Abstract
Numerous injury criteria have been developed to predict brain injury using the kinematic response of the head during impact. Each criterion utilizes a metric that is some mathematical combination of the velocity and/or acceleration components of translational and/or rotational head motion. Early metrics were based on linear acceleration of the head, but recent injury criteria have shifted towards rotational-based metrics. Currently, there is no universally accepted metric that is suitable for a diverse range of head impacts. In this study, we assessed the capability of fifteen existing kinematic-based metrics for predicting strain-based brain response using four different automotive impact conditions. Tissue-level strains were obtained through finite element model simulation of 660 head impacts including occupant and pedestrian crash tests, and pendulum head impacts. Correlations between head kinematic metrics and predicted brain strain-based metrics were evaluated. Correlations between brain strain and metrics based on angular velocity were highest among those evaluated, while metrics based on linear acceleration were least correlative. BrIC and RVCI were the kinematic metrics with the highest overall correlation; however, each metric had limitations in certain impact conditions. The results of this study suggest that rotational head kinematics are the most important parameters for brain injury criteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Closed-head impacts account for the highest percentage of traumatic brain injuries (TBI) diagnosed annually among the United States (US) civilian population.4,47 According to the Centers for Disease Control and Prevention, falls are the most common cause of these impacts, resulting in the largest percentage of non-fatal TBIs (35%), while motor-vehicle collisions have the largest contribution to TBI-related deaths (32%).4 Additionally, an estimated 3.8 million concussions occur every year in the US due to sporting activities, and it is believed that around half of these cases go unreported.17 Brain injuries due to closed-head impacts cover a broad range of mild-to-severe types including concussions and diffuse axonal injuries (DAI), which are believed to be a result of tissue-level deformation caused by inertial loading of the brain.12,19,40 Although these impacts are typically less severe than most forms of penetrating head injuries, they still require significant attention due to the sometimes insidious nature of the resulting pathologies.4
Brain injury risk assessments have typically focused on the resulting kinematics of the head during an impact event. Traditionally, brain injury risk has been achieved through an evaluation of the linear acceleration of the head. For example, the National Operating Committee on Standards for Athletic Equipment (NOCSAE) uses a maximum resultant linear acceleration criterion to evaluate helmet design,33 while the National Highway Traffic Safety Administration (NHTSA) uses a metric based on the time history of linear head acceleration, the Head Injury Criterion (HIC), as the only federally-mandated head injury metric in automobile safety regulation.7 Despite widespread use of translational-based metrics to predict head injury, some question whether they are suitable for assessing most types of brain injury.9,13,29,38,49 In 1943, Holbourn proposed one of the most comprehensive theories for a brain injury mechanism, using the fundamental laws of motion to describe the interaction between the skull and brain during a head impact.19 Combined with the near incompressible nature of brain tissue, Holbourn’s theory makes rotational kinematics seem well suited for studying closed-head brain injuries.
Numerous studies have focused on the development of rotational-based brain injury tolerances.9,14,24–26,29,34,35,39,41,44,45,49,51 Several studies developed thresholds for mild-to-severe brain injury using available human volunteer and animal data. Tolerances for DAI in man, based on angular velocity and acceleration, were proposed using scaled impact kinematics from primate experiments, while concussion risk assessment functions based on rotational kinematics were developed using head impact data from American football athletes.29,39,44,45,56 Some of the earliest efforts to include rotational kinematics in the formulation of brain injury criteria resulted in combined rotational and translational metrics.34,35 These metrics included both angular and linear acceleration components and were typically used to assess different forms of mild-to-moderate brain injuries including concussion. As efficacy of finite element (FE) models of the head improved, research efforts began to focus on deriving kinematic formulations based on correlations between head impact kinematics and tissue-level predictors of brain injury obtained through FE simulation.26,30,49,51,55,56 Many of these metrics were based exclusively on rotational kinematics due to poor correlation between translation kinematics and FE model strains.9,26,49,52
FE models of the human head are perhaps the most suitable tools for studying the complex, tissue-level mechanical response of the brain during a head impact. Several studies have focused on developing brain injury criteria by correlating injury data with tissue-level strains obtained from FE simulation of the associated head impacts.26,30,49–52 Two strain-based brain injury metrics have been used in previous computational research studies to categorize brain injury: maximum principle strain (MPS) and cumulative strain damage measure (CSDM).49 The link between FE strain metrics and brain injury was used as the foundation for the development of several rotational-based brain injury metrics including the Brain Injury Criterion (BrIC).49
Given the various brain injury metrics that have been proposed, it is not always clear which metric should be used to assess head impact severity for a particular loading condition. In this study, we assessed the capability of existing kinematic-based brain injury metrics to predict tissue-level strain responses obtained from FE model simulation using a diverse database of head impacts. A total of fifteen separate kinematic metrics, including fundamental parameters and common injury criteria developed previously, were used in the assessment. Over 600 head impacts from crash test databases and previously published studies were collected, and simulated using two separate FE models of the human head. Assessments were made by comparing correlations between kinematic metrics, which were calculated directly from the head impact data, and strain-based metrics, which were obtained through the FE model simulations. These results identify best performing kinematic-correlates for the prediction of brain tissue strains, and highlight instances where certain injury criteria may not be suitable.
