Abstract
The formation of three-dimensional (3D) multicellular cell spheroids such as microspheres and embryoid bodies has recently gained much attention as a useful cell culture technique, but few studies have investigated the suitability of glass for spheroids formation and culture. In this work, we present a novel three-dimensional microfluidic device made of poly(dimethylsiloxane) (PDMS) and glass for the easy and rapid synthesis and culture of tumor spheroid. The cell culture unit is composed of an array of microwells on the bottom of a glass plate, bigger microwells and elastomeric microchannels on the top of a PDMS plate. Cell suspension can be easily introduced into the cell culture unit and exchange with the external liquid environment by the microfluidic channels. A single tumor spheroid can be formed and cultured in each glass cell culture chamber, the surface of which was modified with poly(vinyl alcohol) to render it to be resistant to cell adhesion. As the cell culture medium could be replaced, spheroids of the human breast cancer (MCF-7) cells were cultured on the chip for 3 days, reaching the diameters of about 150 μm. Furthermore, the MCF-7 cells were successfully cultured on the chip in 2D and 3D culture modes. Results have shown that glass is well suitable for multicellular tumor spheroids culture. The established platform provides a convenient and rapid method for tumor spheroid culture, which is also adaptable for anticancer drug screening and fundamental biomedical research in cell biology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In vitro cell culture has become one of the most important tools for modern biology research. Cells in all living tissues interact with their neighboring cells, soluble factors or the extracellular matrix (ECM) and communicate to establish unique functions. Generally, the majority of cell culture systems were based on rigid two-dimensional (2D) substrates (Liu et al. 2010; Sahai et al. 2011); however, the 2D cell culture systems could not fully match the in vivo cellular microenvironment and mimic some tissue-specific properties of cells (El-Ali et al. 2006; Gao et al. 2012). Recently, researchers have attempted to reduce this gap between cell-based and animal-based studies by developing efficient three-dimensional (3D) cell culture systems. Moreover, 3D cell culture provides more accurate in vivo microenvironments compared with 2D monolayer culture, and a number of studies also verify that 3D culture gene expression profiles have been shown to reflect clinical expression profiles more accurately than those observed in 2D cultures (Kim 2005; Birgersdotter et al. 2005; Yamada and Cukierman 2007). The most common strategy for 3D cell culture was to embed cells in 3D natural or synthetic hydrogels (Kelm et al. 2003; Chen et al. 2010a; Gao et al. 2010; Yoon et al. 2013; Yu et al. 2010; Shi et al. 2013; Kalchman et al. 2013). In 3D cell culture research, hydrogels have been widely used for cell encapsulation and cell culture. However, the most significant challenge for the 3D cell culture system is the limitation of mass transport properties. Inadequate transport of nutrients and waste would decrease tissue quality, cellular metabolic activity and cellular viability. There are several disadvantages that may affect 3D cell culture encapsulated inside hydrogels; for example, transportation of oxygen and nutrients through dense hydrogels may need external mechanical force and the hydrogel-encapsulation models may not be ideal for cell-dense or ECM-poor cells (Gao et al. 2012; Ozawa et al. 2013).
Spheroid culture, the simplest and most feasible 3D cell culture method without using hydrogels, has been chosen as a culture model to mimic and study 3D cell culture (Torisawa et al. 2007). Compared with conventional monolayer culture, the 3D multicellular spheroids could display their unique microenvironment inside a spheroid that simulates more accurately the in vivo microenvironment by reproducing nutrient and signal gradients and by removing the effect of unnatural adhesion to the modified surfaces, so they have higher resistivity to chemicals used during chemotherapy (Yoon et al. 2013). Consequently, the tumor spheroid model is considered to be efficient since it has been used in cancer research for more than 40 years and is currently used in combinatorial therapy-oriented studies (Hirschhaeuser et al. 2010). Tumor spheroids are generated conventionally by continuous agitation of cell suspensions (Agastin et al. 2011; Sakai et al. 2010), cellular aggregation by sedimentation on non-adherent surfaces (Hsiao et al. 2009; Ziolkowska et al. 2012, 2013), microfabricated structures (Wu et al. 2008; Jin et al. 2011) and hanging-drop (HD) method (Wlodkowic et al. 2009; Kim et al. 2012a). These methods all have their unique advantages and disadvantages for forming tumor spheroids. For example, the hanging-drop method has been widely used for the formation of 3D tumor spheroids in biomedical cancer research. However, this method should be extracted and seeded into other culture devices to implement the perfusion culture of spheroids and requires additional off-chip processes of spheroid formation and extraction (Kim et al. 2012b). Moreover, it is incapable of precise control of spheroid size and not amenable to automation for massive and parallel production of spheroids. Therefore, there is no consensus on the method of choice for optimal formation of tumor spheroids, and a variety of alternative methods are still being developed in 3D culture systems.
