Abstract
This study reports on the development of an integrated microfluidic system that performs sample pretreatment, nucleic acid amplification, and optical detection for molecular diagnosis of influenza viruses. The entire analysis protocol including virus lysis, extraction of ribonucleic acid, reverse transcription, polymerase chain reaction, and optical detection was successfully performed using the microfluidic system, which automatically performed the rapid diagnosis and subtyping of the influenza viruses. Signals obtained from an optical detection module could accurately differentiate influenza A/H1 (infA/H1), influenza A/H3 (infA/H3), influenza B (infB), and positive and negative control samples. More importantly, the entire process could be integrated and performed automatically with less human intervention. The experimental results demonstrated that this developed microfluidic system can successfully distinguish between infA/H1, infA/H3, and infB within 60 min. Furthermore, oral swabs from 92 patients were successfully tested using the developed microfluidic system. Thus, it may be a promising tool for rapid detection of novel and seasonal influenza strains in the near future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The spread of infectious diseases, such as influenza, has become a global health concern. It remains a challenge for any health authority or Center for Disease Control (CDC) to quickly and precisely diagnose diseases in order to control the spread of a novel infectious strain. More seriously, the deaths of 250,000–500,000 people annually worldwide attribute to the spread of influenza, and the number of deaths could increase into the millions in some pandemic years (Simonsen et al. 1997). There are three types of influenza viruses, called A, B, and C, which are commonly categorized based on the antigenic differences between two internal structural proteins known as the nucleoprotein (NP) and the matrix protein (M1) (Webster et al. 1992). Influenza viruses A and B can make human beings severely ill, but influenza C only results in mild symptoms in human beings (Matsuzaki et al. 2006). For instance, various subtypes of influenza A virus infections that have caused severe breakouts have been attributed to influenza pandemics. Influenza A can be further classified by differences in the expressed surface proteins on the viral envelope called hemagglutinin (HA) and neuraminidase (NA). To date, 17 subtypes of HA (H1–H17) and 10 subtypes of NA (N1–N10) have been discovered in different combinations from birds, animals, and human beings (Zhu et al. 2012). However, only three HA subtypes (H1–H3) and two NA subtypes (N1–N2) have been found to infect humans frequently (Alexander et al. 1981). Consequently, the majority of clinical issues associated with seasonal influenza A viruses are associated with these subtypes. For example, the H1N1 subtype that emerged in 1918–1919 was responsible for the Spanish flu pandemic that caused the deaths of 50 million to 100 million people worldwide (Johnson and Mueller 2002). Similarly, the H2N2 pandemic was responsible for the Asian flu in 1957, and the H3N2 pandemic was responsible for the Hong Kong flu that killed one million people worldwide in 1968–1969 (Cox and Subbarao 2000). Furthermore, the first appearance of novel subtypes of the influenza virus has led to high-mortality pandemics. Specifically, the novel H1N1 that appeared in April 2009 has caused serious health concerns (Smith et al. 2009). A new H1N1 virus with a new combination of genes from American pigs, Eurasian pigs, birds, and humans infected people and quickly spread worldwide, causing a pandemic that was recognized as a swine-origin influenza virus (Medina and Garcia-Sastre 2011). Recently, influenza infections have become one of the most prevalent diseases. Therefore, it is critical to develop a platform for the rapid and accurate diagnosis of influenza infections, especially for subtyping of the influenza viruses, in order to prevent a pandemic outbreak.
Traditionally, the enzyme-linked immunosorbent assay is one of the most commonly used protocols by hospitals and laboratories for clinical diagnosis (Zheng et al. 1990; Siavashi et al. 2005). However, there exist several concerns for this approach. For instance, it involves several labor-intensive processes requiring a series of tedious washing steps. It also has to be performed by well-trained personnel. Currently, immunoassay kits have been commonly used for fast screening of influenza infections (Chambers et al. 1994; Gavin and Thomson 2003). Moreover, their relatively low sensitivity may not meet the needs of practical applications, especially for sensitive detection of clinical or laboratory tests (Hurt et al. 2009; Faix et al. 2009; Vasoo et al. 2009). Therefore, there exists a critical need to develop systems that can simplify, expedite, and miniaturize the detection of influenza infections.
