Abstract
Determinations of Human chorionic gonadotropin (HCG) are important for diagnosis and monitoring of pregnancy, pregnancy-related diseases and several types of cancers. As a step toward decentralized diagnostic systems, we introduce a format of particle-based immunoassays relying on digital microfluidics (DMF) and magnetic forces to separate and resuspend HCG antibody-coated paramagnetic particles. On this basis, we developed DMF diagnostic platform for automated HCG detection and realized droplet operations at 20 Hz. Using this platform, 10–50 µg/mL of HCG was detected by chemiluminescence method and the linear relationship between HCG concentrations and chemiluminescence signals was obtained. To solve the biofouling problem, we use pluronic additives in reagent droplets. The effect of different additive concentrations on droplet actuation was tested. The DMF immunoassays only take 20 min to finish the whole sample detection process. We propose that the new technique has great potential for eventual use in a fast, low-waste, and inexpensive instrument for the quantitative analysis of proteins and small molecules in low sample volumes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
During early pregnancy, HCG stimulates progesterone production in the corpus luteum. Determinations of HCG are important for diagnosis and monitoring of pregnancy, pregnancy-related diseases and several types of cancer (Stenman et al. 2006; Lee and Han 2010). It is also an extremely sensitive and specific marker for trophoblastic tumors of placental and germ cell origin (Yang et al. 2010). In traditional centralized model, HCG is almost always diagnosed in central clinical laboratories, making it cost-prohibitive in resource-limited settings. In remote regions, transportation from rural communities to laboratories becomes cost prohibitive and time consuming, representing a major obstacle to meet the large needs for HCG detection.
Given the challenge described above, there is great enthusiasm for developing decentralized systems for disease diagnosis and surveillance. This model requires portable assays, and the microfluidic (or “lab on a chip”) community has attempted to address this challenge primarily through systems that rely on fluid flow through enclosed microchannels. In recent years, the microfluidic method has been applied to the rapid analysis of life sciences due to its advantages of being portable, low energy consumption, easy preparation and operation. Hung and Chang (2015) designed a simple microfluidic chip for plasma separation and then observed the fluorescent spots under fluorescent microscope for detecting HCG. Yang et al. (2010) separated β-HCG from fibrinogen using a MEMS size exclusion chromatography column. Zhu and Trau (2012) developed a microparticle array for simultaneous detection of HCG. Although these chips have proved to be able to complete the rapid detection of HCG and have a good detection sensitivity, there are still some limitations. In these microchannel-based methods, HCG was detected off-chip, and these chips have a low degree of automation and require manual operations to move these chips for in vitro detection. Furthermore, These detection chips require mechanical components (micro-pumps, micro-valves, etc.) to drive, adding to the complexity of integrating the measurement components and sample introduction components.
On the other hand, digital microfluidics (DMF) have been proved to be effective detection methods for immunoassays. DMF platform manipulates individual droplets instead of continuous flows and possesses the advantages of high flexibility and fully automated process. Digital microfluidics is also capable of realizing complex fluid operations. For example, some biological assays require washing steps, in which reagents from a first reaction must be completely removed before a new set of reagents is introduced. Such heterogeneous assays are difficult to perform inside fluidic channels, but a washing step can be easily done on digital microfluidic chips (Lee and Han 2010; Sista et al. 2011). In the past decade, significant effort has been focused on developing DMF immunoassays. In the study conducted by Ng et al. (2015), a complete sample preparation was performed on the chip for the detection of rubella infection and immunity, and the chip was placed under a chemiluminescence device for detection. Abdulwahab et al. (2017) report a technique for the rapid determination of patient response to aromatase inhibitor therapy (AIT): an integrated, portable digital microfluidic platform that allows quantification of estradiol (E2) in core needle biopsy (CNB) samples. Although these advantages have motivated the development of DMF-powered immunoassays for small-molecule and protein biomarkers, we are not aware of DMF immunoassays being used for HCG detection.