In recent years, a number of microfluidic chips have been developed for on chip formation of 3D tumor spheroids. These systems have a relatively short history in cell culture but have gained interest from researchers in the biomedical research field because of its ability to produce precise control of the desired product in an extremely small and confined space (Wu et al. 2008; Karp et al. 2007; Sakai and Nakazawa 2007; Hsiao et al. 2009). Microfluidic chips provide a possibility for single spheroid culture, observation and analysis, which is particularly useful for research on cancer tumor physiology. Spheroid formation on chip is a challenging task, so the proposed solutions required sophisticated fabrication methods, which can entail limitations for widespread use of such systems (Ziolkowska et al. 2013). And it is important for tumor spheroid culture to generate uniform spheroids or control the spheroid diameter. Microdevices for generating uniform and massive spheroids have been demonstrated including microwell arrays and non-adherent micropatterns. The microwell array system results in an improvement in homogeneous mass production of cell aggregates, which allows for high throughput measurements using the aggregates. Microwell arrays are frequently fabricated by polyethylene glycol (PEG) (Karp et al. 2007; Mori et al. 2008), PMMA (Sakai et al. 2010) or PDMS (Wong et al. 2011; Ziolkowska et al. 2013). Microwell array and micropatterning are highly effective in massive formation of tumor spheroids, but it has limitations in subsequent cytotoxicity assays for selective drug treatment due to lack of fluidic channels (Kim et al. 2012a). However, to date, few studies have investigated the suitability of glass microwells for tumor spheroid formation and culture.
In this paper, we developed a novel microfluidic system to form and culture tumor spheroid. By using PDMS–glass hybrid chip, we formed a stable and self-contained system for 3D cell culture. The system consisted of an array of microwells and rigid microchannels on the bottom of glass plate and bigger microwells and elastomeric microchannels on the top of PDMS plate. The system was fabricated by the new method of two-step wet etching in glass and a plate of copper alloy for the master mold of PDMS. It is capable of forming multicellular tumor spheroid quickly, changing culture medium for long-term cell culture, and preforming drug testing. On the contrary to spheroid chips previously presented (Ziolkowska et al. 2012), the present chip provides quick spheroid formation and creates uniform spheroids using glass microwells array. Importantly, we show that glass wells are well suited for MCF-7 cells for long-term spheroid culture based on the cell viability and growth assays. MCF-7 cells were successfully cultured on the microfluidic chip in 2D and 3D culture modes. In this sense, this microfluidic device has great potential for anticancer drug screening.
2 Experimental
2.1 Reagents and apparatus
Polydimethylsiloxane (PDMS) elastomer and Sylgard 184 curing agent were both purchased from Dow Corning (Midland, MI, USA). SG2506WC glass (6.35 × 6.35 cm2, with predeposit 145-nm-thick chromium layer and 570-nm-thick S-1805 photoresist) was from Changsha Shaoguang Chrome Blank Co. Ltd. (Changsha, China). MCF-7 cells were kindly provided by Ph.D. candidate Lu Jing from Department of Pharmacology and Toxicology in Sun Yat-sen University (Guangzhou, China), and were grown in the Dulbecco’s modified Eagle’s medium (DMEM) with penicillin, streptomycin, l-glutamine and fugizone that were purchased from Gibco (Gibco Invitrogen Corporation, USA). Fetal bovine serum (FBS), trypsin–EDTA and phosphate buffered saline (PBS) were also obtained from Gibco (Gibco Invitrogen Corporation, USA). Acridine orange (AO) and ethidium bromide (EB) were obtained from SangGon (Sangon Biotech, Shanghai, China). Poly(vinyl alcohol) (PVA) was obtained from Aladdin Reagent (Shanghai, China). Ultrapure (18.2 MΩ cm) was made by on Millipore Simplicity system (Millipore, Bedford, MA, USA), and used for preparation of all aqueous solutions.
A PDC-32G plasma cleaner from Harrick Plasma (Harrick Plasma, USA) was applied to bond PDMS and glass chips. Syringe pump (Model TS-1A, Longer pump Corporation, Baoding, China) was applied for liquid manipulation. A home-made incubator is applied for temperature control when exchanging the medium in the microdevice. An inverted fluorescence microscope (Nikon TS100-F, Japan) coupled with a cooled CCD camera was applied for image record, results of which were analyzed by ImageJ software.
2.2 Microfluidic device design
Figure 1a shows a schematic diagram of the microfluidic chip’s multilayered structure. The structure of the spheroid chip comprises two layers of PDMS plates and one layer of cell culture glass substrate. The cell culture unit is composed of an array of microwells on the bottom of the glass plate and bigger microwells and elastomeric microchannels on the upper of the PDMS plate. The lower layer is a combination of cell culture microwells and microchannels on a glass substrate. The substrate includes 4 × 5 panels of concave microwells (diameters of 800 μm and depths of 150 mm) and the microchannels (500 μm wide and 50 μm deep). The microwells were much deeper than the microchannels in the glass so that we can prevent aggregates washing out. The middle layer, a 2 mm thick PDMS plate, is composed of microchannels (500 μm wide and 50 μm deep), a 4 × 5 well array (diameters of 1,000 μm and depths of 150 mm) and four outlets. Liquid channels are patterned on the layer of the PDMS plate. The PDMS channel is designed with a dead end to facilitate cell capture, whereas the lower glass channel is continuous to allow medium perfusion. The upper PDMS layer has one inlet (0.8 mm in diameter), which is punched through the middle layer. The inlet and outlets are connected to a syringe pump through guiding tubes, which is responsible for cell injection and culture medium perfusion.
