Abstract
In patients with severe hemorrhage, complications such as shock or death may occur if the patient is not treated appropriately and expeditiously. To create a hemostat kit for severe hemorrhage, ultraviolet light irradiation was applied to photocrosslinkable chitosan hydrogel and calcium alginate. As a hemorrhage model, the femoral arteries and veins of anesthetized rats were cut. Hemodynamics and hematological parameters including red blood cell (RBC) count, hemoglobin concentration, hematocrit, white blood cell (WBC) count, and platelet count, and serum parameters including aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were measured as a marker of hemostasis. In rats for which no procedure was used, death occurred within 30 min. By using the hydrogel hemostat, the survival rate rose to 75% or more. RBC count, hemoglobin, hematocrit, and platelet levels were not significantly changed for 3 days. WBC count increased 1 day after hemostasis. AST and ALT increased 1 day after hemostasis, but it decreased 3 days later. The photocrosslinkable chitosan hydrogel and calcium alginate were biodegraded at 3 and 28 days, respectively, by neutrophils and keratinocyte chemoattractant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In cases of severe trauma, especially severe hemorrhage, no procedure can replace surgery. Complications such as shock may occur if the patient is not treated appropriately and expeditiously. Uncontrolled hemorrhage remains the leading cause of death on the battlefield, large-scale disaster site, or contingency operations, thus accounting for half of all such deaths.30 It is also the leading cause of death among combat casualties and is the second major cause of death in civilian trauma patients.1,5,14,24 Severe hemorrhage and trauma are major risk factors leading to the lethal triad that includes persistent hypothermia, acidosis, and inability to form clots.13 Therefore, much attention has been focused on the development of alternative methods for controlling hemorrhage including topical hemostatic dressings. While several agents have been developed, the three most commonly utilized agents on the battlefield include the chitosan acetate bandage, chitosan granules, and zeolite powder.2,16,31,32 The chitosan acetate bandage has gained popularity for its effectiveness with limited side effects, while zeolite powder produces significant thermal tissue injury leading some to recommend its use only as a last resort in life-threatening situations. Kheirabadi et al. reported the result of comparisons of some hemostatic agents.15 Each agent has both advantages and disadvantages; especially, the more effective it works as a hemostasis, the more difficult it is to remove from hemorrhage area because of the residue in lumens. One of the hemostatic agents, chitosan-based agent, was reported to cause a severe inflammatory reaction. Therefore, the development of an effective new hemostat is required.
We previously reported on a photocrosslinkable chitosan hydrogel that contains both lactose moieties and photoreactive azide groups.12,20 Ultraviolet (UV) irradiation of photocrosslinkable chitosan hydrogel solution resulted in an insoluble hydrogel. The photocrosslinkable chitosan hydrogel was reported as a strong tissue adhesive and provided effective air seal from pinholes on isolated small intestinal and aortic tissues, as well as from incisions on isolated tracheal tissue.21 It has been proposed that the photocrosslinkable chitosan molecules could be used as a biologic adhesive in surgical applications.11,21 Alginate, which belongs to the same polysaccharide group as chitosan, is also widely used as a biomedical material. Calcium alginate was first introduced as a wound dressing, and it is evaluated as a possible surgical hemostat.27,28 It releases calcium ions on contact with blood; the increased local calcium concentration stimulates rapid coagulation through platelet aggregation.3 The importance of Ca2+ ion release in the hemostatic action of this material was demonstrated by studies on whole blood coagulation and platelet aggregation.
Based on these results from previous studies, we examined the utility of hemostasis in severe hemorrhage by taking advantage of the sealing effect of photocrosslinkable chitosan hydrogel and the platelet aggregation effect of calcium alginate.
Materials and methods
Animals
This study was conducted in accordance with the guidelines for the care of animal subjects, as defined by the Institutional Review Board of the National Defense Medical College, Tokorozawa, Japan. Male Sprague-Dawley rats (250–400 g, Japan SLC Inc., Shizuoka, Japan) were used for the study. They were anesthetized with an intraperitoneal injection of pentobarbital (50 mg/kg, Abbott Labs, Chicago, IL).
