Abstract
Both autoregulation and CO2 reactivity are known to have significant effects on cerebral blood flow and thus on the transport of oxygen through the vasculature. In this paper, a previous model of the autoregulation of blood flow in the cerebral vasculature is expanded to include the dynamic behavior of oxygen transport through binding with hemoglobin. The model is used to predict the transfer functions for both oxyhemoglobin and deoxyhemoglobin in response to fluctuations in arterial blood pressure and arterial CO2 concentration. It is shown that only six additional nondimensional groups are required in addition to the five that were previously found to characterize the cerebral blood flow response. A resonant frequency in the pressure-oxyhemoglobin transfer function is found to occur in the region of 0.1 Hz, which is a frequency of considerable physiological interest. The model predictions are compared with results from the published literature of phase angle at this frequency, showing that the effects of changes in breathing rate can significantly alter the inferred phase dynamics between blood pressure and hemoglobin. The question of whether dynamic cerebral autoregulation is affected under conditions of stenosis or stroke is then examined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autoregulation has traditionally been taken to refer to the many and complex processes that attempt to maintain cerebral blood flow (CBF) within set limits despite changes in other physiological parameters such as arterial blood pressure (ABP).22 It is a well-established marker of brain health and is thought to be affected in a number of diseased states, including stroke,1,2 although this remains controversial.16 There is thus a very large literature examining the relationship between ABP and CBF, normally measured using Doppler Ultrasound over the middle cerebral artery to give cerebral blood flow velocity (CBFV). The relationship has been characterized in terms of physiological models, see, for example, Ursino et al.,21 or Payne,11 or through use of signal processing techniques, being conventionally expressed in terms of the impulse response (IR),6,8,10,23 or frequency response (FR),9,24 although nonlinear methods have also been used.5
However, CBFV, although representative of the supply of nutrients to and removal of waste products from the brain, is only an indirect measure of these transport processes. Using near infra-red spectroscopy (NIRS), see for example Elwell et al.,3 changes in oxyhemoglobin (O2Hb) and deoxyhemoglobin (HHb) can routinely be monitored noninvasively. These give quantitative measurements of oxygen transport and thus provide complementary information about cerebral vascular behavior, which could help to improve our understanding of autoregulation. However, this will require a greater understanding of the dynamics of oxygen transport, which can be partly achieved through the use of mathematical models, similar to those used to understand autoregulation.
Such models are highly valuable in interpreting experimental data, since such data are strongly influenced by changes in both CBF and cerebral blood volume (CBV), and O2Hb is found in both arterial and venous blood. All these variables are strongly influenced by ABP, but also by changes in other physiological parameters such as arterial CO2 partial pressure.10,13
We thus propose here a physiologically based model of hemoglobin transport, with both arterial and venous compartments, which can be used to interpret the response of O2Hb and HHb to changes in both ABP and arterial CO2 partial pressure. This model is based on a previously developed and validated model that describes the effects of autoregulation on the relationship between ABP and CBF. We then investigate its behavior in terms of its transfer functions, compare it to results from the literature and draw some conclusions about the role of autoregulation under conditions of both normal and reduced CBF.
Model Theory
The hemodynamic model used here is the same as that used previously,11,12 using the well-established equivalent electrical circuit model. Since we make no changes to this part of the model, we provide only a brief summary of the model here and refer the reader to Payne,11 for full details. The model presented previously comprises three compartments (arterial, capillary, and venous), the first and last of these behaving like conventional balloon models, the middle compartment being assumed to have fixed volume. The arterial compartment is further divided into ‘large’ and ‘small’ vessels, only the latter ones exhibiting autoregulation, which occurs by a simple feedback loop based on capillary flow acting to change arterial compliance with a gain and time constant (these being taken as representative of autoregulation level and speed). Using a simple electrical equivalent model, the cerebral vasculature is thus modeled by four resistors (large and small arteries and veins) and two capacitors (arterial and venous), the latter with nonlinear compliance. The model can be shown to exhibit all the experimentally derived features of both static and dynamic autoregulation and has also been used to include the effects of CO2 and neural activity using a single linearly additive feedback mechanism.