Structure and fabrication of the microfluidic device used for tumor spheroid formation and culture. a Schematic illustrations of the 3D layered structure of the PDMS/glass microfluidic chip. The chip consists of two layers of PDMS plate and one layer of cell culture glass plate. b A process-flow diagram of the fabrication procedure of two-step wet etching. Description of the steps is in the test. c Photograph of the fabricated microfluidic chip
2.3 Microfluidic device fabrication
The microfluidic device used for tumor spheroid culture was fabricated from PDMS and glass. Prior to bonding PDMS and glass, cell culture microwells and microchannels were patterned onto a glass plate by standard photolithographic technique and wet chemical etching methods. Briefly, the designed chip pattern was printed on a negative film mask. Then, the chip pattern was transferred onto a SG-2506 borosilicate glass, with photoresist coating by UV light exposure for 60 s. The desired chip image was developed after treatment with developer (0.5 % NaOH) for 30 s. After washing with ultrapure water, the glass plate was dried and heated at 120 °C for 45 min. After that, the untreated photoresist was solidated and the glass plate was soaked in chromium etchant for another 1 min to wash away the exposed chrome. Then, the exposed micropatterns on the surface of glass slide were etched in buffer oxide etchant (HF/NH4F = 1.0 M:1.0 M) at 30 °C. Moreover, we used a two-step wet chemical etching and controlled the etching time to make the different depth of microwells and microchannels (Sun and Yin 2006). Firstly, the microwells and microchannels in the glass plate were etched with HF + NH4F for 50 min. Secondly, several adhesive tapes were taped across microchannels areas, and the microwells of exposed areas were etched for another 100 min. It was finished by flushing the structure with distilled water, acetone and dried in airflow. As a result, the dimension of the cell culture microwells was 150 μm in depth while the microchannels were 50 μm in depth. Thus, the cell culture wells and microchannels were fabricated to provide suitable culturing microenvironments in glass, as shown in Fig. 1b.
The middle and top layers were fabricated using PDMS due to its hydrophobicity and gas permeability. The master mold of the upper layer was a blank glass plate. The middle PDMS microfluidic chips were fabricated by copper molds using computer numeric control (CNC) milling technique, which was developed by our group (Yang et al. 2013). Firstly, the designed microstructure was precisely carved by a CNC milling machine. The copper master mold was fabricated and rinsed with pure water, dried and stored for PDMS molding. Then, PDMS base and curing agent were mixed in the weight ratio of 10:1 and degassed thoroughly by a vacuum pump for about 0.5 h. The mixed PDMS was poured onto the copper mold and cured in an oven for 1 h at 80 °C. The PDMS replica was peeled off carefully from the mold and cut into the designed shape. The inlet and outlets were punched with a flat-tip syringe needle for guiding tubes. Finally, the top PDMS layers and the bottom glass substrate were irreversibly bonded by oxygen plasma treatment for 90 s.
2.4 Cell culture
MCF-7 cells were used as the model cells to demonstrate the functionality of the microfluidic device. The cells were routinely cultured in traditional cell culture dishes in a humidified atmosphere at 37 °C with 5 % CO2, using Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10 % FBS, 100 μg/mL penicillin and 100 μg/mL streptomycin. When the cells had become confluent, they were washed with PBS and passaged. The cell passage was achieved with standard 0.25 % trypsin and neutralized with medium. Then, the cell suspension solution was centrifuged at 1,300 rpm for 4 min, and the cells were resuspended in cell culture medium. Finally, we could inject the appropriate cell suspension into the cell culture microfluidic device for the following experiments. Meanwhile, monolayer cell culture in cell culture glass dishes and PDMS-covered glass dishes was carried out.
2.5 3D Spheroids formation
Tumor spheroid formation in the microfluidic device was demonstrated by the MCF-7 breast cancer cells. Prior to experiment, the microfluidic device was washed with deionized water, 70 % ethanol and PBS, and then we sterilized the microfluidic device using UV treatment for 30 min. To prevent cell adhesion, 0.5 % weight solution of PVA in deionized water was introduced to the device and left for 1-h incubation. After being washed, the cell suspension was introduced into the device using syringe pump. It was very important to remove all the air or bubbles in the channels before cell injection. Then, the system was sealed and placed in a culture chip for incubation for 48 h at 37 °C in a 5 % CO2 humidified air atmosphere before injection of fresh medium. To form a single cell microsphere in each cell culture well, the microfluidic chip was sloped at approximately 10° using a PDMS plate within 48 h of culture (sloping culture). Thereafter, the chip was cultured under a flat condition for normal culture. Culture medium was exchanged every 48 h at a flow rate of 1 μL/min for 60 min. Meanwhile, we kept the temperature which was controlled by a home-made incubator during the exchange process. For control experiments, tumor spheroids were formed on various substrates, including flat PDMS-covered glass dishes, traditional glass dishes and concave microwells in the microfluidic chip (normal 2D and 3D culture). All substrates were coated with 0.5 % weight solution of PVA to prevent cell attachment.
2.6 Computational modeling
Fluid flow in the designed structure was simulated using MEMS Module of COMSOL Multiphysics software version 4.3a.
2.7 Cell analysis
In the case of MCF-7 cells, the size of the spheroid was calculated by measuring its diameter. Two orthogonal diameters, a and b, were measured and used to calculate the geometric mean diameter using ImageJ software. The mean radius (r) of the spheroid was determined according to the following equation:
Cell viability was assessed using a combination of AO and EB. AO is a vital dye that stains both live and dead cells, while EB stains only cells that have lost membrane integrity. Live cells will appear uniformly green, whereas late apoptotic cells will stain orange with dots in the nuclei as a consequence of chromatin condensation, and necrotic cells will also stain orange, but these have a nuclear morphology resembling that of viable cells, with no condensed chromatin. Therefore, living cell rate can be calculated by the morphological assessment. A mixture solution of 100 μg/mL EB and 100 μg/mL AO in 100 mM PBS buffer was applied to the cell for 3 min before washed away by the PBS buffer. For AO/EB-labeled cells, cell viabilities were judged by the color of intracellular fluorescence. The resulting fluorescence were imaged by the fluorescence microscope analyzing system and analyzed by IMAGEJ program.
