Abstract
Although burst and high-frequency (HF) spinal cord stimulation (SCS) relieve neuropathic pain, their effects on neuronal hyperexcitability have not been compared. Specifically, it is unknown how the recharge components of burst SCS—either actively balanced or allowed to passively return—and/or different frequencies of HF SCS compare in altering neuronal activity. Neuronal firing rates were measured in the spinal dorsal horn on day 7 after painful cervical nerve root compression in the rat. Motor thresholds (MTs) and evoked neuronal recordings were collected during noxious stimuli before (baseline) and after delivery of SCS using different SCS modes: 10 kHz HF, 1.2 kHz HF, burst with active recharge, or burst with passive recharge. Spontaneous firing rates were also evaluated at baseline and after SCS. The average MT for 10 kHz SCS was significantly higher (p < 0.033) than any other mode. Burst with passive recharge was the only SCS mode to significantly reduce evoked (p = 0.019) and spontaneous (p = 0.0076) firing rates after noxious pinch. This study demonstrates that HF and burst SCS have different MTs and effects on both evoked and spontaneous firing rates, indicating they have different mechanisms of providing pain relief. Since burst with passive recharge was the only waveform to reduce firing, that waveform may be important in the neurophysiological response to stimulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord stimulation (SCS) is widely used to treat a variety of chronic neuropathic pain conditions for patients whom conventional therapies are inadequate.20 Conventional SCS delivers low-frequency, tonic electrical pulses to the dorsal column of the spinal cord, which provides analgesia but also produces paresthesia sensations (tingling or buzzling) that some patients find uncomfortable.3,20 Both high frequency (HF) SCS and BurstDR™ SCS have been found to be superior to low-frequency tonic SCS in treating neuropathic pain, while also reducing or eliminating paresthesias.4,9,10,11,15,16,17,28 HF SCS administers tonic pulses in kilohertz frequency ranges, and both 1–1.2 kHz HF and 10 kHz HF have shown effective pain relief in animal models and in clinical trials.15,17,21,24,26,29 Most SCS systems approved by the Food & Drug Administration (FDA) are capable of delivering frequencies up to 1.2 kHz, whereas the availability of 10 kHz is more limited only to certain devices. In contrast to tonic SCS, burst stimulation delivers electrical pulses in bursts of several pulses, with the bursts separated by a quiescent period; its efficacy depends on the specific burst parameters used.5 The main stimulation phase of each pulse is followed by the recharge phase, which has the opposite polarity of the stimulation phase to maintain net charge neutrality over the course of the burst. Although the recharge phase can be delivered in either an active or passive manner, the effect, if any, of the recharge phase profile used with the burst SCS paradigm has not been studied experimentally.
Preclinical animal studies investigating the mechanisms of SCS use painful nerve root compression in the rat, since it mimics the clinical symptoms of neuropathic pain, and induces spinal hyperexcitability and glial activation.2,5,6,14,23 Prior studies have shown that monophasic burst SCS (without the recharge phase) effectively suppresses dorsal horn neuronal activity, and may operate through different neurochemical mechanisms than low-frequency tonic stimulation.5,6 Moreover, both monophasic burst SCS and HF SCS reduce mechanical hyperalgesia (i.e., pain) following nerve ligation.5,6,24 However, the effects of biphasic burst SCS and kilohertz HF on spinal neuronal firing remains unclear. Recently, several working theories of the mechanisms of HF SCS have been refuted by preclinical and computational modeling studies, which show that this stimulation paradigm failed to significantly inhibit windup of dorsal horn neurons24 or cause direct activation or conduction block of dorsal column or dorsal root fibers.19 So, the goal of this foundational study was to detect if there are differences in evoked and/or spontaneous neuronal firing rates after application of different modes of SCS in a rat model of painful radiculopathy, including 10 kHz HF, 1.2 kHz HF, and burst SCS with either a passive recharge phase (BurstDR) or an active recharge phase. The results of this study provide a better understanding of these SCS paradigms and their relative neurophysiological effects.