Preparation of Chitosan
Photocrosslinkable chitosan hydrogel was prepared as previously reported.12,21 In brief, chitosan (Yaizu Suisankagaku Industry Co., Ltd., Shizuoka) with a molecular weight of 800–1000 kDa was 80% deacetylated. Azide (p-azidobenzoic acid) and lactose (lactobionic acid) moieties had been introduced into the amino group and approximately 2.5 and 2% of the amino groups in chitosan had been replaced by p-azidobenzoic acid and lactobionic acid, respectively. In this study, 4% photocrosslinkable chitosan hydrogel was prepared by dissolving the lyophilized photocrosslinkable chitosan with phosphate-buffered saline.
Measurement of Binding Strength
In the UV irradiation apparatus, two square slices of ham (2 × 4 cm and 2-mm thick each) were placed side-by-side with the smaller side closely touching each other. Chitosan gel prepared from 4% photocrosslinkable chitosan hydrogel was then applied to the boundary between the two slices over the 2 cm side (with a thickness of 2 mm) to adhere the slices. After UV irradiation (wavelength: 254 and 365 nm; Vilber Lourmat, Torcy, France) for 30, 60, 90, or 120 s, the adhered ham preparations were hung on a hook with a thread attached to the unglued 2 cm side of one ham slice, and subsequently, they were pulled by hanging various weights on the lower 2 cm side (each ham; n = 7). When the adhered ham separated into the original two slices at a certain weight, the cross-sectional area of the adhered chitosan gel (perpendicular to the larger surface of ham) was measured. The binding strength was calculated using the following formula: binding strength = A ÷ B, where B is the cross-sectional area (cm2) of residual photocrosslinkable chitosan hydrogel and A is the weight (g) at which the ham preparations separated into two slices.
Hemostasis Procedure
Photocrosslinkable chitosan hydrogel was applied to Duraseal film (Diversified Biotech, Boston, MA); 99% of UV irradiation is transmitted through the Duraseal. The rat’s femoral artery and vein were exposed and cut with scissors. Calcium alginate was applied to the area of hemorrhage, and firm pressure was applied. The Duraseal film with photocrosslinkable chitosan hydrogel was then applied over hemorrhage area, and firm pressure was applied with UV irradiation for 90 s (Fig. 1). The effective wavelength of UV was examined using two different wavelengths, 256 nm (n = 12) and 354 nm (n = 10). We sutured without removing each materials.
Hemostasis procedure. Photocrosslinkable chitosan hydrogel (PRC) was applied to Duraseal film. The rat’s femoral artery and vein were exposed and cut with scissors. Calcium alginate was applied to the area of hemorrhage, and firm pressure was applied. The Duraseal film with photocrosslinkable chitosan hydrogel was then applied over hemorrhage area, and firm pressure was applied with UV irradiation for 90 s
Measurements of Hemodynamics and Hematological Parameters
Surgical catheters (polyethylene indwelling needle 24G, Terumo Co., Tokyo, Japan) were inserted into the carotid arteries of the rats. The mean arterial pressure (MAP) was measured from the cannulated carotid artery with a polygraph recording system (model RM-6000, Nihon Kohden, Tokyo, Japan). Blood samples were collected from the carotid arteries after suturing and from the tail veins. The red blood cell (RBC) count, hemoglobin concentration, hematocrit, white blood cell (WBC) count, and platelet count were measured with a hematology analyzer (PCE 170, Erma Inc., Tokyo, Japan).
Measurements of Serum Parameters
Serum total protein, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) concentrations were measured with a Fuji dry-chem system (Fuji Film Co., Tokyo, Japan).
Histological Examinations
The rats were euthanized to remove tissue from the area of hemorrhage at 3 and 28 days after hemostasis as shown in Fig. 1. The tissue samples were immersed in 10% formalin for 2 days. Slides were prepared from the fixed tissue specimens and stained with hematoxylin and eosin (H&E).