We now extend the model by incorporating the full hemoglobin transport equations. The nondimensional mass transport equation for venous deoxyhemoglobin can be written in the form:
where E denotes oxygen extraction fraction (OEF) and E o is baseline OEF. h denotes deoxyhemoglobin, v volume, and f in,v and f out,v are the venous inlet and outlet flows, respectively. The venous time constant is the baseline ratio of the venous volume to flow rate:
Throughout this paper, the subscripts “a” and “v” refer to the arterial and venous compartments, respectively and upper case variables denote absolute values, whereas lower case variables denote values as a fraction of their baseline values.
The nondimensional mass transport equation for fractional venous oxyhemoglobin, o v, can also be written:
and a similar equation for fractional arterial oxyhemoglobin, o a:
where the arterial time constant is defined in the same manner as the venous time constant and it is assumed that arterial blood is fully oxygenated. In healthy subjects this is likely to be a good approximation as the blood flowing into the brain is nearly fully saturated. The model could easily be adapted to include the effects of changes in arterial oxygen saturation, but this is not done here for simplicity. As a result of this assumption, deoxyhemoglobin is only found within the venous compartment.
It is also assumed here that the metabolic rate is constant: again changes in metabolism could easily be included, but for reasons of space this is not included here. This gives a direct relationship between changes in OEF and fractional CBF, q:
Note that the terminology Δq refers to changes in fractional CBF from its baseline value, i.e., \( \Updelta q = q - 1 = (Q - \bar{Q})/\bar{Q}. \) CBF is defined as the flow through the capillary compartment: we assume, as in Payne and Tarassenko,12 that the capillary compartment has fixed volume. Thus CBF is equal to both arterial outflow and venous inflow.
The model proposed by Payne11 only models the oxygen dynamics in the tissue compartment, which is tightly coupled to the capillary compartment. We initially included these dynamics within the model derivation outlined below, but it was found that these play a negligible role in the dynamics of O2Hb and HHb compared to the arterial and venous compartment dynamics. However, the resulting transfer functions were considerably more complicated. This compartment has therefore been omitted here as the focus is on providing an insight into the transfer function behavior.
The same procedure is now adopted as in Payne and Tarassenko,12 using a small signal analysis to linearize Eqs. (1), (3), and (4) about their baseline conditions, expressing the transfer functions relating changes in fractional hemoglobin to changes in fractional CBF in terms of the Laplace transform variable, s:
where an additional nondimensional parameter is introduced:
This additional parameter provides a measure of the relationship between flow and volume changes, which is an important part of the cerebral behavior, as will be discussed below.
The relationship between changes in oxyhemoglobin and deoxyhemoglobin and flow are thus strongly influenced by changes in both arterial and venous volumes. These relationships can be directly derived from the flow model presented by Payne,11 or re-arranged from the equations given in the appendix of Payne and Tarassenko,12 to give:
where an additional nondimensional ratio is introduced:
the remaining nondimensional groups being as given in Payne and Tarassenko.12 All the nondimensional groups used in this paper are given in Table 1, together with their definitions, physical explanations and numerical values (these being calculated as described below).
Total oxyhemoglobin is a volume weighted average of the arterial and venous oxyhemoglobin concentrations:
where in the steady state:
Equation (13) then becomes:
The equivalent expression for changes in deoxyhemoglobin is given by Eq. (6). Note that Eq. (6) has 2 poles and 0 zeros, whereas Eq. (15) has 3 poles and 3 zeros: the relative behaviors of oxyhemoglobin and deoxyhemoglobin will thus be significantly different.