Materials and Methods
Head Impact Data
Six degree-of-freedom (6DOF) head kinematic data from a total of 660 head impacts were collected and used in this study. These include sled tests from the University of Virginia (UVa),5,6,8,22,23,48 crash and pendulum tests from NHTSA,36,49 and crash tests from the Insurance Institute for Highway Safety (IIHS).20 The crash and sled test data consists of a variety of impact conditions including frontal, oblique, side, and pedestrian impacts using cadavers and different dummies. The pendulum tests were obtained from a previous study in which several different dummy head forms were impacted at various angles and energies using a pneumatically driven impactor.49 All data was acquired through either public access to crash test databases or peer-reviewed research papers available in the literature. A summary of the impact conditions is shown in Table 1, and a detailed list of the crash tests used in this study is provided in the Electronic Supplementary Material.
All head kinematic data were processed and prepared for calculation of kinematic and strain-based injury metrics. Linear accelerations were filtered to channel frequency class (CFC) 1000 (1650 Hz), angular velocities were filtered to CFC 60 (100 Hz), and angular accelerations were obtained by differentiating the filtered angular velocity data using the central difference method (no additional filtering was needed for the angular acceleration data). A zero-phase shift, digital 8 pole IIR Butterworth filter at the low pass frequencies specified above was used to filter the data. Processed kinematics were measured with respect to a local coordinate system defined by the anatomical axes of the head with an origin fixed at the head center-of-gravity (CG).46
Kinematic-Based Injury Metrics
Fifteen kinematic-based head and brain injury metrics were evaluated in this study. These metrics were selected based their inclusion of a variety of translational and rotational head kinematic parameters consisting of linear and angular velocities and accelerations. Many metrics were formulated using experimental data while others were developed from classical mechanics theories or computational models. In addition, several of these metrics have been incorporated into head or brain injury risk functions using experimental injury data. A brief description of each metric is provided below and summarized in Table 2. Kinematic parameters \(\varvec{a}(t)\), \(\varvec{\alpha}(t)\), and \(\varvec{\omega}(t)\) are the linear acceleration, angular acceleration, and angular velocity time history vectors of the head, respectively. Subscripts in the equations below indicate directional components (x, y, z) and critical values (cr), which are metric parameters, and are included in Table 2.
Maximum Resultant Acceleration and Velocity
The most fundamental kinematic parameters used in head and brain injury risk assessments and helmet safety evaluation are the maximum values of the resultant head angular velocity, and linear and angular acceleration time histories. They are defined as follows:
where \(\varvec{z}\) is equal to \(\varvec{a}\), \(\varvec{\alpha}\), or \(\varvec{\omega}\), and z m is the maximum value of the resultant kinematic variable taken over the entire time history of the event. Distributions and descriptive statistics for the maximum resultant kinematic variables are shown in Fig. 1 and Table 3, respectively.
Gadd Severity Index (GSI)
In 1966, Gadd proposed the severity index as a means of incorporating impact duration into the assessment of head and brain injury potential.10 The GSI was formulated by fitting the Wayne State Tolerance Curve, which is based on skull fracture data.43
where the acceleration units are (g). According to available standards, the integral is evaluated from when \(\left| {\varvec{a}(t)} \right|\) first rises above 4 g to when it falls below 4 g following the maximum value.33
Head Injury Criterion (HIC)
In 1971, Versace adapted the GSI to include a time-averaging component, which became known as HIC.54 HIC is the most commonly used metric for evaluating head and brain injury risk, and is currently the only federally-mandated head injury assessment used in motor vehicle regulation.7
where, the units of acceleration are (g) and t 1, t 2 are selected from the time domain in (s) such that the value of HIC is maximized. Based on current standards, t 2 – t 1 ≤ 15 ms.7
Generalized Acceleration Model for Brain Injury Threshold (GAMBIT)
One of the earliest efforts to combine translational and rotational kinematics for brain injury risk assessment was proposed by Newman in 1986.34 GAMBIT is based on a kinematic analogue to maximum shear stress/strain theory, where the relationship between linear and angular head acceleration was assumed analogous to that of the normal and shear components of maximum in-plane shear, respectively.
where the exponents n, m, and s are empirically determined constants set to two for the current study; in accordance with the original formulation of the criterion.34
Head Impact Power (HIP)
In 2000, Newman et al. proposed another combined kinematic brain injury metric, HIP, with the hypothesis that head injury severity correlates with head impact power.35 The formulation for HIP is based on the rate of change of kinetic energy entering a rigid body with mass and inertia properties based on a 50th percentile adult, human male:
where I ii are the principal moments of inertia of the head, with mass m, about the anatomical axes (i = x, y, z).35
Kleiven’s Linear Combination (KLC)
In 2007, Kleiven et al. found that a linear combination of HIC and \(\omega_{m}\) correlated well with brain tissue MPS obtained from FE simulation of head impacts sustained by American football players.26
where \(\beta_{i}\) are the regression coefficients, and the subscript on HIC represents the constraint that t 2 – t 1 ≤ 36 ms.
