated with metastatic capacity of colorectal carcinomas. Biochem Biophys Res Commun 193:706–710
Verghese-Nikolakaki S, Apostolikas N, Livaniou E, Ithakissios DS, Evangelatos GP (1996) Preliminary findings on the expression of thymosin beta-10 in human breast cancer. Br J Cancer 74:1441–1444
Santelli G, Califano D, Chiappetta G, Vento MT, Bartoli PC, Zullo F, Trapasso F, Viglietto G, Fusco A (1999) Thymosin beta-10 gene overexpression is a general event in human carcinogenesis. Am J Pathol 155:799–804
Viglietto G, Califano D, Bruni P, Baldassarre G, Vento MT, Belletti B, Fedele M, Santelli G, Boccia A, Manzo G, Santoro M, Fusco A (1999) Regulation of thymosin beta10 expression by TSH and other mitogenic signals in the thyroid gland and in cultured thyrocytes. Eur J Endocrinol 140:597–607
Lee S-H, Zhang W, Choi J-J, Cho Y-S, Lee S-H, Kim J-W, Hu L, Xu J, Liu J, Lee J-H (2001) Overexpression of the thymosin β-10 gene in human ovarian cancer cells disrupts F-actin stress fiber and leads to apoptosis. Oncogene 20:6700–6706
Kusinski M, Wdzieczak-Bakala J, Liu JM, Bignon J, Kuzdak K (2006) AcSDKP: a new potential marker of malignancy of the thyroid gland. Langenbecks Arch Surg 391:9–12
Smart N, Hill AA, Cross JC, Riley PR (2002) A differential screen for putative targets of the bHLH transcription factor Hand1 in cardiac morphogenesis. Mech Dev 119:S65–S71
Bock-Marquette I, Saxena A, White MD, Dimaio JM, Srivastava D (2004) Thymosin β4 activates integrin-linked kinase and promotes cardiac cell migration, survival and cardiac repair. Nature 432:466–472
Smart N, Risebro CA, Melville AAD, Moses K, Schwartz RJ, Chien KR, Riley PR (2007) Thymosin β4 induces adult epicardial progenitor mobilization and neovascularization. Nature 445:177–182
Dathe V, Brand-Saberi B (2004) Expression of thymosin beta4 during chick development. Anat Embryol (Berl) 208:27–32
Schultheiss TM, Xydas S, Lassar AB (1995) Induction of avian cardiac myogenesis by anterior endoderm. Development 121:4203–4214
Carmeliet P (2000) Mechanisms of angiogenesis and arteriogenesis. Nat Med 6:389–395
Risau W (1997) Mechanisms of angiogenesis. Nature 386:671–674
von Kodolitsch Y, Franzen O, Lund GK, Koschyk DH, Ito WD, Meinertz T (2004) Coronary artery anomalies Part I: recent insights from molecular embryology. Z Kardiol 93:929–937
Poelmann RE, Lie-Venema H, Gittenberger-de Groot AC (2002) The role of the epicardium and neural crest as extracardiac contributors to coronary vascular development. Tex Heart Inst J 29:255–261
Manasek FJ (1969) Embryonic development of the heart. II. Formation of the epicardium. J Embryol Exp Morphol 22:333–348
Viragh S, Challice CE (1981) The origin of the epicardium and the embryonic myocardial circulation in the mouse. Anat Rec 201:157–168
Munoz-Chapuli R, Gonzalez-Iriarte M, Carmona R, Atencia G, Macias D, Perez-Pomares JM (2002) Cellular precursors of the coronary arteries. Tex Heart Inst J 29:243–249
Wessels A, Perez-Pomares JM (2004) The epicardium and epicardially derived cells (EPDCs) as cardiac stem cells. Anat Rec A Discov Mol Cell Evol Biol 276:43–57
Ward NL, Dumont DJ (2002) The angiopoietins and Tie2/Tek: adding to the complexity of cardiovascular development. Semin Cell Dev Biol 13:19–27
Chen TH, Chang TC, Kang JO, Choudhary B, Makita T, Tran CM, Burch JBE, Eid H, Sucov HM (2002) Epicardial induction of fetal cardiomyocyte proliferation via a retinoic acid-inducible trophic factor. Dev Biol 250:198–207
van Tuyn J, Atsma DE, Winter EM, van der Velde-van Dijke I, Pijnappels DA, Bax NAM, Knaan-Shanzer S, Gittenberger-de Groot AC, Poelmann RE, van der Laarse A, van der Wall EE, Schalij MJ, de Vries AAF (2006) Epicardial cells of human adults can undergo an epithelial-to-mesenchymal transition and obtain characteristics of smooth muscle cells in vitro. Stem Cells 25:271–278, DOI:10.1634/stemcells.2006–0366
Lepilina A, Coon AN, Kikuchi K, Holdway JE, Roberts RW, Burns C, Poss KD (2006) A dynamic epicardial injury response supports progenitor cell activity during zebrafish heart regeneration. Cell 127:607–619
Lien CL, Schebesta M, Makino S, Weber GJ, Keating MT (2006) Gene expression analysis of zebrafish heart regeneration. PLoS Biol 4(8):e260
Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson SM, Li B, Pickel J, McKay R, Nadal-Ginard B, Bodine DM, Leri A, Anversa P (2001) Bone marrow cells regenerate infarcted myocardium. Nature 410:701–705
Murry CE, Soonpaa MH, Reinecke H, Nakajima H, Nakajima HO, Rubart M, Pasumarthi KB, Virag JI, Bartelmez SH, Poppa V, Bradford G, Dowell JD, Williams DA, Field LJ (2004) Haematopoietic stem cells do not transdifferentiate into cardiac myocytes in myocardial infarcts. Nature 428:664–668
Gnecchi M, He H, Noiseux N, Liang OD, Zhang L, Morello F, Mu H, Melo LG, Pratt RE, Ingwall JS, Dzau VJ (2006) Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. FASEB J 20:661–669
Isner JM, Asahara T (1999) Angiogenesis and vasculogenesis as therapeutic strategies for postnatal neovascularization. J Clin Invest 103:1231–1236
Rafii S, Lyden D, Benezra R, Hattori K, Heissig B (2002) Vascular and haematopoietic stem cells: novel targets for anti-angiogenesis therapy? Nat Rev Cancer 2:826–835
Takahashi T, Kalka C, Masuda H, Chen D, Silver M, Kearney M, Magner M, Isner JM, Asahara T (1999) Ischemia- and cytokine-induced mobilization of bone marrow-derived endothelial progenitor cells for neovascularization. Nat Med 5:434–438
Kalka C, Isner JM (2002) [Cardiac and vascular gene therapy in cardiology. Current status and future prospects]. Internist (Berl) 43(Suppl 1):S66–S75
Reyes M, Dudek A, Jahagirdar B, Koodie L, Marker PH, Verfaillie CM (2002) Origin of endothelial progenitors in human postnatal bone marrow. J Clin Invest 109:337–346
Wei J, Blum S, Unger M, Jarmy G, Lamparter M, Geishauser A, Vlastos GA, Chan G, Fischer KD, Rattat D, Debatin KM, Hatzopoulos AK, Beltinger C (2004) Embryonic endothelial progenitor cells armed with a suicide gene target hypoxic lung metastases after intravenous delivery. Cancer Cell 5:477–488
Vajkoczy P, Blum S, Lamparter M, Mailhammer R, Erber R, Engelhardt B, Vestweber D, Hatzopoulos AK (2003) Multistep nature of microvascular recruitment of ex vivo-expanded embryonic endothelial progenitor cells during tumor angiogenesis. J Exp Med 197:1755–1765
Kupatt C, Horstkotte J, Vlastos GA, Pfosser A, Lebherz C, Semisch M, Thalgott M, Buttner K, Browarzyk C, Mages J, Hoffmann R, Deten A, Lamparter M, Muller F, Beck H, Buning H, Boekstegers P, Hatzopoulos AK (2005) Embryonic endothelial progenitor cells expressing a broad range of proangiogenic and remodeling factors enhance vascularization and tissue recovery in acute and chronic ischemia. FASEB J 19:1576–1578
Huff T, Rosorius O, Otto AM, Muller CSG, Ballweber E, Hannappel E, Mannherz HG (2004) Nuclear localisation of the G-actin sequestering peptide thymosin β4. J Cell Sci 117:5333–5341
Golla R, Philp N, Chintipalli J, Hoffmann R, Collins L, Nachmias V (1997) Co-ordinate regulation of the cytoskeleton in 3T3 cells overexpressing thymosin-β4. Cell Motil Cytoskeleton 38:187–200
Moon HS, Even-Ram S, Kleinman HK, Cha HJ (2006) Zyxin is upregulated in the nucleus by thymosin beta4 in SiHa cells. Exp Cell Res 312:3425–3431
Sosne G, Xu L, Prach L, Mrock LK, Kleinman HK, Letterio JJ, Hazlett LD, Kurpakus-Wheater M (2004) Thymosin beta 4 stimulates laminin-5 production independent of TGF-beta. Exp Cell Res 293:175–183
Chang C, Werb Z (2001) The many faces of metalloproteases: cell growth, invasion, angiogenesis and metastasis. Trends Cell Biol 11:S37–S43
Hannappel E, Leibold W (1985) Biosynthesis rates and content of thymosin β4 in cell lines. Arch Biochem Biophys 240:236–241
Huang WQ, Wang QR (2001) Bone marrow endothelial cells secrete thymosin β4 and AcSDKP. Exp Hematol 29:12–18
Huang HC, Hu CH, Tang MC, Wang WS, Chen PM, Su Y (2006) Thymosin β4 triggers an epithelial-mesenchymal transition in colorectal carcinoma by upregulating integrin-linked kinase. Oncogene 26(19):2781–2790
Acknowledgements
We thank all of the investigators who allowed us to reproduce figures and provided originals, as referenced. Our work is supported by the British Heart Foundation and the Medical Research Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smart, N., Rossdeutsch, A. & Riley, P.R. Thymosin β4 and angiogenesis: modes of action and therapeutic potential. Angiogenesis 10, 229–241 (2007). https://doi.org/10.1007/s10456-007-9077-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-007-9077-x