Having derived the transfer functions in terms of changes in CBF, the full expressions for changes in oxyhemoglobin and deoxyhemoglobin in response to both changes in ABP and arterial CO2 concentration can be expressed. The transfer functions for changes in CBF in response to ABP, taken from Payne and Tarassenko,12 and arterial CO2 concentration, derived here from the equations given in Payne,11 are, respectively:
Note that the response to changes in CO2 in the model is assumed to be governed by a first-order low pass filter with gain \( G_{{{\text{CO}}_{2} }} \) and time constant \( \tau_{{{\text{CO}}_{2} }} \), very similar to the CBF response (for more details, the reader is referred to Payne11 and Ursino et al. 21). The overall transfer functions for the two outputs (oxyhemoglobin and deoxyhemoglobin) in terms of the two inputs (ABP and arterial CO2 concentration) can be computed simply by multiplying together the relevant transfer functions quoted above. In the next section, these transfer functions are considered in more detail.
Model Analysis
Before computing the transfer function numerically, the number and nature of the additional nondimensional groups are considered. In addition to the five nondimensional groups used to derive the pressure-flow transfer function (Eq. 16) there are an extra two nondimensional groups required to model the deoxyhemoglobin response (α v and τ v) and a further two parameters for the oxyhemoglobin response (β and E o) to changes in ABP. To investigate the responses to changes in arterial CO2 concentration, two more parameters need to be included (\( G_{{{\text{CO}}_{2} }} /G \) and \( \tau_{{{\text{CO}}_{2} }} \)). The four transfer functions are thus represented purely in terms of 11 nondimensional groups, giving a very compact system representation.
In Payne and Tarassenko,12 it was shown how values for four of the five nondimensional groups in Eq. (16) could be robustly estimated from the experimentally derived IR of the ABP–CBFV coupling. The fifth parameter had to be fixed, so it was decided there to set β 1 = 0.5 as a first approximation (the effects of changing this parameter were investigated in detail). The values thus derived are used here without alteration. The remaining six nondimensional groups in Table 1 are then calculated directly from the model parameters given in Payne.11
The numbers of poles and zeros in the four transfer functions are also briefly considered here, as this information provides an insight into their behavior, as well as an estimate of the number of degrees of freedom present. For deoxyhemoglobin, there are 4 poles and 1 zero for the ABP response and 5 poles and 2 zeros for the CO2 response (with many of these being the same); for oxyhemoglobin, there are 5 poles and 4 zeros for the ABP response and 6 poles and 5 zeros for the CO2 response. At high frequencies, the deoxyhemoglobin response to ABP will be at −270° phase relative to the dc response (there being 3 surplus poles), whereas the oxyhemoglobin response to ABP will be at −90° to the dc response (with 1 surplus pole).
There are a very large number of poles and zeros for the combined O2Hb and HHb behavior (significantly more than for CBFV, which has only 3 poles and 2 zeros). This makes the results more difficult to interpret, but does open up the possibility of extracting more information from the signals. The question of whether all the nondimensional groups could be estimated accurately from experimental measurements of the four impulse responses is an interesting one, but one that we do not pursue here since this is outside the scope of this paper.
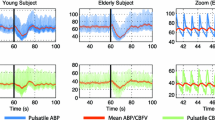
For the parameter values given in Table 1, the transfer functions relating fluctuations in oxyhemoglobin and deoxyhemoglobin to changes in ABP are shown in Fig. 1 in terms of magnitude and phase as functions of frequency. O2Hb shows resonant behavior at around 0.1 Hz, with a peak in gain at this frequency. This is not found in the HHb response. Note that this frequency comes simply from the model assumptions and the particular values of the model parameters used here; it is not fixed of itself. This is particularly interesting, since it implies that there may be significant power in the O2Hb signal but not the HHb signal at this frequency due to the resonant amplification of ABP power.
The behavior of oscillations at this frequency has been widely investigated, particularly in the context of vasomotion, whereby spontaneous oscillations in vascular tone are observed.7 This resonant frequency is lower than that found in the transfer functions for CBF and CBFV, as shown in Fig. 2. This frequency shifting is caused by the low-pass filtering nature of the oxyhemoglobin–CBF transfer function (Eq. 15). Calculating the resonant frequency is mathematically straightforward, but the resulting expression is very complicated and is thus not given here, since it provides no direct insight into the system behavior.