Principal Component Score (PCS)
Another empirically derived model used for predicting concussion in football athletes was developed by Greenwald et al., 2008 using principal component analysis.14 This metric is a linear combination of several of the kinematic metrics mentioned above:
where \(\bar{X} = \left( {X - \mu } \right)/\sigma\) is the standardized value for each kinematic metric. Values for μ and σ were based on the 660 head impacts used in this study.
Combined Probability of Concussion (CP)
CP was developed by Rowson et al., to predict the risk of concussion experienced by football athletes following helmeted head impact.44 The actual kinematic metric is the basis of a logistic function taken from an injury risk curve that relates maximum resultant linear and angular head acceleration to concussion risk,
where β i were obtained from multivariate logistic regression analysis.
Power Rotational Head Injury Criterion (PRHIC)
Beginning in 2011, Kimpara et al., began modifying HIC with rotational kinematic parameters.25 The first of two proposed rotational-based brain injury criteria from this group, PRHIC was developed by replacing the linear acceleration term of HIC with the rotational component of HIP.
where
Rotational Injury Criterion (RIC)
The second rotational-based brain injury criterion proposed by Kimpara et al., was RIC.24 RIC is formulated in a similar manner to PRHIC by replacing the linear acceleration term in HIC with angular acceleration in (rad s−2).
where a constraint of \(t_{2} - t_{1}\) ≤ 36 ms was proposed for both PRHIC and RIC.
Kinematic Rotational Brain Injury Criterion (BRIC)
BRIC was proposed by Takhounts et al., to assess brain injury risk due to DAI in occupant crash tests that otherwise may not have been detected by HIC.51 A preliminary form of the criterion was proposed in 2011 and included both angular velocity and angular acceleration.51
Brain Injury Criterion (BrIC)
In 2013, Takhounts et al., proposed an update to the original BRIC formulation after finding that angular velocity alone was sufficient to predict FE model strains in pendulum and occupant crash tests.49 The updated criterion, BrIC, is formulated using the maximum magnitudes of the three orthogonal head angular velocity components:
where ω icr are directionally dependent critical values that were determined using FE modeling.49
Rotational Velocity Change Index (RVCI)
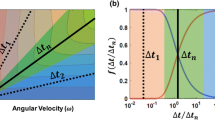
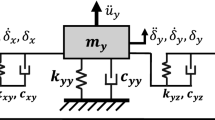
In 2015, Yanaoka et al. proposed RVCI to improve correlations between head kinematics and FE model strains for pedestrian impact events.55 RVCI was formulated by assuming that brain tissue strain was analogous to deformation from a simple spring mass model:
where R i are weighting factors about each orthogonal axis determined using a FE model of the head. A duration constraint of t 2 – t 1 ≤ 10 ms was used since it resulted in the highest correlation between RVCI and FE strains for both occupant and pedestrian crash simulations.55
Strain-Based Injury Metrics
Two previously developed strain-based injury metrics were used in this study (MPS and CSDM). These metrics are calculated using FE models of the head and have been used as tissue-level predictors of diffuse brain injury in many previous computational studies.3,9,26,30,42,49,51,52,55 Two FE models of the human head were used to calculate MPS and CSDM: the Simulated Injury Monitor (SIMon, v4.0), a 50th percentile human male head model developed and publically distributed by NHTSA, and the Global Human Body Models Consortium-owned (GHBMC) 50th percentile male (M50) detailed seated occupant (v4.3) head model. Both models have been used extensively in computational biomechanics research to study intracranial responses due to head impact. These models were previously validated for relative brain-skull motion using experimental data obtained from head impacts performed on cadavers. Details on the development and validation of both models are provided in the literature.28,52
MPS and CSDM were calculated for each of the 660 experimental head impacts by applying 6DOF kinematics directly to the rigid skull of both FE head models. Simulations with the head models were performed without a body similar to other computational TBI research studies.2,3,9,18,21,26,28,30,49–52,55,56 Kinematics were applied to both FE models in their respective local head coordinate systems, which were based on an anatomical configuration that was consistent with the coordinate system used to derive the experimental data.28,46,49 MPS is the maximum value of maximum principal strain occurring over all elements in the brain model.52 In this study, MPS was based on the 95th percentile peak response (by element) to avoid potential numerical issues associated with using the 100th percentile value.42 CSDM is the cumulative volume fraction of elements with MPS exceeding a predefined strain threshold.2,52 In this study, a maximum principal strain threshold of 0.25 was used for CSDM, which was found to be the best predictor of diffuse brain injury when evaluated relative to other threshold values.49 Both brain strain metrics were taken as the maximum value over the entire time history of the impact event. FE simulations were performed using LS-DYNA (v971 R7.1.1, double precision; LSTC, Livermore, CA).
Statistical Methods
Simple linear regression using ordinary least squares was used to assess the capability of each kinematic-based metric to predict MPS and CSDM. An overall assessment was made using the 660 head impacts and simulation results from both SIMon and GHBMC. In an additional assessment using only GHBMC, head impacts were categorized into four separate impact conditions: frontal, oblique, side, and pedestrian. Pendulum tests were included with the crash data for this analysis, and organized into the separate impact conditions based on the impact angle relative to the dummy head, where 0° impacts were considered frontal, 30° and 60° considered oblique, and 90° considered side impacts. Correlations between kinematic-metric and strain-metric were based on the coefficient of determination (R 2). Test for significance was evaluated at the 5% level (α = 0.05).