Animal Treatment for Biodegradation of Materials
Rats were divided into three groups: photocrosslinkable chitosan hydrogel-embedded, calcium alginate-embedded, and non-embedded (sham) groups (n = 6 for each group). Rats were incised the inguinal region, bared femoral artery and vein. The photocrosslinkable chitosan hydrogel were put on the inguinal region, irradiated UV of 356 nm for 90 s, and sutured. Similarly, calcium alginate was implanted into the inguinal region. As sham groups, rats were incised the inguinal region, bared femoral artery and vein, and were sutured.
Measurements of Hemogram
The differential count of leukocytes was measured after embedding each photocrosslinkable chitosan hydrogel and alginate calcium in the subcutaneous inguinal region. Leukocytes were categorized into five groups in a peripheral blood microscopic image. Leukocyte parameters were distinguished in blood smear preparations. Leukocyte segmentation was assessed in a giemsa-stained image of peripheral blood smears. As a sham model, the skin of the inguinal region was incised, detached from neighboring muscle, and sutured. Hemography was performed by a technical service center at Mitsubishi Chemical MKV Company (Tokyo, Japan).
Measurement of Cytokine
The serum levels of tumor necrosis factor (TNF)-α, interferon (INF)-γ, monocyte chemotactic protein (MCP)-1, and keratinocyte chemoattractant (KC) were measured using the respective ELISA kits (Endogen, MA and R&D systems, MN).
Statistical Analysis
Statistical analyses were performed using the Microsoft Excel 2003 software package (Microsoft, Berkeley, CA). Statistical evaluations between two groups were compared with the Student’s t test, and any other statistical evaluations were compared using the one-way analysis of variance, followed by the Bonferroni post hoc test. Data are presented as the mean ± standard error (SE), with p < 0.05 considered statistically significant.
Results
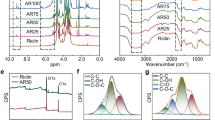
The Binding Strength of Photocrosslinkable Chitosan Hydrogel
UV rays are classified into three main groups; UV-A (400–315 nm), UV-B (315–280 nm), and UV-C (280–100 nm). Wavelengths below 300 nm damage a living tissue. While comparing the binding strength by using different UV wavelength, 356 nm was intentionally higher than 254 nm (Fig. 2). It shows the binding strength of insoluble chitosan gels between the two slices of ham. The change in binding strength by UV irradiation time increased time dependently until 90 s; in cases of further irradiation, binding strength decreased conversely (Fig. 2). When UV irradiation of 356 nm was applied for 90 s, the average binding strength was 30.5 g/cm2. When the irradiation time was short, the binding strength was weak; however, when the irradiation time was longer than 90 s, the gel lost flexibility and broke.
Survival Rate
For rats in which no procedures were provided, death occurred within 30 min due to hypovolemic shock (Fig. 3a). These animals developed decreased MAP (Fig. 3b). When we provided the hemostasis procedure (Fig. 1), survival rate increased. The hemostasis procedure with a wavelength of 356 nm had a survival rate of 90%. The hemostasis procedure with a wavelength of 254 nm had a survival rate of 75%. MAP decreased rapidly with severe hemorrhage, however, the MAP began to rise when it was possible to stop hemorrhage appropriately. After it stopped hemorrhage, it recovered up to 70% with a wavelength of 254 nm, and 80% with a wavelength of 356 nm in 1 day, and returned to normal in 3 days (Fig. 3). However, there was no statistical difference according to UV wavelength.