There is some phase shift at this frequency in both hemoglobin signals, relative to the steady state behavior, with phase decreasing significantly as frequency increases, heading toward −90° in both cases. HHb drops off more rapidly than O2Hb in magnitude with increasing frequency, passing through a frequency at which it is in phase with ABP. These transfer functions can also be interpreted in the context of the separate arterial and venous compartments, as shown in Figs. 3 (for arterial and venous volumes) and 4 (for arterial O2Hb and venous HHb), respectively. The −90° phase shift at high frequencies in both O2Hb and HHb is due physically to the fact that autoregulation is largely inoperative at high frequency and thus the dominant factor in the behavior is the 90° phase shift between flow and venous volume (simply due to the differential relationship between the two).
There is very significant resonance in both arterial and venous volumes at a frequency close to 0.1 Hz, both of which occur at close to zero phase angle (Fig. 3). Note that the resonance in arterial volume is very much larger than that in venous volume. The transfer function for arterial O2Hb is the same as for arterial volume (Eq. 8), thus also showing very significant resonance, whereas the venous O2Hb exhibits only very slight resonance. However, there is significant oscillation at low frequencies in the venous O2Hb, due to its higher compliance.
Discussion
There are few experimental data available in the literature with which to compare the model simulations for O2Hb and HHb, although there is more data for the ABP–CBFV phase shift. The primary source used here is the table of phase angles at 0.1 Hz for ABP–O2Hb (−24°) and ABP–HHb (−210°) given by Reinhard et al. 18 Note that the ABP–CBFV phase is also given, which will be examined in detail later. The values predicted by the model here are found to be −23° and −257°, respectively. The O2Hb phase is thus in very good agreement and the HHb phase in reasonable agreement: however, note that no optimization for the hemoglobin part of the model response has been performed here. Of particular importance is the fact that the ABP–O2Hb is negative and the ABP–HHb is more negative than −180°. In theory, it would be possible to optimize over the parameter space to remove two degrees of freedom from the model, in a similar manner to that performed by Payne and Tarassenko12: however, for reasons that will become obvious below, we simply provide a comparison between model and experiment at this point.
At very low frequencies, the HHb response to fluctuations in ABP tends toward:
and that of O2Hb toward:
The HHb response will be either positive or negative (i.e., in phase or out of phase) dependent solely upon whether α v is less than or greater than 1. Since α v is the ratio of two time constants, this means that if the time constant governing venous transit time \( (\bar{V}_{\text{v}} /F) \) is greater than the time constant governing venous outflow \( (R_{\text{lv}} \bar{C}_{\text{v}} ), \) then HHb will be out of phase with ABP at low frequencies. For the values quoted in Payne,11 the former is some 5–6 times greater.
The parameter α v, in fact, is also the scaling factor between fractional changes in venous flow and venous volume. It thus has significance beyond being simply the ratio between two time constants (although this additional interpretation lends further interest to its experimental value). For a simple compliant vessel, the ratio between changes in flow and volume must be at least 2 (resistance being inversely proportional to radius to the power 4 and volume being proportional to radius squared). In practice, it is bigger than 2: there has been a very large literature on this subject since the first study by Grubb et al.,4 who showed an exponent of 0.38 between CBV and CBF. Hence HHb is always likely to be out of phase with ABP at low frequencies.
