Abstract
Mouse models of Marfan Syndrome (MFS) provide insight into the type and extent of vascular abnormalities manifested in this disease. Inclusion of the mgR mutation causes the otherwise normal extracellular matrix glycoprotein fibrillin-1 to be under-expressed at 15–25% of its normal level, a condition seen in MFS. Aortas in patients with MFS are generally less distensible and may experience dissecting aneurysms that lead to premature death, yet little is known about effects on other large arteries. In this study, common carotid arteries from mice heterozygous (R/+) and homozygous (R/R) for the mgR mutation were studied under biaxial loading and compared to results from wild-type controls (+/+). Carotids from +/+ and R/+ mice exhibited similar biomechanical behaviors whereas those from R/R mice were slightly stiffer in the circumferential direction while dramatically different in the axial direction. That is, R/R carotids were stiffer axially and had lower in vivo axial prestretches. Biaxial stress–stretch data were fit with a four-fiber family constitutive model. The fitted data yielded a lower value of an isotropic parameter for the R/R carotids, which reflects a compromised elastin-dominated amorphous matrix. Overall, it appeared that changes in axial mechanical properties afforded R/R carotids a means to compensate, at least early in maturity (9 weeks of age), for the loss of an important structural constituent as they attempted to maintain structural integrity in response to normal mean arterial pressures and thereby maintain mechanical homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Marfan syndrome (MFS), affecting approximately one out of every 5,000 people,37 is characterized by abnormal bone growth, lens dislocation, and aortic dilation and dissection. This disease results from a variety of mutations in the gene coding for the elastin-associated extracellular matrix glycoprotein fibrillin-1 (FBN1) and spans a wide range of phenotypes.42 Sherratt et al.46 suggest that fibrillin microfibrils act as stiff reinforcing filaments in elastic fibers, possibly limiting the extension of elastin7 and protecting these fibers from fatigue-like damage. Recent studies20,38 show further that these microfibrils are biologically active and play a role in regulating transforming growth factor—β, also a key modulator of extracellular matrix integrity. FBN1 is thus important to extracellular matrix and overall tissue homeostasis.20,38,40
Mice homozygous for the mgR mutation (R/R) produce normal FBN1 at levels 15–25% of normal40 and develop Marfan-like vascular abnormalities. These mice are born with apparently normal vascular elastic lamina, but develop focal calcifications as early as 6 weeks of age.40 As the animal continues to age, one observes a breakdown of elastic lamina within the media as well as an increased synthetic phenotype among the smooth muscle cells, infiltration of inflammatory cells, and increased matrix metalloproteinase levels, which together contribute to subsequent aortic failure.6,9 Due to the devastating effects of aortic dilatation and dissection, the aorta has been studied extensively in MFS. Ultrasound measurements by Jeremy et al.28 suggest that ascending aortas in MFS patients are substantially stiffer than those of age-matched controls. Similar results were found by Marque et al.34 in 3- to 5-month-old R/R mice. Using magnetic resonance imaging, Groenink et al.19 measured decreased distensibility both in the aortic arch and near the aortic bifurcation, as well as increased pulse wave velocities along the aorta, thus indicating that the entire vessel stiffens in MFS.
As Marfan patients live longer due to improved treatment, they will likely face many other vascular complications that affect the normal population, including hypertension and atherosclerosis. Although aortas in both human patients and animal models of MFS are first stiffer then weaker than controls,18,28,34 there has been little research on other arteries. It is imperative, therefore, to gather biomechanical data from the entire Marfan vasculature so that clinicians can better understand other possible vascular complications in Marfan patients and develop appropriate methods of treatment. This paper compares the biaxial mechanical response (cyclic pressure–diameter and axial force–length) of common carotid arteries from wild-type mice with those from mice heterozygous or homozygous for the mgR mutation, a commonly used mouse model of MFS.
Materials and Methods
Vessel Isolation
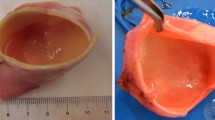
A breeding pair of mice heterozygous for mgR, obtained from Dr. Francesco Ramirez, was used to produce wild type (+/+), heterozygous (R/+), and homozygous (R/R) mice for study. All animal use was approved by the Texas A&M University Institutional Animal Care and Use Committee (IACUC). Briefly, 8- to 14-week-old male mice were restrained by holding the tail with one hand and firmly grabbing the skin behind the neck (scruffing) with the index finger and thumb of the other hand. The mice were then anesthetized using an intraperitoneal injection of sodium pentobarbital (125 mg/kg) and, while the mouse was deeply under, an incision was made from the chest to the neck to expose the thoracic cavity and neck around the esophagus. Both common carotid arteries were excised from near the aortic arch to the carotid bifurcation. Vessels were cleaned of excess perivascular tissue, then placed in warm media, cannulated on 300 μm diameter custom-pulled glass pipettes, and secured using braided 6-0 silk suture.
Mechanical Testing
Cannulated vessels were mounted within a circulating adventitial bath contained within an isolated, temperature controlled chamber. The bath consisted of Dulbecco’s Modified Eagle’s Media, containing 2% heat inactivated fetal bovine serum, 2% l-glutamine, 1000 units/L penicillin, and 1000 g/L streptomycin. A steady flow of 95% air/5% CO2 controlled media pH. A peristaltic pump separately provided adventitial and luminal flow of media, with lumen pressure controlled independently by regulating the air–CO2 pressure on the surface of a media reservoir. A side-mounted, calibrated CCD camera measured vessel diameter while precision stepper motors controlled vessel length. A force transducer was connected to the distal cannula and measured the applied axial force. Further detail on the biaxial testing device, control capabilities, and resolutions can be found in Gleason et al.14
Unloaded dimensions were measured interactively by decreasing the length of an initially stretched vessel at zero pressure until it started to bend (~5 mm), as indicated by the initiation of a crease in the vessel wall. Circumferential and axial stretches were calculated based on these unloaded dimensions. The vessel was then stretched to its predetermined in vivo value \( \lambda_{\text{z}}^{\text{iv}} \) (see below) and preconditioned through three cycles of pressurization from 0 to 160 mmHg (+/+ and R/+) or from 0 to 140 mmHg (R/R) to minimize hysteresis. Pilot studies revealed dramatically increased smooth muscle cell damage/dysfunction in R/R carotids tested to 160 mmHg, hence they were subsequently preconditioned and tested up to 140 mmHg so that all vessels retained “normal” functionality. The computer then performed a pre-programmed routine to achieve various axial stretch and pressure set-points. Wall volume remains nearly constant over short periods (i.e., without growth and remodeling), thus inner radius r i and thus wall thickness h were calculated using incompressibility via11, 14, 24
where \( \bar{V} \) is the mean wall volume, \( \ell \) the current length between the sutures, and r a the outer radius. Wall volume was estimated based on 12–15 interactive measurements of inner and outer radius at multiple static pressures and lengths. Equation (1) thus allowed inner radius to be determined at any pressure and stretch based on known \( \bar{V} \) and \( \ell \) as well as on-line measurements of outer radius via an edge detection algorithm in LabView.
