Abstract
Hydrostatic pressure can affect the structure and function of endothelial cells (ECs). A microfluidic system was built to study how ECs respond to applied pressure. The system included a syringe pump, a PDMS-glass microfluidic chip, and a digital manometer for pressure monitoring. The manometer was connected with the chip in two ways (one was before the inlet and the other after the outlet of the microchannel). The static control and flowing control systems were also set up. Human umbilical vein endothelial cells (HUVECs) were cultured in the 4 cm × 2 mm × 100 μm channel. Pressure of 12 ± 0.5 or 18 ± 0.5 kPa was applied on the cells for 8 h. The F-actin cytoskeleton and the nuclei of the cells were stained for examination and endothelin-1 (ET-1) released from the cells in the channel was assayed by ELISA. The results showed that the cell area and ET-1 concentration increased with the pressure and a higher pressure caused more damages to the cells. This microfluidic system provides a convenient and cost-effective platform for the studies of cell response to pressure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Endothelial cells (ECs) are oblong-shaped cells which line the inner surface of all blood vessels as a single squamous epithelial cell layer. It has been found that ECs are concerned with a number of disease processes. For example, hypertension (i.e., high blood pressure) is associated with functional and morphological alterations of endothelium, which disturbs delicate balance of endothelium-derived factors resulting in endothelial dysfunction (Sainani and Maru 2004). Hemodynamic forces are the most physiologically relevant determinants for the continuous activation of ECs. These stimuli can alter EC morphology and initiate cytoskeletal changes and the release of various vasoactive substances. Hemodynamic forces can be resolved into two principal vectors—shear stress and pressure (Davies et al. 1997). Shear stress is exerted along the same direction as flow of solution. The effect of shear stress on ECs has been investigated extensively, which is usually studied in vitro by subjecting ECs to shear stress in parallel plate flow chambers (Eskin et al. 1984; Diamond et al. 1989; Levesque et al. 1990; Gallik et al. 1989), prefabricated glass microcapillary tubes (“microslides”) (Cooke et al. 1993) or rotary-disk shear-loading devices (Ono et al. 1991). Pressure is exerted radially at right angles to the axis of flow and imposes circumferential stretch on the vessel wall. The effect of pressure on ECs has been studied in vitro by culturing cells in a pressure-loading apparatus where pressure can be regulated (Hishikawa et al. 1995; Muller-Marschhausen et al. 2008; Tokunaga and Watanabe 1987; Schwartz et al. 1999).
Microfluidic devices offer a number of distinct advantages over traditional research platforms for cell culturing, manipulation, and analysis (El-Ali et al. 2006). In recent years, the microfluidic technology has been adapted for vascular and ECs research (van der Meer et al. 2009). The growing environment of ECs in microfluidic devices is closer to the in vivo conditions than well plates. ECs have been cultured in microchannels and subjected to physiological levels of shear stress in multiple parallel channels (Song et al. 2005). A microfluidic device that allows for real-time tracking of ECs that are subjected to shear stress has also been designed (Tkachenko et al. 2009). These microfluidic systems were used to study EC response to shear stress. A microfluidic EC culture model has been fabricated to culture ECs under in vivo-like pressure, flow, strain, and shear stress waveforms (Estrada et al. 2011). This system needed pump, valve, and sensors for generation of physiological pressure, stretch, and shear waveforms.
In this paper, we used an easy-to-fabricate-and-assemble microfluidic system to study EC response to pressure. A microfluidic-based cell research and pressure-loading system was developed. The system includes a syringe pump for medium perfusion and pressure generation, a microfluidic chip for cell culture, a digital manometer for pressure monitor, and some joints and tubes. Human umbilical vein endothelial cells (HUVECs) were cultured on the chip. Atmosphere pressure (control), 12 kPa (medium pressure) and 18 kPa (high pressure) were exerted on the cells in the channel, respectively. The manometer was connected into the system in two ways, one was before the inlet of the channel, and the other was after the outlet of the channel. The static control and flowing control systems were also set up. The F-actin cytoskeleton and the nucleus of the ECs were stained after 8 h perfusion. Cell sizes were measured by using fluorescent staining images and image processing software. To further evaluate the injury of the ECs in the channels in different experimental conditions, the releases of endothelin-1 (ET-1) (Yanagisawa et al. 1988) by the cells were assayed.