Likewise, the O2Hb response will be out of phase with ABP at low frequencies if
Interestingly, this is strongly dependent upon the level of autoregulation present. At very high levels, the O2Hb will be out of phase with ABP, at very low levels, it will be in phase. For the values given in Table 1, Eq. (20) is not satisfied, which thus results in O2Hb being in phase. However, it is possible in subjects with overactive autoregulation for both O2Hb and HHb to be out of phase with ABP: for the values of parameters used here, α 2 would have to increase from 0.29 to 2.17. This is a very large increase, so is unlikely to be observed in practice without concurrent changes in other non-dimensional parameters. It can easily be shown that the venous O2Hb must always be in phase with ABP, but that arterial O2Hb will only be in phase if β 2 > α 2. It is therefore possible for the two compartments to be out of phase with each other: however, since the venous O2Hb component dominates, due to its much larger volume, it is very unlikely that total O2Hb will be out of phase with ABP. All of these results also hold directly for the responses to changes in arterial CO2 concentration.
The experimental results for phase angle quoted above were measured in a study where paced breathing was used at 6 breaths per minute (0.1 Hz). This increases the power at this frequency in the signals being recorded, enabling more robust measures of gain and phase to be measured. However, it also increases the power in the arterial CO2 concentration at this frequency, which may influence the inferred phase angle between ABP and O2Hb. It has previously been shown14 that not accounting for the effects of CO2 fluctuations can give rise to a significant error in the phase angle calculated between ABP and CBFV. Using the transfer functions derived here, it is possible to estimate the error that would be induced by CO2 fluctuations to see whether this is likely to be a significant effect.
It was shown by Peng et al. 14 that this error in inferred phase angle is
where
and A denotes the amplitude of the signal, and H and ϕ denote the gain and phase of the transfer functions, respectively, the subscripts “C” and “P” denoting the two inputs (CO2 and ABP) driving the output. The phase of the CO2 fluctuations relative to the ABP fluctuations is given by θ C. Taking the values for transfer function magnitude and phase predicted by the model and assuming that the fractional fluctuations in both ABP and CO2 are the same, as a first-order approximation, and in phase with each other, giving the smallest error, gives a phase error of 16.6°.
Since both O2Hb and HHb are directly driven by flow and volume changes, which are in turn driven by fluctuations in ABP and CO2, the compensation in phase angle due to variability in CO2 will be the same for both hemoglobin signals and for CBFV since it only directly affects the behavior of CBF: note that this makes the phase angle between the two hemoglobin signals a much more robust measure than either signal with respect to ABP in the presence of unmeasured variability.
Since there are no data in the literature to enable us to compare the effects of paced breathing on the O2Hb and HHb responses, we examine its effect on the ABP–CBFV response. As outlined above, changes in CO2 power at this frequency will have the same effect on the O2Hb and HHb responses as on the CBFV response. Any results derived for the ABP–CBFV phase angle will thus be identical for the ABP–O2Hb and the ABP–HHb responses.
There has been a series of studies by Reinhard and co-workers examining the phase angle at 0.1 Hz between ABP and CBFV in a range of subject groups and under conditions of both spontaneous and paced breathing. When examining unilateral stenosis subjects, for stenosis levels of 90–99% (43 subjects), the phase angle was found to be 20° and 39° on the ipsilateral and contralateral sides, respectively, for spontaneous breathing conditions, compared to 32° and 66° for paced breathing conditions; whereas for 100% stenosis levels (24 subjects), the corresponding phase angles were found to be 24° and 42° for spontaneous breathing and 31° and 48° for paced breathing conditions, respectively.15 They concluded that “Inter-method agreement [between the two methods] … is poor for phase,” the phase angle being consistently larger under conditions of paced breathing for both sides and for both groups, indicating both that the change in breathing conditions has a significant effect on the phase angle and that this effect is larger on the unaffected side than on the affected side.
