Abstract
We describe the development of experimental platforms to quantify the regeneration of injured central nervous system (CNS) neurons by combining engineering technologies and primary neuronal cultures. Although the regeneration of CNS neurons is an important area of research, there are no currently available methods to screen for drugs. Conventional tissue culture based on Petri dish does not provide controlled microenvironment for the neurons and only provide qualitative information. In this review, we introduced the recent advances to generate in vitro model system that is capable of mimicking the niche of CNS injury and regeneration and also of testing candidate drugs. We reconstructed the microenvironment of the regeneration of CNS neurons after injury to provide as in vivo like model system where the soluble and surface bounded inhibitors for regeneration are presented in physiologically relevant manner using microfluidics and surface patterning methods. The ability to control factors and also to monitor them using live cell imaging allowed us to develop quantitative assays that can be used to compare various drug candidates and also to understand the basic mechanism behind nerve regeneration after injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The field of biological studies has offered many collaborative works to engineering and has been challenged by employing microtechnologies to address various problems in currently available methodologies. For example, the capability to generate miniaturized artificial platforms that manipulate living systems has inspired to develop many footprints of analytical devices such as gene chips, lab-on-a-chip, more recently cells-on-a-chip.
Especially in the field of neuroscience, microfluidics-based experimental platforms have offered precise spatio-temporal control of cellular microenvironment such that we could explore various neuronal events. By combining microfluidic technology and the neurobiology, we could overcome variety of technical limitations in neurobiology such as culturing primary neurons,31 isolating axons,29,30 patterning cultured neurons,26 controlling the neurite outgrowth for mimicking axonal injury,33 local protein synthesis in axon,14 axonal regeneration,23 and neuron-to-cell spread of viruses.18 Although, microfluidics opened the gate for innovative applications in neuroscience, there are still many questions to be answered. For instance, the inability of central nervous system (CNS) neurons to regenerate after injury, while young peripheral neurons easily regenerate, has posed a very long-standing question for scientists. The intrinsic differences between CNS neurons and peripheral nervous system (PNS) neurons, and the differences between the two types of environments have been implicated and studied for many years since CNS neuron regeneration after injury can have tremendous clinical implications. Initially, the leading hypothesis used to be that with age and development CNS neurons lose their ability to re-grow and regenerate. However, Aguayo and colleagues7 successfully demonstrated that adult CNS injured neurons are capable of extending long processes if the environment is favorable, namely if there is a graft of peripheral nervous tissue in the CNS lesion site. This finding revolutionized the research on neuronal regeneration; the limiting factor to CNS regeneration is not intrinsic to the neurons of the CNS, but is the environment that these neurons have to grow within.
According to the previous studies, the inhibitory microenvironments from the complex molecular composition of the scar and damaged myelin have rather been implicated as major contributing factors to CNS regeneration failure.2,11,27,28,36 For example, upregulation and accumulation of numerous compounds such as chondroitin sulfate proteoglycans (CSPG’s)17,20 and myelin associated inhibitors (MAG, Nogo, OMgp)5,6,8,9,27 have been shown to be the major contributors to this growth inhibitory environment.
Efforts that promote axons to overcome the growth inhibitory nature of these compounds can therefore provide an attractive drug discovery strategy for treating trauma in the adult CNS neurons. Yet, progress in treatments is severely restricted due to the limitations in currently available in vitro assays for testing agents that may promote axonal regeneration after injury. First, current assays cannot distinguish different forms of growth that are relevant for regeneration after injury (growth with branching that is characteristic of long-distance growth in tracts vs. arborizing growth characteristics of axons seeking targets). The second limitation is the lack of appropriate method to induce axonal injury with precisely controlled manner. Finally, it is difficult to apply candidate drugs to soma or axons selectively.
