Abstract
Background We present a fundamental theoretical framework for analysis of energy dissipation in any component of the circulatory system and formulate the full energy budget for both venous and arterial circulations. New indices allowing disease-specific subject-to-subject comparisons and disease-to-disease hemodynamic evaluation (quantifying the hemodynamic severity of one vascular disease type to the other) are presented based on this formalism. Methods and Results Dimensional analysis of energy dissipation rate with respect to the human circulation shows that the rate of energy dissipation is inversely proportional to the square of the patient body surface area and directly proportional to the cube of cardiac output. This result verified the established formulae for energy loss in aortic stenosis that was solely derived through empirical clinical experience. Three new indices are introduced to evaluate more complex disease states: (1) circulation energy dissipation index (CEDI), (2) aortic valve energy dissipation index (AV-EDI), and (3) total cavopulmonary connection energy dissipation index (TCPC-EDI). CEDI is based on the full energy budget of the circulation and is the proper measure of the work performed by the ventricle relative to the net energy spent in overcoming frictional forces. It is shown to be 4.01 ± 0.16 for healthy individuals and above 7.0 for patients with severe aortic stenosis. Application of CEDI index on single-ventricle venous physiology reveals that the surgically created Fontan circulation, which is indeed palliative, progressively degrades in hemodynamic efficiency with growth (p < 0.001), with the net dissipation in a typical Fontan patient (Body surface area = 1.0 m2) being equivalent to that of an average case of severe aortic stenosis. AV-EDI is shown to be the proper index to gauge the hemodynamic severity of stenosed aortic valves as it accurately reflects energy loss. It is about 0.28 ± 0.12 for healthy human valves. Moderate aortic stenosis has an AV-EDI one order of magnitude higher while clinically severe aortic stenosis cases always had magnitudes above 3.0. TCPC-EDI represents the efficiency of the TCPC connection and is shown to be negatively correlated to the size of a typical “bottle-neck” region (pulmonary artery) in the surgical TCPC pathway (p < 0.05). Conclusions Energy dissipation in the human circulation has been analyzed theoretically to derive the proper scaling (indexing) factor. CEDI, AV-EDI, and TCPC-EDI are proper measures of the dissipative characteristics of the circulatory system, aortic valve, and the Fontan connection, respectively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
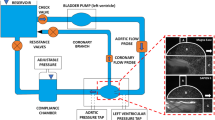
Pioneered advances in computational, analytical and experimental cardiovascular fluid dynamics6,14,27,29,32,42 currently enable patient-specific quantitative hemodynamic analysis of several disease pathologies and for any surgically created pathway, almost routinely.7,36,39,41 While the current technology allows detailed spatial/temporal prediction of hemodynamic/physiological parameters of interest, such as wall shear stress indices, pressure drops, blood trauma parameters and hydrodynamic energy dissipation, the clinical significance of the absolute values of these parameters, for the patient under consideration is still vague. For instance, how can the clinician use detailed information such as pressure drops or raw energy dissipation rate data in a patient and translate it to treatment decisions? Clinical management often relies on “indexing” as a way to establish a threshold number or an acceptable range for a given parameter (e.g. stroke volume is indexed as (1) stroke volume index defined as ratio to body surface area; or (2) Ejection fraction defined as ratio to end diastolic volume). If the index value crosses a threshold or is outside the acceptable range, then clinical action is warranted. Indexing as termed in the medical community is analogous to normalizing variables in dynamically similar physical systems with the exception that an indexed quantity is not necessarily dimensionless. Most parameters or variables used by the medical community are indexed and the “normalizing” factor is often debated based on empirical analysis of large patient data sets.
Currently there is no recognized quantitative index for normalizing hemodynamic power generated by the ventricle or energy dissipation rate at circulatory components such as valves, connections, or stenosis regions. Clinical experience, over the years, provided several rule-of-thumb indices to individualize the disease-specific hemodynamic patient-specific parameters, yet for most applications these indices lack rigorous hemodynamic foundation or are incomplete as they are solely based on crude allometric principles (i.e. change in shape with size).17,21
Our interest in this manuscript is particularly on hydrodynamic energy dissipation in the circulatory system, which occurs due to friction imposed by the viscosity of blood. Mechanical power produced by the contraction of the heart is continuously dissipated into heat via viscous friction as evident by the loss of total pressure from the arterial to the venous sides of the systemic and pulmonary circulations. In certain pathological situations such as vessel or valve stenosis13 (e.g. aortic stenosis) or unfavorable vessel geometries causing flow separation and/or collision (e.g. Fontan vessel anatomies),10,11 energy dissipation may far exceed tolerable levels. Independent of the disease type, high energy dissipation always impacts the pumping ventricle that, together with the peripheral vasculature, adapts itself to work harder to overcome the added drag in order to meet the functions of the circulatory system, always resulting in chronic heart failure as a secondary disease.
Traditionally, a cardiologist would determine the hemodynamic severity of the lesion based on crude global measures such as pressure gradients between the arterial and venous side. Using a global parameter is a fair assumption as in a closed loop circulation system the specific location of high energy dissipation is not relevant when assessing the energetic impact on the ventricle.2 On the other hand, the relevance of the parameters used is more questionable. Although pressure gradients describe the precise mechanical environment, they fail to capture the net physical impact on the circulatory system. From a fluid mechanical point of view, energy dissipation expressed in Watts fully describes the hemodynamic severity as well as the impact on the pumping ventricle. However, this parameter has been utilized in a limited number of biomedical studies1,26,28 and has just recently been recognized by clinicians as an evaluation criteria for disease severity, particularly for aortic stenosis and Fontan surgical connections. For aortic stenosis, which is an arterial disease, an index based on total pressure (static plus dynamic) loss, which is a pseudo-indicator of energy dissipation based on Bernoulli’s Equation, is widely used,13 while raw energy loss has been proposed to assess the severity of the Fontan connections clinically.31,41 Nevertheless, both applications lack a proper aforementioned framework that would enable a standardized way to develop such indices and more importantly unify the hemodynamic assessment of all dissipative lesions of the circulatory system. Such unification will enable disease-to-disease hemodynamic comparison and eliminate separate disease-specific standards or clinical rules-of-thumb.