Alternatively, molecular detection may provide a more sensitive and selective diagnosis. Traditional reverse-transcription polymerase chain reaction (RT-PCR) and slab-gel electrophoresis can be used for detection of an influenza infection (Atmar et al. 1996; Smith et al. 2003; Hindiyeh et al. 2005). However, it usually takes more than 4 h for gene amplification, separation of the amplified DNA segments, and detection. Furthermore, tedious sample pretreatment steps such as virus isolation and RNA extraction are still labor-intensive and time-consuming processes. Therefore, there is a great need to develop a new platform to automate and to quickly perform these above-mentioned processes.
For a conventional molecular diagnosis assay, a critical issue was that the RNA samples were easily degraded by the surrounding RNases (Chirgwin et al. 1979; Chomczynski 1993). Therefore, there is a great need to develop a rapid and efficient extraction method to collect RNA from the viruses. Furthermore, the entire process should be integrated and performed automatically with less human intervention. Recently, various methods for extracting RNA have been reported (Akin et al. 1998; Cao et al. 2003; Li et al. 2006). For instance, in order to reduce the labor-intensive process necessary to obtain high-quality RNA, magnetic beads have been widely employed for RNA extraction (Choi et al. 2000; Huang et al. 2002; Gijs 2004; Li et al. 2008). Recently, specific nucleotide probes conjugated onto the surface of magnetic beads by utilizing the carboxylated linkage (Hawkins et al. 1994) have been integrated into microfluidic systems to enhance their performance. Due to the fact that high surface-to-volume ratio of the magnetic beads selectively modified with a variety of detection targets, the application of oligonucleotide-conjugated magnetic beads for isolation of specific nucleic acid sequences involved DNA hybridization (Jungell-Nortamo et al. 1988) can be greatly improved. Hence, sequence-specific hybridization capture on magnetic beads can be further easily manipulated, sorted, and concentrated in the microfluidic systems. Therefore, more bead-based assays have been extensively employed recently on microfluidic systems (Lien et al. 2009; Liu et al. 2009; McCalla et al. 2012). In comparison with the conventional method (Chomczynski and Mackey 1995), the extraction of RNA samples can be stably extracted and easily performed by applying an external magnetic field.
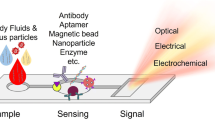
In the recent years, micro-electro-mechanical systems (MEMS) technology has been extensively employed for lab-on-a-chip (LOC) applications. These microfluidic systems comprised interconnected fluidic microchannel networks, microvalves, micromixers, micropumps, and reaction chambers may perform many of the required protocol steps (Auroux et al. 2002; Grodzinski et al. 2004; Vilkner et al. 2004). In the past two decades, LOCs that can provide even superior performance when compared with their large-scale counterparts have been successfully demonstrated. For instance, our previous study showed that sample pretreatment of viruses could be performed using a microfluidic system (Wang et al. 2012). However, it was relatively costly since it used fluorescent TaqMan probes. Furthermore, optical detection was still challenging to integrate into a single system, which is crucial for fast and accurate diagnosis of viruses.
In this study, we therefore develop a microfluidic system for automatic detection of influenza viruses in patient samples. The microfluidic system consists of a microfluidic control module for the transport of small amount of fluids, a magnet for magnetic isolation of RNA, a temperature control module equipped with a thermoelectric (TE) cooler, and an optical detection module with a fluorescent dye (SYBR Green dye) for detecting the amplified RT-PCR products. Current MEMS and microfluidic systems that detect influenza usually suffer from limited sample processing capability, as they typically detect only the presence of a single target at a time. Since the diagnosis, as well as the administration of treatments for influenza infections, requires the testing of multiple potential viruses (e.g., infA/H1, infA/H3, and infB), these existing systems are thus insufficient as realistic diagnostics. To overcome this limitation, the developed microfluidic system may perform parallel assays to simultaneously detect and subtype infA/H1, infA/H3, and infB while also including the three positive controls and one negative control as assay verification. Note that we used three types of DNA for the positive controls, one infA/H1-positive test, one infA/H3-positive test, and one infB-positive test. More importantly, this microfluidic system is capable of performing the entire assay, including virus lysis, RNA extraction, reverse transcription, polymerase chain reaction, and integrated optical detection in a completely automated fashion. As a further improvement, this new magnetic-bead-based microfluidic system could rapidly diagnose and subtype various influenza viruses within 60 min, which has shortened the assay time by approximately 45 % when compared to our previous study (110 min). Using patient samples, this microfluidic system showed a higher accuracy and was more time-efficient. Totally, 92 clinical specimens were successfully tested. An oral swab from a patient with suspected influenza infections can be rapidly detected using the microfluidic system. Using this approach, the results from this study revealed that the analysis can be automatically performed with a smaller biosample (10 μL), and less sample/reagent consumption in a shorter period of time (within 60 min).