Here we introduced microfluidic-based experimental platforms that utilize the compartmentalized culture of primary neurons, surface micropatterning, and laser microbeam induced injury techniques to mimic the complexity of injury and regeneration of CNS neurons. We simulated the inhibitory microenvironment of injured CNS neurons by providing alternatively patterned substrate with permissive/non-permissive coating. In addition, we were able to apply drugs selectively in the somal and axonal region using fluidic isolation in a microfluidic neuron culture chamber. Furthermore, we introduced the integrated use of laser microbeam dissection within a microfluidics-based culture platform to produce precise zones of neuronal injury. These in vitro assays, herein described, showed potential for high-content/throughput screening of drugs to block inhibitory effect of Nogo, MAG, OMgp, and CSPG and/or to promote the regeneration of injured CNS axons.
Traditional In Vitro Assays to Study Injury in CNS Neurons
In order to treat the trauma in CNS, various in vitro assays with controlled experimental conditions have been traditionally employed, where direct effects of the neuron outgrowth inhibitors can be investigated at the cellular and molecular level. Progress in regards to the myelin inhibitors, for instance, has been supported to a large degree by the neurite outgrowth assay and growth cone collapse assay, which are performed in cell culture plates coated with myelin or myelin inhibitor proteins. Through the use of these two assays, three major inhibitory proteins for suppressing axon outgrowth were identified in CNS myelin. While these assays have proved useful for addressing questions related to myelin associated growth inhibitor molecules in neuronal development and elongation, they suffer from two major limitations. First, it is not able to probe the axons independently from the cell bodies. The second limitation is that these assays do not provide an appropriate method to induce axonal injury in vitro. Axonal damage is critical to the etiology of CNS injuries and neurodegenerative disease. In attempting to mimic CNS axonal injury, various tools such as rubber impactors with electrically driven vertical shaft,10 a sharp metal knife25 and pulled glass electrodes19 have been developed. These tools could generate crush injury of axons to mimic spinal cord injury and also perform a quantitative analysis of regenerated axons. But, these methods can cut just a few axons at a time with a complex and expensive micromanipulator with lack of reproducibility and less control.
Traditional Compartmentalized Culture Methods
The Campenot chamber firstly allowed for isolation of axons from the cell bodies in different compartments and for severing the isolated axons by supplying neurotrophic factors to artificially stimulate axonal growth from macro-scaled cultures across grease layers.3 In the evolution of in vitro axonal injury models, Campenot chambers were used to induce injury on isolated axons. Isolated axons from cell bodies are easily cut by directing a water jet toward one of the side compartments through a 22 gauge needle.4 This method has generated a uniform front of regenerating axons, and has facilitated quantification of both the pattern and the timing of neuritic regeneration. CNS neurons related with most neurodegenerative diseases and injuries (e.g., cortical, hippocampal and spinal cord neurons) have not been successfully cultured in Campenot chambers because these neurons are traditionally difficult to culture. Therefore, Ivins’ Chambers were also developed for isolating hippocampal axons, which had a thin coverslip and a grease layer.15 However, Champenot and Ivins’ Chamber had the tendency to leak easily and difficulty to image due to the usage of opaque grease sealing layer.
Neuron Culture and Axon Isolation in Microfluidic Devices
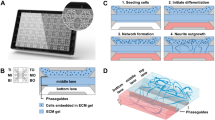
To overcome drawbacks in currently available assays for investigating the trauma in CNS neurons, Jeon’s group developed a device for isolating axon.24,29,31 As shown in Fig. 1, Jeon’s device incorporates microgrooves (10 μm wide, 3 μm high and 150–900 μm in length) to allow the isolation of axons from cell bodies, such that their physiological and biochemical change by treatment can be studied in distinct part of neurons. The optically transparent PDMS adheres to a poly-l-lysine coated coverslip. Rat CNS neurons are added to the somal-side reservoir and are drawn into the somal channel (blue) by capillary action. Within 3–4 days, axonal growth is guided into the axonal side (red) through the microgrooves. A volume difference between the somal side and axonal side (~50 μL) allows chemical microenvironments to be isolated to axons for over 20 h owing to the high fluidic resistance of the microgrooves. The high fluidic resistance of microgrooves produces small but sustained flow between the compartments that counteracts diffusion.26,31 Fluidic isolation of the somal compartment from the axonal compartment is established by difference of volumes filled each chamber resulting in a hydrostatic pressure. The microgrooves also prevented the passage of cell bodies and guide neurite growth into the axonal isolation compartment.24,29,31 This device can be provided as a highly adaptable platform to resemble many aspects in the neurodegeneration and injury of CNS neurons.