Mechanical testing consisted of cycling pressure from 0 to 160 mmHg (+/+, R/+) or 0 to 140 mmHg (R/R) twice at each of three fixed axial stretches \( \lambda_{\text{z}}^{{ + / + ,{\text{R}}/ + }} \) = 1.65, 1.75, 1.85 and \( \lambda_{\text{z}}^{\text{R/R}} \) = 1.55, 1.65, 1.70; these different values of stretch allowed each vessel to be tested above, near, and below its in vivo value. Next, the program tested the axial force–length response at each of three fixed pressures (P = 60, 100, 140, or 160 mmHg) while the axial load was varied twice from 0 to 8.8 mN (0.9 g). The mechanical results at a fixed pressure of 140 mmHg were interpolated for +/+ and R/+ data using a three-point interpolation from the 60, 100, and 160 mmHg tests. Intersections of axial force–stretch curves at three values of fixed pressure estimate the in vivo axial stretch.5,10,21,24,48,50 This stretch may help optimize the vessel against buckling during normal movement and is a crucial characteristic to compare vessels in vitro.5 Based on the aforementioned pilot results, and resultant setting of R/R set-points for stretch and peak pressures lower than those for +/+ and R/+ carotids, group-to-group comparisons were based on interpolations across a range of axial stretches with the only common stretch set-point at λ z = 1.65.
Following mechanical testing, we evaluated both endothelial and smooth muscle functionality. Phenylephrine (10−5 M) was added to the adventitial bath and the diameter was allowed to equilibrate for 15 (+/+, R/+) or 30 (R/R) minutes to determine smooth muscle contractility. The goal was to elicit maximal contractility independent of rate of contraction, thus allowing either 15 or 30 min for equilibration was irrelevant provided the vessel reached a steady state contraction after adding PE. The R/R vessels were generally less responsive to phenylephrine, possibly due to alterations in cell phenotype as described in Bunton et al.6 Nevertheless, a 30% constriction was considered functional for all groups. Next carbamycholine chloride (10−5 M) was added to test endothelial-dependent smooth muscle relaxation and all vessels were allowed to equilibrate for 15 min. A 10% dilation was considered functional for all groups. Sodium nitroprusside (10−4 M), which tests endothelial-independent relaxation, was then added to the bath and all vessels were allowed to equilibrate again for 15 min. Finally, the media was replaced with a Hank’s Balanced Salt Solution (HBSS) without calcium and magnesium but containing sodium nitroprusside (10−5 M) and EGTA (2 × 10−3 M) to ensure full smooth muscle relaxation (i.e., to render the vessel passive or fully dilated). Mechanical testing described above was repeated for the passive state.
Basic information on the animals used for testing is shown in Table 1. Note that no two carotids were tested from the same animal and the only statistically significant difference was between the weights of the heterozygous (R/+) and homozygous (R/R) mice. Mice from the R/R group were tested at an earlier age to avoid aortic aneurysm related deaths found to occur at or after 13 weeks. Despite the apparent difference in ages, mean ages did not differ significantly among the three genotypes. Furthermore, within the narrow range of ages considered, statistical analysis revealed that age did not significantly affect mechanical behavior, a result confirmed by independently testing an additional +/+ carotid artery at 8 weeks of age (data not shown).
Data Analysis
Stress is an important metric in arterial biomechanics because it correlates well with many aspects of growth and remodeling.3,27 Mean circumferential and axial Cauchy wall stresses were estimated by12,16,24
where P is the transmural pressure, r a, r i the deformed inner and outer radii, respectively, and f T the measured axial force. Circumferential stretch ratios were calculated at the mid-wall, where \( r_{\text{mid}} = \left( {r_{\text{a}} + r_{\text{i}} } \right)/2. \) Basal tone refers to an arterial caliber with smooth muscle contraction or relaxation dictated by hemodynamic and environmental cues. The basal (b) or passive (p) circumferential \( \lambda_{\theta }^{\text{b/p}} , \) axial \( \lambda_{\text{z}}^{\text{b/p}} , \) and radial \( \lambda_{\text{r}}^{\text{b/p}} \) stretches were calculated from unloaded basal and loaded basal and passive states via
where ρ and L are radii and axial length in the unloaded basal configuration, respectively.