Results
Overall Assessment
The assessment using all 660 head impacts and GHBMC revealed better correlation between rotational-based kinematic metrics and FE strains when compared to translational-based metrics (Fig. 2a). BrIC was the overall best correlate with MPS (R 2 = 0.778; Fig. 3a), while RVCI correlated slightly better with CSDM (R 2 = 0.797; Fig. 3b). Of the combined rotation-translation metrics, which generally correlated better when compared to translation-only metrics, KLC had the highest correlation (R 2 = 0.402–0.443; Fig. 2a) and GAMBIT had the lowest correlation (R 2 = 0.032–0.041; Fig. 2a). Kinematic metrics including maximum angular velocity and angular acceleration had similar correlation with both MPS and CSDM (R 2 = 0.549–0.595; Fig. 2a), while maximum linear acceleration had the lowest overall correlation (R 2 = 0.017, Fig. 3c). The correlation between HIC and FE strains was also very low (R 2 = 0.146, Fig. 3d).
Trends between SIMon and GHBMC were similar; however correlations between kinematic metrics and FE strains were slightly higher in SIMon (Fig. 2b). Table 4 shows the relative ranking of kinematic-based metrics with respect to R 2 values from correlations with MPS and CSDM. Results from the regression analysis using GHBMC are provided in Table 5. All coefficients were statistically significant unless otherwise indicated (Table 5).
Assessment by Impact Condition
When separated by impact condition, trends were similar to those observed in the overall assessment. In frontal impacts, BrIC had the highest correlation with FE strains (R 2 = 0.730, 0.705) for MPS and CSDM, respectively (Fig. 4a). In oblique impacts, BrIC had the highest correlation with MPS (R 2 = 0.793), while RVCI was highest with CSDM (R 2 = 0.840; Fig. 4b). In side impacts, again, BrIC had the highest correlation with MPS (R 2 = 0.652), and RVCI was highest with CSDM (R 2 = 0.739; Fig. 4c). Finally, for pedestrian impacts, RVCI correlated best with both MPS and CSDM (R 2 = 0.730, 0.705), respectively, followed by RIC (Fig. 4d).
Discussion
Many risk assessment models have been developed to predict brain injury using the kinematic response of the head. An effective injury criterion can have a substantial impact on how we predict, diagnosis, and prevent brain injury, from assessing the severity of a head impact in football with output from wearable sensors, to evaluating the efficacy of automobile restraint systems for preventing head injury during a crash. The kinematic metric that establishes the severity of a head impact is some mathematical combination of the velocity and/or acceleration components of translational and/or rotational head motion. In this study, 15 kinematic-based metrics were compared to FE model-predicted brain strain results from simulations using a broad range of head impacts taken from different automotive crash modes. The relative performance of each kinematic metric was evaluated based on correlations with two strain-based predictors of brain injury, MPS and CSDM.
Efficacy of strain-based FE metrics (MPS and CSDM) for predicting diffuse brain injuries including concussion and DAI, is a vital assumption of this research. Several experimental studies have identified that strain-based measures are good predictors of diffuse brain injury and functional impairment using different animal models.1,31,53 Although experimentally measured brain-tissue strains are preferred to establish a direct link between mechanical-metric and physical injury response, they are difficult to obtain due to complexity of the organ and challenges associated with testing. Other studies have leveraged FE brain models to measure various mechanical variables including strain, strain rate, stress, and pressure for correlations with brain injury data from either simulated injurious impacts using animals or field studies involving humans.3,26,30,49,52,56 In particular, Takhounts et al., and Kleiven found that metrics based on strain predicted diffuse brain injuries better when compared to other mechanically-based metrics including pressure.26,52 Although animal data offer potentially useful information, the assumptions associated with scaling (kinematic and geometric) and relating equivalency of brain deformation and injury tolerances to humans are problematic.37,49 Further, existing field impact databases are dominated by non-injury data, under-reporting of concussion injuries, and rely on kinematics data from sensor systems that are not rigidly coupled to the head.44 While tissue strain appears to be the correct mechanical variable for prediction of diffuse brain injury, future work should be done to evaluate correlations between existing strain-based risk assessment models and injury data.