Methods
Painful Nerve Root Compression Surgery
Male Holtzman rats (275–299 g; Envigo; Indianapolis, IN, USA) were housed with free access to food and water. All experimental procedures were approved by the University of Pennsylvania Institutional Animal Care and Use Committee and carried out under the guidelines of the Committee for Research and Ethical Issues of the International Association for the Study of Pain.32
Painful nerve root compression was imposed in rats (n = 5) under isoflurane inhalation anesthesia (4% for induction, 2.5% for maintenance) as previously described.6,13,25,30 The number of rats in this study is small and the recording protocol used in this study limits data acquisition to only 1–3 neurons per rat. But, using pilot data from this study and prior work,5,6 6–21 neurons are predicted to be needed for significance in most outcomes. This study used 9 neurons which was predicted to be adequate to detect differences for one of the stimuli (pinch) used to evoke responses. Briefly, each rat was placed in a prone position and a midline incision was made from the base of the skull to the T2 thoracic spinous process. The spinal column was exposed via muscle resection, followed by a C6/C7 laminectomy and partial facetectomy on the right side to expose the unilateral C7 dorsal nerve root. The right dorsal root was compressed using a 10-gf microvascular clip (World Precision Instruments; Sarasota, FL, USA) for 15 min (Fig. 1a). After clip removal, the incision was closed using 3-0 polyester suture and surgical staples and rats were monitored during recovery in room air. Prior to, and at day 7 after, nerve root compression, mechanical hyperalgesia was measured by applying a series of von Frey filaments to the plantar surface of the bilateral forepaws of each rat to ensure behavioral sensitivity was present during SCS application.
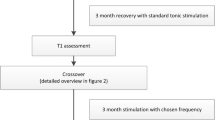
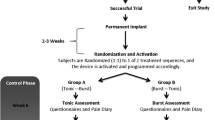
Schematic of injury procedure, SCS application and dorsal horn neuron recording, and the SCS protocol. (a) On day 0, the C7 dorsal nerve root underwent a painful 15-min compression using a vascular clip. (b) On day 7 after the compression, a monopolar SCS electrode was placed at the midline of the C3/C4 dorsal columns. Evoked neural firing was recorded from the ipsilateral C7 dorsal horn. After recording baseline responses, SCS was applied for 5 min. Neuron responses were recorded immediately (0 min), 2, 5, 10, and 15 min after SCS. (c) Each of the four SCS modes was applied in a randomized order: burst with active recharge, burst with passive recharge, 10 kHz HF, and 1.2 kHz HF. Schematics of burst SCS with active and passive recharge show the different recharge components.
Neuron Recordings & Spinal Cord Stimulation
Extracellular electrophysiological recordings were performed at day 7 after nerve root compression, in which neuronal firing rates were measured in response to different SCS modes. Rats were anesthetized with sodium pentobarbital (45 mg/kg, i.p.) and given supplementary doses (5–10 mg/kg, i.p.) as needed based on hind foot and corneal reflexes. The C3–C8 spinal cord was exposed by laminectomy and dural resection. Rats were placed on a stereotaxic frame (David Kopf Instruments; Tujunga, CA, USA) using ear bars and a vertebral clamp at T2 to immobilize the rat and stabilize the cervical spine for recordings. Core temperature was maintained at 35–37 °C using a temperature controller equipped with a rectal probe (Physitemp; Clifton, NJ, USA).