In summary, a unified/standardized analytical framework for energy dissipation with reliable clinical indices of efficiency requires the incorporation of patient size and cardiac output on overall energy dissipation magnitudes. This step is necessary as comparing any energy dissipation measurements between patients with different sizes and cardiac outputs will obviously carry little meaning. Keeping that observation in mind, this manuscript will first formulate the full energy budget of human circulation based on the actual energy spent by the pumping ventricle. Proper dimensional analysis of the energy budget would then provide the basis to develop proper indices that are flow and size independent, for direct and correct use in clinical practice. In this framework the energy dissipation and energy budget of the circulation will be revisited through rigorous engineering dimensional analysis.3 The scaling of energy dissipation occurring at any component in the circulation system is examined with respect to patient size and cardiac output. This is followed by the formulation of the mean mechanical energy budget of the circulatory system. Based on this formulation, we present three new indices: The first one is a circulatory system level index that is not disease specific, called the circulation energy dissipation index (CEDI), which quantifies the dissipative characteristic of the entire circulatory system as a whole. The two additional indices are disease specific indexes namely: (1) aortic valve energy dissipation index (AV-EDI); and (2) total cavopulmonary energy dissipation index (TCPC-EDI). These indices are the proper indices to asses the severity of the respective lesion, i.e. aortic stenosis and the Fontan connection respectively.
The paper is organized as follows: section Theoretical Analysis details the theoretical analysis of energy dissipation at any component of the circulatory system using dimensional analysis. In section Mean Circulation Energy Budget and the Framework for New Indices the global energy budget of the entire circulatory system is formulated based on results from dimensional analysis. The three new non-dimensional energy dissipation measures of the whole circulatory system (CEDI), aortic stenosis (AV-EDI), and TCPC surgical connection (TCPC-EDI) are introduced. In section Application of Indices Based on Published Data, we apply these new indices to both normal and single ventricle physiologies, using published clinical data and large clinical databases. Section Discussion is the clinical relevance of these new measures contributing interesting insights on these disease states which is followed by the final Conclusions section.
Theoretical Analysis
Consider hydrodynamic energy dissipation occurring across any component of the circulatory system. Just like the energy dissipation at a pipe fitting is completely and sufficiently governed by the flow through the pipe, density, viscosity, size of the pipe, and the nature of the fitting (e.g. contraction ratio), the time averaged energy dissipation, ɛ, at any component of the circulatory system generally depends on the mean flow rate or cardiac output, Q, the blood density, ρ, the kinematic viscosity, ν, the characteristic size of the geometry, which is governed by the patient body surface area, BSA,34 and a dimensionless quantity representing the shape of the geometry, S. Note that the results of this paper will remain the same if we were to chose a different measure for patient size (such as size of aorta, or size of heart) as all these quantities are now known to scale with BSA.
Note that in almost all cases, the variable representing pathology is S, which can be as simple as a percentage occlusion for the case of stenosis or as complex as vessel orientations, offsets and relative sizes of vessels for bifurcations, confluences, etc. Typical examples of the latter multi-branch anatomical components include the aortic arch and the surgically created Fontan venous pathways (TCPC) utilized in right-heart by-pass.30,35,40 In general, S is a vector quantity with as many components as necessary to fully describe the shape of the geometry and is equivalent to the series of ratios r′, r′′, r′′′ in Buckingham’s paper on the rigorous proof and application of dimensional analysis in physically similar systems (in our case healthy and diseased individuals).3 The functional dependence of mean energy dissipation on the above mentioned independent variables is represented in Eq. (1):
Note that we neglect variables that characterize the time varying characteristics such as, heart rate, compliance, etc. as their effect on the time averaged (mean) characteristics of the circulation is implicit. For instance, if a patient had abnormal compliance then that would be reflected in changes in flow characteristics. The above relationship between six variables can be reposed as a relationship between non-dimensional groups using the Buckingham π theorem.3 As derived in the Appendix, Buckingham π theorem shows that ɛ must scale with the term \( \rho{\frac{{Q^{3} }}{{BSA^{2} }}} \) and the dimensionless representation of Eq. (1) becomes:
where Re is the Reynolds number. The Reynolds number as derived in Eq. (A12) is based on a characteristic velocity scale as the ratio of cardiac output to BSA (i.e. cardiac index in SI units) and a characteristic length scale defined as \( \sqrt {BSA} . \) The above dimensionless relation is general and applicable to mean energy dissipation across any component in the human circulatory system. However, further simplification of Eq. (2) depends solely on the specific component of the circulatory system, e.g. valve, stenosis, bifurcation, TCPC, etc. Note that the left hand side of Eq. (2), is similar to the Power number, a common dimensionless number used in engineering that is the ratio of the frictional energy to the inertial energy. For the human circulation, \( \rho \frac{{Q^{3} }}{{BSA^{2} }} \) is a scale for the total inertial (kinetic) power available to which energy dissipation, ɛ, is shown to be directly proportional. Equation (2) provides further insights into that relation, showing that the proportionality factor is not a constant but depends on the flow regime and the geometry of the component, characterized by Re and S, respectively.
Mean Circulation Energy Budget and the Framework for New Indices
When applied to the specific circulatory component, the right hand side of Eq. (2) is an energy dissipation index (EDI) that directly relates the hydrodynamic efficiency of that component to its geometrical configuration. For a given BSA and cardiac output, a geometry that offers little resistance to flow, such as a large vessel, will yield little energy dissipation and in turn a low EDI. Conversely, a constricted vessel will yield higher dissipation and thus a higher EDI. Equation (2) is our basis to form disease specific indices such as AV-EDI and TCPC-EDI later introduced in this section.
Apart from allowing the proper definition of disease specific indices, the formulation of the time-averaged energy dissipation across any single component of the circulatory system, given by Eq. (2), also allows for the mathematical formulation of the mean energy budget of the entire circulatory system. The mean power, \( \dot{E}_{\text{v}} , \) produced by the ventricle is simply:
where T is the duration of the cardiac cycle, P is the ventricular pressure, and V the ventricular volume. Note that the integral is only during systole as this is the only time when ventricular muscles impart new mechanical energy into the blood stream. The work done by the muscles translates into both kinetic and potential energy of the entire blood in the circuit (either systemic or pulmonary). All of the power produced (Eq. 3) is eventually dissipated as heat (Eq. 2) at every component of the circulatory system. Therefore application of energy conservation principle combined with Eq. (2) defines the energy budget of the entire cardiovascular system as:
where f i (Re i , S i ) is the proportionality constant for each component dependent on the local Reynolds number, Re i and the geometric shape factor characterized by S i .