The microfluidic-based neuron culture platform directs axonal growth of CNS neurons and fluidically isolates axons. (a) The photograph of neuron culture device that contains food dye for channel visualization. (b) The culture chamber consists of a PDMS mold containing a relief pattern of somal and axonal compartments (1.5 mm wide, 7 mm long, 100 μm high) connected by microgrooves (10 μm wide, 3 μm high). (c), (e) phase micrographs of 6 DIV neurons cultured in the microfluidic device and (d) Confocal micrograph of Tau (green) and MAP5 (red) immunostained neurons, which demonstrate all processes crossing the barrier are axons
Mimetic Microenvironment with Soluble Inhibitory Proteins
The neuron culture device could be utilized as an in vitro model for CNS axonal injury and regeneration because we could generate an injury of axons by vacuum aspiration and apply localized chemical treatments to CNS axons. Utilizing this property, Jeon’ group intensively investigated the effects of myelin inhibitors on regeneration of injured CNS axons.23 Figure 2 outlines the procedure, where rat E18 cortical neurons were seeded into the somal (left) compartment and cultured for 7 days. Isolated axons were cut by vacuum aspiration from the axonal compartment (Fig. 3). Due to high fluidic resistance of the microgrooves, however, the cell bodies in the somal compartment were not disturbed. After injury, neurobasal medium was added to both compartments and the samples were incubated for 24 h. To monitor the regeneration of injured axons, time-lapse images were taken for 16 h post axotomy. Figure 3 shows the re-growth patterns of the injured axons in the axonal compartment. In this configuration the truly re-generating axons (white arrows) can be distinguished from their un-injured cohorts (black arrows). Using this platform, we investigated the inhibitory effect of myelin proteins on injured axons by applying soluble Nogo-66 and MAG-Fc proteins. Time-lapse micrographs revealed that the injured axons exhibit a dynamic behavior and were able to regenerate in normal neurobasal medium. After axotomy, normal medium without Nogo-66 was added to the axonal side immediately. It has been previously shown that the Nogo gene encodes three isoforms (Nogo-A, B, C); all of which contain a 66-amino acid extracellular domain termed Nogo-66. Our rational for choosing Nogo-66 was based solely on the importance of this stretch of amino acid sequence in interacting with the cell surface Nogo receptor (NGR) and mediating its inhibitory effects.12 MAG has also been shown to be a very potent inhibitor of axonal growth in vitro and is likely to play an important role in preventing regeneration immediately after injury.21,22 It has further been shown that the three myelin-associated inhibitors, Nogo, MAG, and OMgp, exert their inhibition by interacting with the same receptor (NGR), highlighting a clearly defined target for overcoming myelin inhibition of CNS regeneration. Axons were removed from the axonal compartment of microfluidic devices to mimic axonal injury. Following axotomy by vacuum aspiration, we treated different concentrations of Nogo-66 on both somal and axonal compartments for 24 h. Upper panel of Fig. 3b shows regenerated axons in normal culture medium and in presence of Nogo (100 nM Nogo-66 protein). Supported by previous reports, these results clearly indicate that Nogo inhibits CNS axonal regeneration.