A custom-built monopolar platinum ball electrode (2.5 mm diameter) connected to a spring (1.5 mm diameter) was placed at the midline of the C3/C4 dorsal column and held in place by a micromanipulator (Fig. 1b).5,6 A return grounding electrode (copper wire with ~ 300 μm diameter) was attached to the skin at the caudal end of the incision using an alligator clip. Stimulation was run under constant current control. One of four SCS modes was applied: (1) biphasic 10 kHz HF [pulse width (PW) = 30 μs], (2) biphasic 1.2 kHz HF [PW = 200 µs], (3) biphasic burst with active recharge, or (4) biphasic burst with passive recharge (Fig. 1c; Table 1). The active recharge phase was generated by injecting current across the electrodes in a manner that was equal and opposite in amplitude to the main stimulation pulse, and is used to rapidly maintain net charge neutrality after delivery of each pulse. In contrast, the passive recharge phase was generated by allowing current to flow from a coupling capacitor to the electrodes in a decaying exponential fashion, such that net charge neutrality is maintained over the course of a burst, but not after individual pulses. Both burst paradigms used 5 pulses/burst, 500 Hz intra-burst frequency, PW = 1000 μs, and a 40 Hz inter-burst frequency (Fig. 1c). Almost all of the SCS modes were applied using an isolated pulse stimulator (A-M Systems Model 2100; Sequim, WA, USA). Burst SCS with passive recharge was applied using an externally applied implantable pulse generator (IPG) (Eon Mini™ Pulse Generator; Abbott, Plano, TX, USA). For each SCS mode, the motor threshold (MT) was identified by delivering that SCS mode in each rat, and finding the stimulation intensity at which small muscular contractions were observed in the paraspinal musculature or forelimbs, using the same parameters listed in Fig. 1c.5,6
Wide dynamic range (WDR) neurons were identified in the ipsilateral C7 dorsal horn based on their characteristic responses to non-noxious (brush) and noxious (pinch) stimuli to the ipsilateral forepaw.6 For each neuron, recordings were performed before and after each stimulation and the nerve root and spinal cord were kept hydrated during all recordings by repeated application of sterile saline. Once a WDR neuron was detected in the microelectrode recordings, the following recording protocol was initiated to obtain baseline neuronal activity before SCS application: (1) measurement of resting-state firing for at least 10 s, (2) measurement of evoked firing during five 1-s noxious stimulations using a 26 g von Frey filament applied to the ipsilateral forepaw (Stoelting; Wood Dale, IL, USA), and (3) measurement of evoked firing during a 10-s noxious pinch applied using a forceps to the ipsilateral forepaw.5,6 One of the four SCS modes was then randomly selected and applied for 5 min at 90% of MT, in alignment with prior studies.4,23,26,28 The recording protocol performed at baseline was then repeated at 0 (immediately after), 2, 5, 10, and 15 min after the end of the SCS period (Fig. 1b). Following that 15-min recording period, the recording procedures outlined above were repeated on the same neuron for the remaining SCS modes, with each neuron undergoing stimulation with all four SCS modes in a randomized order (Table 1). For each neuron, randomization was performed prior to any experimental procedure. After the four SCS modes were delivered, the tungsten microelectrode was moved in some animals to record from additional neurons in the C7 dorsal horn, and the entire recording process was performed again.
Extracellular voltage potentials were recorded from the ipsilateral C7 spinal dorsal horn using a glass-insulated tungsten microelectrode (FHC; Bowdoin, ME, USA) (Fig. 1b). The recording electrode (shank diameter of 125 μm; length of 70 mm) was secured onto a micromanipulator to hold it in place during the experiment. Signals were amplified with a gain of 103 and passband filtered between 0.3 and 3 kHz (World Precision Instruments; Sarasota, FL, USA). Signals were also processed with a 60 Hz noise eliminator (HumBug; Quest Scientific, North Vancouver, BC, Canada) and digitally sampled and stored at 25 kHz (Micro1401; CED, Cambridge, England).
Extracellular voltage potentials were spike-sorted using Spike2 (CED; Cambridge, UK) and firing rates were calculated. Evoked firing rates during noxious stimulation were determined by counting the number of spikes generated during application of the 26 g filament or the pinch, and subtracting the resting-state firing rate. In addition, spontaneous firing rates were determined during the 2-s period immediately prior to and after application of the stimuli (26 g von Frey filament or pinch) at baseline (prior to SCS application) and 5, 10, and 15 min after SCS. The evoked and spontaneous firing rates were normalized to baseline and compared between SCS types using ANOVA followed by post hoc Tukey’s test (JMP; Cary, NC, USA).