In the rest of this section, we introduce three new indices, CEDI, AV-EDI, and TCPC-EDI.
CEDI: An Index to Gauge the Efficiency of the Circulation
From the above Eq. (4), it is clear that the ratio CEDI (circulatory energy dissipation index) defined as:
CEDI is a dimensionless measure of the entire frictional resistance (or head loss coefficient) of the circuit through which the ventricle pumps the blood. The right hand side of Eq. (5) only depends on non-dimensional quantities describing each component of the human circulation. S i is reasonably constant over all healthy individuals and for most cases a weak dependence with respect to gender and age is justified as a first approximation. In addition, it can be shown that Re i scales linearly with \( \sqrt {BSA} \) (given that cardiac output scales linearly with BSA and all vascular dimensions scale linearly with \( \sqrt {BSA} \) 34). Therefore, for healthy adult humans, the term \( \sum\limits_{\text{allcomponents}} {f_{i} \left( {Re_{i} ,S_{i} } \right)} \) is hereby presumed as a pseudo-universal constant, and that the calculated value significantly departs for individuals with any abnormality (flow regime and anatomy) in the circulation system. One must note here that this constant is independent of the condition of the pump itself and therefore is not a measure of the efficiency of the ventricle in converting chemical energy into mechanical energy, but rather a measure of the total energy dissipated for a given patient relative to the amount of frictional energy dissipation “expected” for his or her BSA and cardiac output. CEDI directly provides the effective energy that is spent in overcoming frictional forces similar to the “head loss constant” widely used in hydraulics.
To yield a clinically reasonable scale for CEDI, the units of Q in the denominator of Eq. (5) should be L/s while the rest should be in SI units. A high CEDI indicates a high ventricular power spent relative to the expected frictional energy dissipation and is thus indicative of a highly dissipative circulatory system. Different baseline CEDI values for normal circulation may be required when applying CEDI evaluation to children rather than adults, due to differences in vasculature that is not topologically similar to adult vasculature configuration. Finally, it should be realized that CEDI is an easy to compute index and is thus highly relevant for clinical practice as it is (demonstrated in the following section) sensitive to abnormalities in the circulation.
AV-EDI: Proper Measure for Aortic Stenosis
Several measures exist to quantify the degree of severity of aortic stenosis. The traditional methods of calculating the effective orifice area using the Gorlin Equation,16 as well as the direct evaluation of area using the “continuity method” applied to ultrasound Doppler measurements are known to be flow dependent4 and thus non-standard. The Gorlin equation is \( A_{\text{A}} \propto \frac{Q}{{\sqrt {\Updelta P} }} \) where ΔP is the pressure drop across the valve.
A more recent measure is the energy loss index (ELI) proposed in Garcia et al. 13 It is straightforward to show that the general result (Eq. 2) is consistent with the ELI measure of aortic stenosis but with a caveat as demonstrated below. In the case of aortic stenosis, total pressure loss, E L , across a stenotic aortic valve is given by:
where A A is the aortic cross-sectional area in cm2. The above equation is the same as Eq. (2) in Garcia et al. 13 where S replaces the ratio between the effective orifice area, EOA, of the aortic valve and the aortic cross-sectional area in cm2, i.e. S ≡ EOA/A A, and Q is expressed in mL/s instead of L/min. From this equation, energy dissipation in Watts may be easily computed as ɛ = QE L, which, after the correct unit conversion, gives:
where Q is now expressed in liter/s. Using the fact that aortic cross-sectional area is directly proportional to patient BSA,34 i.e. A A ∝ BSA, Eq. (7) may be rearranged in the form of Eq. (2):
where K is a constant equal to \( 5.33 \times 10^{ - 5} \frac{{BSA^{2} }}{{A_{\text{A}}^{2} }}\frac{1}{\rho } \). Note that Eq. (7) was derived by Garcia et al. 13 with an implicit assumption of Reynolds number independence. Comparison of Eq. (8) with Eq. (7) shows that K should depend on the Reynolds number based on dimensional analysis. Reynolds number of flow through the valve certainly depends on the condition of the valve, gender, and age. However, the assumption that the overall dependence on Reynolds number may be weak is valid given that the Reynolds number of flow through the aorta is fairly high (~5000, based on peak bulk velocity and aorta diameter). Using the empirical relationship between A A and BSA (i.e. A A/BSA ≈ 2.25 cm2/m2) by Sluysmans and Colan,34 K is computed to be a constant of about 1.03 × 10−8 for normal circulation.
The above expression shows that the term \( \left( {\frac{1}{S} - 1} \right)^{2} \) is directly proportional to energy dissipation in the valve and as such is a true gauge of the efficiency of the stenotic valve. The caveat is that this expression slightly differs from the energy loss index (ELI) proposed by Garcia et al. 13 which was defined as \( ELI = \frac{{A_{\text{A}} \times EOA}}{{A_{\text{A}} - EOA}} \cdot \frac{1}{BSA} = \frac{S}{{\left( {1 - S} \right)}} \cdot \frac{{A_{\text{A}} }}{BSA}. \) Contrary to \( \left( {\frac{1}{S} - 1} \right)^{2} \) the ELI index is not a linear measure of energy dissipation through the valve. However, it can be shown that both expressions are related with the following proportionality:
We therefore define a new index, named aortic valve energy dissipation index (AV-EDI), as a modification to the ELI index, given by the following equation:
AV-EDI and ELI are equivalent and carry no new information. AV-EDI, which is simply the inverse squared of ELI, is the correct representative of the energy efficiency of a stenotic aortic valve owing to its linear association with the energy dissipation as opposed to ELI which as an inverse-squared association. Therefore a 10-fold increase in AV-EDI directly implies a 10-fold increase in energy dissipation. Figure 1 depicts the AV-EDI plotted as a function of S, which is the measure of percent orifice opening. From Eq. (8) it is clear that energy dissipation approaches infinity as EOA approaches zero, keeping flow through the valve constant, and zero as EOA approaches A A. These two extremes are physiologically not possible as a normal native valve cannot have an EOA equal to A A. However, the figure shows the importance of the pressure recovery term as a function of S, an issue previously debated in literature.19,25 The energy dissipation clearly approaches the Gorlin power law relationship given by \( \varepsilon \propto \frac{1}{{S^{2} }} \) (as S → 0 while the influence of pressure recovery increases as S → 1. The AV-EDI index is therefore truly the complete representation of energy efficiency of the aortic valve.