Only diffuse brain injury types were considered in this study. Focal injuries such as contusion or subdural hematoma, which typically result from high acceleration, short duration impacts that potentially involve skull fracture, may be due to different injury mechanisms including highly localized pressure gradients within the head.9 In the current study, the skull was modeled as a rigid structure, and correlations between kinematic and FE-based pressure metrics were not evaluated. Furthermore, only global measures of MPS and CSDM were used in this study. Although regional-based metrics have been investigated, more work is needed to clarify whether region specific criteria improves correlations with different types of brain injury.18,26
When predicting FE model brain strain, rotational-based kinematic metrics performed better than translational-based metrics. This result was not surprising given the amount of theoretical, experimental, and computational work available in the literature to support this finding. Holbourn theorized that the incompressible nature of brain tissue makes it susceptible to shear deformations during rotational motion of the head, and negligible deformations during translational motion.19 Experimentally, several studies have observed that rotational head motion is potentially more useful in predicting brain injuries than translation motion.11,13,38,40 Ommaya et al. observed no symptoms of cerebral concussion in specimens subjected to pure linear acceleration, while the opposite was true when only pure rotations were applied.38 Computational FE models of the head and brain have also demonstrated low correlation between translational kinematic parameters and FE strains.9,26,49,52 Through development of BrIC, Takhounts et al. reported low correlation between translational kinematic metrics (maximum resultant linear acceleration and HIC) and brain deformation metrics (MPS and CSDM).49 Gabler et al. demonstrated that excessively high magnitudes of pure linear head accelerations were required to generate the same MPS and CSDM as relatively low magnitudes of pure angular head acceleration.9
In this study, MPS was defined as the 95th percentile (by element) maximum principal strain of all the elements in the brain rather than the 100th percentile maximum principal strain as in previous studies.9,26,49,52 This was done to alleviate simulation results of the entire brain from being driven by the response of a single element.42 The overall correlation between most of the fifteen kinematic-based metrics and 95th percentile MPS was higher in both FE models than with the 100th percentile MPS (R 2 values increased by approximately 0.1); however trends in the relative performance of kinematic metrics were not affected using the 100th percentile MPS. Furthermore, the 95th percentile MPS correlated better with CSDM (R 2 = 0.939 vs. 0.806 for the 100th percentile MPS). Based on these results, future research on the development of kinematic brain injury criteria should be made with 95th percentile peak MPS responses.
We observed that metrics based on angular velocity had the best correlation with MPS and CSDM. Across each impact condition either BrIC or RVCI was the top performing metric. This result was not surprising given that both of these metrics were developed from FE model responses. A majority of the head impacts used in the current study were also used by Takhounts et al. to develop BrIC, while RVCI was developed using correlations with MPS and CSDM based on head impacts acquired from frontal and pedestrian whole-body, dummy crash test simulations.49,55
However, both BrIC and RVCI have their limitations: For pedestrian impact events, which had head angular velocities longer in duration than the other three crash modes, BrIC was not well correlated (R 2 ~ 0.5) with MPS and CSDM. A previous parametric study using SIMon demonstrated that for a given magnitude of angular head velocity, brain strain decreased as the duration of the velocity pulse increased beyond 50 ms.9 Thus, the critical angular velocity values of BrIC are too low for impacts exceeding 50 ms in duration, and BrIC would over estimate the amount of brain deformation in these cases. One way to improve correlations between BrIC and FE strains in longer duration events, would be to include angular acceleration in the formulation. This was accomplished by Takhounts et al., in an earlier version of the criterion (BRIC); however, Takhounts et al., found low correlation between angular acceleration and FE strains, and thus excluded it from the mathematical form.49,51 In the current study, correlations between angular acceleration and strain-based metrics were good overall, and higher than correlations for angular velocity in side and pedestrian impact conditions. This may be due to inclusion of longer duration impact events in these two conditions (pedestrian and far-side), which were not investigated by Takhounts et al. In this study, angular acceleration was obtained by differentiating filtered angular velocity data, since protocols for processing angular acceleration data from various surrogates and impact conditions have not been established. Furthermore, instructions for processing kinematic data were not clearly described by Takhounts et al. 49
RVCI was better correlated to MPS and CSDM for pedestrian impacts than BrIC, and the integration limits selected for RVCI appear to be well tuned to the longer duration event. However, for shorter duration head impacts, mainly those generated from pendulum impact, RVCI did not correlate as well as BrIC (and thus, BrIC was overall a more predictive metric). Although both BrIC and RVCI have been shown to correlate well with FE model strains over a broad range of head impact conditions, we believe that further work is necessary to develop a more robust kinematic metric, which can predict tissue-level FE strains over all durations in a more continuous manner.
When comparing the results of this study with findings from similar studies, we observed mixed trends. Hernandez et al., evaluated a large number of kinematic and FE-based brain injury metrics relative to injury outcomes using head impact data from football, boxing, and mixed martial arts.18 Based on their assessment, maximum resultant angular acceleration, GAMBIT, and HIP were among the best kinematic-based predictors of the injury data, while BrIC and maximum resultant angular velocity performed similar to translation-only metrics.18 This preliminary investigation involved 110 head impacts of which only two injuries were used for the assessment, so their conclusions may potentially change with additional injury data points. Brain injury metrics have also been evaluated using field data from automotive-related crashes to assess the efficacy of kinematic-based brain injury criteria.27,32 Results from these studies found that injury rates predicted by HIC and CP were more closely matched with real-world rates than BrIC. However, these field studies do not specifically assess the kinematic metric of HIC, CP, or BrIC, they assess the injury risk function associated with the metric, which is an issue not addressed in the current study.
Previously, Ji et al., evaluated three independently developed and validated FE models of the human head by checking consistency across several brain mechanical responses.21 They observed remarkable differences in every mechanical response variable assessed. In this study, two different FE models of the human head (SIMon and GHBMC) were used, and strain results were compared to assess consistency. The correlation trends were similar regardless of the FE model used, with rotational-based metrics performing better than translational ones. Specifically, BrIC and RVCI were the best performing metrics and maximum resultant linear acceleration had the lowest correlation with MPS and CSDM. Consistency between the models suggests that these conclusions are not model dependent.