Results
All rats developed behavioral sensitivity, with the threshold for paw withdrawal decreasing from 16.3 ± 6 g before injury (at day 0) to 10.6 ± 9 g at day 7. Recordings for all SCS modes were made from 9 neurons. The average MT was highest for 10 kHz HF (516 ± 317 µA), which is significantly greater than the MT for 1.2 kHz HF (65 ± 28 µA) (p = 0.002), burst with active recharge (37 ± 21 µA) (p = 0.001), and burst with passive recharge (200 ± 61 µA) (p = 0.03) burst (Table 1). No other significant differences in MTs are identified between SCS modes.
Evoked neural firing rates measured during noxious stimulation were assessed before and after delivery of SCS for the different stimulation modes (Figs. 2 and 3). The normalized firing rate is not significantly different after SCS with any HF or burst stimulation mode in response to the 26 g filament noxious input (Figs. 2 and 4). However, with a noxious pinch input, the normalized firing rate does exhibit significant changes, depending on which SCS mode was applied (Figs. 3 and 4). At 5 min after delivering burst SCS with active recharge, the normalized firing rate increases compared to baseline (p = 0.006) and 0 min (p = 0.003) (Fig. 4). Further, the firing rate at 5 min after burst with active recharge is significantly higher than that for 1.2 kHz HF (p = 0.039) and burst with passive recharge (p = 0.037) at that same post-SCS time (Fig. 4). In contrast, burst SCS with passive recharge reduces the normalized firing rate in response to a pinch overall at 5, 10, and 15 min (p < 0.04) compared to baseline (Fig. 4), indicating that there is a persistent reduction, relative to baseline firing rates, in neuronal firing of responsive neurons.
Quantification of evoked neuronal firing rate measured during noxious stimulation at baseline (BL) and after delivery of 10 kHz HF, 1.2 kHz HF, burst with active recharge, or burst with passive recharge. All values were normalized to baseline. No significant differences in firing rate were detected for any SCS waveform in response to 26 g von Frey stimulation. Following burst SCS with passive recharge, the normalized firing rate in response to noxious pinch was significantly lower at 5, 10, and 15 min compared to baseline (*p < 0.04). Conversely, 5 min after burst SCS with active recharge, the normalized firing rate was increased relative to baseline (#p < 0.006) and 0 min (*p < 0.003). Firing was also elevated at 5 min after burst SCS with active recharge compared to 1.2 kHz HF (*p < 0.039) and burst SCS with passive recharge (#p < 0.037) at that same time point.
Normalized spontaneous firing rates are significantly altered after burst SCS with passive recharge, but not by any other SCS mode tested in this study (Fig. 5). Burst SCS with passive recharge significantly reduces spontaneous firing rates at 5 min (p < 0.0230) and 10 min (p < 0.0163) after SCS, as compared to baseline spontaneous activity (Fig. 5). Spontaneous firing rates are unchanged following 10 kHz, 1.2 kHz, and burst with active recharge (Fig. 5).
Quantification of spontaneous neuronal firing rates in the 2-s period before and after noxious stimulation for each SCS mode. All values were normalized to baseline. Spontaneous activity was unchanged for burst with active recharge, 10 kHz HF, and 1.2 kHz HF. However, following pinch, burst SCS with passive recharge significantly reduced spontaneous activity at 5 and 10 min compared to baseline activity (*p < 0.023).
Discussion
The results of this pilot study suggest that burst and HF SCS have different motor thresholds and effects on spinal neuronal firing rates in response to noxious pinch in rats with painful nerve root compression. Moreover, the frequency of HF SCS (10 kHz vs. 1.2 kHz) does affect the motor thresholds, but does not alter the firing rate in response to noxious stimuli in this pain model. Lastly, burst SCS with passive recharge reduces evoked and spontaneous firing rates during noxious pinch (Figs. 4 and 5), indicating a reduction in neuropathic pain transmission, whereas burst with active recharge has different effects.