TCPC-EDI: Proper Measure for Fontan Connection
The left hand side of Eq. (2) when applied to the Fontan connection is defined as the TCPC energy dissipation index (TCPC-EDI), which is purely a function of Reynolds number and the non-dimensional geometric factor(s) S. This index is similar to the AV-EDI index for dissipation across stenosed aortic valves. Note that Q in the denominator of the left hand side must be in L/s to yield magnitudes in the same scale as CEDI.
Application of Indices Based on Published Data
In this section we present a brief examination of CEDI for various lesions in both arterial and venous systems, and calculate actual patient-specific values of AV-EDI and TCPC-EDI from the available published clinical data. CEDI is examined in bi-ventricular as well as single ventricular physiologies. Cases for bi-ventricular configuration include aortic stenosis, cardiomyopathy, and myocardial infarction in a bi-ventricular configuration, while cases for single ventricle physiology include the Blallock Tausig (BT) shunt, and Fontan connection representing different post-operative stages. AV-EDI is examined for various clinical stages of aortic stenosis, i.e. moderate stenosis, and severe stenosis. Due to the complex nature of the TCPC, we examine TCPC-EDI only with respect to a single geometric factor based on available in vitro energy dissipation data. All these results are discussed in section Discussion in detail. All error bars represent standard error in the mean.
CEDI in Arterial Bi-Ventricle Physiology
Figure 2 compares the CEDI for healthy individuals with that calculated for two severe diseases of the circulatory system whose ventricular pressure–volume (P–V) data has been published18,22,37: (1) severe aortic stenosis, and (2) history of ventricle abnormality. The systemic CEDI for healthy individuals was estimated by assuming that cardiac output for healthy individuals is approximately 3.5 L min−1 m−2 times BSA and the mean pressure of the left ventricle over systole is in the range 90–120 mmHg.34 This yields a CEDI of about 4.01 ± 0.16. Within the severe aortic stenosis group, Hachichi et al. 18 presented data among those whose cardiac output was normal, and those who had low cardiac output (consequently low pressure gradient across the valve). Mean CEDI for these two groups was 7.26 ± 0.31 and 13.08 ± 0.78, respectively, Fig. 2. Both groups of disease states are found to be significantly different than the healthy CEDI (p < 0.001).
Comparison of circulation energy dissipation index (CEDI) between healthy individuals, patients with two types of aortic stenosis, and patients with two types of ventricular abnormality, based on previously published data.18,22,34 Statistical comparison between pathological cases with normal case yields p value < 0.001, except for cardiomyopathy. Error bars represent standard error in the estimated mean CEDI
CEDI is also presented for two types of ventricular abnormality (data published by Kameyama et al.22), one with cardiomyopathy and one with history of myocardial infarction to provide a comparative basis. Mean CEDI for these two groups was 3.41 ± 0.32 and 9.75 ± 0.70, respectively. A statistical comparison between the presented patient groups with healthy individuals plotted in Fig. 1 yields a p value <0.001 for the myocardial infarction group. No significant statistical difference between healthy and cardiomyopathy states was observed.
CEDI in Venous Single Ventricle Physiology
Single ventricle patients are patients born with severe cyanosis due to a volume overloaded single functioning ventricle.24 These patients typically undergo a three-stage surgery where the native circulatory physiology is altered step-by-step for gradual transformation to the single ventricle physiology. For the first stage (conducted within the first few weeks of life), patients undergo surgery where a single outflow tract is reconstructed for the single ventricle. Oxygen saturation is restored via the Blallock-Taussig shunt (BT shunt). The shunt connects a high pressure systemic vessel such as the sub-clavian artery to the pulmonary artery to augment flow through the lungs. During the second stage (typically conducted before 9 months age) the shunt is removed. High flow to the lungs is ensured via the Bi-directional Glenn or Hemi-Fontan connection where the superior vena cava is connected to the pulmonary artery. Thus all the venous return from the upper portion of the body is routed to the heart via the lungs thus ensuring oxygenation. In the third-stage, the inferior vena cava is also connected to the bi-directional Glenn or Hemi-Fontan connection thus creating a total cavopulmonary connection (TCPC) where all the venous return is routed through the lungs.15 For a thorough review of single ventricle physiology and the various complications the reader is re-directed to Fontan and Baudet11 and Khairy et al. 24
Only two studies (i.e. Senzaki et al. 33 and Sundareswaran et al. 37) have addressed the single ventricle circulation at the system level (i.e. PV loop analysis or direct energy estimation). Compilation of the data from these two studies enabled to examine how CEDI varies in single ventricle patients at different stages of the palliative cure.
Figure 3 shows a comparison of averaged CEDI for these three different patient populations based on published data33,37 with a comparison to the CEDI of a healthy adult and child. The CEDI for normal children (age 3.8 ± 3.2 years) was 1.27 ± 0.97, while that for the BT shunt group (age 2.8 ± 3.2 years) was 0.73 ± 0.87. The CEDI for the younger Fontan group published in Senzaki et al. 33 (age 4.5 ± 3.8 years) was 2.70 ± 0.97. For the older Fontan group studied in Sundareswaran et al. 37 (age 11.0 ± 6.0 years) the CEDI value was 8.1 ± 5.2. Statistical comparison between any group yields statistically significant differences (p < 0.001).
Comparison of circulation energy dissipation index (CEDI) between healthy individuals (adult and 4 year old children), patients with single ventricle physiologies namely: BT shunt group and a young Fontan patient group in Senzaki et al.,33 Older Fontan patient group from Sundareswaran et al. 37 Error bars represent standard error in the estimated mean CEDI
Figure 4 shows the above raw CEDI data the Fontan patient groups plotted with respect to BSA. For the data, CEDI correlated positively with BSA with p < 0.001 respectively. Comparison with average CEDI value for a severe aortic stenosis patient group, 7.7 ± 0.32 is also plotted.