Schematic diagram shows axotomy procedure in the microfluidic device. The steps are described in the diagram. A glass pipette connected to vacuum is placed in the bottom reservoir leading to the axonal compartment (red). Aspiration was applied for 5–10 s. Axons are severed when a bubble passes through the channel. Aspiration is continued until all media from the opposite reservoir is removed and the main channel is emptied. To increase the efficiency of the severing, the reservoirs are filled with fresh media and the aspiration is repeated from the top reservoir
(a) Time-lapse imaging of axons for 16 h after lesion. Note that re-generating axons (white arrowheads) can be distinguished from the following un-injured cohorts (black arrowheads). (b) Phase-contrast micrographs Nogo treated axons 24 h post axotomy. Nogo-66 was added to both axonal and somal chambers for 24 h before taking the micrographs. (c) Fluorescence micrographs of MAG-Fc treated axons 24 h post axotomy. Axons were stained with Calcein AM. MAG-Fc was added to both axonal and somal chambers for 24 h before taking the micrograph
As illustrated in the phase-contrast images, even simple inspection of the devices indicated that in the presence of Nogo, the average length of regenerated axons was noticeably shorter than controls. Regenerated axon lengths were reduced to ~80% of control by the Nogo-66. Following procedures described above, the inhibitory effects of myelin associated glycoprotein, MAG, was also quantitatively examined (bottom panel of Fig. 3b). The length of regenerated axons was measured after 24 h of MAG-Fc (250 nM) treatment. Quantitative analysis revealed that MAG diminished the average length of regenerated axons to ~75% of the control.23
Mimetic Microenvironment with Surface Bounded Inhibitory Proteins
Microfluidics-based neuron culture chamber used physical barrier that is made of microstructures to isolate axons and mimic the microenvironment of CNS injuries. Jeon’s group also utilized micro-patterned substrate of biochemical cues to generate the microenvironment with surface bounded inhibitory proteins in CNS injury. We developed a microfluidic based strip assay that utilized cultures of dissociated neurons to model the organized structure of the spinal cord such as spatial separation of the axonal extensions from the cell bodies.33 Micromolding in capillaries (MIMIC) was used to pattern fine strips of inhibitive and permissive substrates on a solid support. We also introduced simple pinch valves, as virtural barrier between two sets of channels, one designated for selective loading of the cells and the other for patterning strips onto the surface. The compartment designated for cell loading can be fluidically isolated with a barrier that is formed by local constriction or tapering of the patterning channels. As shown in Fig. 4, a member of the CSPG family, lines (150 μm wide) were patterned on PLL coated substrate, while the cell-loading area was coated with laminin. As shown in the overlay (Fig. 4a), CSPG is strictly confined to its lanes, and can be distinguished from the PLL background, while laminin is confined to the cell-loading area. To demonstrate the applicability of the valves, aggrecan lines (150 μm wide) were patterned on PLL coated substrate by MIMIC. The cell-loading area was coated with laminin. To evaluate the fluidic isolation between the strips and cell culture area, the cover slips were stained with CS56 (red) and anti-laminin (green) following the removal of the stamp. An examination of stained samples reveals the quality and distribution of the inhibitory strips, in addition to the fluidic isolation between the regions. Figure 4b shows the selective spatial distribution of the cell bodies and axons after 10 days culture. In this configuration the cell bodies are located on the laminin-coated area (left-hand side); while axons are extended on the patterned substrate. Rat cortical neurons were cultured on a permissive substrate (laminin) remain on the PLL coated regions while avoiding aggrecan (non-permissive) strips.