3 Results and discussion
3.1 Microfluidic design
We have fabricated a novel microfluidic chip comprised of two layers of PDMS plate using copper molds and one layer of cell culture glass plate using wet etching technology to generate 3D spheroid (Fig. 1a). The two layers of PDMS are composed of an inlet on the top layer, four outlets and an array of big wells and channels on the bottom of the second layer. The array of small wells on glass plate is manually aligned with the 4 × 5 PDMS well array for bounding. The upper channels of the middle layer are designed with a dead end for facilitating cell capture, and the channels of bottom layer are allowed medium perfusion. The wide microchannels (500 μm wide and 50 μm deep) could decrease the shear stress of the fluid flow for cells, and the height of microchannels can prevent the spheroids washing out from the wells. After most of the cells have aggregated to form a spheroid, the redundant cells were easily washed off by flushing the fresh culture medium into the microchannels. Each cell culture well (diameters of 800 μm and depths of 150 mm) on glass plate is deeper than the microchannel and protects the cells from direct expose to the medium exchange.
Wet etching has long been applied for the fabrication of microfluidic glass chip (Huang et al. 2013; Chen et al. 2010b). However, in recent years, it always deemed as a second choice because of isotropic etching character. This isotropy character could lead to opposite effects on concaved and convex structures for glass chip fabrication (Xu et al. 2012, 2013). Thus, we try to turn this disadvantage to an advantage by fabricating concave wells in the microfluidic chip to form the tumor spheroid instead of using PDMS cylindrical wells. Some studies have demonstrated that concave microwells are more effectively generate homogeneous tumor spheroid than planar PDMS surfaces or cylindrical microwells (Wong et al. 2011). Moreover, using two-step wet etching, we could get multidepth microfluidic channels and wells on glass plate. Figure 1b shows the two-step wet etching fabrication process. This may trigger our further exploration to the fabrication and application of glass chip.
In addition, the microfluidic would promote the formation of tumor spheroid because the height of inlet is much higher than the outlets. Although static cell culture is often used in the spheroid formation, they cannot facilitate the cells to form a single spheroid. Therefore, we developed an intermittent dynamic culture mode for this study. We applied hydrostatic pressure to establish a minute volume difference between the inlet and outlets, which resulted in a slow flow through the cell culture wells. These ways provide a dynamic environment in the microwells, allowing to form tumor spheroids rapidly.
3.2 Cell seeding and simulations
The uniformity of the cell seeding is considered to be one of the most important steps or markers of the experiment. Uniformity of spheroid sizes is attributed to the uniformity of cell seeding density. For anticancer drug assays, homogenous tumor spheroids are necessary for statistical analysis. Computational simulations (Fig. 2a) have shown uniform fluid flow in the microchannels. The experimental results indicated that cell seeding uniformity was good and standard deviation between the rows was lower than 10 % (data not shown). Cells introduced to the system were distributed uniformly in all of the four microchannels. It was observed that the cell culture reservoir was placed under the same row parallel to the channel. Figure 2b–d shows different simulation results of the fluid flow using COMSOL Multiphysics of fluid motion in the designed cell culture device. If the wells on the PDMS plate are the same size as the wells on the glass plate, it is difficult for the device to align correctly and satisfy uniformity. If a microfluidic device have been fabricated and aligned badly, we cannot see good uniformity of cell seeding. Microsystem alignment and bonding were crucial steps of fabrication, which must have a significant effect on the cell seeding uniformity. However, for our device, it is easy to fabricate and align correctly and rapidly. It is observable that the cell culture well should be in the center of the channel, which is important for the cell spatial uniformity. During our work, most of the microfluidic chips are fully usable in the experiment.
Simulation results of the fluid flow using COMSOL Multiphysics of fluid motion in the designed microfluidic device. a The simulation of fluid flow for two cell culture units in the chip. b The designed cell culture unit. The channel is 500 μm wide and 50 μm deep. Cell culture concave microwell is 800 μm wide and 150 μm deep on glass plate, and the PDMS microwell is 1,000 μm wide and 150 μm high on PDMS plate. c The cell culture glass microwell without PDMS microwell. d The theoretical cell culture PDMS unit. The cell culture microwell is cylindrical and the cylindrical microwell is 800 μm wide and 150 μm deep
3.3 Glass modification
Cell detachment on the glass plate is an important factor for the formation of tumor spheroid, so the modification of the glass surface with different substances has been investigated. The attachment of cells to various substrates is often dictated and controlled by the ability of adhesion proteins to adsorb onto the polymer surface, and cells cannot adhere to a surface unless cell adhesion proteins are present. In general, the driving force for protein adsorption to hydrophilic surfaces is enthalpic, whereas the driving force for adsorption to hydrophobic surfaces is entropic (Nuttelman et al. 2001). In particular, PVA is one of the very few vinyl polymers soluble in water that has been studied intensively because of its attractive features for medical applications such as good film-forming ability, processability and high hydrophily. PVA does not support cell attachment due to its highly hydrophilic nature. Although cell adhesion proteins bind stronger to surfaces with greater hydrophobicity, there is an associated loss of activity. Bovine serum albumin (BSA) or PEG was commonly used to modify the PDMS surface to form the spheroid, but the modification time and effect were not elaborated in detail. These materials reproduce to some extent the structural properties of the ECM, and they do not provide specific peptide recognition sequences required to promote cell attachment via surface receptors such as the integrin (Zajaczkowski et al. 2003). In this work, the glass was coated with 0.5 % (w/v) PVA and 3 % (w/v) BSA separately, and the PBS was used as a control. After the surface modification for 1, 12 and 24 h, respectively, MCF-7 cells were introduced to the glass dish, and then, the culture dish was incubated in a CO2 incubator for 24 h to allow the cells to form tumor spheroid. In Fig. 4a, we found that MCF-7 cells could form tumor spheroid on PVA-coated glass after 1 h or BSA-coated glass after 24 h. After BSA treated for 12 h, it was not clear to form spheroids and some cells adhered to the surface. They all could keep their health morphology and have a high cell viability. Hence, PVA, a non-degradable flexible biocompatible polymer, was finally selected as the material for tumor spheroid on chip.