Four-Fiber Family Model
Constitutive modeling can be used to describe and predict the stress response of tissue. A 2-D representation of Cauchy stress in the circumferential and axial directions is15
where \( \sigma_{\text{r}} \ll \sigma_{\theta } \) and \( \sigma_{\text{r}} \ll \sigma_{\text{z}} \) and W is the strain energy function. We employed a structurally motivated strain energy function that incorporates the isotropic contributions of the elastin-dominated amorphous matrix and anisotropic contributions of families of oriented collagen fibers (and possibly circumferentially oriented passive smooth muscle). Specifically, consider a four-fiber family model of the form23
where c, \( c_{1}^{k} , \) and \( c_{2}^{k} \) are material parameters that must be determined via nonlinear regression and k represents a fiber family. I 1 is the first principal invariant of the right Cauchy–Green tensor such that \( I_{1} = \lambda_{\theta }^{2} + \lambda_{\text{z}}^{2} + \lambda_{\text{r}}^{2} \) and λ k is the stretch of the kth fiber family, determined by
where \( \alpha_{\text{o}}^{k} \) is the angle of the kth fiber family with respect to the axial direction of the blood vessel in a reference (unloaded) configuration. This constitutive relation has demonstrated its effectiveness in describing stress-strain behaviors of healthy and diseased mouse carotid arteries.13
To find values of the eight unknown parameters (c, \( c_{1}^{1} , \) \( c_{2}^{1} , \) \( c_{1}^{2} , \) \( c_{2}^{2} , \) \( c_{1}^{3} , \) \( c_{2}^{3} , \) \( \alpha_{\text{o}} \)), we performed a constrained multi-dimensional nonlinear minimization (simplex method using a modification of the MATLAB routine fminsearch with upper and lower bounds) using biaxial stress–stretch data for the wild-type (+/+), heterozygous (R/+), and homozygous (R/R) carotid arteries. An objective function was defined to minimize the error,23,24
where N is the number of data points within each set (typically ~200 points), including the multiple pressure–diameter and axial force–length protocols. The experimental (exp) stress represents the mean wall stress in circumferential and axial directions defined by Eqs. (3)–(4) whereas the model (mod) stress is determined by Eqs. (8)–(11). Initial guesses for the minimization were (c, \( c_{1}^{1} , \) \( c_{2}^{1} , \) \( c_{1}^{2} , \) \( c_{2}^{2} , \) \( c_{1}^{3} , \) \( c_{2}^{3} , \) α o) = (1 kPa, 1 kPa, 1, 1 kPa, 1, 1 kPa, 1, 45 deg), noting that actual computations were performed in radians. A convergence criterion tolerance was set at 10−10.
Statistical Analysis
The built-in MATLAB function for multi-way analysis of variance, ANOVAN, was used in conjunction with a “Bonferroni” post-hoc analysis from the function MULTCOMPARE to assess statistical differences among the three genotypes. A value of p < 0.05 was considered significant and denoted within some figures by an arrow (→) pointing in the direction of continued statistical significance. The symbol (*) denotes statistically significant differences between +/+ and R/R, (**) for differences between R/+ and R/R, or (***) for differences between +/+ and R/+. Results are typically presented as mean ± the standard deviation (SD) from the mean.
Results
Axial Stretch and Force Responses
Averaged, basal, in vivo axial stretches for wild-type (+/+), heterozygous (R/+), and homozygous (R/R) mice were \( \lambda_{\text{z}}^{\text{iv}} \) = 1.71 ± 0.018, 1.72 ± 0.017, and 1.63 ± 0.018, respectively (Figs. 1a–1c; Table 2), and passive axial stretches were similarly \( \lambda_{\text{z}}^{\text{p,iv}} \) = 1.72 ± 0.017, 1.73 ± 0.020, and 1.64 ± 0.015 (i.e., there was no statistical difference between basal and passive values). Note, therefore, that the in vivo axial stretch for R/R mice was significantly less than that for both +/+ and R/+ mice at p < 0.05. Basal values of the associated in vivo force for +/+, R/+, and R/R mice were f T = 3.63 ± 0.231, 3.34 ± 0.216, and 2.85 ± 0.231 mN, respectively (Figs. 1a–1c), and passive values of axial force were \( f_{\text{T}}^{\text{p}} \) = 3.43 ± 0.211, 3.67 ± 0.250, and 2.40 ± 0.186 mN. Again, the in vivo value for R/R was statistically less than that for +/+ and R/+ at p < 0.05, which were not statistically different from one another (p > 0.05). Recall from Table 2 that the individual in vivo arterial cross-sectional areas at 100 mmHg were not significantly different among genotypes.
Averaged axial force–stretch data with basal smooth muscle tone at fixed pressures of 60, 100, and 140 for +/+, R/+, and R/R. Note that a cross-over point/intersection estimates the in vivo axial stretch (vertical lines),5,48 which was taken here to be the mean of the values determined from the three different comparisons possible (e.g., 60–100, 60–140, and 100–140 mmHg)
Averaged axial force–pressure data (Figs. 2a–2b) show that the in vivo estimation for all genotypes (+/+, R/+, R/R) yielded a relatively flat relation at \( \lambda_{\text{z}}^{\text{iv}} \) as expected48 while an axial stretch above or below the in vivo value yielded an increasing or decreasing force as pressure increased. These data indicate that +/+ and R/+ carotids are similar mechanically in the axial direction (Figs. 2a, 2b). That the magnitude of the in vivo axial force was lower for R/R (2.85 ± 0.231 mN) compared to both +/+ and R/+ vessels (3.63–3.34 mN) is also seen easily in Fig. 2. Axial force was not significantly influenced by smooth muscle contractility presumably because the cells are oriented primarily in the circumferential direction.
Averaged axial force–pressure results at (a) common fixed axial stretch of \( \lambda_{\text{z}} = 1.65, \) and (b) individual in vivo axial stretches: \( \lambda_{\text{z}}^{\text{iv}} = 1.72 \) for +/+ (—), \( \lambda_{\text{z}}^{\text{iv}} = 1.71 \) for R/+ (- - -), and \( \lambda_{\text{z}}^{\text{iv}} = 1.63 \) for R/R (····). The → indicates the direction of continued statistical difference for the R/R relative to +/+ (*) or R/+ (**) at p < 0.05, all other comparisons being not statistically significant at this confidence level
Averaged pressure–diameter results at individual in vivo axial stretches for (a) basal smooth muscle tone and (b) passive smooth muscle for each genotype: +/+ (—), R/+ (- - -), and R/R (····). All comparisons between genotypes, for both basal and passive groups, are not statistically significant at the p < 0.05 confidence level
Pressure and Diameter Responses
Cyclic pressurization at a common axial stretch of 1.65 allowed direct numerical comparison of responses among the three genotypes. Further testing was performed at stretches above and below the individual in vivo (\( \lambda_{\text{z}}^{\text{iv}} \)) stretches, with the behavior interpolated at \( \lambda_{\text{z}}^{\text{iv}} \) (not known a priori); see Supplemental Figs. 1 and 2. Recall that all fixed pressure and axial stretch testing was performed with basal, then no (i.e., a passive or fully dilated vessel) smooth muscle tone. Figure 3a shows characteristic changes in diameter as pressure increased at basal tone. The R/R vessels appeared to be distended or dilated slightly compared to +/+ and R/+, but statistical analysis revealed no difference. The passive increase in diameter with increased pressurization (Fig. 3b) was slightly greater in R/+ and R/R than in +/+, perhaps suggesting a slightly greater basal tone in R/+ than R/R (cf. Fig. 3a), but again these differences did not reach significance as seen below. Geometric comparisons among the three genotypes also revealed marked similarities (Table 2) except for the aforementioned lower value of the in vivo axial stretch in the R/R carotids.