Motor thresholds varied between SCS modes and from animal to animal. The average MT for 10 kHz HF SCS was significantly higher than that of the other SCS modes used in this study. In contrast, Shechter et al. reported no difference in MT between 50 Hz, 1 kHz, and 10 kHz SCS in the rat.24 This inconsistency could be attributed to differences in lead placement between the two studies, since stimulation was delivered to the C4 spinal level in the current study, whereas Schechter et al. used SCS at the thoracic spinal cord (T10–T12).24 Although differences in the MT could also be due to the different stimulators, both stimulators used in this study generate a current controlled stimulation waveform. Because the anatomy of the spinal cord varies between spinal levels, the stimulation intensity needed to obtain motor threshold could be influenced by the location of stimulation.
Burst SCS with passive recharge reduced neuronal firing rates after noxious pinch, whereas burst SCS with active recharge and HF SCS did not have the same effect. It is unclear why the burst waveform shape had an impact on neuronal firing rates, but the passive recharge phase appears to be important in reducing neuronal hyperexcitability. Moreover, the difference in effects observed between burst SCS with passive recharge and HF SCS suggests that these paradigms likely operate via different spinal mechanisms.
Spontaneous neuronal firing is associated with pain states, and burst SCS with passive recharge reduced spontaneous activity after pinch.7,22 Spontaneous neural activity is indicative of central sensitization,18 which has been demonstrated previously in this painful cervical radiculopathy model.27 Indeed, many of the clinical hallmarks of central sensitization are developed in this model within 1 day of injury and maintained at day 7, the timepoint probed for SCS here, as well as being sustained at later times.2,6,14,23 A previous clinical study found that a higher degree of central sensitization in chronic pain patients was associated with greater analgesic effects from low-frequency, tonic SCS therapy.1
While the findings in the current study suggest that burst with passive recharge is most effective in reducing spontaneous activity, and possibly central sensitization, additional investigations of other measures of central sensitization in the context of specific SCS modes (i.e., burst, tonic, HF) would be informative in better understanding such effects. Further, the reduction in spontaneous firing rates was only observed at 5 and 10 min after passive recharge burst application (Fig. 5); spontaneous activity returned at 15 min, suggesting that such an effect may be only temporary. Nevertheless, it should be noted that all statistical comparisons used baseline values, so they do take into account any variability of neurons, rats and order.
Although this pilot study does provide important information about the effects of different SCS modes on spinal neuronal firing rates, the findings must be taken in light of several limitations. First, with only five rats and nine neurons, the statistical power of the study is limited. However, this study is adequately powered to show statistically significant changes to the neuronal firing rates with different SCS modes (Figs. 4 and 5) and similar, previously-published work has used comparable sample sizes.8,28 Of note, the only significant findings were with pinch stimuli which power analyses predicted to require smaller sample sizes; the sample sizes needed to detect differences in von Frey stimuli were in the range of 15–27 neurons. Nevertheless, since the trends in the data suggest such differences exist (Figs. 4 and 5) and there is large variability among individuals clinically, the findings from this study support differences in these SCS modes and their utility. Since two different stimulators were used to deliver the different SCS modes (Eon Mini and A-M Systems Model 2100), it is possible that using different stimulators could introduce a confounding factor. Of note, each neuron did undergo every SCS mode, adding to the power of the study. The randomization of SCS mode order also minimized any bias due to order of application and helped ensure validity with using the different stimulators since each neuron underwent every SCS mode. This work used a monopolar ball electrode, which has been used in several other preclinical studies,8,23,26,31 but may create electrical fields that are different from bipolar or multipolar configurations that are commonly used with clinical electrode arrays. Further, given that there is still rather limited information about SCS mechanisms, these data, although limited, do provide foundational information and since preclinical models in the rat have been shown to relate to those observed clinically,11,12 they help identify areas for future investigation. Since it is possible that the electrode shape and configuration may affect the response of the spinal cord neurons to SCS, additional studies are needed to compare the effects of burst and HF SCS modes with the multielectrode arrangements used clinically.