3.4 Spheroid formation
Culture of tumor spheroid on a non-adhesive surface was used as a macroscale reference to the tumor spheroid microsystem (Fig. 3). Glass is a hydrophilic material and should be modified to render it with more hydrophilic property. PDMS is a hydrophobic material so that it may prevent cell attachment to form spheroids. Figure 4b showed the optical and fluorescence images of the spheroid culture on the plane dish for 5 days. MCF-7 cells were cultured on PDMS-covered dishes and PVA-coated glass dishes to compare their results. We also performed the MCF-7 cells cultured in classic way using cell culture glass dish. There was no impossible for changing cell culture medium in culture dish because the cells gravitated and aggregated to form several spheroids which were suspended in the whole medium. However, we found that hydrophobic PDMS surface could prevent cell attachment but some cells still adhered to the PDMS surface. MCF-7 cells on PDMS-covered dishes cannot form aggregates or spheroids, and we should enhance the effect using the PVA to modify the surface. Meanwhile, MCF-7 cells cultured on PVA-coated glass dishes could form aggregates within 24-h culture. It was observed that several spheroids were inhomogenously formed on the plane non-adhesive glass dish which provides bad uninform size uniformity. After 48 h cultivation, tumor spheroids on non-adhesive glass dish have high cell viability. On the sixth day, gradual decrease in cell viability can be observed.
MCF-7 cells cultured on flat glass dish. a The effect of different surface modification of glass on MCF-7 cell culture. Scale bar is 200 μm. b Time-lapse images of MCF-7 cells cultured on the plane glass surface, PDMS surface and PVA-coated glass surface. Cell viability was also performed. Green and red fluorescence indicates viable cells and dead cells, respectively. The same frames could not have been captured due to fluidity of the batch culture. Scale bar is 200 μm (color figure online)
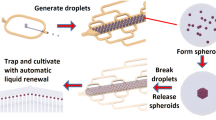
Figure 5a, b illustrates the concept of how tumor spheroid forms in the novel chip. Briefly, the microwells and microchannels of the microfluidic device were treated by PVA to be resistant to cell adhesion. Then, MCF-7 cells are introduced to the whole volume of the microsystem and gravity enforced cells to the sides of cell culture wells. Since the wells are resistant to cell adhesion, the cells self-aggregate to form tumor spheroids. After 48 h cultivation, we remove unaggregrated cells in the microwells and several small tumor spheroids in the microchannels. The spheroid size is already larger than the height of the microchannel. At last, the tumor spheroid becomes substantially spherical due to continued cell proliferation.
Formation of multicellular tumor spheroids in the microwells. a Scheme for the spheroids formation using normal culture and sloping culture methods. b Schematic diagram of the process for the spheroids formation in the microsystem. c The image of MCF-7 aggregation within first 24 h by normal culture method(a) and sloping method(c). Scale bar is 200 μm
The size of spheroid formed on the chip was attributed to the concentration of the injected cell suspension. If the number of cells introduced into the device was too low, it was difficult to form a single spheroid. It can cause several small spheroids in each well. On the other hand, if too high number of cells was introduced to the device, it is unhealthy for cells to form spheroids because of the toxic metabolism in the microwells. Too high density also had a bad effect on the uniformity of cell seeding density. During our practice, 1–8 × 107 cells/mL was optimal and it provided good results. In order to wash out unaggregrated cells, cell culture medium was introduced into the microfluidic device at the rate of 1 μL/min by syringe pumps. The choice of flow rate was limited by the damage of cells caused by the shear stress. According to the formula (Kim et al. 2007), shear stress <0.001 dyn/cm2 is known as harmless for cells on the surface of the culture chamber. In the present work, the flow rate was obviously below the shear stress to disturb cell function.