Although various intracranial responses were used to rigorously evaluate both FE models, it is possible that the head kinematics and strain-based responses obtained in the current study fall outside the range of experimental data used to validate these models. Relative brain-skull displacement was previously validated using experimentally measured data from cadavers that were subjected to blunt head impacts in all three anatomical planes.15,16 These tests were designed to provide direct measurement of brain-tissue displacements for validation of FE models with application to TBI mechanisms in automotive and sport-related head impact environments. Head motion reported in the tests by Hardy et al. varied up to 291 g, 24 rad s−2, and 37 rad s−1 in maximum resultant linear head CG acceleration, angular acceleration, and angular velocity, respectively. Approximately 97, 100, and 60%, respectively, of the 660 head impacts in the current study fall within these ranges. Although only 60% of the angular velocities attained in the current study were covered by the Hardy et al. dataset, several studies have applied angular velocities from occupant and pedestrian crash tests with magnitudes exceeding 65 rad s−1 to the SIMon and GHBMC models without having significant stability issues.49–52,55
Conclusions
The performance of fifteen kinematic-based brain injury metrics was assessed by comparing their correlation to tissue-level strain responses obtained from 660 head impacts simulated in two separate FE models of the human head. Results revealed rotation-only-based metrics to have higher correlation with FE model strains when compared to combined rotation-translation and translation-only metrics. Based on these findings, and the FE models used to derive strain-based metrics, kinematic brain injury criteria targeting closed head injuries, including DAI and concussion, should be based solely on rotational head kinematics. Furthermore, two angular velocity-based metrics, BrIC and RVCI, were found to have the highest overall correlation with this dataset. Although these metrics showed high capability for predicting FE model strains, their efficacy is limited to a specific regime of loading. Future kinematic-based brain injury criteria development should look to improve upon these two metrics. Doing so will help improve kinematic-to-strain predictions over a broader range of head impact conditions, and increase capabilities to discriminate the efficacy of improved countermeasures targeted for use in the design of head safety systems.
References
Bain, A. C., and D. F. Meaney. Tissue-level thresholds for axonal damage in an experimental model of central nervous system white matter injury. J. Biomech. Eng. 122:615–622, 2000.
Bandak, F. A. On the mechanics of impact neurotrauma: a review and critical synthesis. J. Neurotrauma 12:635–649, 1995.
Bandak, F. A., A. X. Zhang, R. E. Tannous, F. DiMasi, P. Masiello, and R. H. Eppinger. Simon: a simulated injury monitor; application to head injury assessment. In: Proceedings: International Technical Conference on the Enhanced Safety of Vehicles (Vol. 2001, p. 7), National Highway Traffic Safety Administration, 2001.
CDC. CDC | Rates of TBI-related Emergency Department Visits, Hospitalizations, and Deaths | Traumatic Brain Injury | Injury Center. www.cdc.gov.
Crandall, J. Injury Criteria Development: THOR Metric SD-3 Shoulder Advanced Frontal Crash Test Dummy. NHTSA Biomechanics Database, 2013. www-nrd.nhtsa.dot.gov.
Crandall, J. ATD Thoracic Response Test Development: 20 Degree Far Side Oblique Frontal, Front Passenger Position. NHTSA Biomechanics Database, 2014. www-nrd.nhtsa.dot.gov.
Department of Transportation NHTSA Docket Number 69-7, Notice 19. Occupant Crash Protection—Head Injury Criterion, S6.2 of MVSS 208
Forman, J. L., Lopez-Valdes F, D. J. Lessley, P. Riley, M. Sochor, S. Heltzel, J. Ash, R. Perz, R. W. Kent, T. Seacrist, K. B. Arbogast, H. Tanji, and K. Higuchi. Occupant kinematics and shoulder belt retention in far-side lateral and oblique collisions: a parametric study. Stapp Car Crash J. 57:343–385, 2013.
Gabler, L. F., J. R. Crandall, and M. B. Panzer. Investigating brain injury tolerance in the Sagittal Plane using a finite element model of the human head. Int. J. Automot. Eng. 7:37–43, 2016.
Gadd, C. W. Use of a weighted-impulse criterion for estimating injury hazard. SAE Technical Paper, 1966.
Gennarelli, T. A., J. M. Abel, H. Adams, and D. Graham. Differential tolerance of frontal and temporal lobes to contusion induced by angular acceleration. In: Proceedings of the 25th Stapp Car Crash Conference, 1979, pp. 563–586.
Gennarelli, T. A., L. E. Thibault, J. H. Adams, D. I. Graham, C. J. Thompson, and R. P. Marcincin. Diffuse axonal injury and traumatic coma in the primate. Ann. Neurol. 12:564–574, 1982.
Gennarelli, T. A., L. E. Thibault, and A. K. Omaya. Comparison of linear and rotational acceleration in experimental cerebral concussion. In: Proceedings of the 15th Stapp Car Crash Conference, Society of Automotive Engineers, New York, 1971.