2 Materials and methods
2.1 Design and fabrication of the microfluidic chip
A straight channel with a length of 4 cm, width of 2 mm, and height of 100 μm was used in this paper. The microchannel structure was fabricated in PDMS (Sylgard 184, Dow Corning, USA) by rapid prototyping and replica molding techniques (Duffy et al. 1998). Briefly, the negative relief of PDMS was formed by curing the prepolymer (Sylgard 184, Dow Corning, USA) on a silanized Si master having a positive relief of the channels formed in photoresist (SU-8 2075, MicroChem, USA) on its surface. Inlets were drilled using a blunted and beveled syringe needle. Finally, an oxygen plasma treatment was performed by a plasma cleaner (PDC-32G, Harrick Scientific Products, Inc.) to bonding the PDMS replica to a clean glass slide, to form a complete microfluidic chip.
2.2 Experimental setup
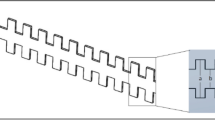
The system includes a syringe pump (KDS200, KD Scientific, USA) and a syringe, a microfluidic chip, a digital manometer (M382, As-one, Japan), and some joints and tubes (inner diameter × external diameter: 1 × 2 mm and 3 × 5 mm). The schematic diagrams of the two types of connection used in this study were shown in Fig. 1; one was called T-type connection system (Fig. 1a) and the other called I-type connection system (Fig. 1b). Cells could be cultured in the microchannel. The syringe mounted on the syringe pump was connected to the inlet of the chip. In the T-type connection system, the probe of the manometer was connected in the inlet tube before the input of the microchannel by using a T-joint (1.5 mm × 2 ↔ 3.0 mm, ISIS Co., Ltd.) and there was a clamp on the outlet tube to stop medium flowing through the channel. The medium in the syringe could be perfused to the tube of the manometer probe to generate pressure. In the I-type connection system, the probe of the manometer was directly connected to the outlet tube. The medium which flow to the probe should flow through the channel. The photos of the microfluidic chip-based pressure experimental systems were shown in Fig. 2.
2.3 Cell culture
Prior to cell seeding, all the chips, tubes, and joints were autoclaved for 20 min at 121 °C. Next, a 50 μg/mL human fibronectin (HFN, Millipore) solution was injected into the channels using a 1 mL syringe to promote cell adhesion. Leave the chips for 1 h at a 37 °C incubator and then remove the HFN solution using the syringe. Finally, the chips were dried in the clear hood at room temperature (RT).
HUVECs, endothelial cell medium, trypsin/EDTA solution, and trypsin neutralization solution were purchased from ScienCell (San Diego, CA, USA). The cells were cultured in T-25 culture flasks (Corning, USA) treated with a 10 μg/mL HFN solution. Cells were removed from the flasks with trypsin/EDTA solution when about 80 % confluent and then resuspended in endothelial cell medium. The number of cells was adjusted to about 5 × 106/mL. Thereafter, the cell suspension was carefully injected into the channels and the chips were incubated at 37 °C with 5 % CO2. After the cells adhered to the glass surface, the medium was replaced every 12 h. Cells were inspected and recorded by a microscope (Ti-s, Nikon, Japan) and a CCD camera (Ds-Ri1, Nikon, Japan). Cells were used between passages 3 and 6.
2.4 Pressure experiment procedure
Cells were ready for pressure experiments when they attained 70–80 % confluence. The medium were replaced before the pressure experiments. Then, 6 mL medium were loaded in a 10 mL syringe. The syringe, tubes, joints, chip, and the manometer were connected as shown in Figs. 1 and 2, and the outlet tube was clamped for the T-type system. The chip was placed in the incubator at 37 °C with 5 % CO2, and the pump and the manometer were left outside the incubator. The flow rate of the pump was set at 30–50 μL/min, and the manometer was monitored until the pressure was increased to 12 or 18 kPa. Then, the pump was adjusted to a smaller flow rate (5–10 μL/min) to stabilize the pressure at 12 ± 0.5 or 18 ± 0.5 kPa for 8 h. After 8 h, the pump was stopped and the medium in the channel and the tubes was collected (about 5 mL).