AV-EDI Applied to Aortic Stenosis Patient Data
To provide a detailed feel for AV-EDI, Fig. 5 shows AV-EDI calculated for the published aortic stenosis data.13,18 Notice that AV-EDI increases with severity of aortic stenosis with a magnitude of 0.28 ± 0.12 for a normal healthy aortic valve. Notice that moderate aortic stenosis has an AV-EDI that is one order of magnitude higher while patients with severe aortic stenosis (including those with low cardiac output) have an AV-EDI magnitude of above 3.0. Note that the new index successfully captures the severity of paradoxical low flow patients who are at a risk of possible mismanagement.5,18
Aortic valve energy dissipation index (AV-EDI) compared for various published aortic stenosis study groups: (1) normal/healthy, (2) moderate stenosis patients, i.e. free from events such as aortic replacement or death, (3) severe aortic stenosis patients who ultimately either received a replacement valve or died, (4) severe aortic stenosis patients with normal cardiac output, and (5) severe aortic stenosis patients who presented with low cardiac output and low pressure gradient
TCPC-EDI Applied to Patient-Specific Energy Dissipation Data
Anatomically accurate in vitro models of six patients with TCPCs were fabricated and the energy dissipation was experimentally determined for flow conditions ranging from resting cardiac output to two and three times the resting cardiac output at 50–50 flow split condition between the left pulmonary artery (LPA) and right pulmonary artery (RPA). The resting cardiac outputs were based on phase contrast MRI measurements in vivo. The purpose of conducting the energy dissipation experiments at both 50–50 flow split is to evaluate the TCPC-EDI with flow split as the control. Details on the experimental methodology used to determine the hydrodynamic energy dissipation characteristics of TCPCs, flow conditions, MRI protocols, etc. can be found in literature.8,9,23 To illustrate the application of Eq. (2) for analyzing this data we chose to investigate the relationship between energy dissipation and LPA minimum cross-sectional area in the in vitro model (i.e. the bottle neck region) with and without non-dimensionalization.
Figure 6a shows the dimensional energy dissipation results plotted for all the different flow conditions. The data is clearly complex spanning over different patients with different resting and exercise cardiac outputs and with variation in the shape of their TCPC geometries. This complexity is evident with the scatter seen in Fig. 6a. We now non-dimensionalize the data as dictated by Eq. (2). The shape factor S under investigation is the LPA minimum cross-sectional area, which we non-dimensionalize by patient BSA since LPA area, like all vessels, scales with BSA.34 The corresponding non-dimensionalized data are plotted in Fig. 6b. A clear and strong correlation between the LPA minimum size and energy dissipation in the TCPC emerges (R 2 = 0.88, p < 0.05).
Discussion
In this section we discuss the relevance of the three new indices CEDI, AV-EDI, and TCPC-EDI based on their calculations from published data in the previous section. Specific emphasis is laid on the clinical relevance and new insights on the diseases.
CEDI in Bi-Ventricular Physiology
It is interesting to note that CEDI significantly differs for all the patient groups when compared to healthy individuals with the exception of cardiomyopathy (Fig. 2). The most severe being for the case of severe aortic stenosis with low flow whose mean CEDI indicates an effective energy load on the ventricle was the highest. This class of aortic stenosis may represent the end stage of the disease where clearly the high CEDI value indicates a highly dissipative circulation. For the case of cardiomyopathy, CEDI is comparable to normal levels, which is expected since CEDI is by definition independent of the condition of the ventricle and only characterizes the energy dissipation in the systemic circuit.
Note that CEDI is also significantly elevated in the patient group with a history of myocardial infarction suggesting sustained energy dissipation in the systemic circulation. This is not surprising as most patients who suffer from myocardial infarction often have an underlying condition such as hypertension, hypercholesterolemia, and coronary artery disease, all of which indicate a high-friction dissipative systemic circulation.
In summary, CEDI as presented above (Fig. 2) is a clear and sensitive indicator of energy efficiency of the circulatory system (minus the ventricle) with a value of about 4.01 ± 0.16 for healthy individuals, enabling disease-to-disease comparisons. Elevated CEDI indicates severe dissipative forces in the circulatory system as evident for the cases of aortic stenosis. CEDI is also seen to be insensitive to inefficiencies with the pump itself as depicted by the normal CEDI values of patients with cardiomyopathy.
CEDI in Single Ventricular Physiology
From Fig. 3, the averaged CEDI for normal children aged about 3.8 years is lower than the averaged CEDI for normal adults. This implies that the effective energetic load on the ventricle in children is lower and therefore lesser mechanical “effort” for the ventricle. It may therefore be inferred that the relative dissipation in the healthy circulation increases with age and/or BSA.
Also from Fig. 3, notice that the BT shunt group has a prominently lesser dissipative circulation than that of a normal child. This is attributed to the net reduction in overall resistance offered to the pumping ventricle due to the systemic to pulmonary shunt which reduces the volume overload of the single-ventricle. As an analogy, it is equivalent to a “short-circuit” that would result in high flow output from the ventricle. Although beneficial to the ventricle due to drastically reduced mechanical effort, this does not necessarily ensure a normal/appropriate balance of systemic-pulmonary flow ratio (Q p/Q s) and adequate oxygenation.
Comparison of CEDI between the younger Fontan patient group presented in Senzaki et al. 33 with that of normal children of about the same age shows that the average circulation for the Fontan groups was over 100% more dissipative (p < 0.001) (Fig. 3). This directly implies that the Fontan single ventricle needs to work twice as hard to achieve a desired cardiac output. However, when comparing this CEDI to that of normal adults, the mechanical effort in these Fontan ventricles is significantly lesser than that experienced by an adult ventricle.
CEDI comparison between the older Fontan patient group in Sundareswaran et al.37 with that from Senzaki et al.33 shows a stark difference (Fig. 3). The older Fontan patients have a CEDI three times that of younger Fontan patients in Senzaki et al.33 (p < 0.001) and over twice that of healthy adult CEDI. Given that CEDI is not dependent on the condition of the ventricle, clearly there exist remarkable differences in the dissipative characteristics of the circulation in Fontan patients with age. The reason behind the observed significant difference in CEDI magnitudes between the younger Fontan group and the older Fontan group, is further examined in Fig. 4.