Here, we use a format of particle-based immunoassays relying on DMF to achieve fast HCG detection. These assays use HCG antibodies-immobilized magnetic particles to capture the analyte from the sample and enzyme-linked antibodies to transduce analyte-binding events to chemiluminescent signal. The whole process, including chemiluminescence detection, is achieved on-chip automatically. The use of magnetic particles as solid support is attractive as this approach offers a dramatic increase in the surface-area-to-volume ratio and serves as a simple mechanism to reproducibly deliver antibodies into a microfluidic device. Furthermore, the use of chemiluminescence is particularly advantageous because few optical components are required (e.g., no excitation source, filters, or lenses). We propose that this approach represents a useful step toward the development of fast, low-waste, and inexpensive instrument for the quantitative analysis of proteins in low sample volumes.
2 Experiment
2.1 DMF chip design and fabrication
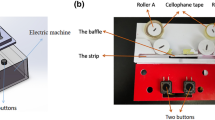
The DMF chip consists of two parallel substrates with the droplet sandwiched inbetween (Wang and Jones 2015). An array of individually addressable electrodes is patterned on the bottom substrate, on top of which we coat a dielectric layer and a hydrophobic layer. The top substrate, with a transparent conductive coating, serves as a continuous ground electrode, and we coat a hydrophobic layer on top of this electrode. We fabricate the chip on a glass substrate and the layout of bottom electrodes is shown in Fig. 1a. There are three components in the bottom electrodes including connecting pads, on-chip reservoirs and reaction region. Through the connecting pads, the driving voltage is loaded into the individual electrodes in reaction region. The sample, reagents and other solutions are stored in the on-chip reservoirs at the very beginning. Droplets are dispensed, delivered to the reaction region for immunoassay. All processes including chemiluminescence detection are automatically completed on-chip. The size of each electrode in the branches is 1 mm. The spacing between two neighboring electrodes is 40 µm. A pogo pin connector is used to connect the DMF chip to voltage control circuits (Fig. 1b).
The digital microfluidic chip. a Top view of the DMF device, showing 6 reservoirs to accommodate reagents, 36 actuation electrodes to carry out the immunoassay protocol and detection steps, 40 connecting pads to load the driving voltage to actuation electrodes. b Self made pogo pin connector, witch is used to connect DMF chip to voltage control circuits
The fabrication process is schematically shown in Fig. 2. The glass substrate cleaned with acetone and isopropanol was first sputtered with a 200 nm Al film. Then the Al film was patterned into a two-dimensional electrode array by standard lithography process and wet etching. Subsequently, a 3 µm Parylene layer was coated on top of the electrodes. The Parylene surface was then coated with a 100 nm Teflon-AF layer to finish the process of the bottom plate. An ITO glass coated with Teflon-AF film was used as the top plate and connected to the bottom plate by double sided tapes, the thickness of the double sides tapes was 100 µm.
2.2 HCG immunoassay and on-chip detection
2.2.1 Reagents and materials
Reagents used HCG ELISA were purchased from Zhaorui bio-tech Co. (Shanghai, China). Paramagnetic particles were purchased from So-Fe Biomedical Co. (Shanghai, China). Pluronic L64, comprising stable peroxide (H2O2) and luminol solution were purchased from Sigma Chemical. Deionized (DI) water used in our experiments has a resistivity of 18 MΩ cm at 25 °C. Photomultiplier tube (PMT) was purchased from Hamamatsu Co. (Hamamatsu, Japan).
2.2.2 DMF immunoassay
Using the particle separation and resuspension techniques, we propose a DMF indirect ELISA for HCG. As shown in Fig. 3, HCG antibody-coated magnetic particles (Sista et al. 2008a, b; Vergauwe et al. 2011) is used to capture the analyte from the sample. After incubation and washing, HRP-conjugated antibody HCG is added to form double antibody sandwich immunocomplexes. After another incubation and washing, H2O2 and Luminol are added to the particles, and the resulting chemiluminescence is measured as relative light units (RLUs) using photomultiplier tube (PMT) on-chip.
Before experiments, HCG antibody-immobilized magnetic particles were prepared off-chip and bovine serum albumin (BSA) was added to block the active group on the surface of magnetic particles. The use of magnetic particles as solid support is attractive as this approach offers a dramatic increase in the surface-area-to-volume ratio, the magnetic particles serve as a simple mechanism to reproducibly deliver antibodies into a microfluidic device.
An important step in HCG immunoassays is the process of removing unbound reagents from the magnetic particles. Here, we successfully achieved on-chip particle separation and resuspension as shown in Fig. 4. This process is capable of removing greater than 90% of unbound reagents in one washing step (Ng et al. 2012). We used 1 µm diameter paramagnetic particles for HCG immunoassays, and a cube magnet with suitable size was used to separate the particles from the diluent.