Effect of hemostasis as in Fig. 1. Moreover, comparison based on using different UV wavelengths of 356 nm (closed circle) or 254 nm (open circle). Survival rate after hemostasis (a), time-dependent change of MAP (b), RBC counts (c), hemoglobin concentrations (d), hematocrit levels (e), platelet counts (f), and WBC count (g) in rats undergoing hemostasis
Haematological Value and Serum Biochemical Constituents
We measured RBC count, hemoglobin, and hematocrit as markers of internal hemorrhage. RBC count, hematocrit, hemoglobin, and platelet levels were not significantly changed for 3 days (Figs. 3c–3f). No difference was observed according to the different UV wavelengths used. WBC count increased 1 day after the rats were treated (Fig. 3g). The effects of hemorrhage on liver function were also investigated. AST and ALT increased 1 day after the rats were treated, but decreased 3 days later (Figs. 4a, 4b). With a UV wavelength of 254 nm, the AST and ALT values were higher than those with a UV wavelength of 365 nm. Total protein levels showed no significant change for 3 days (Fig. 4c).
Biodegradation of Materials
Three days after carrying out hemostasis, when the hemorrhagic area was exposed, photocrosslinkable chitosan hydrogel did not retain its original form—a liquid residue of photocrosslinkable chitosan hydrogel and alginate calcium was observed (Fig. 5a). Twenty-eight days after carrying out hemostasis, when the hemorrhagic area was exposed, neither photocrosslinkable chitosan hydrogel nor alginate calcium was seen, a very small area of scar tissue was seen, but healthy subcutaneous tissue was recovered (Fig. 5b). Three days after carrying out hemostasis, several neutrophils and very few macrophages migrated around the liquid residue of photocrosslinkable chitosan hydrogel and alginate calcium (Figs. 5c–5f). Twenty-eight days after carrying out hemostasis, granulation tissue was forming, with a small residue of alginate (Figs. 5g, 5h).
The photograph of re-incision in hemorrhage area at 3 days (a) and 28 days (b) after hemostasis as in Fig. 1. Histological sections of H&E staining showing hemorrhage area at 3 days (c–f) and 28 days (g, h). c and d show several neutrophils and very few macrophages around the liquid residue of photocrosslinkable chitosan hydrogel. Black arrows show the liquid residue of photocrosslinkable chitosan hydrogel. Similarly, e and f show several neutrophils and very few macrophages around the calcium alginate. Black arrows show calcium alginate. g and h show dermal granulation tissue and very little residue of calcium alginate. Black arrows show residue of calcium alginate. Bar = 100 μm
Hemogram
Since the biodegradation of photocrosslinkable chitosan hydrogel after hemostasis were high, at first, we measured the differential count of leukocytes in blood. The number of neutrophils reached a high peak (60%) in 3 h after hemostasis, increased again 3 days later (Fig. 6a). To investigate the mechanism of biodegradation of photocrosslinkable chitosan hydrogel and alginate calcium, without hemorrhage, the differential count of leukocytes was measured after embedding each photocrosslinkable chitosan hydrogel and alginate calcium in the subcutaneous inguinal region. For rats in which photocrosslinkable chitosan hydrogel and alginate calcium were embedded, the number of leukocytes in the blood increased at 3 days (Fig. 6b). For rats in which photocrosslinkable chitosan hydrogel was embedded, the number of neutrophils reached a peak 3 h after embedding and decreased 3 days later (Fig. 6c). For rats in which alginate calcium was embedded, the number of neutrophils reached a peak 6 h after embedding and decreased 1 day later, but the number of neutrophils increased again 3 days later (Fig. 6d). In sham groups, the number of neutrophils reached a peak 6 h after treatment and decreased after that (Fig. 6e).