Simple pinch valves, narrow necks work as virtual barriers, between the strips and cell culture area fluidically separating the regions. (a) CSPG is strictly confined to its lanes, and can be distinguished from the PLL background (black), while laminin is confined to the cell-loading area. (b) A phase-contrast photograph taken after 10 DIV. (c) The structure of the valves is further demonstrated by the phase-contrast image and a close up of the junction between the patterning channels and the cell-loading area. (d) Effect of chondroitinase-ABC treatment on axons growing in microfluidic strip assay device. 10 DIV cortical neurons growing on aggrecan-PLL patterned strips on glass
In order to demonstrate the application in drug screening for SCI, we used chondroitinase-ABC as a model drug to overcome the nerve-inhibitory effect of aggrecan. As shown in Fig. 4d, we observed striking changes in growth cone morphology and axonal projections when we treated patterned cells with chondroitinase-ABC, an enzyme that removes the CSPG’s GAG side chains without degradation of the core protein. Neuronal processes were shown to move freely across the strips in random manner. Axons avoid inhibitor-coated areas until a drug is applied to help axons overcome the inhibition or breakdown the surface-bound inhibitors. Axons avoid aggrecan strips and are confined to PLL strips during entire experimental period. After 30 min chondroitinase -ABC treatment, axons are observed to randomly extend across the pattern. Higher resolution micrographs indicate that aggrecan inhibition is overcome not only in the growth cones but in the middle of the strips as well.
Precisely Controlled Generation of Axonal Injury Using Laser
We recently described the integrated use of pulsed laser microbeams and microfluidics based surface patterned culture to examine the dynamics of axonal injury and regeneration in vitro.13 Pulsed femtosecond laser microbeams have been used to produce axonal injury in vivo in animal models, which are attractive tools for cell microsurgery in vivo due to their ability to generate extremely localized damage zones in single cells.1,32,35 However, the high cost and complex operation of these femtosecond laser systems makes them impractical for many researchers. Also, the high intensities associated with the use of ultrashort laser pulses produce photochemical effects such as the production of reactive oxygen species and direct biomolecular damage.34 Therefore, we utilized nanosecond and picosecond laser microbeams at visible wavelengths in order to minimize the possibility of photochemical damage. In this study, we used 180 ps duration laser pulses to create reproducible and precisely controlled zones of axonal injury of cultured primary neurons on alternating strip pattern of aggrecan and PLL (Fig. 5).13 The precision of the laser microbeam irradiation allowed partial or complete transection of the individual neurite bundles using single laser pulse energy of 400 nJ or 800 nJ, respectively. By varying laser pulse energy, a single laser microbeam exposure can produce partial or complete transection (Figs. 5d, 5e) while preserving both the proximal and the distal segments of the transected neurites.13
(a) Microfluidic-based culture platform using surface micropatterning. (b) Before and (c) after illustrations of laser induced axotomy to provide precise damage to selected neurons while preserving both the proximal and distal segments of transected axons and leaving the cell bodies intact. Axotomy of 25 μm axon strips using a single 180 ps laser pulse. Axotomy was performed on the lower strip, leaving the neighboring upper strip unaffected. Images taken 1 min following laser pulse delivery: (d) partial and (e) complete transections, using Ep = 400 nJ and 800 nJ, respectively. On single axon of E18 embryonic neuron, white boxes indicate the before (f) and after (g) phase-contrast micrographs of axotomy based on laser induced axotomy
This integrated microfluidics-based platform with laser irradiation offers several advantages over other in vitro models of axonal injury.10,19,23,25 First, the microfluidic approach allows explicit and precise manipulation of the spatial organization of CNS neurons. The alternating surface pattern of aggrecan and PLL controls the outgrowth of neurites toward specific regions and also polarize their growth to allow anterograde and retrograde directions to be clearly defined by the directionality of the growing bundles. Second, picosecond laser microbeam irradiation produces precise and reproducible zones of axonal injury within the bundles such that it allows us to determine important parameters, such as dieback of proximal neurite segment, and anterograde degeneration involving the distal neuritic segment. Finally, the integrated microfluidic platform with laser microbeam is free from effects of many systemic and homeostatic influences, and allows control of the extracellular environment.