3 Results and discussion
3.1 Droplet actuation and on-chip assay
3.1.1 Droplet movement and biofouling
In our system, droplets were formed by on-chip dispensing process. We investigated time sequences of activating electrodes to optimize droplet generation. The driving power was set to be 110 V, 50 Hz in our experiment. We demonstrated repeatable DI water droplet generation on our automated system and the highest generation rate we obtained was about 20 Hz. The sequence of steps for droplet generation and combination was shown in Fig. 5.
In digital microfluidics, the movement of droplets is impeded by drag force arising from differential surface energy. Many of the reagents used for immunoassays locally increases the surface energy (Yoon and Garrell 2003), impeding the movement of aqueous droplets. To solve the biofouling problem, we use pluronic additives in reagent droplets (Au et al. 2011).The effect of different additive concentrations on droplet actuation was tested and shown in Fig. 6. Concentrations from 0.05% (v/v) to 0.14% (v/v) of Pluronic L64 were added to the droplet containing 3 µg/mL HCG. Each concentration was evaluated three times on different devices. During each test, a 0.1 µL droplet was actuated between three adjacent electrodes. The speed of the droplets was observed to decrease over time. Device failure was defined as any case in which a droplet required more than 10 s to complete a movement step from one electrode to the next. The time until device failure were recorded for each condition. The error bars represent the standard deviation between three measurements performed on-chip. Error bars are ± 1 SD. In this work, all regents used on DMF devices were supplemented with Pluronic L64 at 0.11% to facilitate droplet operations.
3.1.2 DMF HCG immunoassay
The assay described here was designed for the detection of HCG in patient serum. To optimize and calibrate the method, we used HCG antigen solution to simulate human serum. HCG antigens were detected on-chip with a 7-step indirect ELISA procedure (Fig. 7). (a) A drop of HCG antibody-immobilized magnetic particle (10 mg/mL) suspension was dispensed from a reservoir, and the particles were separated from the diluent. (b) A droplet of sample containing HCG antigen was dispensed, delivered to the particles, mixed for 6 min, and separated from particles. (c) The particles were washed in 4 successive droplets of wash buffer. (d) A droplet of HRP-conjugated HCG antibody (20 µg/mL) was dispensed, delivered to the particles, and mixed for 4 min. (e) Step c was repeated. (f) A droplet of H2O2 (0.1 M) and Luminol (0.02 M) solution was dispended and merged with the particles; the solutions and particles were mixed for 10 s. (g) The mean chemiluminescent signal over 5 s was obtained with the integrated PMT on-chip. All immunoassay processes including chemiluminescence detection were automatically completed on-chip within 20 min. After that, chemiluminescence signal was successfully obtained on detection zone. To detect the chemiluminescence intensity, PMT was automatically moved to the top of the on-chip detection zones to collect optical signals. We obtained the relationship between the chemiluminescence intensity and electrical signals (Fig. 8). Using DMF chip, 10–50 µg/mL of HCG was detected by chemiluminescence method. The signal intensity at a solution concentration of 0 indicates background noise.
Video sequence of on-chip HCG immunoassay procedure. a HCG antibody-immobilized magnetic particles are separated. b HCG sample reconstituted the particles and incubated. c After washing steps, droplet of HRP-conjugated HCG antibody reconstituted the particles and incubated. d After washing steps, a droplet of H2O2 and Luminol solution reconstituted the particles to activate enzymatic reaction and chemiluminescence is measured in detection zones by using PMT on-chip automatically
3.2 Process time
The whole process time is mainly determined by the two incubation times in the on-chip immunoassay process—the conjugate incubation time and the HCG antigen incubation time. We optimized the incubation times through an experiment study of the chemiluminescence signal at different incubation stages. By setting the HCG antigen incubation time long enough (7 min), we tested the chemiluminescence signal at different conjugate incubation times, as shown in Fig. 9a. As can be seen it takes at least 200 s to complete conjugate incubation. Similarly, the chemiluminescence signal was tested at different HCG antigen incubation times, in this case, the conjugate incubation time was set to be 5 min (Fig. 9b). Accordingly, it takes at least 400 s to complete the HCG immune response. As a result, in our DMF HCG immunoassay we set the conjugate and HCG antigen incubation time as 4 min and 6 min respectively. But still the whole immunoassay processes including on-chip chemiluminescence detection can be completed within 20 min.