The time-dependent changes in hemogram after hemostasis as in Fig. 1(a). The time-dependent changes in hemogram when photocrosslinkable chitosan hydrogel (c), or calcium alginate (d) was implanted in the subcutaneous inguinal region. WBC count (b). The time-dependent changes in hemogram of sham (e)
The Secretion of Cytokine
The concentrations of interferon-γ, TNF-α, KC, and MCP-1 in serum were measured using ELISA. The concentration of TNF-α reached a peak 9 h after embedding each photocrosslinkable chitosan hydrogel and alginate calcium, and then was not detected at all. In the sham group, TNF-α was not detected at all (Fig. 7a). The concentration of KC (815 pg/mL) reached a peak 6 h after embedding photocrosslinkable chitosan hydrogel, and decreased to 25% of peak hour after 1 day. The concentration of KC (231 pg/mL) increased slowly 9 h after calcium alginate was implanted, and detected at the same level for 3 days afterward (Fig. 7b). The concentration of MCP-1 (21 ng/mL) reached a peak 3 days after embedding photocrosslinkable chitosan hydrogel. It showed no significant differences between the group embedded calcium alginate and sham (Fig. 7c). Interferon-γ was not detected at all in all groups.
The time-dependent change of concentrations of cytokines such as TNF-α (a) and chemokine such as KC (b) and MCP-1 (c) in serum when photocrosslinkable chitosan hydrogel or calcium alginate was implanted in the subcutaneous inguinal region. It did not detect INF-γ at all. *p < 0.05, **p < 0.01, ***p < 0.001, each vs. sham-operated group at the same time
Discussion
Chitin is a linear homopolymer of 1,4-β-linked N-acetyl-d-glucosamine, and chitosan is a partially N-deacetylated chitin. Polysaccharides, such as chitin and chitosan, are advantageous in their application as a wound dressing material.6 Both chitin and chitosan have several useful and advantageous biological properties in their application as a wound dressing, namely biocompatibility, biodegradability, hemostatic activity, antibacterial activity, and the ability to accelerate wound healing.10,23,25 It is reported that the hemostatic mechanism of chitosan may be independent of the classical coagulation cascade.26 During the process of hemostasis, activation of platelet adhesion and aggregation have an initial and critical role.3 Moreover, chitosan enhances platelet adhesion and aggregation accompanied by a significant increase in platelet Ca2+ and increased expression of glycoprotein IIb/IIIa on platelet membranes.7 In normal physiological conditions, platelets do not adhere to endothelial cells. However, in wounds, damaged vessel walls, or ruptured atherosclerotic plaque, platelet adherence to exposed subendothelial tissue is a critical step in hemostasis or thrombosis.
We previously reported a photocrosslinkable chitosan hydrogel containing both lactose moieties and photoreactive azide groups.12,20 UV irradiation of a photocrosslinkable chitosan hydrogel aqueous solution resulted in an insoluble hydrogel within 90 s. This hydrogel was able to firmly adhere two pieces of sliced ham together (Fig. 2), as well as effectively seal air leakage from pinholes in small intestinal, tracheal, and thoracic aortal tissues.21 In animal studies, the photocrosslinkable chitosan hydrogel also exhibited perfect sealing properties for artery hemostasis and provided air-sealing capacity in the lung.21 However, photocrosslinkable chitosan hydrogel is not able to stop severe hemorrhage. We noticed that the photocrosslinkable chitosan hydrogel was not able to bind tissue when there was fluid such as blood between the photocrosslinkable chitosan hydrogel and the tissue. In severe hemorrhage, this photocrosslinkable chitosan hydrogel has a low water absorption rate; the excess blood interfered with conjugation of the azide group and the amino group of proteins. Therefore, photocrosslinkable chitosan hydrogel alone cannot stop severe hemorrhage.