In a similar study, performed solely under paced breathing conditions,18 a comparison between control subjects and subjects with stenosis found that the phase angle for ABP–CBFV was 64° in the controls, whereas it reduced to 34° for the ipsilateral side and remained stable at 67° on the contralateral side for the subjects with stenosis. These values are in good agreement with the results above for 90–99% stenosis levels. The corresponding results for ABP–O2Hb and ABP-HHb were −24° and −209° for the controls and −29° and −261° for the ipsilateral side and −13° and −205° for the contralateral side in the stenosis subjects. The phase angle was thus significantly altered in the ipsilateral side compared to the control group for both ABP–CBFV and ABP–HHb, but not for ABP–O2Hb. The changes in the O2Hb and HHb phase angles under conditions of stenosis are thus noticeably different, which cannot be explained purely in terms of the change in vascular reactivity. There are thus additional confounding factors present, which will need further investigation: however, given that this is the only available study in the literature, it is difficult to draw too many firm conclusions.
In another similar study, performed on stroke subjects under conditions of spontaneous breathing, it was found that there was no significant difference in ABP–CBFV phase between affected and unaffected sides, between controls and stroke subjects or between different days after treatment.16 It was thus concluded that there is no “major disturbance of dynamic autoregulation in acute ischemic stroke.”
There is a clear difference between the results from these studies when obtained under conditions of either spontaneous breathing or paced breathing. There is also an alteration in the difference between control subjects (or unaffected hemispheres) and affected hemispheres under the different conditions: the ABP–CBFV phase is significantly larger under conditions of paced breathing in control subjects and unaffected hemispheres than under spontaneous breathing, whereas for the affected sides, there is a much smaller difference under the two breathing conditions.
The static vascular reactivity to CO2 has also been measured for the same subject groups, enabling a comparison to be made between the ipsilateral and contralateral sides in stenosis.17 In the unaffected hemispheres, the CO2 reactivity was approximately 2.1%/mmHg, but on the affected sides it was around 1.2%/mmHg (based on 58 subjects with severe unilateral stenosis). This indicates that the reactivity declines by approximately 40% under conditions of severe stenosis. This drop in reactivity under conditions of reduced flow has been previously reported by Reivich,19 and the values quoted are in very close agreement with each other. The resulting phase error would then drop to 11.5°, compared to 16.6°, as calculated by Eq. (21), if it is assumed that this fractional drop in reactivity is the same at 0.1 Hz. The predicted alteration in inferred phase angle under different breathing conditions and the predicted change in this alteration when considering conditions of reduced vascular reactivity are both in good qualitative agreement with the experimental data outlined above.
Two other studies have been performed to examine the effects of stroke on dynamic cerebral autoregulation.1,2 However, it is difficult to compare these results with those above, since the autoregulation response is quantified in terms of changes in AutoRegulation Index (ARI), an index developed to measure autoregulation status on a scale of 0–9.20 Deriving the phase angle for comparison with the results above and the model proposed here is thus not simple. It should also be noted that the results obtained in these two studies were calculated using only short transient events in the signals, rather than the complete frequency response. We do not thus consider these results further.
Having investigated the phase relationships between ABP and O2Hb/HHb in the context of the CO2 response, the effects of varying the model parameters are now investigated, similar to the approach set out in Payne and Tarassenko,12 where the effects of changes in autoregulation gain and time constant were quantified in terms of the IR. Here, the effects of the same parameters are characterized in terms of the phase relationships at 0.1 Hz. The variation in phase angles at 0.1 Hz with fractional nondimensional gain and time constant are shown in Figs. 5 and 6, respectively.
Phase angle at 0.1 Hz changes by only a relatively small amount as autoregulation status changes: if feedback is abolished completely both the ABP–O2Hb and ABP–HHb phase angles decrease by only 29° and 25°, respectively. There is thus approximately a 2.5°–3° change in phase angle for every 10% drop in autoregulation feedback. The phase angle is less sensitive to changes in the feedback time constant, with a turning point: it would not be possible to infer the time constant from the phase angle. The change in phase angle at 0.1 Hz with variations in the feedback status would seem to indicate it is likely to be difficult to infer changes in autoregulation status solely by measuring this phase angle, unlike the way in which the phase angle between ABP and CBFV has been used to assess autoregulatory status. Note also that the phase angle between O2Hb and HHb, which is much less sensitive to fluctuations in CO2, is almost completely invariant with feedback gain. A further difficulty with using O2Hb and HHb as measures of autoregulation is that there are many more parameters controlling their behavior and changes in autoregulation gain are unlikely to be unaccompanied by other changes in physiological parameters.