The static control and flowing control channels were also set up. In the case of the static control, the chip with HUVECs was placed in the incubator, with medium change and collection at the same time as other chips. In the case of the flowing control, the pump, tubes, and the chip were connected as shown in Fig. 1b and an empty reservoir was connected at the outlet of the channel instead of the manometer for medium collection. The flow rate of the pump was set at 10 μL/min, and medium was kept flowing for 8 h. Then, the medium in the tubes, channel, and the reservoir were collected (about 5 mL). The medium were centrifuged and the supernatants were dispensed into EP tubes and then stored at −20 °C for ET-1 assay. The cells in the channel could be used for actin filament and nuclear staining or kept on culturing for measuring the ET-1 release after pressure experiments.
2.5 Actin filament and nuclear staining
After exposure to pressure and flow for 8 h, HUVECs in the channels were stained for actin filaments and nuclei with Alexa Fluor 488 phalloidin (Invitrogen, Carlsbad, CA, USA) and 4′,6-diamidino-2-phenylindole (DAPI, Invitrogen), respectively. First, cells were gently washed twice with Dulbecco’s PBS and then fixed with 3.7 % paraformaldehyde solution (Sigma-Aldrich) in PBS for 10 min at RT and washed twice with PBS. Then, the cells were permeabilized with 0.1 % Triton X-100 (Sigma-Aldrich) in PBS solution. Actin filaments were stained with Alexa Fluor 488 phalloidin in PBS (1:40) including 1 % bovine serum albumin (Sigma-Aldrich). Subsequently, the chips were placed in dark for 20 min at RT and then washed twice with PBS. During the nuclear staining stage, the DAPI stock solution was diluted into PBS (1:300) to make a 0.2 μg/mL (600 nM) solution. Infuse the 600 nM solution into the channels and place the chips for 2 min. Wash two or more times with PBS. Fluorescence images were recorded by a microscope (Ti-s, Nikon, Japan) and a CCD camera (Ds-Ri1, Nikon, Japan).
2.6 Cell size measurement
Cell size was estimated by using fluorescent staining images (40× magnification) and image processing software. The cell boundaries were distinguished and mapped from the actin filaments staining image to obtain the total cell area in an image. The average cell size was evaluated by measuring the total cell area and divided it by the number of cell nucleus in the nuclear staining image of the same microscopic field. Measurements were made of five sets of randomly captured images in each experimental condition, and the areas were averaged. Results represent as the mean ± SD values in the text and figures. Student’s t test (p value < 0.05) was used to determine statistical significance.
2.7 Assay of ET-1
After collecting the medium during the pressure experiments, the chips were placed in the incubator at 37 °C with 5 % CO2. After 16 h, the medium in the channels were collected from the outlet tubes by adding fresh medium from the inlet tubes. Then, we centrifuged the medium and dispensed the supernatant into EP tubes, followed by storing them at −20 °C for ET-1 assay.
Cell culture supernatant was collected from several independent experiments, with more than three channels per each experimental condition. The quantitative determination of ET-1 concentrations in these samples was performed by using an ELISA-based commercial assay kit (Human Endothelin-1 Immunoassay kit QET00B, R&D systems). A microplate reader (Genios plus, Tecan) was used to measure the intensity of light emitted in relative light units (RLU). The standard curve was generated by using logistic fit of the data, with concentrations on the x-axis and RLU values on the y-axis. The concentration from RLU for each sample was determined using the standard curve. Curve fitting, concentration values, and graphs were prepared using software OriginPro 8 (OriginLab, Northampton, MA). All the experiments were carried out more than three times. The data are expressed as the mean ± SD values in the text and figures. Student’s t test (p value < 0.05) was used to determine statistical significance.