Alginate is an anionic polysaccharide comprising β-d-mannuronate and its C5 epimer, α-l-glucuronate. In extracted form, it absorbs water quickly; in water, it is capable of absorbing 200–300 times its own weight.9 Calcium alginate was first introduced as a wound dressing, and it is evaluated as a possible surgical hemostat. Calcium alginate dressings are designed to liberate calcium early in the acute phase to promote hemostasis through platelet aggregation. The importance of Ca2+ ion release in the hemostatic action of this material was demonstrated by studies on whole blood coagulation and platelet aggregation. In the process of platelet activation and aggregation, Ca2+ is one of the most important cellular second messengers that determine platelet action.8 Ca2+ ions activate coagulation by stimulating platelets and the clotting factors VII, IX, and X.8 Because alginate has a very high water absorption rate, it was used to compensate for the weak point of photocrosslinkable chitosan hydrogel. Based on these previous studies, we attempted to stop severe hemorrhage with a combination of photocrosslinkable chitosan hydrogel and calcium alginate (Fig. 1). As a conventional treatment we used chitosan-based gauze, CELOX (Seaberg Co. OR), on severe bleeding models. Time to complete hemostasis was about 10 min in the group of CELOX used vs. <3 min in the group of our materials used. When the wavelength was 356 nm, the survival rates (90%) were comparable (data not shown). Since we developed the hemostasis kit for use in battlefields or large-scale disaster sites, where many people injured and a brief period of treatment required, the difference of 7 min can be fatal in terms of getting medical care to the injured. Moreover, even if bleeding is temporarily arrested, there is a possibility of rebreeding when the blood pressure recovers or the body is moved. By sealing on whole hemorrhage area, the gel produces a rebreeding prevention effect. Since prolonged direct pressure to the area of injury in the neck and the face tends to make it hard to ensure adequate breathing. On the other hand, in disaster sites, not all medics would carry this UV irradiation apparatus. We tested to arrest severe bleeding in the open air with the sun’s UV rays (instead of the UV irradiation apparatus). It went successful when the sunlight was in the summer (data not shown).
We were surprised that photocrosslinkable chitosan hydrogel did not visually exist in the hemostasis area 3 days after hemostasis, and calcium alginate did not visually exist in the hemostasis area 28 days after hemostasis (Fig. 4). The mechanism of high biodegradation of photocrosslinkable chitosan hydrogel and calcium alginate was unspecified. It is important to investigate this mechanism for its clinical applications. Chitosan is a biodegradable molecule, and it has been reported that migrated neutrophils degrade chitosan molecules by secretion of lysozyme18 and chitotriosidase,19,29 in addition to phagocytosis of the molecules. When photocrosslinkable chitosan hydrogel was implanted, the ratio of the neutrophilic leukocytes in blood increased excessively at an early stage (Fig. 5b). Similarly, KC in serum increased excessively at an early stage (Fig. 6c). With control rats (Fig. 5d), when the body was incised, the neutrophil levels in blood increased 3 h after the operation. Chitosan could induce fibroblasts to secrete interleukin (IL)-8 and KC with neutrophil migration.17 Chitosan binds and activates complement proteins circulating in the blood, which can eventually cause neutrophil migration.4 Moreover, it was reported that neutrophil-like cells secreted the potent neutrophil chemokine IL-8, the same kind of CXC-chemokine as KC, when exposed to chitosan and IL-8 levels increased.22 It is assumed that the secretion of KC was promoted by exposing the neutrophils to chitosan, and neutrophil levels in the blood increased further. The biodegradation during the short time of only 3 days is not phagocytosis by macrophages, but also phagocytosis by neutrophils. Photocrosslinkable chitosan hydrogel was almost completely biodegraded by these actions in 3 days. When calcium alginate was implanted, neutrophil levels in the blood decreased temporarily 1 day after the implantation, although they increased again 3 days later. The neutrophils might be activated by secreted KC for the long term; although the amount of KC is less than that in implantation of the photocrosslinkable chitosan hydrogel, biodegradation will progress slowly through interactions of neutrophils and KC.
In this study, we developed a hemostatic kit (see Fig. 1) for severe hemorrhage using photocrosslinkable chitosan hydrogel and calcium alginate with a rat amputation model using the femoral artery and vein. This hemostatic mechanism used both whole blood coagulation and platelet aggregation by the action of calcium alginate and sealing effect of photocrosslinkable chitosan hydrogel. Moreover, if these materials remain within the body, they will be biodegraded in approximately 28 days by neutrophils. Further studies are needed to confirm these results and verify biodegradation of these materials in humans.