Having investigated the effects of changes in both autoregulation status (through the model) and CO2 reactivity (through experimental data interpreted in the context of this model), we are finally able to consider the likely role of autoregulation impairment under conditions of stenosis or stroke. The effects of changes in autoregulation status on phase angle are likely to be of the order of only 10–20° for even large changes in autoregulation status, but changes in phase angle of similar or greater magnitude are observed experimentally when breathing patterns are altered from spontaneous to paced breathing. This leads us to propose the hypothesis that under conditions of stenosis or stroke, it is changes in vascular CO2 reactivity, which are well established as being caused by changes in flow, that are more significant, any changes in autoregulation status having a much smaller effect on the phase angle. It is thus likely to be difficult to infer any such changes in autoregulation status under differing physiological conditions.
However, it should be stressed that the scarcity of available data in the literature means that there are few results from which to draw such a substantive conclusion in the context of stroke, brain injury or brain trauma. Even the effects of aging on this phase angle are yet to be determined experimentally. Such studies will be extremely valuable in helping to assess the clinical potential of NIRS as a marker of changes in brain function and in helping to understand the underlying physiological processes and how they are altered under situations of physiological stress. It is likely, though, that multi-modal measurements of CBFV, O2Hb, and HHb, performed in response to a variety of different stimuli and interpreted in the context of a model such as the one proposed here, will open up the greatest possibility of interpreting cerebral dynamics fully.
Conclusions
Using an extended mathematical model of the cerebral vasculature, the transfer functions between both oxyhemoglobin and deoxyhemoglobin and both ABP and CO2 have been derived and calculated. The behavior in the region around 0.1 Hz appears to be the most promising for studying the response under different conditions: however, the use of paced breathing does seem to introduce a significant confounding factor into the analysis. This should be carefully compensated for when doing future studies and can easily be done using the approach set out here. There remains much more work to be performed, particularly experimentally, in terms of exploring how the phase relationships are affected by changes in autoregulation status and whether significant changes can be determined that could potentially be used to help diagnose and monitor brain injured patients.
References
Dawson, S. L., M. J. Blake, R. B. Panerai, and J. F. Potter. Dynamic but not static cerebral autoregulation is impaired in acute ischaemic stroke. Cerebrovasc. Dis. 10:126–132, 2000.
Eames, P. J., M. J. Blake, S. L. Dawson, R. B. Panerai, and J. F. Potter. Dynamic cerebral autoregulation and beat to beat blood pressure control are impaired in acute ischaemic stroke. J. Neurol. Neurosurg. Psychiatry 72:467–472, 2002.
Elwell, C. E., M. Cope, A. D. Edwards, J. S. Wyatt, D. T. Delpy, and E. O. R. Reynolds. Identification of adult cerebral hemodynamics by near-infrared spectroscopy. J. Appl. Physiol. 77:2753–2760, 1994.
Grubb, R. L., M. E. Raichle, J. O. Eichling, and M. M. Ter-Pogossian. The effects of changes in PaCO2 on cerebral volume, blood flow and vascular mean transit time. Stroke 5:630, 1974.
Mitsis, G. D., and V. Z. Marmarelis. Modeling of nonlinear physiological systems with fast and slow dynamics: I. Methodology. Ann. Biomed. Eng. 30:272–281, 2002.
Mitsis, G. D., R. Zhang, B. D. Levine, and V. Z. Marmarelis. Modeling of nonlinear physiological systems with fast and slow dynamics: II. Application to cerebral autoregulation. Ann. Biomed. Eng. 30:555–565, 2002.
Nilsson, H., and H. Aalkjaer. Vasomotion: mechanisms and physiological importance. Mol. Interv. 3:79–89, 2003.