3 Results
3.1 HUVECs on the chip
The results of cell culture in channels were shown in Fig. 3. Cells were dispersed with pipettes until they were separated, and injected immediately into the channels to produce a well-proportioned distribution. Cells were ready for the pressure experiment when they attained 70–80 % confluence (Figs. 3a and b). Cells in the channel were recorded 0 h (Fig. 3c) and 16 h after the pressure experiment (Fig. 3d), respectively.
3.2 Image staining and cell size measurement
HUVECs cultured in the channel which was connected to T-type or I-type system were maintained in culture for 8 h under 12 ± 0.5 or 18 ± 0.5 kPa pressure and compared to the static and flowing control (10 μL/min, 8 h). Following the pressure experiment, the actin filament (F-actin) and nuclear of the HUVECs were stained and recorded using fluorescence microscopy. The F-actin and nuclear fluorescence images of each experimental condition obtained at 40 × objective magnification were overlaid and shown in Fig. 4. HUVECs cultured in the flowing control system (Fig. 4d) exhibited an aligned ellipsoidal phenotype in comparison with that in static control channel (Fig. 4a), in which cells were randomly oriented and polygonal in shape. The directions of the actin filament of the cells cultured in the T-type system under 12 kPa (Fig. 4b) were relative disorder than that of the cells cultured in the I-type system under 12 kPa (Fig. 4e). Cultured in the T-type and I-type system under 18 kPa for 8 h (Fig. 4c and f), most of the cytoskeletons collapsed and the actin filament bundles disappeared. Moreover, the distance between the cells under control and the pressure of 12 kPa is larger than that of 18 kPa.
The cell morphologies were also evaluated after pressure treatment. The average cell areas of each condition were shown in Fig. 5. It was found that the cell area increased with pressure increase (T-type 18 kPa > T-type 12 kPa > static control, I-type 18 kPa > T-type 12 kPa > flowing control). Significant difference was observed between control and 18 kPa, whereas no significant difference was observed between 12 kPa and 18 kPa or control and 12 kPa. Moreover, the cell areas under flow were found to be larger than that without flow under the same pressure (I-type 18 kPa > T-type 18 kPa, I-type 12 kPa > T-type 12 kPa, and flowing control > static control), and significant differences were observed between the two conditions of these three groups (p < 0.05).
3.3 ET-1 production from HUVECs
ET-1 is a potent vasoconstrictor. ET-1 may participate in vascular damage in cardiovascular diseases and in blood pressure elevation in experimental models and in human hypertension (Schiffrin 2001; Iglarz and Schiffrin 2003). Hypertensive subjects display significantly higher plasma levels of ET-1 than normotensives (Shichiri et al. 1990). After the application of pressure for 8 h in our experiment, the medium in the tubes, channel, and the reservoir were collected for ET-1 assay. The results were shown in Fig. 6. It was found that the ET-1 concentration was increased with the pressure increase (T-type 18 kPa > T-type 12 kPa > static control, I-type 18 kPa > T-type 12 kPa > flowing control). Significant difference was observed between control and 18 kPa, whereas no significant difference could be seen between 12 kPa and 18 kPa or control and 12 kPa (p < 0.05). Moreover, the ET-1 concentrations under flow were found to be much larger than those without flow under the same pressure (I-type 18 kPa ≫ T-type 18 kPa, I-type 12 kPa ≫ T-type 12 kPa, and flowing control ≫ static control).
After the pressure experiments, the cells were further cultured for 16 h and the ET-1 release during the 16 h was shown in Fig. 7. The ET-1 concentrations released from the cells in channels under flow for 8 h were higher than those of the cells without flow (I-type > T-type, flowing control > static control) with significant differences observed (p < 0.05). Moreover, the ET-1 concentration from the cells under 18 kPa was higher than 12 kPa and control. Significant difference was observed between flowing control and I-type 18 kPa, whereas no significant difference was observed between 12 kPa and 18 kPa or control and 12 kPa, or among T-type 18 kPa, 12 kPa, and static control.