Despite the power of testing each mode on every neuron, there is the potential for carry-over effects (including long-lasting plasticity changes) and order effects from stimulating each animal with multiple SCS modes in a sequential manner. However, this same study design has been used elsewhere,6,24,28 and these effects were controlled for through the use of a 15-min washout period and random order of delivery for each SCS mode. It is also possible that HF stimulation was not delivered for a sufficient duration to generate effects in the dorsal horn. While the same 5-min stimulation protocol was used in previous studies of low-frequency tonic and burst stimulation,6 other studies testing HF SCS modes have used a minimum stimulation time of 15 min.24,26 Changes in neuronal firing during the stimulation period were not measured due to stimulus artifacts in the electrophysiological signal during SCS. As such, some effects generated by SCS may not have been detected. A previous study demonstrated peak pain reduction during HF SCS,24 suggesting that the electrophysiological effects of HF SCS likely are also evident, and possibly even more pronouced, during SCS rather than after SCS.
Nevertheless, studies comparing different SCS modes, including burst and HF stimulation, are very few, highlighting the need for investigations into the effects of these stimulation paradigms. In the clinical setting, Kinfe et al. reported significant reductions in lower leg VAS scores for patients with predominant back pain using BurstDR SCS, but not with delivery of 10 kHz HF SCS, and observed a greater responder rate for the former compared to the latter.16 The results of the current study, which suggest that burst SCS and HF SCS have different electrophysiological effects on spinal neuronal activity, may in part explain that clinical finding. Regardless, to our knowledge this is the first study that directly compares burst SCS with passive or active recharge, and the findings point towards the importance of the passive recharge phase in reducing spinal hyperactivity and central sensitization.
References
Campbell, C. M., L. F. Buenaver, S. N. Raja, et al. Dynamic pain phenotypes are associated with spinal cord stimulation-induced reduction in pain: a repeated measures observational Pilot study. Pain Med. 16(7):1349–1360, 2015. https://doi.org/10.1111/pme.12732.
Chang, Y.-W., and B. A. Winkelstein. Schwann cell proliferation and macrophage infiltration are evident at day 14 after painful cervical nerve root compression in the rat. J. Neurotrauma 28(12):2429–2438, 2011. https://doi.org/10.1089/neu.2011.1918.
Compton, A. K., B. Shah, and S. M. Hayek. Spinal cord stimulation: a review. Curr. Pain Headache Rep. 16(1):35–42, 2012. https://doi.org/10.1007/s11916-011-0238-7.
Courtney, P., A. Espinet, B. Mitchell, et al. Improved pain relief with burst spinal cord stimulation for two weeks in patients using tonic stimulation: results from a small clinical study. Neuromodulation 18(5):361–366, 2015. https://doi.org/10.1111/ner.12294.
Crosby, N. D., M. D. Goodman Keiser, J. R. Smith, M. E. Zeeman, and B. A. Winkelstein. Stimulation parameters define the effectiveness of burst spinal cord stimulation in a rat model of neuropathic pain. Neuromodulation 18:1–8, 2015. https://doi.org/10.1111/ner.12221.
Crosby, N. D., C. L. Weisshaar, J. R. Smith, M. E. Zeeman, M. D. Goodman-Keiser, and B. A. Winkelstein. Burst and tonic spinal cord stimulation differentially activate GABAergic mechanisms to attenuate pain in a rat model of cervical radiculopathy. IEEE Trans. Biomed. Eng. 62(6):1604–1613, 2015. https://doi.org/10.1109/TBME.2015.2399374.
Crosby, N. D., C. L. Weisshaar, and B. A. Winkelstein. Spinal neuronal plasticity is evident within 1 day after a painful cervical facet joint injury. Neurosci. Lett. 542:102–106, 2013. https://doi.org/10.1016/j.neulet.2013.03.019.