References
Acosta, J. A., J. C. Yang, R. J. Winchell, R. K. Simons, D. A. Fortlage, P. Hollingsworth-Fridlund, and D. B. Hoyt. Lethal injuries and time to death in a level I trauma center. J. Am. Coll. Surg. 186(5):528–533, 1998.
Alam, H. B., D. Burris, J. A. DaCorta, and P. Rhee. Hemorrhage control in the battlefield: role of new hemostatic agents. Mil. Med. 170(1):63–69, 2005.
Austin, S. K. Haemostasis. Medicine 37(3):133–136, 2009.
Benesch, J., and P. Tengvall. Blood protein adsorption onto chitosan. Biomaterials 23(12):2561–2568, 2002.
Champion, H. R., R. F. Bellamy, C. P. Roberts, and A. Leppaniemi. A profile of combat injury. J. Trauma 54(5 Suppl):S13–S19, 2003.
Chandy, T., and C. P. Sharma. Chitosan—as a biomaterial. Biomater. Artif. Cells Artif. Organs 18(1):1–24, 1990.
Chou, T. C., E. Fu, C. J. Wu, and J. H. Yeh. Chitosan enhances platelet adhesion and aggregation. Biochem. Biophys. Res. Commun. 302(3):480–483, 2003.
Duerbeck, N. B., D. G. Chaffin, and P. Coney. Platelet and hemorrhagic disorders associated with pregnancy: a review. Part I. Obstet. Gynecol. Surv. 52(9):575–584, 1997.
Gardner, R. L. Application of alginate gels to the study of Mammalian development. Methods Mol. Biol. 254:383–392, 2004.
Hirano, S. Chitin biotechnology applications. Biotechnol. Annu. Rev. 2:237–258, 1996.
Ishihara, M., K. Ono, M. Sato, K. Nakanishi, Y. Saito, H. Yura, T. Matsui, H. Hattori, M. Fujita, M. Kikuchi, and A. Kurita. Acceleration of wound contraction and healing with a photocrosslinkable chitosan hydrogel. Wound Repair Regener. 9(6):513–521, 2001.
Ishihara, M., K. Nakanishi, K. Ono, M. Sato, M. Kikuchi, Y. Saito, H. Yura, T. Matsui, H. Hattori, M. Uenoyama, and A. Kurita. Photocrosslinkable chitosan as a dressing for wound occlusion and accelerator in healing process. Biomaterials 23(3):833–840, 2002.
Kauvar, D. S., R. Lefering, and C. E. Wade. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J. Trauma 60(6 Suppl):S3–S11, 2006.
Kheirabadi, B. S., M. R. Scherer, J. S. Estep, M. A. Dubick, and J. B. Holcomb. Determination of efficacy of new hemostatic dressings in a model of extremity arterial hemorrhage in swine. J. Trauma 67(3):450–460, 2009.
Kheirabadi, B. S., J. W. Edens, I. B. Terrazas, J. S. Estep, H. G. Klemcke, M. A. Dubick, and J. B. Holcomb. Comparison of new hemostatic granules/powders with currently deployed hemostatic products in a lethal model of extremity arterial hemorrhage in swine. J. Trauma 66(2):316–326, 2009.
Kozen, B. G., S. J. Kircher, J. Henao, F. S. Godinez, and A. S. Johnson. An alternative hemostatic dressing: comparison of CELOX, HemCon, and QuikClot. Acad. Emerg. Med. 15(1):74–81, 2008.
Mori, T., M. Okumura, M. Matsuura, K. Ueno, S. Tokura, Y. Okamoto, S. Minami, and T. Fujinaga. Effects of chitin and its derivatives on the proliferation and cytokine production of fibroblasts in vitro. Biomaterials 18(13):947–951, 1997.
Muzzarelli, R. A. A. Biochemical significance of exogenous chitins and chitosans in animals and patients. Carbohydr. Polym. 20(1):7–16, 1993.