2 Materials and methods
2.1 Experimental process
Magnetic beads (stock concentration = 4 × 108 beads/mL, bead diameter = 4.5 μm, Dynabeads® Myone™ Carboxylic Acid, Invitrogen, USA) conjugated with various subtype-specific nucleotide probes including an InfA/H1 probe (5′-TTTTTTTTTTAGACACAATATGTATAGGCTACCATG-3′), an InfA/H3 probe (5′-TTTTTTTTTTAGAATAAGCATCTATTGGACAATAGT-3′), and an InfB probe (5′-TTTTTTTTTTACTACTCATGGTAGTAACATCCAATG-3′) were first loaded into the sample chambers, respectively (Fig. 1a; Wang et al. 2012). A temperature of 95 °C was then applied to lyse the viruses using a temperature control module, followed by hybridizing the released viral RNA with the oligonucleotide probes, which were conjugated onto the surface of the magnetic beads at a temperature of 60 °C (Fig. 1b). Then, the magnetic beads with the attached viral RNA were magnetically purified (Fig. 1c). The RNA was then reverse-transcribed into DNA (Fig. 1d), followed by a nucleic acid amplification step (Fig. 1e) using the same temperature control module. Finally, the amplified RT-PCR products were detected by an optical detection module (Fig. 1f) using a SYBR Green dye.
2.2 Chip design and fabrication process
Figure 2a shows an exploded view of the integrated microfluidic chip consisting of two polydimethylsiloxane (PDMS, Sylgad 184A/B, Dow Corning Corp., USA) layers and one glass plate. The developed microfluidic chip was designed for performing sample pretreatment, nucleic acid amplification, and optical detection for molecular diagnosis of influenza viruses. The entire process including virus lysis, extraction of RNA, a one-step RT-PCR process, and optical detection was integrated into the microfluidic chip, which automatically performed the rapid diagnosis and subtyping of the influenza virus. Table 1 lists the detailed protocol and the operating conditions for each process step. The developed microfluidic chip consisted of a two-layer PDMS structures (i.e., a thick PDMS layer and thin PDMS layer) and one glass substrate, as schematically shown in Fig. 2b. Two major components integrated in this chip were normally closed microvalves (Yang et al. 2009) and four suction-type micropumps (Weng et al. 2011a, b). Note that the four suction-type micropumps were used for one infA/H1 test, one infA/H3 test, one infB test, and one negative control test. Both of them were fabricated using microfabrication processes. Briefly, the master molds with microfluidic structures on polymethylmethacrylate were formed using a computer-numerical-control machining process (EGX-400, Roland Inc., Japan) equipped with a 0.5-mm drill bit (Yang et al. 2009). Utilizing a PDMS replication technique, the inverse microstructures of the fluidic channels and the air chambers could be obtained. The thick-film PDMS layer and thin-film PDMS layer were then bonded together using an oxygen plasma treatment. Finally, a soda-lime glass substrate (G-Tech Optoelectronics Corp., Taiwan) was bonded with the PDMS structures to form the microfluidic chip. A photograph of the integrated microfluidic chip, which can automatically perform the entire analysis process, is shown in Fig. 2c. The dimensions of the chip were measured to be 7.5 cm × 5.9 cm.