Stress
Altered states of stress may be initiators or indicators of disease. Although differences between groups did not reach statistical significance for the circumferential direction, the stress–stretch curves (Fig. 4) for R/+ carotids were shifted slightly to the right (less stiff) compared to those for +/+. As expected, smooth muscle relaxation caused vessel dilation at any given pressure, causing distinct shifts in pressure–diameter (cf. Fig. 3b) and corresponding σ θ –λ θ plots (Figs. 4a–4c) relative to basal responses. Carotids from +/+ and R/+ mice exhibited similar axial stress responses (Figs. 5a–5c). A visual comparison of responses suggests that R/R vessels experienced greater values of axial stress for comparable axial stretches. Similarities in variables used to calculate stress (Eqs. 3–4) can be seen in Table 2.
Averaged passive circumferential stress–stretch responses at multiple fixed axial stretches as well as passive and basal responses interpolated for the individual in vivo axial stretch (—). All comparisons between genotypes at \( \lambda_{\text{z}}^{\text{iv}} \) are not statistically significant at this confidence level
Averaged axial stress–stretch results for basal smooth muscle tone at fixed pressures of 60, 100, and 140 mmHg for +/+, R/+, and R/R carotid arteries. The → indicates the direction of continued statistical difference for R/R relative to +/+ (*) or R/+ (**) at p < 0.05. All other comparisons between genotypes are not statistically significant at this confidence level
A representative dose–response curve for one +/+ vessel and all vasoreactants is shown in Fig. 6A. Phenylephrine (PE: 10−5 M) was added to the otherwise basal vessel at point (a) to test smooth muscle contractility and point (b) represents the vessel in its “maximum” contractile state. Carbamycholine chloride (CCh: 10−5 M) was added at point (b) to test endothelial-dependent smooth muscle relaxation: point (c). As nitric oxide was depleted, the diameter returned toward its contracted state: points (d). Sodium nitroprusside (SNP: 10−4 M) was then added to the bath to elicit endothelial-independent smooth muscle relaxation at points (d)–(e). The media was replaced with Hank’s Balanced Salt Solution (HBSS) without calcium or magnesium, but containing sodium nitroprusside (10−5 M) and EGTA (2 × 10−3 M) to ensure full smooth muscle relaxation by depleting intracellular and extracellular stores of calcium at point (e). The gap in diameter data between points (e) and (f) occurred when exchanging media with HBSS. Mean values of circumferential stretch for each genotype (+/+, R/+, and R/R) at each smooth muscle cell functional reference point (a)–(f) can been seen in Fig. 6B. By comparing the fully passive state (f) to the basal one (a), one observes that the in vitro “basal” state of all vessels had little smooth muscle tone. Circumferential stretch changed less for the R/R carotid than for +/+ or R/+ for all levels of smooth muscle activation, but differences did not reach significance.
(A) Representative diameter dose–response for a +/+ carotid, relative to basal (a), before and after the addition of (b) Phenylephrine (PE) at 10−5 M, (c–d) Carbamycholine chloride (CCh) at 10−5 M, (e) Sodium nitroprusside (SNP) at 10−4 M, and (f) calcium and magnesium-free Hank’s Balanced Salt Solution (HBSS) containing sodium nitroprusside (10−5 M) and EGTA (2 × 10−3 M), with maximally contracted and fully relaxed states at (b) and (f), respectively. (B) Steady state diameter dose–responses for +/+, R/+, and R/R. Error bars represent standard deviation from the mean and all state-specific comparisons among genotypes are not statistically significant at p < 0.05
Four-Fiber Family Model
The unknown parameters in the four-fiber family strain energy function (Eqs. 10–11) were determined via minimization of the objective (error) function described by Eq. (12) for each vessel in the passive state. Fiber families 1 and 2 were defined to be primarily axial, with \( \alpha_{\text{o}}^{1} = 0 \) deg, and circumferential, with \( \alpha_{\text{o}}^{2} = 90 \) deg. Furthermore, for the diagonal families, \( \alpha_{\text{o}}^{4} = - \alpha_{\text{o}}^{3} \) was represented by one angle α o. Results of the parameter estimation for the +/+, R/+, and R/R carotids can be seen in Table 3; note the 8- to 9-fold lower value of the parameter c, associated with the elastin-dominated matrix, for the R/R compared with the +/+ and R/+ carotids. Associated illustrative predicted pressure–diameter and force–pressure results are compared to experimental data for one mouse from each of two data sets (Figs. 7a–7b). An illustrative fit to stress-stretch data can be seen in Supplemental Fig. 3.
Predicted (*) and experimentally measured (○) (a) Pressure–circumferential stretch responses for passive +/+ mouse #3 (with c = 24.292 kPa, \( c_{1}^{1} = 0.469 \) kPa, \( c_{2}^{1} = 0.493 \), \( c_{1}^{2} = 1.873 \) kPa, \( c_{2}^{2} = 0.278 \), \( c_{1}^{3} = 0.021 \) kPa, \( c_{2}^{3} = 1.425 \), \( \alpha_{\text{o}}^{{}} = 39.98 \) deg.), and (b) axial force vs. pressure for passive R/R mouse #2 (with c = 0.234 kPa, \( c_{1}^{1} = 7.086 \) kPa, \( c_{2}^{1} = 0.178 \), \( c_{1}^{2} = 4.978 \) kPa, \( c_{2}^{2} = 0.082 \), \( c_{1}^{3} = 0.265 \) kPa, \( c_{2}^{3} = 0.937 \), and α = 30.86 deg.). These results are illustrative of results for other data sets
Discussion
Fibrillin-1 (FBN1) is one of many microfibrils constituting elastic fibers,1,8,43 but its precise role in the vasculature remains unknown. It has been suggested that these microfibrils may play a role in transferring load to elastin, which constitutes 90% of the elastic fibers, and they may help optimize load bearing by orienting these fibers along directions of stress.32 Some suggest that FBN1 may act as a protective scaffold that prevents elastin from over-extending,7,46 thus it has more of a maintenance role for existing elastic fibers rather than being involved in early assembly.40 FBN1 deficient mice are similar to wild-type mice at birth, but they develop marked vascular defects. It appears, therefore, that there are some compensatory structural adaptations during development, which may involve up-regulating other microfibrils or altering fibrillar collagens. Possible tissue-level manifestations of such compensatory adaptations are not known, however.