3.5 Culture of spheroids and viability assay
The first 24 h culture is critical for the success of the spheroid formation. We compare the formation of spheroids in the microfluidic device with normal and sloping method. The experiments were repeated thrice for each method. In Fig. 5c, it was found that the formation of the spheroid was slower in the microsystem than in the PVA-covered glass dish. After 24 h of incubation, a cancer aggregate of the MCF-7 cells was formed in the microwells, whereas the same number of cells aggregated more than ten clusters by normal culture method. In Fig. 6a, on day 2, the cells still formed several fragments in irregular clumps. Subsequently, we found that more than two spheroids were formed in the microwell on the chips under normal stationary tumor spheroid culture. The spheroids possessed smooth surfaces and high circularity, and the spheroid configuration was maintained despite further cell proliferation. Some cells were found to be adhered to the bottom surface of the microwells. Previous studies (Sakai and Nakazawa 2007) had demonstrated that the formation of a single spheroid in each microwell was difficult for the conditions in which the microwell diameter exceeded 500 μm. The cells in small-diameter microwells can easily aggregate and form single spheroids, whereas those in large-diameter microwells aggregate and form several small spheroids. The microwell diameter of 800 μm is too large for a single spheroid formation, and the culture medium is static, which cannot promote a single spheroid synthesis. To solve this problem, we used the sloping culture technology to form a single spheroid in each microwell of the chips with a microwell diameter of more than 800 μm. Meanwhile, the device could facilitate the spheroids because of the intermittent dynamic culture. In case of MCF-7 cells, as the sloping culture technology and fluxion of the culture medium are combined, tumor spheroid formation must be promoted. The results showed that spheroids on chip under sloping dynamic culture were formed within 3 days of culture, but spheroid formation which took the shape of almost perfect under stationary culture occurred in 5 days of culture.
Results of MCF-7 cells cultured in the microfluidic device for 2D and 3D. a Optical images of a microwell for 2D standard monoculture at day 0(a), day 1(b), day 3(c), tumor spheroid culture at day 0(d), day 2(e), day 3(f) by 3D normal culture method and tumor spheroid culture at day 0(g), day 1(h), day 3(i) by 3D sloping culture method. Scale bar is 200 μm. b Size of tumor spheroids cultured in the microfluidic system by 3D sloping culture. Results compared with a control of 2D standard culture of MCF-7 cells. c The formation ratio of tumor spheroids by the 3D normal and sloping culture methods. d The percentage of spheroids diameter in the total population. The average diameter was 150 μm. The images were used to measure the diameters of spheroids after generating the spheroids
The image of the tumor spheroid growth was observed by optical microscope. Diameters of spheroids were measured using image analysis software. The growth of tumor spheroids is presented in Fig. 6a. We observed that cell aggregation was noticeable after a 1 day culture with the formation of primitive. After 3 days of culture, the average size of spheroids was about 150 μm and 90 % of the spheroids had the diameters of 140–160 μm. Between days 3 and 5, spheroids were 150 μm in diameter and then remained constant (Fig. 6b). After 5 days of culture, cell viability assay was performed using the live/dead cell viability assay. The cell viability was over 90 %. To compare different results, monolayer 2D culture, glass dish spheroid culture and normal stationary spheroid culture were performed. The formation ratio of tumor spheroids by the 3D normal and sloping culture methods is shown in Fig. 6c. The proportions of microwells containing spheroids were about 15 % (1 day), 40 % (2 days) and 80 % (3 days) by 3D normal culture, while the proportion in device was about 80 % (1 day), 90 % (2 days) and 96 % (3 days) by 3D sloping culture, which was much higher than the 3D normal culture method. Formation and culture of multicellular tumor spheroid in the designed microsystem have some advantages over previous studies. It can easily form a single tumor spheroid by sloping culture method. The handing of the spheroids produced is straightforward because the spheroids are trapped in the microwells. Our data showed that applicability of glass substratum for spheroids formation is well suited.
4 Conclusions
We studied a novel microfluidic system that enabled the easy and rapid formation and culture tumor spheroid and the influence of glass substrate on the formation of tumor spheroids. The three-dimensional microfluidic platform comprised of two layers of PDMS plate using copper molds and one layer of cell culture glass plate using wet etching technology. The results show that spheroids could be formed naturally and uniformly with the microstructure and cultured for 3 days to the diameter of 150 μm due to strong cell–cell interactions and the exchange of cell culture medium via the microchannels. The high cell viability was maintained within this time. Our results also demonstrated that the suitability of glass microwell chip for tumor spheroid culture is well suited. It is expected to be widely used for live cell applications and promising applications in the future. The established platform provides a convenient and fast method for tumor spheroid culture, which is adaptable for analysis of cell-to-cell interactions and fundamental biomedical research. Moreover, the system can be easily coupled with a concentration gradient generator (Yang et al. 2011, 2013; Jedrych et al. 2011) to form a prospective system for anticancer drug screening on tumor cells.