3.3 Detection accuracy
The result in Fig. 8 shows a general linear profile, but there are variations at some data points. We suspect two main influencing factors for these variations: biofouling and particle aggregation. (1) DMF surface is typically formed from a hydrophobic material such as Teflon-AF, it is quite prone to biofouling because of its hydrophobicity (Luk et al. 2008). The use of Pluronic L64 solves this issue at low reagent concentrations, but there are still biofouling at increased concentrations, such as 50 µg/mL. This result indicates that pre-dilution would be required when detecting high concentration samples. (2) Aggregation effect of magnetic particles is another factor to influence the detection result. During the experiment, it is possible that the magnetic particles be aggregated together when the particles were modified with antigens and antibodies, see Fig. 10. As a result part of HRP-conjugated HCG antibody will be unable to participate in chemiluminescence reaction. This problem can be effectively alleviated by applying a varied magnetic field, this perturbation can increase the dispersion of magnetic particles to desired resuspension as shown in Fig. 10b. In our future research, we will develop an motor controlled magnet to automatically apply varied magnetic field in the particle resuspension step.
The lower limit of our current system for HCG detection is 1 µg/mL. The chemiluminescence signal at lower than this concentration cannot be successfully detected. This detection limit needs further improvement. There are some factors to affect the result. (1) Adding enhancers was a method to strengthen luminescence signals (Chen et al. 2017). HRP–luminol chemiluminescence reaction was performed as follows: luminol catalyzed to the ground state by HRP and an enhancer in alkaline and oxidant condition was accompanied by light quantum emission. Sakharov and Vdovenko (2013) have proposed hypothesis of the mechanism of co-enhancer. In the mechanism of co-enhancer based on the mechanism of HRP–luminol-based chemiluminescence reaction, the secondary enhancer accelerates peroxidase-catalyzed primary enhancer by hydrogen peroxide to produce cation radical for increasing chemiluminescence intensity. (2) In the experiment, we also found that increasing the volume of the reaction solution in a certain range can increase the intensity of chemiluminescence. It needs to design larger driving electrodes by optimizing the chip structure parameters, this part of content needs additional research.
The relative standard deviation (RSD) of DMF approach was ranging from 9 to 12% for the HCG detection assay. The advantage of automatic detection is significant, as the multiple containers and manual sample handling can lead to loss of sample and introduction of contaminants. In addition, the automation of DMF would eliminate the human error introduced by technicians working in different laboratories. In previously reported results (Liu et al. 2009) using off-chip protocol, the reaction process and the washing process required large amount of samples of 920 µL. The total time to achieve detection result was approximately over 1 h. In this work, the on-chip protocol is shown to achieve better performance. The required sample volume is reduced to 7 µL, and the total time to result is within 20 min.
The results described above demonstrate that DMF can be used to implement particle-based immunoassays with very high performance. With reduced reagent consumption and analysis time, DMF devices outperformed standard well-plate ELISA, and resulted in significant improvements in assay sensitivity. We developed the methods of quantitative analysis of proteins, which has great potential for eventual use in a fast, low-waste, and inexpensive instrument for the point-of-care testing devices.
4 Conclusions
We have completed the particle-based immunoassay on DMF without the aid of oil carrier fluid. This format allowed the realization of on-chip particle separation and resuspension which is capable of removing greater than 90% of unbound reagents in one step. Using this method, we successfully obtained the linear relationship between the HCG antigen concentration and the chemiluminescence signal. Compared to conventional technique, this method reduced reagent volumes and analysis time by 100-fold and 10-fold, respectively. We propose that the new technique has great potential for a fast, low-waste, and inexpensive instrument for the quantitative analysis of proteins in low sample volumes.