Cuellar, J. M., K. Alataris, A. Walker, D. C. Yeomans, and J. F. Antognini. Effect of high-frequency alternating current on spinal afferent nociceptive transmission. Neuromodulation 16(4):318–327, 2013. https://doi.org/10.1111/ner.12015.
De Ridder, D., S. Vanneste, M. Plazier, E. van der Loo, and T. Menovsky. Burst spinal cord stimulation: toward paresthesia-free pain suppression. Neurosurgery 66(5):986–990, 2010. https://doi.org/10.1227/01.NEU.0000368153.44883.B3.
de Vos, C. C., M. J. Bom, S. Vanneste, M. W. P. M. Lenders, and D. de Ridder. Burst spinal cord stimulation evaluated in patients with failed back surgery syndrome and painful diabetic neuropathy. Neuromodulation 17(2):152–159, 2014. https://doi.org/10.1111/ner.12116.
Deer, T., K. V. Slavin, K. Amirdelfan, et al. Success using neuromodulation with BURST (SUNBURST) study: results from a prospective, randomized controlled trial using a novel burst waveform. Neuromodulation 21(1):56–66, 2018. https://doi.org/10.1111/ner.12698.
Demartini, L., G. Terranova, M. A. Innamorato, et al. Comparison of tonic vs. burst spinal cord stimulation during trial period. Neuromodulation 22(3):327–332, 2019. https://doi.org/10.1111/ner.12867.
Hubbard, R. D., Z. Chen, and B. A. Winkelstein. Transient cervical nerve root compression modulates pain: load thresholds for allodynia and sustained changes in spinal neuropeptide expression. J. Biomech. 41:677–685, 2008. https://doi.org/10.1016/j.jbiomech.2007.09.026.
Hubbard, R. D., and B. A. Winkelstein. Transient cervical nerve root compression in the rat induces bilateral forepaw allodynia and spinal glial activation: mechanical factors in painful neck injuries. Spine 30(17):1924–1932, 2005. https://doi.org/10.1097/01.brs.0000176239.72928.00.
Kapural, L., C. Yu, M. W. Doust, et al. Novel 10-kHz High-frequency therapy (HF10 Therapy) is superior to traditional low-frequency spinal cord stimulation for the treatment of chronic back and leg pain: the SENZA-RCT randomized controlled trial. Anesthesiology 123(4):851–860, 2015. https://doi.org/10.1097/ALN.0000000000000774.
Kinfe, T. M., S. Muhammad, C. Link, S. Roeske, S. R. Chaudhry, and T. L. Yearwood. Burst spinal cord stimulation increases peripheral antineuroinflammatory interleukin 10 levels in failed back surgery syndrome patients with predominant back pain. Neuromodulation 20(4):322–330, 2017. https://doi.org/10.1111/ner.12586.
Kinfe, T. M., B. Pintea, C. Link, et al. High frequency (10 kHz) or Burst spinal cord stimulation in failed back surgery syndrome patients with predominant back pain: preliminary data from a prospective observational study. Neuromodulation 19(3):268–275, 2016. https://doi.org/10.1111/ner.12379.
Latremoliere, A., and C. J. Woolf. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J. Pain 10(9):895–926, 2009. https://doi.org/10.1016/j.jpain.2009.06.012.
Lempka, S. F., C. C. McIntyre, and K. L. Kilgore. Computational analysis of kilohertz frequency spinal cord stimulation for chronic pain management. Anesthesiology 122(6):1362–1376, 2015. https://doi.org/10.1097/ALN.0000000000000649.
Linderoth, B., and R. D. Foreman. Physiology of spinal cord stimulation: review and update. Neuromodulation 2(3):150–164, 1999. https://doi.org/10.1046/j.1525-1403.1999.00150.x.
North, J. M., K.-S. J. Hong, and P. Y. Cho. Clinical outcomes of 1 kHz subperception spinal cord stimulation in implanted patients with failed paresthesia-based stimulation: results of a prospective randomized controlled trial. Neuromodulation 19(7):731–737, 2016. https://doi.org/10.1111/ner.12441.