We characterized, for the first time, the biaxial mechanical behaviors of common carotid arteries from mice homozygous (R/R) for the mgR mutation, which yields a 75–85% reduction in the extracellular matrix glycoprotein fibrillin-1, and we compared results with those from both normal wild-type (+/+) mice and those heterozygous (R/+) for the mgR mutation. Findings revealed that R/R carotids exhibited circumferential mechanical and functional behaviors similar to both wild-type and heterozygous mice. Although this similarity may seem surprising at first, it is important to note two important observations. First, pressure–diameter tests on mouse carotid arteries from many other mutant models also reveal a surprising similarity in circumferential mechanics: see results from Loufrani et al.33 and Dye et al.10 for two models of muscular dystrophy (mdx and sgcd-/-), Schiffers et al.45 for a vimentin null model, Lacolley et al.31 for a desmin null model, Wagenseil et al.49 for an elastin haploinsufficiency model, and Mercier et al.36 for a semicarbazide-sensitive amine-oxidase null model. In other words, although some mutants are embryonic or perinatal lethal because of cardiovascular insufficiencies (e.g., elastin null and lysyl oxidase null), it appears that despite some differences in geometry and baseline hemodynamics, carotid arteries often can compensate during development to achieve at least an early mechanical homeostasis even when there are marked genetic defects in cytoskeletal proteins, cytoskeletal–extracellular matrix interactions, or cross-linking of extracellular matrix components. Second, our results are given for carotid arteries from R/R mice aged 9.5 ± 0.91 weeks. It is likely that carotid arteries from older R/R mice would begin to exhibit marked changes in circumferential mechanical and functional behavior due to progressive calcification, fragmentation of elastin, loss of smooth muscle functionality, and increased inflammation similar to reports of aortic changes in these mice.9,34,40 Indeed, such progressive loses of structural integrity resemble an accelerated arterial aging, wherein one observes similar elastocalcinosis, fragmentation of elastin, and loss of smooth muscle functionality.2,17,39,41 Nevertheless, much could be learned about vascular biology if we understood better the mechanisms responsible for the early compensatory adaptations responsible for the findings reported here.
Whereas circumferential biomechanical behavior was similar among the three genotypes, the R/R carotids exhibited markedly different axial properties. The in vivo axial stretch was significantly lower in R/R carotids than in R/+ and +/+ carotids and so too for the axial stress when assessed at individual in vivo axial stretches (Figs. 1, 5). With regard to mechanical homeostasis, the latter may suggest a slight overcompensation in the reorganization of wall constituents (perhaps mainly collagen in the axial direction) given a lack of increase in wall thickness (Table 2), yet the lower stress could also be protective biaxially. That is, a lower axial stress could compensate in part for a higher circumferential stress if one considered a multiaxial metric of wall stress (e.g., magnitude or invariant of the Cauchy stress tensor). Recall that the R/R arteries showed slight increases in mean circumferential stress and diameter compared to the +/+ controls at near in vivo conditions (13.3% increase in circumferential stress; 5.5% increase in diameter); this increased level of circumferential stress compared well to prior results for R/R aortas though not for the degree of enlargement (14.3% increase in circumferential stress; 27% increase in diameter). The potential importance of multiaxial stresses reminds us that there is much to learn with regard to the best continuum metric to use in modeling stress-mediated growth and remodeling.25 Although most investigators have not considered axial mechanics when studying carotids from mutant models,31,33,36,45 biaxial results for elastin haploinsufficient mice revealed a similar decrease in the in vivo axial prestretch.49 Because this model has 30% less elastin whereas the mgR/mgR model has 75–85% less fibrillin-1, which is thought to decrease the structural effectiveness of elastin, these results are qualitatively consistent. Indeed, it appears that the in vivo axial prestretch depends in large part on the ratio of collagen to elastin,26 hence any loss of elastin would be expected to decrease elastic recoil which in turn would increase the unloaded length and decrease the in vivo stretch. That this, changes in axial stretch appear to be mechanically compensatory—by decreasing the biaxial state of stress, structurally compromised cells or matrix may be slightly less vulnerable to mechanical damage, an idea that is supported further by similar findings for muscular dystrophy models.10
Aortas from MFS patients have reduced distensibility,18,28,29 which, similar to effects of aging, can alter hemodynamics by increasing pulse pressure.17,39 Increased pulse pressure, in turn, is increasingly recognized as an important indicator or initiator of diverse vascular diseases,4,44 and may contribute to what some feel is a cyclic fatigue induced failure of the arterial wall in MFS.28,29 Marque et al.34 reported +/+ and R/R blood pressures to be 124/91 and 131/88, respectively, at similar heart rates in 3- to 5-month-old mice. Noting the statistically significant increased pulse pressure in the RR mice (43 vs. 33 mmHg), computed mean aortic circumferential stresses ranged over the cardiac cycle from 117 ± 12.0 to 188 ± 15.4 kPa for the +/+ mice and 127 ± 10.2 to 222 ± 16.8 for the R/R mice, thus suggesting that R/R vessels may experience greater cyclic stresses in vivo. Cyclic loading may be important to age related fragmentation of elastin and its acceleration in MFS.