References
Agastin S, Giang UBT, Geng Y, DeLouise LA, King MR (2011) Continuously perfused microbubble array for 3D tumor spheroid model. Biomicrofluidics 5(2). doi:10.1063/1.3596530
Birgersdotter A, Sandberg R, Ernberg I (2005) Gene expression perturbation in vitro—a growing case for three-dimensional (3D) culture systems. Semin Cancer Biol 15(5):405–412. doi:10.1016/j.semcancer.2005.06.009
Chen MCW, Gupta M, Cheung KC (2010a) Alginate-based microfluidic system for tumor spheroid formation and anticancer agent screening. Biomed Microdevices 12(4):647–654. doi:10.1007/s10544-010-9417-2
Chen Y, Choi JY, Choi SJ, Seo TS (2010b) Sample stacking capillary electrophoretic microdevice for highly sensitive mini Y short tandem repeat genotyping. Electrophoresis 31(17):2974–2980. doi:10.1002/elps.201000270
El-Ali J, Sorger PK, Jensen KF (2006) Cells on chips. Nature 442(7101):403–411. doi:10.1038/nature05063
Gao D, Liu JJ, Wei HB, Li HF, Guo GS, Lin JM (2010) A microfluidic approach for anticancer drug analysis based on hydrogel encapsulated tumor cells. Anal Chim Acta 665(1):7–14. doi:10.1016/j.aca.2010.03.015
Gao D, Liu HX, Jiang YY, Lin JM (2012) Recent developments in microfluidic devices for in vitro cell culture for cell-biology research. Trac-Trends Anal Chem 35:150–164. doi:10.1016/j.trac.2012.02.008
Hirschhaeuser F, Menne H, Dittfeld C, West J, Mueller-Klieser W, Kunz-Schughart LA (2010) Multicellular tumor spheroids: An underestimated tool is catching up again. J Biotechnol 148(1):3–15. doi:10.1016/j.jbiotec.2010.01.012
Hsiao AY, Torisawa YS, Tung YC, Sud S, Taichman RS, Pienta KJ, Takayama S (2009) Microfluidic system for formation of PC-3 prostate cancer co-culture spheroids. Biomaterials 30(16):3020–3027. doi:10.1016/j.biomaterials.2009.02.047
Huang P-H, Xie Y, Ahmed D, Rufo J, Nama N, Chen Y, Chan CY, Huang TJ (2013) An acoustofluidic micromixer based on oscillating sidewall sharp-edges. Lab Chip 13(19):3847–3852. doi:10.1039/C3LC50568E
Jedrych E, Pawlicka Z, Chudy M, Dybko A, Brzozka Z (2011) Evaluation of photodynamic therapy (PDT) procedures using microfluidic system. Anal Chim Acta 683(2):149–155. doi:10.1016/j.aca.2010.10.005
Jin H-J, Cho Y-H, Gu J-M, Kim J, Oh Y-S (2011) A multicellular spheroid formation and extraction chip using removable cell trapping barriers. Lab Chip 11(1):115–119. doi:10.1039/c0lc00134a
Kalchman J, Fujioka S, Chung S, Kikkawa Y, Mitaka T, Kamm RD, Tanishita K, Sudo R (2013) A three-dimensional microfluidic tumor cell migration assay to screen the effect of anti-migratory drugs and interstitial flow. Microfluid Nanofluid 14(6):969–981. doi:10.1007/s10404-012-1104-6
Karp JM, Yeh J, Eng G, Fukuda J, Blumling J, Suh K-Y, Cheng J, Mahdavi A, Borenstein J, Langer R, Khademhosseini A (2007) Controlling size, shape and homogeneity of embryoid bodies using poly(ethylene glycol) microwells. Lab Chip 7(6):786–794. doi:10.1039/b705085m
Kelm JM, Timmins NE, Brown CJ, Fussenegger M, Nielsen LK (2003) Method for generation of homogeneous multicellular tumor spheroids applicable to a wide variety of cell types. Biotechnol Bioeng 83(2):173–180. doi:10.1002/bit.10655
Kim JB (2005) Three-dimensional tissue culture models in cancer biology. Semin Cancer Biol 15(5):365–377. doi:10.1016/j.semcancer.2005.05.002
Kim L, Toh Y-C, Voldman J, Yu H (2007) A practical guide to microfluidic perfusion culture of adherent mammalian cells. Lab Chip 7(6):681–694. doi:10.1039/b704602b
Kim C, Bang JH, Kim YE, Lee SH, Kang JY (2012a) On-chip anticancer drug test of regular tumor spheroids formed in microwells by a distributive microchannel network. Lab Chip 12(20):4135–4142. doi:10.1039/c21c40570a
Kim T, Doh I, Cho YH (2012b) On-chip three-dimensional tumor spheroid formation and pump-less perfusion culture using gravity-driven cell aggregation and balanced droplet dispensing. Biomicrofluidics 6(3). doi:10.1063/1.4739460
Liu WM, Sun P, Yang LY, Wang JF, Li L, Wang JY (2010) Assay of glioma cell responses to an anticancer drug in a cell-based microfluidic device. Microfluid Nanofluid 9(4–5):717–725. doi:10.1007/s10404-010-0584-5
Mori R, Sakai Y, Nakazawa K (2008) Micropatterned organoid culture of rat hepatocytes and HepG2 cells. J Biosci Bioeng 106(3):237–242. doi:10.1263/jbb.106.237
Nuttelman CR, Mortisen DJ, Henry SM, Anseth KS (2001) Attachment of fibronectin to poly(vinyl alcohol) hydrogels promotes NIH3T3 cell adhesion, proliferation, and migration. J Biomed Mater Res 57(2):217–223. doi:10.1002/1097-4636(200111)57:2<217:aid-jbm1161>3.0.co;2-i
Ozawa F, Ino K, Arai T, Ramon-Azcon J, Takahashi Y, Shiku H, Matsue T (2013) Alginate gel microwell arrays using electrodeposition for three-dimensional cell culture. Lab Chip. doi:10.1039/C3LC50455G