4 Discussion
ECs are exposed to several mechanical forces in vivo, including fluid shear, substrate tension, and hydrostatic pressure. Exposure of ECs in vitro to these mechanical forces also affects cell morphology and function. Many experiments have been achieved in the past for studying cell behavior under flow, a popular way to applying shear stresses to adhering cells. Microfluidic perfusion systems have more defined flow characteristics that consume minute amount of reagents and are amenable to multiplexing. Therefore, EC biology, including polarization, migration, cytotoxicity, chemotaxis, and directional angiogenesis, were often investigated on perfusion systems (Shamloo et al. 2008; Barkefors et al. 2009). Unlike shear stress, relatively few microfluidic systems have focused on the direct effects of hydrostatic pressure on EC structure and function. However, evaluation of pressure on ECs in vitro shows that increased pressure results in EC proliferation, morphologic changes, and enhanced ET-1 release (Sumpio et al. 1994; Hishikawa et al. 1995). In this study, we report the design and validation of a simple microfluidic perfusion system capable of producing hydrostatic pressure on cells, and the pressure can be monitored by a manometer. This system is easy to set up and could provide various pieces of information with reduced consumption of cells and medium. The medium in the channel could be collected for the test of cell secretion; the cells in the channel could be stained for the investigation of morphology or removed from the channel and collected for other assays.
Under the same manometer pressure, the cell area and ET-1 concentration in I-type system were both larger than that in T-type system. To explain these phenomena, the shear stresses in both systems were estimated. The average shear stress of the monolayer cells in the microchannel (τ: N/cm2) was determined by the following formula: τ = 6μQ/wh2, where μ is fluid viscosity (10−7 N s/cm2, approximate value), Q is flow rate (mL/s), w is channel width (0.2 cm), and h is channel height (0.01 cm). In the T-type system, the manometer was connected before the inlet of the chip and the outlet tube was clamped. Therefore, medium were perfused to the tube of the manometer probe instead of flowing through the channel where cells were cultured. In comparison, the manometer was directly connected to the outlet tube in the I-type system, and the medium flowing to the manometer should also flow through the channel. Therefore, Q T-type = Q static control = 0, Q I-type = Q flowing control = 5 mL/8 h = 1.736 × 10−4 cm3/s, and thus, τ T-type = τ static control = 0, τ I-type = τ flowing control = 0.521 dyn/cm2. The cells in the I-type and the flowing control system sustained higher shear stress than in the T-type and the static control system.
The channel dimension used in this paper is 4 cm × 2 mm × 100 μm. The equivalent diameter d of the channel is about 190 μm (d = 4A/L = 4 × w×h/2(w + h), where A is cross-sectional area and L is perimeter). The common dimension of blood vessels is from a diameter of about 25 mm in the aorta to only 8 μm in the capillaries. More specifically, the diameter of human pial arteries is from 200 to 1,200 μm (Thorin-Trescases et al. 1997), muscular arteries-distributing arteries from 0.3 to 1.0 cm, arterioles from 10 μm to 0.3 cm, and venules from 8 to 100 μm (http://www.rci.rutgers.edu/~uzwiak/AnatPhys/Blood_Vessels.html). The channel used in this paper could mimic those vessels. Moreover, it is easy to fabricate microchannel of different dimensions to mimic different vessels. Narrow channels (<225 μm) could influence ECs’ morphology, on the contrary, cells in 225-μm-wide microchannels have the same shape index as control cells cultured on plain collagen-coated plastic slides (Gray et al. 2002). In the T-type system, Q and τ are zero. The channel dimension has minimal influence with the ECs function and pressure. In the I-type system, if w and/or h are changed, τ will changed. After the 8 h pressure experiment, the cellular morphology, cell area, and ET-1 concentration might be changed mainly due to the influences of different shear stresses.