Whereas mean stresses can and should be estimated from hemodynamic loads and wall geometry (cf. Eqs. 3 and 4), values of which can be obtained in vivo, structurally motivated constitutive relations (cf. Eqs. 8–11) allow one to begin to relate such stresses to load bearing constituents and their possible changes during adaptations or disease progression. The parameter estimation and fitting of data (Table 3; Fig. 7; Supplemental Fig. 3) demonstrated the utility of a four-fiber family constitutive model to describe mean biaxial Cauchy stresses at multiple axially loaded and pressurized states for both healthy and diseased carotids. This finding is consistent with a recent report that this four-fiber family model is superior to the well-accepted phenomenological model of Fung in fitting mouse carotid data in health and muscular dystrophy13; note, too, that it was recently shown that this four-family model is not over-parameterized in general and thus is sufficient for many purposes of modeling.51 Minimal hysteresis was observed during loading and unloading cycles at 0.01 Hz (data not shown), further justifying the use of an elastic model. Whereas minimization of the objective function e was based directly on stress (Eq. 12; Supplemental Fig. 3), a good test of the fit to data was to predict the structurally important and directly measured pressure–diameter and axial force–pressure responses. Figure 7 illustrated the very good predictions that were achieved, as, for example, for pressure-distension for +/+ mouse #3 and force–pressure for R/R mouse #2 (cf. Table 3). Of particular note, the mean best-fit value of the isotropic stress parameter (c) was 8–9 times lower for the R/R mice than for the +/+ and R/+ mice (Table 3). Because this term is meant to represent the elastin-dominated amorphous matrix, which has a nearly isotropic response,22 this result suggests that R/R carotids had decreased elastin effectiveness as expected. Mathematically, of course, some of an “isotropic response” could be accommodated within the model by increasing together the values of the parameters associated with the four oriented fiber families, which are meant to reflect primarily the fibrillar collagen. Such a uniform increase in collagen parameters did not occur for the R/R carotids. Rather, the only difference for the R/R carotids was in values of the parameters associated with the axially oriented fibers: \( c_{1}^{1} \) and \( c_{2}^{1} \), the former of which showed a trend toward a slight increase and the latter a slight decrease. Again, this finding was consistent with the empirical observation that the primary mechanical difference exhibited by the R/R carotids was in the axial direction. Interpreting such changes in axial material behavior is complicated by the associated reduction of the in vivo axial stretch, which could have resulted largely from a decreased elastin effectiveness but also compensatory alterations in axial collagen that may help normalize a multiaxial metric of wall stress important in mechanical homeostasis. There is clearly a need to begin to correlate standard histological metrics with modeling parameters, but this must be done carefully. For example, similar net effects could result from a net decrease in elastin (e.g., degradation) or simply a decrease in elastin effectiveness (e.g., fragmentation or altered prestretch); measurements of changes in collagen to elastin ratio must be augmented, therefore, with finer detail on elastin structure.
Current treatments of MFS seek primarily to prevent aortic dilation and dissection.20,37 Hence, β-blocker therapy and limiting exhaustive exercise are prescribed for their negative chronotropic and inotropic effects, respectively. These therapeutic approaches reduce the hemodynamic stress on the aortic wall in an attempt to avoid an initial insult that may progress to an aneurysm and ultimately dissection or rupture. Most elastic arteries experience only minimal cyclic axial extensions due to the rhythmic contractions of the heart, with the exception of the pulmonary artery and ascending aorta, while all elastic vessels experience marked cyclic changes in diameter. Aortic dissection in MFS frequently occurs in the ascending aorta, which thus could be due to the unusual combination of cyclic biaxial changes in length and diameter (i.e., axial and circumferential stress) known to occur there. Hence, the degree of multiaxial cyclic distension may be important to arterial stability in MFS, which implicates the possible importance of pulse pressure and heart rate, yet direct cardiac induced cyclic changes in axial extension may play a much greater role than previously thought based on our findings for carotids that diminished fibrillin-1 affected primarily the axial direction. Recently, TGF-β neutralizing antibodies and the angiotension II receptor antagonist, Losartan, have demonstrated promising results for preventing aneurysms in a different mouse model for Marfan Syndrome6 (FBN1C1039FG/+). TGF-β plays complex roles in collagen turnover,30 but there is a need to understand better its mechanoregulation, particularly with regard to possible differential effects on families of collagen having different orientations, again emphasizing a need for careful histological correlates.
Examining arterial mechanics in vitro allows one to control carefully both the applied pressure and axial force. Our findings suggest that axial wall mechanics, particularly via the in vivo axial stretch, plays a particularly important, likely coupling, role in contributing to mechanical homeostasis and thus overall structural integrity. Unfortunately, current in vivo measurement modalities such as MRI, ultrasound, or catheter mounted pressure transducers only enable one to infer arterial distensibility or estimate circumferential stiffness via the pulse wave velocity; they cannot directly reveal changes in axial stiffness. At present, the only possible means to estimate axial mechanics is via the use of computational biomechanics as revealed by recent studies on humans.35,47 There is a need, however, for model refinement via better validation based on additional histological and immunohistological data, and more biaxial biomechanical data, particularly on the aorta in models of Marfan syndrome.
References
Arteaga-Solis, E., B. Gayraud and F. Ramirez. Elastic and collagenous networks in vascular diseases. Cell Struct. Funct. 25:69-72, 2000. doi:10.1247/csf.25.69
Atkinson, J. Age-related medial elastocalcinosis in arteries: mechanisms, animal models, and physiological consequences. J Appl Physiol. 105:1643-51, 2008. doi:10.1152/japplphysiol.90476.2008
Baek, S., K. R. Rajagopal and J. D. Humphrey. A theoretical model of enlarging intracranial fusiform aneurysms. J Biomech Eng. 128:142-9, 2006. doi:10.1115/1.2132374
Boutouyrie, P., C. Bussy, P. Lacolley, X. Girerd, B. Laloux and S. Laurent. Association between local pulse pressure, mean blood pressure, and large-artery remodeling. Circulation. 100:1387-93, 1999.
Brossollet, L. J. and R. P. Vito. An alternate formulation of blood vessel mechanics and the meaning of the in vivo property. J. Biomech. 28:679-687, 1995. doi:10.1016/0021-9290(94)00119-O
Bunton, T. E., N. J. Biery, L. Myers, B. Gayraud, F. Ramirez and H. C. Dietz. Phenotypic alteration of vascular smooth muscle cells precedes elastolysis in a mouse model of Marfan syndrome. Circ. Res. 88:37-43, 2001.
Carton, R. W., J. Dainauskas and J. W. Clark. Elastic properties of single elastic fibers. J. Appl. Physiol. 17:547-551, 1962.