Sahai R, Cecchini M, Klingauf M, Ferrari A, Martino C, Castrataro P, Lionetti V, Menciassi A, Beltram F (2011) Microfluidic chip for spatially and temporally controlled biochemical gradient generation in standard cell-culture Petri dishes. Microfluid Nanofluid 11(6):763–771. doi:10.1007/s10404-011-0841-2
Sakai Y, Nakazawa K (2007) Technique for the control of spheroid diameter using microfabricated chips. Acta Biomater 3(6):1033–1040. doi:10.1016/j.actbio.2007.06.004
Sakai Y, Yoshida S, Yoshiura Y, Mori R, Tamura T, Yahiro K, Mori H, Kanemura Y, Yamasaki M, Nakazawa K (2010) Effect of microwell chip structure on cell microsphere production of various animal cells. J Biosci Bioeng 110(2):223–229. doi:10.1016/j.jbiosc.2010.01.021
Shi Y, Gao XH, Chen LQ, Zhang M, Ma JY, Zhang XX, Qin JH (2013) High throughput generation and trapping of individual agarose microgel using microfluidic approach. Microfluid Nanofluid 15(4):467–474. doi:10.1007/s10404-013-1160-6
Sun Y, Yin XF (2006) Novel multi-depth microfluidic chip for single cell analysis. J Chromatogr A 1117(2):228–233. doi:10.1016/j.chroma.2006.03.088
Torisawa Y-s, Takagi A, Nashimoto Y, Yasukawa T, Shiku H, Matsue T (2007) A multicellular spheroid array to and viability realize spheroid formation, culture, assay on a chip. Biomaterials 28(3):559–566. doi:10.1016/j.biomaterials.2006.08.054
Wlodkowic D, Faley S, Skommer J, McGuinness D, Cooper JM (2009) Biological implications of polymeric microdevices for live cell assays. Anal Chem 81(23):9828–9833. doi:10.1021/ac902010s
Wong SF, No DY, Choi YY, Kim DS, Chung BG, Lee SH (2011) Concave microwell based size-controllable hepatosphere as a three-dimensional liver tissue model. Biomaterials 32(32):8087–8096. doi:10.1016/j.biomaterials.2011.07.028
Wu LY, Di Carlo D, Lee LP (2008) Microfluidic self-assembly of tumor spheroids for anticancer drug discovery. Biomed Microdevices 10(2):197–202. doi:10.1007/s10544-007-9125-8
Xu BY, Yan XN, Zhang JD, Xu JJ, Chen HY (2012) Glass etching to bridge micro- and nanofluidics. Lab Chip 12(2):381–386. doi:10.1039/c1lc20741e
Xu BY, Hu SW, Qian GS, Xu JJ, Chen HY (2013) A novel microfluidic platform with stable concentration gradient for on chip cell culture and screening assays. Lab Chip 13(18):3714–3720. doi:10.1039/c3lc50676b
Yamada KM, Cukierman E (2007) Modeling tissue morphogenesis and cancer in 3D. Cell 130(4):601–610. doi:10.1016/j.cell.2007.08.006
Yang F, Chen ZG, Pan JB, Li XC, Feng J, Yang H (2011) An integrated microfluidic array system for evaluating toxicity and teratogenicity of drugs on embryonic zebrafish developmental dynamics. Biomicrofluidics 5(2). doi:10.1063/1.3605509
Yang J, Chen Z, Ching P, Shi Q, Li X (2013) An integrated microfluidic platform for evaluating in vivo antimicrobial activity of natural compounds using a whole-animal infection model. Lab Chip. doi:10.1039/C3LC50264C
Yoon S, Kim JA, Lee SH, Kim M, Park TH (2013) Droplet-based microfluidic system to form and separate multicellular spheroids using magnetic nanoparticles. Lab Chip 13(8):1522–1528. doi:10.1039/c3lc41322e
Yu LF, Chen MCW, Cheung KC (2010) Droplet-based microfluidic system for multicellular tumor spheroid formation and anticancer drug testing. Lab Chip 10(18):2424–2432. doi:10.1039/c004590j
Zajaczkowski MB, Cukierman E, Galbraith CG, Yamada KM (2003) Cell-matrix adhesions on poly(vinyl alcohol) hydrogels. Tissue Eng 9(3):525–533. doi:10.1089/107632703322066705
Ziolkowska K, Kwapiszewski R, Stelmachowska A, Chudy M, Dybko A, Brzozka Z (2012) Development of a three-dimensional microfluidic system for long-term tumor spheroid culture. Sens Actuators B-Chem 173:908–913. doi:10.1016/j.snb.2012.07.045
Ziolkowska K, Stelmachowska A, Kwapiszewski R, Chudy M, Dybko A, Brzozka Z (2013) Long-term three-dimensional cell culture and anticancer drug activity evaluation in a microfluidic chip. Biosens Bioelectron 40(1):68–74. doi:10.1016/j.bios.2012.06.017
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant Nos. 21375152 and 21075139). The authors thank Dr. Karina Ziolkowska (Warsaw University of Technology, Department of Microbioanalytics, Warsaw, Poland), Dr. Dan Gao (The Key Laboratory of Chemical Biology, Tsinghua University, Shenzhen, China) for valuable discussion and Prof. Peiqing Liu (New Drug Screening Center, Sun Yat-sen University) for the help of cell culture.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, D., Lu, J., Chen, Z. et al. A novel three-dimensional microfluidic platform for on chip multicellular tumor spheroid formation and culture. Microfluid Nanofluid 17, 831–842 (2014). https://doi.org/10.1007/s10404-014-1373-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10404-014-1373-3