Prospective Studies for Investigating Injury and Regeneration of CNS Neurons Using Microfluidic Platforms
We expect that microfluidic platforms could be a promising tool to study cellular and molecular events regulating regeneration of injured CNS neurons. CNS is represented as billions of neurons and even more complex interconnected cellular interactions. Moreover, neuronal connectively and metabolism is tightly regulated by interaction between different subtypes of neuronal and glial cells such as neurons, astrocytes, microglia, and oligodendrocytes. Hence, co-culturing neuronal and glial cells would be considered as more physiologically relevant in vitro model for injury and regeneration in CNS. For example, we showed a simplified method for visualizing myelination such that rat primary neurons and oligodendrocytes could be co-cultured in a microfluidic platform.29 In this paper, we described micrometer scaled approaches for manipulating neurons such as microfluidic based compartmentalized culture and surface micropatterning technique. Although these methods make up for the limitation in conventional tissue culture, they need to be scaled down for developing in vitro assays that can handle biological events in single neuronal scale. We recently showed the crosstalk between growth cone and nanotopographical ECM cues using micro- and nano-technology.16 Further studies will be followed up to dissect out molecular mechanisms of regeneration in single cell level. Considering the scale of cells, most of in vitro microfluidic platforms to study injury and regeneration of CNS neuron have utilized primary cells, which are restricted by limited number of cells and by variability among individual animals. Stem cell technology enables us to generate relatively uniform population of neuronal and glial cells. Especially, we can perform pathological/mechanistic studies for healthy and disease state of nervous system using induced pluripotent stem cells. Using the ability to control microenvironment of cultured neurons, microfluidic platforms can be used in generating in vivo like niche for stem cell derived cell components in the nervous system. We suggest an interdisciplinary work that combines microfluidic technology with stem cell biology to identify neuronal integrity and dissect out targeting signaling pathways for screening pharmaceutical molecules to promote CNS regeneration or to block inhibitory signals on injured neurons.
Conclusions
Studying spinal cord injury and regeneration has been hampered due to the lack of: (a) appropriate in vitro model to reconstruct spatially localized and reproducible areas of injury for the study of axonal regrowth and (b) assays to evaluate the efficacy of chemicals that may provide axonal regeneration after injury. Microfluidics based experimental platforms can provide a novel methodology to direct and isolate neuronal processes and to mimic in vivo like microenvironment of injured CNS neurons and their regeneration. Using compartmentalized and surface patterned cell culture technique, we were able to precisely generate the inhibitory microenvironment of spinal cord injury with both soluble and surface-bounded factors. Furthermore, we could perform drug-screening assay that aims to find candidate for chemicals to overcome inhibitory microenvironment with axonal injury and/or promote the regeneration of injured axons. We also integrated the pulsed laser microbeam irradiation with microfluidic neuronal cell culture and time-lapse microscopy allows the study of dynamics of axonal injury and regrowth under controlled conditions. This utilization was provided to create precisely localized injury to neuronal processes permits axons to be severed without injury to the cell bodies or the underlying matrix. Using time-lapse microscopy we could quantitatively image for both proximal and distal segments that provides direct measurement of sequential changes in neurite response, such as dieback, anterograde degeneration, and regeneration. In summary, microfluidics based in vitro model of axonal injury herein provides a suitable platform to study CNS injury and regeneration, since the platforms offer excellent control of physiologically relevant injury parameters in vitro such as the generation of localized injury and selective application of candidate drugs toward a specific region of neurons.
References
Bourgeois, F., and A. Ben-Yakar. Femtosecond laser nanoaxotomy properties and their effect on axonal recovery in C. elegans. Opt. Express 15:8521–8531, 2007.
Busch, S. A., and J. Silver. The role of extracellular matrix in CNS regeneration. Curr. Opin. Neurobiol. 17:120–127, 2007.
Campenot, R. B. Local control of neurite development by nerve growth factor. Proc. Natl Acad. Sci. USA. 74:4516–4519, 1977.
Campenot, R. B. Development of sympathetic neurons in compartmentalized cultures. II. Local control of neurite survival by nerve growth factor. Dev. Biol. 93:13–21, 1982.
Caroni, P., and M. E. Schwab. Antibody against myelin-associated inhibitor of neurite growth neutralizes nonpermissive substrate properties of CNS white matter. Neuron 1:85–96, 1988.