Charbonneau, N. L., R. N. Ono, G. M. Corson, D. R. Keene and L. Y. Sakai. Fine tuning of growth factor signals depends on fibrillin microfibril networks. Birth Defects Res. 72:37-50, 2004. doi:10.1002/bdrc.20000
Chung, A. W., K. Au Yeung, G. G. Sandor, D. P. Judge, H. C. Dietz and C. van Breemen. Loss of elastic fiber integrity and reduction of vascular smooth muscle contraction resulting from the upregulated activities of matrix metalloproteinase-2 and -9 in the thoracic aortic aneurysm in Marfan syndrome. Circ Res. 101:512-22, 2007. doi:10.1161/CIRCRESAHA.107.157776
Dye, W. W., R. L. Gleason, E. Wilson and J. D. Humphrey. Altered biomechanical properties of carotid arteries in two mouse models of muscular dystrophy. J. Appl. Physiol. 103:664-72, 2007. doi:10.1152/japplphysiol.00118.2007
Gleason, R. L. and J. D. Humphrey. Effects of a sustained extension on arterial growth and remodeling: a theoretical study. J. Biomech. 38:1255-61, 2005. doi:10.1016/j.jbiomech.2004.06.017
Gleason, R. L. and J. D. Humphrey. A 2D constrained mixture model for arterial adaptations to large changes in flow, pressure and axial stretch. Math. Med. Biol. 22:347-69, 2005. doi:10.1093/imammb/dqi014
Gleason, R. L., W. W. Dye, E. Wilson, and J. D. Humphrey. Quantification of the mechanical behavior of carotid arteries from wild-type, dystrophin-deficient, and sarcoglycan-delta knockout mice. J. Biomech. 41:3213-3218, 2008.
Gleason, R. L., S. P. Gray, E. Wilson and J. D. Humphrey. A multiaxial computer-controlled organ culture and biomechanical device for mouse carotid arteries. J. Biomech. Eng. 126:787-795, 2004. doi:10.1115/1.1824130
Gleason, R. L., L. A. Taber and J. D. Humphrey. A 2-D model of flow-induced alterations in the geometry, structure, and properties of carotid arteries. J. Biomech. Eng. 126:371-81, 2004. doi:10.1115/1.1762899
Gleason, R. L., E. Wilson and J. D. Humphrey. Biaxial biomechanical adaptations of mouse carotid arteries cultured at altered axial extension. J. Biomech. 40:766-776, 2007. doi:10.1016/j.jbiomech.2006.03.018
Greenwald, S. E. Ageing of the conduit arteries. J Pathol. 211:157-72, 2007. doi:10.1002/path.2101
Groenink, M., A. de Roos, B. J. Mulder, J. A. Spaan and E. E. van der Wall. Changes in aortic distensibility and pulse wave velocity assessed with magnetic resonance imaging following beta-blocker therapy in the Marfan syndrome. Am. J. Cardiol. 82:203-8, 1998. doi:10.1016/S0002-9149(98)00315-4
Groenink, M., A. de Roos, B. J. Mulder, B. J. Verbeeten, J. Timmermans, A. H. Zwinderman, J. A. Spaan and E. E. van der Wall. Biophysical properties of the normal-sized aorta in patients with Marfan syndrome: evaluation with MR flow mapping. Radiology. 219:535-540, 2001.
Habashi, J. P., D. P. Judge, T. M. Holm, R. D. Cohn, B. L. Loeys, T. K. Cooper, L. Myers, E. C. Klein, G. Liu, C. Calvi, M. Podowski, E. R. Neptune, M. K. Halushka, D. Bedja, K. Gabrielson, D. B. Rifkin, L. Carta, F. Ramirez, D. L. Huso and H. C. Dietz. Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science. 312:117-121, 2006. doi:10.1126/science.1124287
Han, H. C. and Y. C. Fung. Longitudinal strain of canine and porcine aortas. J. Biomech. 28:637-641, 1995. doi:10.1016/0021-9290(94)00091-H
Holzapfel, G. A., T. C. Gasser and R. W. Ogden. A New Constitutive Framework for Arterial Wall Mechanics and a Comparative Study of Material Models Journal of Elasticity 61:1-48, 2000. doi:10.1023/A:1010835316564
Hu, J. J., S. Baek, and J. D. Humphrey. Stress-strain behavior of the passive basilar artery in normotension and hypertension. J. Biomech. 40:2559–2563, 2007. doi:10.1016/j.jbiomech.2006.11.007; Corrigendum J. Biomech. 41:239, 2008
Humphrey, J. D. Cardiovascular Solid Mechanics: Cells, Tissues, and Organs. New York; Springer, 2002.
Humphrey, J. D. Vascular adaptation and mechanical homeostasis at tissue, cellular, and sub-cellular levels. Cell Biochem Biophys. 50:53-78, 2008. doi:10.1007/s12013-007-9002-3
Humphrey, J. D., J. F. Eberth, W. W. Dye and R. L. Gleason. Fundamental role of axial stress in compensatory adaptations by arteries. J Biomech. 42:1-8, 2009. doi:10.1016/j.jbiomech.2008.11.011
Humphrey, J. D. and K. R. Rajagopal. A constrained mixture model for arterial adaptations to a sustained step change in blood flow. Biomech Model Mechanobiol. 2:109-26, 2003. doi:10.1007/s10237-003-0033-4
Jeremy, R. W., H. Huang, J. Hwa, H. McCarron, C. F. Hughes and J. G. Richards. Relation between age, arterial distensibility, and aortic dilatation in the Marfan syndrome. Am. J. Cardiol. 74:369-373, 1994. doi:10.1016/0002-9149(94)90405-7
Jondeau, G., P. Boutouyrie, P. Lacolley, B. Laloux, O. Dubourg, J. P. Bourdarias and S. Laurent. Central pulse pressure is a major determinant of ascending aorta dilation in Marfan syndrome. Circulation. 99:2677-81, 1999.
Jones, J. A., J. R. Barbour, R. E. Stroud, S. Bouges, S. L. Stephens, F. G. Spinale and J. S. Ikonomidis. Altered transforming growth factor-beta signaling in a murine model of thoracic aortic aneurysm. J Vasc Res. 45:457-68, 2008. doi:10.1159/000127437
Lacolley, P., P. Challande, S. Boumaza, G. Cohuet, S. Laurent, P. Boutouyrie, J. A. Grimaud, D. Paulin, J. M. Lamazière and Z. Li. Mechanical properties and structure of carotid arteries in mice lacking desmin. Cardiovascular Research. 51:178-87, 2001. doi:10.1016/S0008-6363(01)00278-4
Lillie, M. A., G. J. David and J. M. Gosline. Mechanical role of elastin-associated microfibrils in pig aortic elastic tissue. Connect Tissue Res. 37:121-41, 1998. doi:10.3109/03008209809028905
Loufrani, L., K. Matrougui, D. Gorny, M. Duriez, I. Blanc, B. I. Levy and D. Henrion. Flow (shear stress)-induced endothelium-dependent dilation is altered in mice lacking the gene encoding for dystrophin. Circulation. 103:864-70, 2001.