Greenwald, R. M., J. T. Gwin, J. J. Chu, and J. J. Crisco. Head impact severity measures for evaluating mild traumatic brain injury risk exposure. Neurosurgery 62:789, 2008.
Hardy, W. N., C. D. Foster, M. J. Mason, K. H. Yang, A. I. King, and S. Tashman. Investigation of head injury mechanisms using neutral density technology and high-speed biplanar x-ray. Stapp Car Crash J. 45:337–368, 2001.
Hardy, W. N., M. J. Mason, C. D. Foster, C. S. Shah, J. M. Kopacz, H. Yang, A. I. King, J. Bishop, and M. Bey. A study of the response of the human cadaver head to impact. Stapp Car Crash J. 51:17–80, 2007.
Harmon, K. G., J. A. Drezner, M. Gammons, K. M. Guskiewicz, M. Halstead, S. A. Herring, J. S. Kutcher, A. Pana, M. Putukian, and W. O. Roberts. American Medical Society for Sports Medicine position statement: concussion in sport. Br. J. Sports Med. 47:15–26, 2013.
Hernandez, F., L. C. Wu, M. C. Yip, K. Laksari, A. R. Hoffman, J. R. Lopez, G. A. Grant, S. Kleiven, and D. B. Camarillo. Six degree-of-freedom measurements of human mild traumatic brain injury. Ann. Biomed. Eng. 43:1918–1934, 2015.
Holbourn, A. H. S. Mechanics of head injuries. Lancet 242:438–441, 1943.
IIHS TechData. Insurance Institute for Highway Safety. Ruckersville, VA. https://techdata.iihs.org/.
Ji, S., H. Ghadyani, R. P. Bolander, J. G. Beckwith, J. C. Ford, T. W. McAllister, L. A. Flashman, K. D. Paulsen, K. Ernstrom, S. Jain, R. Raman, L. Zhang, and R. M. Greenwald. Parametric comparisons of intracranial mechanical responses from three validated finite element models of the human head. Ann. Biomed. Eng. 42:11–24, 2014.
Kerrigan, J., C. Arregui-Dalmases, and J. Crandall. Assessment of pedestrian head impact dynamics in small sedan and large SUV collisions. Int. J. Crashworth. 17:243–258, 2012.
Kerrigan, J. R., J. R. Crandall, and B. Deng. A comparative analysis of the pedestrian injury risk predicted by mechanical impactors and post mortem human surrogates. Stapp Car Crash J. 52:527–567, 2008.
Kimpara, H., and M. Iwamoto. Mild traumatic brain injury predictors based on angular accelerations during impacts. Ann. Biomed. Eng. 40:114–126, 2012.
Kimpara, H., Y. Nakahira, M. Iwamoto, S. Rowson, and S. Duma. Head injury prediction methods based on 6 degree of freedom head acceleration measurements during impact. Int. J. Automot. Eng. 2:13–19, 2011.
Kleiven, S. Predictors for traumatic brain injuries evaluated through accident reconstructions. Stapp Car Crash J 51:81–114, 2007.
Laituri, T. R., R. E. El-Jawahri, S. Henry, and K. Sullivan. Field-based assessments of various AIS2+ head risk curves for frontal impact. SAE Technical Paper, 2015.
Mao, H., L. Zhang, B. Jiang, V. V. Genthikatti, X. Jin, F. Zhu, R. Makwana, A. Gill, G. Jandir, A. Singh, et al. Development of a finite element human head model partially validated with thirty five experimental cases. J. Biomech. Eng. 135:111002, 2013.
Margulies, S. S., and L. E. Thibault. A proposed tolerance criterion for diffuse axonal injury in man. J. Biomech. 25:917–923, 1992.
Marjoux, D., D. Baumgartner, C. Deck, and R. Willinger. Head injury prediction capability of the HIC, HIP, SIMon and ULP criteria. Accid. Anal. Prev. 40:1135–1148, 2008.
Meaney, D. F., D. H. Smith, D. I. Shreiber, A. C. Bain, R. T. Miller, D. T. Ross, and T. A. Gennarelli. Biomechanical analysis of experimental diffuse axonal injury. J. Neurotrauma 12:689–694, 1995.
Mueller, B., A. MacAlister, J. Nolan, and D. Zuby. Comparison of HIC and BRIC head injury risk in IIHS frontal crash tests to real-world head injuries. In: Proceedings of the 24th International Technical Conference on the Enhanced Safety of Vehicles, 2015.
National Operating Committee on the Standards for Athletic Equipment (NOCSAE). Standard test method and equipment used in evaluating the performance characteristics of protective headgear/equipment. National Operating Committee on the Standards for Athletic Equipment, Overland Park, KS, 2012.
Newman, J. A generalized acceleration model for brain injury threshold (GAMBIT). In: Proceedings of the 1986 International IRCOBI Conference on the Biomechanics of Impact, 1986.
Newman, J. A., N. Shewchenko, and E. Welbourne. A proposed new biomechanical head injury assessment function—the maximum power index. Stapp Car Crash J. 44:215–247, 2000.
NHTSA NVS | Vehicle Crash Test Database (www-nrd.nhtsa.dot.gov/database/VSR/veh/QueryVehicle.aspx).