Crutcher, K. A. Tissue sections from the mature rat brain and spinal cord as substrates for neurite outgrowth in vitro: extensive growth on gray matter but little growth on white matter. Exp. Neurol. 104:39–54, 1989.
David, S., and A. J. Aquayo. Axonal elongation into peripheral nervous system “bridges” after central nervous system injury in adult rats. Science 214:931–933, 1981.
Domeniconi, M., Z. Cao, T. Spencer, R. Sivasankaran, K. Wang, E. Nikulina, N. Kimura, H. Cai, K. Deng, Y. Gao, Z. He, and M. Filbin. Myelin-associated glycoprotein interacts with the Nogo66 receptor to inhibit neurite outgrowth. Neuron 35:283–290, 2002.
Domeniconi, M., and M. T. Filbin. Overcoming inhibitors in myelin to promote axonal regeneration. J. Neurol. Sci. 233:43–47, 2005.
Fayaz, I., and C. H. Tator. Modeling axonal injury in vitro: injury and regeneration following acute neuritic trauma. J. Neurosci. Methods 102:69–79, 2000.
Filbin, M. T. Myelin-associated inhibitors of axonal regeneration in the adult mammalian CNS. Nat. Rev. Neurosci. 4:703–713, 2003.
Fournier, A. E., T. GrandPre, and S. M. Strittmatter. Identification of a receptor mediating Nogo-66 inhibition of axonal regeneration. Nature 409:341–346, 2001.
Hellman, A. N., B. Vahidi, H. J. Kim, W. Mismar, O. Steward, N. L. Jeon, and V. Venugopalan. Examination of axonal injury and regeneration in micropatterned neuronal culture using pulsed laser microbeam dissection. Lab. Chip 10:2083–2092, 2010.
Hengst, U., A. Deglincerti, H. J. Kim, N. L. Jeon, and S. R. Jaffrey. Axonal elongation triggered by stimulus-induced local translation of a polarity complex protein. Nat. Cell Biol. 11:1024–1030, 2009.
Ivins, K. J., E. T. Bui, and C. W. Cotman. Beta-amyloid induces local neurite degeneration in cultured hippocampal neurons: evidence for neuritic apoptosis. Neurobiol. Dis. 5:365–378, 1998.
Jang, K.-J., M. S. Kim, D. Feltrin, N. L. Jeon, K.-Y. Suh, and O. Pertz. Two distinct filopodia populations at the growth cone allow to sense nanotopographical extracellular matrix cues to guide neurite outgrowth. PLoS ONE 5:e15966, 2010.
Jones, L. L., R. U. Margolis, and M. H. Tuszynski. The chondroitin sulfate proteoglycans neurocan, brevican, phosphacan, and versican are differentially regulated following spinal cord injury. Exp. Neurol. 182:399–411, 2003.
Liu, W. W., J. Goodhouse, N. L. Jeon, and L. W. Enquist. A microfluidic chamber for analysis of neuron-to-cell spread and axonal transport of an alpha-herpesvirus. PLoS ONE 3:e2382, 2008.
Mandolesi, G., F. Madeddu, Y. Bozzi, L. Maffei, and G. M. Ratto. Acute physiological response of mammalian central neurons to axotomy: ionic regulation and electrical activity. FASEB J. 18:1934–1936, 2004.
McKeon, R. J., R. C. Schreiber, J. S. Rudge, and J. Silver. Reduction of neurite outgrowth in a model of glial scarring following CNS injury is correlated with the expression of inhibitory molecules on reactive astrocytes. J. Neurosci. 11:3398–3411, 1991.
McKerracher, L., S. David, D. L. Jackson, V. Kottis, R. J. Dunn, and P. E. Braun. Identification of myelin-associated glycoprotein as a major myelin-derived inhibitor of neurite growth. Neuron 13:805–811, 1994.