Normal blood pressure at rest is within the range of 100–140 mmHg systolic (top reading) and 60–90 mmHg diastolic (bottom reading). High blood pressure is said to be present if it is persistently at or above 140/90 mmHg (18.6/12.0 kPa) (Cutler et al. 2008). The present study also provided evidence that high pressure (18 kPa) could cause more damages to cells than medium pressure (12 kPa) and atmosphere pressure (control), and these effects could last for a period of time after the pressure was removed, especially with the existence of solution flow. Cell area and ET-1 concentration increased with the pressure increase in both T-type and I-type connection system after the 8 h pressure-loading experiments. Then, the medium in the microchannels were changed. The ET-1 concentrations of the fresh medium of the 18 kPa channel were still higher than 12 kPa and control during the 16 h after the pressure-loading experiments (Fig. 7), especially with the effect of shear stress in the I-type system.
5 Conclusions
In summary, we have established a microfluidic-based cell research and pressure monitoring system. The system is easy to assemble, which includes a syringe pump, a microfluidic chip, and a digital manometer. HUVECs were cultured on the chip. The manometer was used to monitor the pressure and could be connected in two modes, i.e., before the inlet of the channel (T-type connection) or after the outlet of the channel (I-type connection). After 8 h perfusion, the staining results of F-actin cytoskeleton and the nucleus of the ECs and the releases of ET-1 by the cells in the channel showed obvious differences between T-type connection, I-type connection, flowing control, and static control systems. High pressure caused more serious injury to the cells than medium pressure and atmosphere pressure. This study used HUVECs and two typical pressure values—12 and 18 kPa; nevertheless, the method proposed here is flexible and can be used for other cells under different pressures. This work demonstrates that this microfluidic system provides a convenient and cost-effective platform for the study of cell response to pressure.
References
Barkefors I, Thorslund S, Nikolajeff F, Kreuger J (2009) A fluidic device to study directional angiogenesis in complex tissue and organ culture models. Lab Chip 9(4):529–535. doi:10.1039/b814691h
Cooke BM, Usami S, Perry I, Nash GB (1993) A simplified method for culture of endothelial cells and analysis of adhesion of blood cells under conditions of flow. Microvasc Res 45(1):33–45. doi:10.1006/mvre.1993.1004
Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ (2008) Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension 52(5):818–827. doi:10.1161/HYPERTENSIONAHA.108.113357
Davies PF, Barbee KA, Volin MV, Robotewskyj A, Chen J, Joseph L, Griem ML, Wernick MN, Jacobs E, Polacek DC, dePaola N, Barakat AI (1997) Spatial relationships in early signaling events of flow-mediated endothelial mechanotransduction. Annu Rev Physiol 59:527–549. doi:10.1146/annurev.physiol.59.1.527
Diamond SL, Eskin SG, McIntire LV (1989) Fluid flow stimulates tissue plasminogen activator secretion by cultured human endothelial cells. Science 243(4897):1483–1485
Duffy DC, McDonald JC, Schueller OJA, Whitesides GM (1998) Rapid prototyping of microfluidic systems in poly(dimethylsiloxane). Anal Chem 70(23):4974–4984
El-Ali J, Sorger PK, Jensen KF (2006) Cells on chips. Nature 442(7101):403–411. doi:10.1038/nature05063
Eskin SG, Ives CL, McIntire LV, Navarro LT (1984) Response of cultured endothelial cells to steady flow. Microvasc Res 28(1):87–94
Estrada R, Giridharan GA, Nguyen MD, Roussel TJ, Shakeri M, Parichehreh V, Prabhu SD, Sethu P (2011) Endothelial cell culture model for replication of physiological profiles of pressure, flow, stretch, and shear stress in vitro. Anal Chem 83(8):3170–3177. doi:10.1021/ac2002998