a An exploded view of the integrated microfluidic chip. It consisted of two PDMS layers and one glass plate. b A schematic illustration of the integrated microfluidic chip consisting of a thick-film PDMS layer, a thin-film PDMS layer, and a glass substrate. c A photograph of an assembled microfluidic chip. The dimensions of the chip were measured to be 7.5 cm × 5.9 cm (length × width)
2.3 Working principle
The working principle of the suction-type micropump is schematically illustrated in Fig. 3. The driving force for liquid transport is the negative gauge pressure that creates a suction force. Figure 3a shows the initial state of the suction-type micropump. The sample fluid was first loaded into the inlet chamber. Figure 3b shows the deflections of the PDMS membranes when there was a negative gauge pressure in the air chambers, such that the fluidic sample could be drawn into the fluidic reservoir. Then, the normally closed microvalve on the left side was released when the normally closed microvalve on the right side was switched on (Fig. 3c). With this approach, the floating-block structure in the left microchannel can be switched off to push the sample forward. Next, all the PDMS membranes of the micropump and the right normally closed microvalve were released to push the liquid forward into the outlet chamber (Fig. 3d). The activation time of each step was set to be 1 s. Therefore, a total of 3 s per cycle was used. Digital signals from a custom-made control circuit were used to regulate electromagnetic valves (EMVs, SMC Inc., S070M-5BG-32, Japan) to control the motion of these membranes. Detailed information about this micropump could be found in our previous work (Weng et al. 2011a, b). In this study, the integrated microfluidic system that can perform the entire process for the detection of influenza viruses has been demonstrated. It can carry out multiple reactions for multiple detections of influenza viruses. Successful demonstration for the rapid detection and subtyping of influenza viruses from clinical samples has been achieved using the developed microfluidic system.
The working principle for the micropump. a The initial state of the suction-type micropump. b The PDMS membranes were deflected by the negative gauge pressure in the air chambers. c The normally closed microvalve on the left-hand side was released when the normally closed microvalve on the right-hand side was switched on. d With this approach, the floating-block structure in the left microchannel can be switched off to push the sample forward. Next, all of the PDMS membranes of the micropump and right normally closed microvalve were released to push the liquid forward into the outlet chamber
2.4 Custom-made system
Figure 4a shows a schematic illustration of the microfluidic detection system. The custom-made system consists of an air compressor (UN-90 V, UNI-CROWN Inc., Taiwan) equipped with several EMVs (S070M-5BG-32, SMC Inc., Japan) to control the motion of the PDMS membranes for transport fluids, a magnet to collect the magnetic beads for purification of RNA, and a temperature control module (USB4718, Advantech Corp., Taiwan) equipped with a thermoelectric (TE) cooler (TEC1-127.10, TANDE Corp., Taiwan) for RT-PCR thermal process, and an optical detection module is comprised of a laser (MBL5, CNI Corp., China) to excite fluorescent dyes, a band-pass filter (525/20 BP, Chroma Technology Corp., USA) and a dichroic mirror (505LP, Chroma Technology Corp., USA) to filter light with wavelengths ranging from 515 to 535 nm, a PMT (R928, Hamamatsu Corp., Japan) for the collection of fluorescent signals, a collimating lens (NT45-233, ONSET ELECTRO-OPTICS Corp., Taiwan) to focus the lights, and a data acquisition card (USB4716, Advantech Corp., Taiwan) to transform fluorescent signals into electronic signals. The dimensions of the custom-made system were measured to be 45 × 40 × 35 cm, as shown in Fig. 4b. The magnet could be controlled to place underneath the microfluidic chip during the operation.
2.5 Virus preparation
InfA/H1 (a subtype of H1N1, 95N2H1), InfA/H3 (a subtype of H3N2, A/California/7/2004), and InfB (94N399IB) were first mixed in serum separately and then added to washed, near-confluent (90 %) monolayers of Madin-Darby canine kidney (MDCK) cells and incubated at 35 °C with 5 % CO2. The virus/serum mixture was then replaced with a serum-free medium supplemented with 0.05 % Trypsin–EDTA (Invitrogen™, USA), and the cells were incubated at 35 °C with 5 % CO2. After harvesting the supernatant from the culture medium, this virus-containing culture supernatant was stored at −80 °C prior to usage. The initial titers of the stock of the three viruses were measured to be 1.28 hemagglutinin units (HAU). All operations were carried out according to the safety instructions provided by the National Institutes of Health in Taiwan.