From Fig. 4, it is clear that as with the normal circulation, the Fontan circulation also becomes more dissipative with age or BSA. However, the extent of increase in CEDI is clearly beyond 2 units. Now if one assumes that these patients received comparable care and treatment, it may be a valid hypothesis that the Fontan circulation gradually degrades with time. This fact provides the hemodynamic founding of the “palliative” (i.e. not curative) nature of the single-ventricle disease and can explain a number of the so-called “failed-Fontan” cases during third and forth decades of life.20 A seminal study by Fontan and Kirklin,12 based on clinical observations, demonstrate that the single ventricle circulation gradually degrades even after a perfect surgical operation and remain a hazard. As demonstrated here the prediction of this trend, independently, based solely on the new energetic indices deserves further attention. This finding together with our recent study that quantified the decrease in cardiac output38 once again highlights the importance of venous surgical resistance in the single-ventricle energy cascade and physiology.
Based on the mean CEDI value computed for the aortic stenosis group, it is important to note that at about a typical patient BSA of 1.0 m2 the condition of the Fontan circulation system may be considered as severe as that of a severe aortic stenosis group. While severe aortic stenosis patients have treatment options such as valve replacement, it is quite discomforting that the average Fontan patient of BSA 1.0 m2 (i.e. child less than 10 years age) is not considered for immediate intervention as there aren’t many treatment options other than cardiac transplantation, and a re-operation of the TCPC for optimization is still debated. Nevertheless, the data in Fig. 4 strongly suggests a need for improvements and bold innovation in single ventricle patient care.
AV-EDI
AV-EDI as defined (mathematically simply inverse squared of ELI), has the same positive predictive value as that of ELI. Nevertheless, through this new definition and linear association to energy, it has been demonstrated that moderate aortic stenosis has energy dissipation one order of magnitude higher than that for a normal aortic valve. Furthermore, the data (Fig. 5) also demonstrates that severe aortic stenosis has energy dissipation roughly twice that of moderate cases.
It is clear that although AV-EDI completely characterizes the severity of aortic stenosis, it does not predict the outcome of aortic valve replacement especially in certain low cardiac output patients who have a concomitant ventricular disease. To be able to assess the outcome of aortic valve replacement, AV-EDI needs to be compared with an independent and proper index characterizing the ventricular function.
TCPC-EDI
From Fig. 6 it is evident that there exists a clear and strong correlation between the LPA minimum size and energy dissipation in the TCPC irrespective of all other possible shape factors that varied between these six patients (R 2 = 0.88, p < 0.05). This observation is consistent with our earlier local CFD studies.31 Furthermore, note that the energy dissipation for the same patient (data points for constant cross-sectional area), which correspond to the variation of energy dissipation for the different flow conditions (resting and exercise conditions) do not exactly collapse to a single point. Given that influence of cardiac output is already taken into consideration by the non-dimensionalization, this lack of exact collapse implies that there exists a significant dependence with Reynolds number and other possible shape dependent parameters such as extra cardiac vs. intra atrial geometries. The overall scatter to either side of the power law fit depicts the dependence from all other shape factors and any measurement errors which will be improved by extending this analysis to more patients in future communications.
As illustrated again in Fig. 6, the exercise of applying the theoretical concepts developed in section Theoretical Analysis on a complex data set shows that it is extremely important to normalize physical data based on sound physical justification. As illustrated here a fundamental engineering concept, dimensional analysis, allows for establishing relationships between several variables associated with a complex dataset. Such cases are frequently observed in medical and clinical data, and performing statistical analysis alone may not provide the necessary correlations. The process of non-dimensionalization implicitly handles non-linear dependence between variables (e.g. energy dissipation was found to be proportional to the cube of cardiac output), and thus greatly lowers experimental “scatter” which is often mistaken for patient variability. The present example shows that even with a small data set, it is possible to achieve good statistical correlations provided the data is organized through a dimensionless formulation (Eq. 2).
Conclusion
The above theoretical analysis shows that the formulation of energy dissipation given in Eq. (2) indeed simplifies the complex physics of energy dissipation in human circulation that could be applied to various pathologies. This analysis allowed the formulation of the full circulation energy budget and the definition of new clinical indices: (1) circulation energy dissipation index (CEDI), (2) aortic valve energy dissipation index (AV-EDI) and (3), total cavopulmonary energy dissipation index (TCPC-EDI).
The introduction of CEDI and its application to previously published datasets on patients with varying circulatory pathologies and physiologies shows that the new index is an extremely powerful measure to quantify the overall “condition” of the systemic circulation. CEDI is a direct measure of energy efficiency and is insensitive to complex circuit arrangements where the ventricle itself could be the inefficient component. Figures 2–4 demonstrate how CEDI can be used to compare energy efficiencies between various diseases, including the complex single-ventricle physiologies all in a unified manner. For single ventricle patients, CEDI for the first time reveals a hemodynamic insight to the palliative nature of the Fontan procedure at the system level (Fig. 4).
The AV-EDI index was shown to be directly proportional to the energy dissipation across the aortic valve, and closely related to existing energy loss index (ELI). By definition the AV-EDI index has an equally positive predictive value as the traditional ELI in diagnosing the severity of aortic valve stenosis and directly gauges the level of energy dissipation in a stenosed aortic valve.
TCPC-EDI is introduced here as the index to quantify the efficiency of the TCPC connection. It is shown to be strongly correlated to one of the narrowest regions of the connection. Studies investigating the influence of secondary shape factors are in progress and planed for future communications.
References
Berger DS, Li JKJ, Noordergraaf A. Arterial Wave-Propagation Phenomena, Ventricular Work, and Power Dissipation. Annals of Biomedical Engineering. 1995;23(6):804–811. doi:10.1007/BF02584479
Blick EF, Stein PD. Work of Heart—General Thermodynamics Analysis. Journal of Biomechanics. 1977;10(9):589–595. doi:10.1016/0021-9290(77)90039-2
Buckingham E. On physically similar systems, illustrations of the use of dimensional equations. Physical Review. 1914;4(4):345–376. doi:10.1103/PhysRev.4.345
Burwash LG, Thomas DD, Sadahiro M, Pearlman AS, Verrier ED, Thomas R, Kraft CD, Otto CM. Dependence of Gorlin Formula and Continuity Equation Valve Areas on Transvalvular Volume Flow-Rate in Valvular Aortic-Stenosis. Circulation. 1994;89(2):827–835.