Gallik S, Usami S, Jan KM, Chien S (1989) Shear stress-induced detachment of human polymorphonuclear leukocytes from endothelial cell monolayers. Biorheology 26(4):823–834
Gray BL, Lieu DK, Collins SD, Smith RL, Barakat AI (2002) Microchannel platform for the study of endothelial cell shape and function. Biomed Microdevices 4(1):9–16
Hishikawa K, Nakaki T, Marumo T, Suzuki H, Kato R, Saruta T (1995) Pressure enhances endothelin-1 release from cultured human endothelial cells. Hypertension 25(3):449–452
Iglarz M, Schiffrin EL (2003) Role of endothelin-1 in hypertension. Curr Hypertens Rep 5(2):144–148
Levesque MJ, Nerem RM, Sprague EA (1990) Vascular endothelial cell proliferation in culture and the influence of flow. Biomaterials 11(9):702–707
Muller-Marschhausen K, Waschke J, Drenckhahn D (2008) Physiological hydrostatic pressure protects endothelial monolayer integrity. Am J Physiol Cell Physiol 294(1):C324–C332. doi:10.1152/ajpcell.00319.2007
Ono O, Ando J, Kamiya A, Kuboki Y, Yasuda H (1991) Flow effects on cultured vascular endothelial and smooth muscle cell functions. Cell Struct Funct 16(5):365–374
Sainani GS, Maru VG (2004) Role of endothelial cell dysfunction in essential hypertension. J Assoc Physicians India 52:966–969
Schiffrin EL (2001) Role of endothelin-1 in hypertension and vascular disease. Am J Hypertens 14(6 Pt 2):83S–89S
Schwartz EA, Bizios R, Medow MS, Gerritsen ME (1999) Exposure of human vascular endothelial cells to sustained hydrostatic pressure stimulates proliferation. Involvement of the alphaV integrins. Circ Res 84(3):315–322
Shamloo A, Ma N, Poo MM, Sohn LL, Heilshorn SC (2008) Endothelial cell polarization and chemotaxis in a microfluidic device. Lab Chip 8(8):1292–1299. doi:10.1039/b719788h
Shichiri M, Hirata Y, Ando K, Emori T, Ohta K, Kimoto S, Ogura M, Inoue A, Marumo F (1990) Plasma endothelin levels in hypertension and chronic renal failure. Hypertension 15(5):493–496
Song JW, Gu W, Futai N, Warner KA, Nor JE, Takayama S (2005) Computer-controlled microcirculatory support system for endothelial cell culture and shearing. Anal Chem 77(13):3993–3999. doi:10.1021/ac050131o
Sumpio BE, Widmann MD, Ricotta J, Awolesi MA, Watase M (1994) Increased ambient pressure stimulates proliferation and morphologic changes in cultured endothelial cells. J Cell Physiol 158(1):133–139. doi:10.1002/jcp.1041580117
Thorin-Trescases N, Bartolotta T, Hyman N, Penar PL, Walters CL, Bevan RD, Bevan JA (1997) Diameter dependence of myogenic tone of human pial arteries possible relation to distensibility. Stroke 28(12):2486–2492
Tkachenko E, Gutierrez E, Ginsberg MH, Groisman A (2009) An easy to assemble microfluidic perfusion device with a magnetic clamp. Lab Chip 9(8):1085–1095. doi:10.1039/b812184b
Tokunaga O, Watanabe T (1987) Properties of endothelial cell and smooth muscle cell cultured in ambient pressure. In Vitro Cell Dev Biol 23(8):528–534
van der Meer AD, Poot AA, Duits MH, Feijen J, Vermes I (2009) Microfluidic technology in vascular research. J Biomed Biotechnol 2009:823148. doi:10.1155/2009/823148
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332(6163):411–415. doi:10.1038/332411a0
Acknowledgments
The work was supported by National Basic Research Program of China (No. 2011CB933102), National Natural Science Foundation of China (No. 61078074 and 11004205) and Hong Kong RGC (No. GRF604712). The authors thank Dr. Jing Li from the School of Public Health, Peking University, for his kind permission to use the microplate reader. The authors also express gratitude to Dr. Zhizhu He for helpful discussions.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Li, L., Yang, Y., Shi, X. et al. A microfluidic system for the study of the response of endothelial cells under pressure. Microfluid Nanofluid 16, 1089–1096 (2014). https://doi.org/10.1007/s10404-013-1275-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10404-013-1275-9