Marque, V., P. Kieffer, B. Gayraud, I. Lartaud-Idjouadiene, F. Ramirez and J. Atkinson. Aortic wall mechanics and composition in a transgenic mouse model of Marfan syndrome. Arterioscler Thromb Vasc Biol. 21:1184-9, 2001. doi:10.1161/hq0701.092136
Masson, I., P. Boutouyrie, S. Laurent, J. D. Humphrey and M. Zidi. Characterization of arterial wall mechanical behavior and stresses from human clinical data. J Biomech. 41:2618-27, 2008. doi:10.1016/j.jbiomech.2008.06.022
Mercier, N., M. Osborne-Pellegrin, K. El Hadri, A. Kakou, C. Labat, L. Loufrani, D. Henrion, P. Challande, S. Jalkanen, B. Feve and P. Lacolley. Carotid arterial stiffness, elastic fibre network and vasoreactivity in semicarbazide-sensitive amine-oxidase null mouse. Cardiovasc Res. 72:349-57, 2006. doi:10.1016/j.cardiores.2006.08.008
Milewicz, D. M., H. C. Dietz and D. C. Miller. Treatment of aortic disease in patients with Marfan syndrome. Circulation. 111:e150-7, 2005 doi:10.1161/01.CIR.0000155243.70456.F4
Neptune, E. R., P. A. Frischmeyer, D. E. Arking, L. Myers, T. E. Bunton, B. Gayraud, F. Ramirez, L. Y. Sakai and H. C. Dietz. Dysregulation of TGF-β activation contributes to pathogenesis in Marfan syndrome. Nat. Genet. 33:407-411, 2003. doi:10.1038/ng1116
O’Rourke, M. F. and J. Hashimoto. Mechanical factors in arterial aging: a clinical perspective. J Am Coll Cardiol. 50:1-13, 2007. doi:10.1016/j.jacc.2006.12.050
Pereira, L., S. Y. Lee, B. Gayraud, K. Andrikopoulos, S. D. Shapiro, T. Bunton, N. J. Biery, H. C. Dietz, L. Y. Sakai and F. Ramirez. Pathogenetic sequence for aneurysm revealed in mice underexpressing fibrillin-1. Proc. Natl. Acad. Sci. U. S. A. 96:3819-3823, 1999. doi:10.1073/pnas.96.7.3819
Pezet, M., M. P. Jacob, B. Escoubet, D. Gheduzzi, E. Tillet, P. Perret, P. Huber, D. Quaglino, R. Vranckx, D. Y. Li, B. Starcher, W. A. Boyle, R. P. Mecham and G. Faury. Elastin haploinsufficiency induces alternative aging processes in the aorta. Rejuvenation Res. 11:97-112, 2008. doi:10.1089/rej.2007.0587
Pyeritz, R. The Marfan syndrome. Annu. Rev. Med. 2000 51:481-510, doi:10.1146/annurev.med.51.1.481
Ramirez, F. and L. Pereira. The fibrillins. Int. J. Biochem. Cell Biol. 31:255-9, 1999. doi:10.1016/S1357-2725(98)00109-5
Safar, M. E. Pulse pressure, arterial stiffness, and cardiovascular risk. Curr Opin Cardiol. 15:258-63, 2000. doi:10.1097/00001573-200007000-00009
Schiffers, P. M., D. Henrion, C. M. Boulanger, E. Colucci-Guyon, F. Langa-Vuves, H. van Essen, G. E. Fazzi, B. I. Levy and J. G. De Mey. Altered flow-induced arterial remodeling in vimentin-deficient mice. Arterioscler Thromb Vasc Biol. 20:611-6, 2000.
Sherratt, M. J., C. Baldock, J. L. Haston, D. F. Holmes, C. J. Jones, C. A. Shuttleworth, T. J. Wess and C. M. Kielty. Fibrillin microfibrils are stiff reinforcing fibres in compliant tissues. J. Mol. Biol. 332:183-93, 2003. doi:10.1016/S0022-2836(03)00829-5
Stalhand, J., A. Klarbring and M. Karlsson. Towards in vivo aorta material identification and stress estimation. Biomech Model Mechanobiol. 2:169-86, 2004. doi:10.1007/s10237-003-0038-z
Van Loon, P., W. Klip and E. L. Bradley. Length-force and volume-pressure relationships of arteries. Biorheology. 14:181-201, 1977.
Wagenseil, J. E., N. L. Nerurkar, R. H. Knutsen, R. J. Okamoto, D. Y. Li and R. P. Mecham. Effects of elastin haploinsufficiency on the mechanical behavior of mouse arteries. Am J Physiol Heart Circ Physiol. 289:H1209-17, 2005. doi:10.1152/ajpheart.00046.2005
Weizsacker, H., H. Lambert and K. Pascale. Analysis of the passive mechanical properties of rat carotid arteries. J. Biomech. 16:703-715, 1983. doi:10.1016/0021-9290(83)90080-5
Zeinali-Davarani, S., J. Choi, and S. Baek. On parameter estimation for biaxial mechanical behavior of arteries. J. Biomech. 42:524-530, 2009.
Acknowledgments
This work was supported, in part, by Grants from the NIH (HL-64372, HL-86418, EB-04106). We thank Professor F. Ramirez, UMDNJ-Robert Wood Johnson Medical School for supplying breeding pairs for the fibrillin-1 deficient mice, as well as Ms. K. Miller for technical assistance and Professor R.L. Gleason for continued advice on mechanical testing.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Eberth, J.F., Taucer, A.I., Wilson, E. et al. Mechanics of Carotid Arteries in a Mouse Model of Marfan Syndrome. Ann Biomed Eng 37, 1093–1104 (2009). https://doi.org/10.1007/s10439-009-9686-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-009-9686-1