Panerai, R. B. System identification of human cerebral blood flow regulatory mechanisms. Cardiovasc. Eng. 4:59–71, 2004.
Panerai, R. B., S. L. Dawson, and J. F. Potter. Linear and nonlinear analysis of human dynamic cerebral autoregulation. Am. J. Physiol. 277:H1089–H1099, 1999.
Panerai, R. B., D. M. Simpson, S. T. Deverson, P. Mahony, P. Hayes, and D. H. Evans. Multivariate dynamic analysis of cerebral blood flow regulation in humans. IEEE Trans. Biomed. Eng. 47:419–423, 2000.
Payne, S. J. A model of the interaction between autoregulation and neural activation in the brain. Math. Biosci. 204:260–281, 2006.
Payne, S. J., and L. Tarassenko. Combined transfer function analysis and modelling of cerebral autoregulation. Ann. Biomed. Eng. 34:847–858, 2006.
Peng, T., A. B. Rowley, P. N. Ainslie, M. J. Poulin, and S. J. Payne. Multivariate system identification for cerebral autoregulation. Ann. Biomed. Eng. 36:308–320, 2008.
Peng, T., A. B. Rowley, P. N. Ainslie, M. J. Poulin, and S. J. Payne. Wavelet phase synchronization analysis of cerebral blood flow autoregulation. IEEE Trans. Biomed. Eng., in press
Reinhard, M., T. Muller, B. Guschlbauer, J. Timmer, and A. Hetzel. Transfer function analysis for clinical evaluation of dynamic cerebral autoregulation—a comparison between spontaneous and respiratory-induced oscillations. Physiol. Meas. 24:27–43, 2003.
Reinhard, M., M. Roth, B. Guschlbauer, A. Harloff, J. Timmer, M. Czosnyka, and A. Hetzel. Dynamic cerebral autoregulation in acute ischemic stroke assessed from spontaneous blood pressure fluctuations. Stroke 36:1684–1689, 2005.
Reinhard, M., M. Roth, T. Muller, B. Guschlbauer, J. Timmer, M. Czosnyka, and A. Hetzel. Effect of carotid endarterectomy or stenting on impairment of dynamic cerebral autoregulation. Stroke 35:1381–1387, 2004.
Reinhard, M., E. Wehrle-Wieland, D. Grabiak, M. Roth, B. Guschlbauer, J. Timmer, C. Weiller, and A. Hetzel. Oscillatory cerebral hemodynamics—the macro- vs. microvascular level. J. Neurol. Sci. 250:103–109, 2006.
Reivich, M. Arterial PCO2 and cerebral hemodynamics. Am. J. Physiol. 206:25–35, 1964.
Tiecks, F. P., A. M. Lam, R. Aaslid, and D. W. Newell. Comparison of static and dynamic cerebral autoregulatory measurements. Stroke 26:1014–1019, 1995.
Ursino, M., A. Ter Minassian, C. A. Lodi, and L. Beydon. Cerebral hemodynamics during arterial and CO2 pressure changes: in vivo prediction by a mathematical model. Am. J. Physiol. 279:H2439–H2455, 2000.
Vespa, P. What is the optimal threshold for cerebral perfusion pressure following traumatic brain injury? Neurosurg Focus 15(6):E4, 2003.
Zhang, R., J. H. Zuckerman, C. A. Giller, and B. D. Levine. Transfer function analysis of dynamic cerebral autoregulation in humans. Am. J. Physiol. 274:H233–H241, 1998.
Zhang, R., J. H. Zuckerman, and B. D. Levine. Spontaneous fluctuations in cerebral blood flow: insights from extended duration recordings in humans. Am. J. Physiol. 278:H1848–H1855, 2000.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Payne, S.J., Selb, J. & Boas, D.A. Effects of Autoregulation and CO2 Reactivity on Cerebral Oxygen Transport. Ann Biomed Eng 37, 2288–2298 (2009). https://doi.org/10.1007/s10439-009-9763-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-009-9763-5