Nishimura, K., C. Ishihara, S. Ukei, S. Tokura, and I. Azuma. Stimulation of cytokine production in mice using deacetylated chitin. Vaccine 4(3):151–156, 1986.
Ono, K., Y. Saito, H. Yura, K. Ishikawa, A. Kurita, T. Akaike, and M. Ishihara. Photocrosslinkable chitosan as a biological adhesive. J. Biomed. Mater. Res. 49(2):289–295, 2000.
Ono, K., M. Ishihara, Y. Ozeki, H. Deguchi, M. Sato, Y. Saito, H. Yura, M. Sato, M. Kikuchi, A. Kurita, and T. Maehara. Experimental evaluation of photocrosslinkable chitosan as a biologic adhesive with surgical applications. Surgery 130(5):844–850, 2001.
Park, C. J., N. P. Gabrielson, D. W. Pack, R. D. Jamison, and A. J. W. Wagoner. The effect of chitosan on the migration of neutrophil-like HL60 cells, mediated by IL-8. Biomaterials 30(4):436–444, 2009.
Rao, S. B., and C. P. Sharman. Use of chitosan as a biomaterial: studies on its safety and hemostatic potential. J. Biomed. Mater. Res. 34(1):21–28, 1997.
Sauaia, A., F. A. Moore, E. E. Moore, K. S. Moser, R. Brennan, R. A. Read, and P. T. Pons. Epidemiology of trauma deaths: a reassessment. J. Trauma 38(2):185–193, 1995.
Shigemasa, Y., and S. Minami. Applications of chitin and chitosan for biomaterials. Biotechnol. Genet. Eng. Rev. 13:383–420, 1996.
Thatte, H. S., S. Zagarins, S. F. Khuri, and T. H. Fischer. Mechanisms of poly-N-acetyl glucosamine polymer-mediated hemostasis: platelet interactions. J. Trauma 57(1 Suppl):S13–S21, 2004.
Thomas, S. Alginate dressings in surgery and wound management: Part 1. J. Wound Care 9:56–60, 2000.
Thomas, S. Alginate dressings in surgery and wound management—Part 2. J. Wound Care 9:115–119, 2000.
van Eijk, M., C. P. van Roomen, G. H. Renkema, A. P. Bussink, L. Andrews, E. F. Blommaart, A. Sugar, A. J. Verhoeven, R. G. Boot, and J. M. Aerts. Characterization of human phagocyte-derived chitotriosidase, a component of innate immunity. Int. Immunol. 17(11):1505–1512, 2005.
Ward, K. R., M. H. Tiba, W. H. Holbert, C. R. Blocher, G. T. Draucker, E. K. Proffitt, G. L. Bowlin, R. R. Ivatury, and R. F. Diegelmann. Comparison of a new hemostatic agent to current combat hemostatic agents in a Swine model of lethal extremity arterial hemorrhage. J. Trauma 63(2):276–284, 2007.
Wedmore, I., J. G. McManus, A. E. Pusateri, and J. B. Holcomb. A special report on the chitosan-based hemostatic dressing: experience in current combat operations. J. Trauma 60(3):655–658, 2006.
Whang, H., W. Kirsch, Y. Zhu, C. Yang, and S. Hudson. Hemostatic agents derived from chitin and chitosan. J. Macromol. Sci. C Poly. Rev. 45(4):309–323, 2005.
Acknowledgments
We thank Yaizu Suisankagaku Industry Co., Ltd., for supplying photocrosslinkable chitosan hydrogel. We thank Ms. Ishida for proofreading. We thank Mr. Furukawa and Mr. Kuroda for their fresh advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Smadar Cohen oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Hattori, H., Amano, Y., Nogami, Y. et al. Hemostasis for Severe Hemorrhage with Photocrosslinkable Chitosan Hydrogel and Calcium Alginate. Ann Biomed Eng 38, 3724–3732 (2010). https://doi.org/10.1007/s10439-010-0121-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-010-0121-4