Quinn, K. P., L. Dong, F. J. Golder, and B. A. Winkelstein. Neuronal hyperexcitability in the dorsal horn after painful facet joint injury. Pain 151(2):414–421, 2010. https://doi.org/10.1016/j.pain.2010.07.034.
Rothman, S. M., K. J. Nicholson, and B. A. Winkelstein. Time-dependent mechanics and measures of glial activation and behavioral sensitivity in a rodent model of radiculopathy. J. Neurotrauma 27(5):803–814, 2010. https://doi.org/10.1089/neu.2009.1045.
Shechter, R., F. Yang, Q. Xu, et al. Conventional and kilohertz-frequency spinal cord stimulation produces intensity- and frequency-dependent inhibition of mechanical hypersensitivity in a rat model of neuropathic pain. Anesthesiology 119(2):422–432, 2013. https://doi.org/10.1097/ALN.0b013e31829bd9e2.
Smith, J. R., P. A. Galie, D. R. Slochower, C. L. Weisshaar, P. A. Janmey, and B. A. Winkelstein. Salmon-derived thrombin inhibits development of chronic pain through an endothelial barrier protective mechanism dependent on APC. Biomaterials 80:96–105, 2016. https://doi.org/10.1016/j.biomaterials.2015.11.062.
Song, Z., B. A. Meyerson, and B. Linderoth. High-frequency (1 kHz) spinal cord stimulation—Is pulse shape crucial for the efficacy? A pilot study. Neuromodulation. 18(8):714–720, 2015. https://doi.org/10.1111/ner.12344.
Syré, P. P., C. L. Weisshaar, and B. A. Winkelstein. Sustained neuronal hyperexcitability is evident in the thalamus after a transient cervical radicular injury. Spine. 39(15):E870–E877, 2014. https://doi.org/10.1097/brs.0000000000000392.
Tang, R., M. Martinez, M. Goodman-Keiser, J. P. Farber, C. Qin, and R. D. Foreman. Comparison of burst and tonic spinal cord stimulation on spinal neural processing in an animal model. Neuromodulation 17(2):143–151, 2014. https://doi.org/10.1111/ner.12117.
Thomson, S. J., M. Tavakkolizadeh, and S. Love-Jones. Effects of rate on analgesia in kilohertz frequency spinal cord stimulation: results of PROCO randomized controlled trial. Neuromodulation 21(1):67–76, 2018. https://doi.org/10.1111/ner.12746.
Weisshaar, C. L., J. P. Winer, B. B. Guarino, P. A. Janmey, and B. A. Winkelstein. The potential for salmon fibrin and thrombin to mitigate pain subsequent to cervical nerve root injury. Biomaterials 32(36):9738–9746, 2011. https://doi.org/10.1016/j.biomaterials.2011.09.021.
Yakhnitsa, V., B. Linderoth, and B. A. Meyerson. Spinal cord stimulation attenuates dorsal horn neuronal hyperexcitability in a rat model of mononeuropathy. Pain 79(2–3):223–233, 1999.
Zimmermann, M. Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16(2):109–110, 1983. https://doi.org/10.1016/0304-3959(83)90201-4.
Acknowledgments
This work was supported by a sponsored research contract from St. Jude Medical/Abbott. We would like to thank Martha Zeeman for her technical support with data analysis. Drs. Kent and Venkatesan were employees of Abbott; although they both contributed to the study design and provided editorial input and review of the manuscript, they were not involved in performing the study or analyzing the data. Dr. Winkelstein has received research funding from St. Jude Medical/Abbott.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Xiaoxiang Zheng oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kent, A.R., Weisshaar, C.L., Venkatesan, L. et al. Burst & High-Frequency Spinal Cord Stimulation Differentially Effect Spinal Neuronal Activity After Radiculopathy. Ann Biomed Eng 48, 112–120 (2020). https://doi.org/10.1007/s10439-019-02336-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-019-02336-8