References
Abdulwahab S, Ng AH, Dean CM et al (2017) Towards a personalized approach to aromatase inhibitor therapy: a digital microfluidic platform for rapid analysis of estradiol in core-needle-biopsies. Lab Chip 17(9):1594–1602
Au SH, Kumar P, Wheeler AR (2011) A new angle on pluronic additives: advancing droplets and understanding in digital microfluidics. Langmuir ACS J Surf Colloids 27(13):8586–8594
Chen G, Jin MJ, Du PF et al (2017) A review of enhancers for chemiluminescence enzyme immunoassay. Food Agric Immunol 28(2):315–327
Hung MS, Chang HY (2015) A simple microfluidics for real-time plasma separation and hCG detection from whole blood. J Chinese Inst Eng 38(6):685–691
Lee JH, Han J (2010) Concentration-enhanced rapid detection of human chorionic gonadotropin (hCG) on a Au surface using a nanofluidic preconcentrator. Microfluid Nanofluid 9(4-5):973–979
Lee J, Moon H, Schoellhammer T, Kim CJ (2002) Electrowetting and electrowetting-on-die-lectric for microscale liquid handling. Sens Actuators A Phys 95(2):259–268
Liu JT, Liu RP, Wang MX, Liu CX, Luo JP, Cai XX (2009) Detection of human chorionic gonadotropin by highly sensitive magnetic enzyme-linked chemiluminescent immunoassay. Chin J Anal Chem 37(7):985–988
Luk VN, Mo G, Wheeler AR (2008) Pluronic additives: a solution to sticky problems in digital microfluidics. Langmuir 24(12):6382–6389
Ng AH, Choi K, Lobinson JM, Wheeler AR (2012) Digital microfluidic magnetic separation for particle-based immunoassays. Anal Chem 84(20):8805–8812
Ng AH, Lee M, Choi K, Fischer AT, Robinson JM, Wheeler AR (2015) Digital microfluidic platform for the detection of rubella infection and immunity: a proof of concept. Clin Chem 61(2):420–429
Sakharov IY, Vdovenko MM (2013) Mechanism of action of 4-dialkylaminopyridines as secondary enhancers in enhanced chemiluminescence reaction. Anal Biochem 434(1):12–14
Sista R, Hua Z, Thwar P, Sudarsan A, Srinivasan V, Eckhardt A, Pollack M, Pamula V (2008a) Development of a digital microfluidic platform for point of care testing. Lab Chip 8(12):2091–2104
Sista RS, Eckhardt AE, Srinivasan V, Pollack MG, Pamula VK (2008b) Heterogeneous immunoassays using magnetic beads on a digital microfluidic platform. Lab on a Chip 8(12):2188
Sista RS, Eckhardt AE, Wang T et al (2011) Digital microfluidic platform for multiplexing enzyme assays: implications for lysosomal storage disease screening in newborns. Clin Chem 57(10):1444
Stenman UH, Tiitinen A, Alfthan H, Valmu L (2006) The classification, functions and clinical use of different isoforms of HCG. Hum Reprod Update 12:769–784
Vergauwe N, Witters D, Ceyssens F, Vermeir S, Verbruggen B, Puers R, Lammertyn J (2011) A versatile electrowetting-based digital microfluidic platform for quantitative homogeneous and heterogeneous bio-assays. J Micromech Microeng 21(5):054026
Wang W, Jones TB (2015) Moving droplets between closed and open microfluidic systems. Lab Chip 15(10):2201
Yang Y, Choi S, Chae J (2010) Separation of beta-human chorionic gonadotropin from fibrinogen using a MEMS size exclusion chromatography column. Microfluid Nanofluid 8.4:477–484
Yoon JY, Garrell RL (2003) Preventing biomolecular adsorption in electrowetting-based biofluidic chips. Anal Chem 75(19):5097
Zhu Q, Trau D (2012) Multiplex detection platform for tumor markers and glucose in serum based on a microfluidic microparticle array. Anal Chim Acta 751(751):146–154
Acknowledgements
This work was supported by National Science Foundation (no. 61504060), and by the Fundamental Research Funds for the Central Universities (30915118835, 30916011201, 30915011302).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the topical collection “2018 International Conference of Microfluidics, Nanofluidics and Lab-on-a-Chip, Beijing, China” guest edited by Guoqing Hu, Ting Si and Zhaomiao Liu
Rights and permissions
About this article
Cite this article
Piao, Y., Wang, X., Xia, H. et al. Digital microfluidic platform for automated detection of human chorionic gonadotropin. Microfluid Nanofluid 23, 1 (2019). https://doi.org/10.1007/s10404-018-2168-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10404-018-2168-8