Carabello BA. Aortic stenosis - Two steps forward, one step back. Circulation. 2007;115(22):2799–2800. doi:10.1161/CIRCULATIONAHA.107.705848
Caro CG. Arterial fluid mechanics and artherogenesis. Recent Advances in Cardiovascular Disease. 1981;II:6–11.
Cebral JR, Castro MA, Burgess JE, Pergolizzi RS, Sheridan MJ, Putman CM. Characterization of cerebral aneurysms for assessing risk of rupture by using patient-specific computational hemodynamics models. American Journal of Neuroradiology. 2005;26(10):2550–2559.
de Zelicourt D, Pekkan K, Kitajima H, Frakes D, Yoganathan AP. Single-step stereolithography of complex anatomical models for optical flow measurements. Journal of Biomechanical Engineering-Transactions of the ASME. 2005;127(1):204–207. doi:10.1115/1.1835367
de Zelicourt DA, Pekkan K, Wills L, Kanter K, Forbess J, Sharma S, Fogel M, Yoganathan AP. In vitro flow analysis of a patient-specific intraatrial total cavopulmonary connection. Annals of Thoracic Surgery. 2005;79(6):2094–2102. doi:10.1016/j.athoracsur.2004.12.052
Ensley AE, Lynch P, Chatzimavroudis GP, Lucas C, Sharma S, Yoganathan AP. Toward designing the optimal total cavopulmonary connection: An in vitro study. Annals of Thoracic Surgery. 1999;68(4):1384–1390. doi:10.1016/S0003-4975(99)00560-3
Fontan F, Baudet E. Surgical Repair of Tricuspid Atresia. Thorax. 1971;26(3):240–248.
Fontan F, Kirklin JW, Fernandez G, Costa F, Naftel DC, Tritto F, Blackstone EH. Outcome after a Perfect Fontan Operation. Circulation. 1990;81(5):1520-1536.
Garcia D, Pibarot P, Dumesnil JG, Sakr F, Durand LG. Assessment of aortic valve stenosis severity - A new index based on the energy loss concept. Circulation. 2000;101(7):765–771.
Giddens DP, Zarins CK, Glagov S. The Role of Fluid-Mechanics in the Localization and Detection of Atherosclerosis. Journal of Biomechanical Engineering-Transactions of the Asme. 1993;115(4):588–594. doi:10.1115/1.2895545
Giroud JM, Jacobs JP. Fontan’s operation: evolution from a procedure to a process. Cardiology in the Young. 2006;16:67–71. doi:10.1017/S1047951105002350
Gorlin R, Gorlin SG. Hydraulic formula for calculation of area of stenotic mitral valve, other valves and central circulatory shunts. American Heart Journal. 1951;41(1):1–29. doi:10.1016/0002-8703(51)90002-6
Gould SJ. Allometry and Size in Ontogeny and Phylogeny. Biological Reviews of the Cambridge Philosophical Society. 1966;41(4):587-&. doi:10.1111/j.1469–185X.1966.tb01624.x
Hachicha Z, Dumesnil JG, Bogaty P, Pibarot P. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation. 2007;115(22):2856–2864. doi:10.1161/CIRCULATIONAHA.106.668681
Heinrich RS, Fontaine AA, Grimes RY, Sidhaye A, Yang S, Moore KE, Levine RA, Yoganathan AP. Experimental analysis of fluid mechanical energy losses in aortic valve stenosis: Importance of pressure recovery. Annals of Biomedical Engineering. 1996;24(6):685–694. doi:10.1007/BF02684181
Huddleston CB. The failing Fontan: options for surgical therapy. Pediatric Cardiology. 2007;28(6):472–476. doi:10.1007/s00246-007-9008-z
Huxley JS. Problems of Relative Growth. London: Methuen & Co., Ltd.; 1932.
Kameyama T, Asanoi H, Ishizaka S, Yamanishi K, Fujita M, Sasayama S. Energy-Conversion Efficiency in Human Left-Ventricle. Circulation. 1992;85(3):988–996.
Katajima, H. D. In Vitro Fluid Dynamics of Stereolithographic Single Ventricle Congenital Heart Defects from In Vivo Magnatic Resonance Imaging [PhD], Atlanta: School of Biomedical Engineering, Georgia Institute of Technology, 2007.
Khairy P, Poirier N, Mercier LA. Univentricular heart. Circulation. 2007;115(6):800–812. doi:10.1161/CIRCULATIONAHA.105.592378
Levine RA, Jimoh A, Cape E.G, McMillan S, Yoganathan AP, Weyman AE. Pressure Recovery Distal to a Stenosis - Potential Cause of Gradient Overestimation by Doppler Echocardiography. Journal of the American College of Cardiology. 1989;13(3):706–715.
Liu HD, Narusawa U. Flow-induced endothelial surface reorganization and minimization of entropy generation rate. Journal of Biomechanical Engineering-Transactions of the Asme. 2004;126(3):346–350. doi:10.1115/1.1762895
Nerem RM. Vascular Fluid-Mechanics, the Arterial-Wall, and Atherosclerosis. Journal of Biomechanical Engineering-Transactions of the Asme. 1992;114(3):274–282. doi:10.1115/1.2891384
Painter, P., P. Eden, and H.-U. Bengtsson. Pulsatile blood flow, shear force, energy dissipation and Murray’s Law. Theor. Biol. Med. Model. 3:31, 2006.