Ommaya, A. K. Biomechanics of head injury: experimental aspects. Biomech. Trauma 13:245–269, 1985.
Ommaya, A. K., and T. A. Gennarelli. Cerebral concussion and traumatic unconsciousness. Correlation of experimental and clinical observations of blunt head injuries. Brain 97:633–654, 1974.
Ommaya, A. K., A. E. Hirsch, P. Yarnell, and E. H. Harris. Scaling of experimental data on cerebral concussion in sub-human primates to concussion threshold for man. DTIC Document, 1967.
Ommaya, A. K., S. D. Rockoff, M. Baldwin, and W. S. Friauf. Experimental concussion: a first report. J. Neurosurg. 21:249–265, 1964.
Ono, K., A. Kikuchi, M. Nakamura, H. Kobayashi, and N. Nakamura. Human head tolerance to sagittal impact reliable estimation deduced from experimental head injury using subhuman primates and human cadaver skulls. SAE Technical Paper, 1980.
Panzer, M. B., B. S. Myers, B. P. Capehart, and C. R. Bass. Development of a finite element model for blast brain injury and the effects of CSF cavitation. Ann. Biomed. Eng. 40:1530–1544, 2012.
Patrick, L. M., H. R. Lissner, and E. S. Gurdjian. Survival by design: head protection. In: Proceedings of American Association for Automotive Medicine Annual Conference, Vol. 7. Association for the Advancement of Automotive Medicine, 1963.
Rowson, S., and S. M. Duma. Brain injury prediction: assessing the combined probability of concussion using linear and rotational head acceleration. Ann. Biomed. Eng. 41:873–882, 2013.
Rowson, S., S. M. Duma, J. G. Beckwith, J. J. Chu, R. M. Greenwald, J. J. Crisco, P. G. Brolinson, A.-C. Duhaime, T. W. McAllister, and A. C. Maerlender. Rotational head kinematics in football impacts: an injury risk function for concussion. Ann. Biomed. Eng. 40:1–13, 2012.
SAE. J211/1: Instrumentation for impact test—part 1—electronic instrumentation. Technical Report, SAE International, 1995.
Santiago, L. A., B. C. Oh, P. K. Dash, J. B. Holcomb, and C. E. Wade. A clinical comparison of penetrating and blunt traumatic brain injuries. Brain Inj. 26:107–125, 2012.
Subit, D., J. Kerrigan, J. R. Crandall, K. Fukuyama, K. Yamazaki, K. Kamiji, and T. Yasuki. Pedestrian-vehicle interaction: kinematics and injury analysis of four full scale tests. In: Proceedings of the International Research Council on Biomechanics of Injury (IRCOBI), 2008.
Takhounts, E. G., M. J. Craig, K. Moorhouse, J. McFadden, and V. Hasija. Development of brain injury criteria (Br IC). Stapp Car Crash J. 57:243–266, 2013.
Takhounts, E. G., R. H. Eppinger, J. Q. Campbell, R. E. Tannous, et al. On the development of the SIMon finite element head model. Stapp Car Crash J. 47:107, 2003.
Takhounts, E. G., V. Hasija, S. A. Ridella, S. Rowson, and S. M. Duma. Kinematic rotational brain injury criterion (BRIC). In: Proceedings of the 22nd Enhanced Safety of Vehicles Conference. Paper no. 11-0263, 2011.
Takhounts, E. G., S. A. Ridella, V. Hasija, R. E. Tannous, J. Q. Campbell, D. Malone, K. Danelson, J. Stitzel, S. Rowson, and S. Duma. Investigation of traumatic brain injuries using the next generation of simulated injury monitor (SIMon) finite element head model. Stapp Car Crash J 52:1–31, 2008.
Thibault, L. E., T. A. Gennarelli, S. S. Margulies, J. Marcus, and R. Eppinger. The strain dependent pathophysiological consequences of inertial loading on central nervous system tissue. In: International IRCOBI Conference on the Biomechanics of Impacts, Bron, France, 1990.
Versace, J. A Review of the Severity Index. Warrendale, PA: SAE International, 1971.
Yanaoka, T., Y. Dokko, and Y. Takahashi. Investigation on an injury criterion related to traumatic brain injury primarily induced by head rotation. SAE Technical Paper, 2015.
Zhang, L., K. H. Yang, and A. I. King. A proposed injury threshold for mild traumatic brain injury. J. Biomech. Eng. 126:226–236, 2004.
Acknowledgments
The authors thank the Partnership for Dummy Technology and Biomechanics (PDB) for support and funding for this research. We also thank Dr. Erik Takhounts, Vikas Hasija, and Daniel Parent of NHTSA, and David Zuby, Becky Mueller, and Anna MacAlister of IIHS for their help in obtaining head kinematic data from the NHTSA and IIHS databases, respectively.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Karol Miller oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gabler, L.F., Crandall, J.R. & Panzer, M.B. Assessment of Kinematic Brain Injury Metrics for Predicting Strain Responses in Diverse Automotive Impact Conditions. Ann Biomed Eng 44, 3705–3718 (2016). https://doi.org/10.1007/s10439-016-1697-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1697-0