Mukhopadhyay, G., P. Doherty, F. S. Walsh, P. R. Crocker, and M. T. Filbin. A novel role for myelin-associated glycoprotein as an inhibitor of axonal regeneration. Neuron 13:757–767, 1994.
Park, J. W., B. Vahidi, H. J. Kim, S. W. Rhee, and N. L. Jeon. Quantitative analysis of CNS axon regeneration using a microfluidic neuron culture device. Biochip J. 2:44–51, 2008.
Park, J. W., B. Vahidi, A. M. Taylor, S. W. Rhee, and N. L. Jeon. Microfluidic culture platform for neuroscience research. Nat. Protoc. 1:2128–2136, 2006.
Quilty, M. C., W. P. Gai, D. L. Pountney, A. K. West, and J. C. Vickers. Localization of alpha-, beta-, and gamma-synuclein during neuronal development and alterations associated with the neuronal response to axonal trauma. Exp. Neurol. 182:195–207, 2003.
Rhee, S. W., A. M. Taylor, C. H. Tu, D. H. Cribbs, C. W. Cotman, and N. L. Jeon. Patterned cell culture inside microfluidic devices. Lab. Chip 5:102–107, 2005.
Schwab, M. E., and D. Bartholdi. Degeneration and regeneration of axons in the lesioned spinal cord. Physiol. Rev. 76:319–370, 1996.
Silver, J., and J. H. Miller. Regeneration beyond the glial scar. Nat. Rev. Neurosci. 5:146–156, 2004.
Taylor, A. M., M. Blurton-Jones, S. W. Rhee, D. H. Cribbs, C. W. Cotman, and N. L. Jeon. A microfluidic culture platform for CNS axonal injury, regeneration and transport. Nat. Methods 2:599–605, 2005.
Taylor, A. M., S. W. Rhee, and N. L. Jeon. Microfluidic chambers for cell migration and neuroscience research. Methods Mol. Biol. 321:167–177, 2006.
Taylor, A. M., S. W. Rhee, C. H. Tu, D. H. Cribbs, C. W. Cotman, and N. L. Jeon. Microfluidic multicompartment device for neuroscience research. Langmuir 19:1551–1556, 2003.
Tirlapur, U. K., and K. König. Targeted transfection by femtosecond laser. Nature 418:290–291, 2002.
Vahidi, B., J. W. Park, H. J. Kim, and N. L. Jeon. Microfluidic-based strip assay for testing the effects of various surface-bound inhibitors in spinal cord injury. J. Neurosci. Methods 170:188–196, 2008.
Vogel, A., J. Noack, G. Hüttman, and G. Paltauf. Mechanisms of femtosecond laser nanosurgery of cells and tissues. Appl. Phys. B Lasers Optics 81:1015–1047, 2005.
Yanik, M. F., H. Cinar, H. N. Cinar, A. D. Chisholm, Y. Jin, and A. Ben-Yakar. Neurosurgery: functional regeneration after laser axotomy. Nature 432:822, 2004.
Yiu, G., and Z. He. Glial inhibition of CNS axon regeneration. Nat. Rev. Neurosci. 7:617–627, 2006.
Acknowledgments
This work was supported by the Graduate Studies Abroad Fellowship (KRF-2005-215-D00030), WCU (World Class University) program through the Korea Research Foundation funded by the Ministry of Education, Science and Technology (R31-2008-000-10083-0), Pioneer Research Center Program (2011-0001643), Biomembrane Plasricity Research Center (2011-0000841) through the National Research Foundation (NRF) funded by the National Research Foundation (NRF) funded by the Ministry of Education, Science and Technology and the Industrial Source Technology Development Program (10033657) of the Ministry of Knowledge Economy (MKE) of Korea.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Jong Hwan Sung oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Kim, H.J., Park, J.W., Park, J.W. et al. Integrated Microfluidics Platforms for Investigating Injury and Regeneration of CNS Axons. Ann Biomed Eng 40, 1268–1276 (2012). https://doi.org/10.1007/s10439-012-0515-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-012-0515-6