Pedley TJ. Mathematical modelling of arterial fluid dynamics. Journal of Engineering Mathematics. 2003;47(3–4):419–444. doi:10.1023/B:ENGI.0000007978.33352.59
Pekkan K, De Zelicourt D, Ge L, Sotiropoulos F, Frakes D, Fogel MA, Yoganathan AP. Physics-driven CFD modeling of complex anatomical cardiovascular flows - A TCPC case study. Annals of Biomedical Engineering. 2005;33(3):284–300. doi:10.1007/s10439-005-1731-0
Pekkan K, Kitajima HD, de Zelicourt D, Forbess JM, Parks WJ, Fogel MA, Sharma S, Kanter KR, Frakes D, Yoganathan AP. Total cavopulmonary connection flow with functional left pulmonary artery stenosis - Angioplasty and fenestration in vitro. Circulation. 2005;112(21):3264–3271. doi:10.1161/CIRCULATIONAHA.104.530931
Peskin CS, McQueen DM. Cardiac Fluid-Dynamics. Critical Reviews in Biomedical Engineering. 1992;20(5–6):451-&.
Senzaki H, Masutani S, Kobayashi J, Kobayashi T, Sasaki N, Asano H, Kyo S, Yokote Y, Ishizawa A. Ventricular afterload and ventricular work in Fontan circulation - Comparison with normal two-ventricle circulation and single-ventricle circulation with Blalock-Taussig shunts. Circulation. 2002;105(24):2885–2892. doi:10.1161/01.CIR.0000018621.96210.72
Sluysmans T, Colan SD. Theoretical and empirical derivation of cardiovascular allometric relationships in children. Journal of Applied Physiology. 2005;99(2):445–457. doi:10.1152/japplphysiol.01144.2004
Soerensen DD, Pekkan K, de Zelicourt D, Sharma S, Kanter K, Fogel M, Yoganathan AP. Introduction of a new optimized total cavopulmonary connection. Annals of Thoracic Surgery. 2007;83(6):2182–2190. doi:10.1016/j.athoracsur.2006.12.079
Steinman DA. Image-based computational fluid dynamics modeling in realistic arterial geometries. Annals of Biomedical Engineering. 2002;30(4):483–497. doi:10.1114/1.1467679
Sundareswaran KS, Kanter KR, Kitajima HD, Krishnankutty R, Sabatier JF, Parks WJ, Sharma S, Yoganathan AP, Fogel M. Impaired power output and cardiac index with hypoplastic left heart syndrome: A magnetic resonance imaging study. Annals of Thoracic Surgery. 2006;82(4):1267–1277. doi:10.1016/j.athoracsur.2006.05.020
Sundareswaran, K. S., K. Pekkan, L. P. Dasi, H. D. Kitajima, K. Whitehead, M. A. Fogel, and A. P. Yoganathan. Significant impact of the total cavopulmonary connection resistance on cardiac output and exercise performance in single ventricles. Circulation 116(16_MeetingAbstracts):II_479-c, 2007.
Tang BT, Cheng CP, Draney MT, Wilson NM, Tsao PS, Herfkens RJ, Taylor CA. Abdominal aortic hemodynamics in young healthy adults at rest and during lower limb exercise: quantification using image-based computer modeling. American Journal of Physiology-Heart and Circulatory Physiology. 2006;291(2):H668-H676. doi:10.1152/ajpheart.01301.2005
Wang C, Pekkan K, de Zelicourt D, Horner M, Parihar A, Kulkarni A, Yoganathan AP. Progress in the CFD modeling of flow instabilities in anatomical total cavopulmonary connections. Annals of Biomedical Engineering. 2007;35(11):1840–1856. doi:10.1007/s10439-007-9356-0
Whitehead KK, Pekkan K, Kitajima HD, Paridon SM, Yoganathan AP, Fogel MA. Nonlinear power loss during exercise in single-ventricle patients after the Fontan - Insights from computational fluid dynamics. Circulation. 2007;116(11):I165-I171. doi:10.1161/CIRCULATIONAHA.106.680827
Wood NB. Aspects of fluid dynamics applied to the larger arteries. Journal of Theoretical Biology. 1999;199(2):137–161. doi:10.1006/jtbi.1999.0953
Acknowledgement
The authors gratefully acknowledge the Bioengineering Research Partnership (BRP) grant from NIH (HL67622).
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Dimensional Analysis
Re-writing Eq. (1) in the general form:
With each of the variable with the following dimensions:
According to the Buckingham π theorem,3 any relationship between n variables spanning d dimensions may be reduced to an equivalent relationship between k = n − d dimensionless groups π1, π2,…, π k . Equation (1) has six variables spanning three dimensions (i.e. mass, [M], length, [L], and time, [T], dimensions). Therefore, it can be expressed as a relationship between 6 − 3 = 3 dimensionless variables given as:
Choosing Q, ρ, and BSA as our fundamental variables that span M, L, and T, we can obtain a specific form for Eq. (A2) by solving the following equations:
Solving for Eq. (A3) for a 1, b 1, c 1:
Gives: \( a_{1} = - 1,b_{1} = 0,c_{1} = \frac{1}{2} \)
Solving for Eq. (A4) for a 2, b 2, c 2
Gives: a 2 = −3, b 2 = −1, c 2 = 2
And finally solving Eq. (A5) for a 3, b 3, c 3 gives a 3 = 0, b 3 = 0, c 3 = 0, as S by definition is dimensionless.
Therefore the specific forms of the three dimensionless groups are::
Examination of Π1 indicates that it is a form of a special Reynolds number, \( Re = \frac{{Q \times BSA^{ - 1/2} }}{\upsilon }, \) where the characteristic velocity scale is \( Q/BSA, \) and the characteristic length scale is \( \sqrt {BSA}. \) Reynolds number is always an important dimensionless group for any fluid flow problem dictating the dependence on the fluid flow regime (i.e. laminar, to turbulence).
Examination of Π2 indicates that the energy dissipation rate has been non-dimensionalized by a “body-level” kinetic energy scale given by \( \rho \frac{{Q^{3} }}{{BSA^{2} }} \).
The shape variable, S, is by definition dimensionless and thus is directly third dimensionless group without need for non-dimensionalization.
Solving for Π2 in Eq. (A2) and using results (A12)–(A14) finally gives:
Rights and permissions
About this article
Cite this article
Dasi, L.P., Pekkan, K., de Zelicourt, D. et al. Hemodynamic Energy Dissipation in the Cardiovascular System: Generalized Theoretical Analysis on Disease States. Ann Biomed Eng 37, 661–673 (2009). https://doi.org/10.1007/s10439-009-9650-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-009-9650-0