Clinical specimens were obtained from the Microbiology and Immunology Laboratory of National Cheng Kung University (NCKU) in Taiwan and the Department of Pathology of NCKU Hospital in Taiwan. These clinical specimens were stored at −80 °C until tested. A total of 92 clinical samples were collected, 30 of which were known negative samples and the other 62 samples were known positive samples.
2.6 Positive control
The cloning protocol followed the user guide for the TOPO TA cloning® kit (Invitrogen Co., USA). The RT-PCR products were used by using specific forward/reverse primer pairs to amplify the HA gene of infA/H1, infA/H3, and infB. All 6 μL cloning mixtures contained 4 μL of freshly made PCR products, 1 μL of TOPO® vector, and 1 μL of salt solution. The mixture was gently mixed and incubated for 5 min at room temperature. One tube of Shot® E. coli cell was thawed on ice. Two microliters of cloning mixture was added to Shot® E. coli, mixed gently, and put on ice. All of the mixtures were incubated on ice for 30 min and heat-shocked for 30 s at 42 °C without shaking. Finally, 250 μL of LB broth was added to the transformation mixture and shaking continuously at 37 °C for 1 h. Fifty microliters of this transformation solution was then spread on a LB-Amp (ampicillin 100 mg/mL, Sigma Co., USA) plate and then incubated overnight at 37 °C. The transformants were finally selected and analyzed by a subtype-specific PCR for the detection of influenza virus.
2.7 One-step RT-PCR protocol
PCR amplification is a well-known method for the amplification of nucleic acids and can be used to verify whether the released RNA can be stably extracted and converted to stable complementary DNA (cDNA). In this study, a one-step RT-PCR with hydrolysis probes was applied to the diagnosis of various RNA viruses. The RNA purified either from patient samples or from cultured laboratory samples was further examined using a commercial kit (KK4660 KAPA SYBR® FAST One-Step qRT-PCR kit, ABI Prism™, USA). All the RT-PCR processes were performed using the temperature control module equipped with a TE cooler, which was placed underneath the microfluidic chip. Twenty microliters of reaction reagents was used, which was composed of 5 μL of bead-captured viral RNA sample, 10 μL of KAPA SYBR FAST qPCR Master Mix (2×), 0.4 μL of deoxyuridine triphosphate (dUTP, 10 mM), 0.4 μL of KAPA RT Mix (50×), 0.4 μL of each primer for InfA/H1, InfA/H3, and InfB forward/reverse primers (Wang et al. 2012), and 3.4 μL of double-distilled water (ddH2O). The reaction reagents were first loaded into the RT-PCR chamber and were pumped to the reaction chamber. The cDNA synthesis process at 42 °C for 5 min was followed by thermocycling processes, which included an initial denaturing step at 95 °C for 5 min, then denaturing at 95 °C for 3 s, annealing at 58 °C for 20 s, and extension at 72 °C for 1 s for a total of 40 cycles. Finally, the amplified RT-PCR products were detected by an integrated optical detection module.
For the negative control, the template RNA was replaced by RNase-free water. In order to confirm the PCR process, we used three types of DNA for the positive controls, which were cloned from hemagglutinin fragment of InfA/H1 (2.68 μg/mL), InfA/H3 (2.43 μg/mL), and InfB (2.05 μg/mL), respectively. Twenty microliters of the reaction reagents was used, which was composed of 1 μL of the positive-control DNA sample, 10 μL of KAPA SYBR FAST qPCR Master Mix (2×), 0.4 μL of dUTP (10 mM), 0.4 μL of KAPA RT Mix (50×), 0.4 μL of each primer for InfA/H1, InfA/H3, and InfB forward/reverse primers, and 7.4 μL of ddH2O. These control samples were loaded into the corresponding InfA/H1, InfA/H3, and InfB-positive-control chamber. Note that the signals from the three positive controls (InfA/H1, InfA/H3, and InfB) were around 0.834, 0.828, and 0.794 V, respectively. All of the three controls were measured with strong signals using the optical detection module for confirming our experiments. If one of their signals is close to one for the negative control (double-distilled water), the platform is not reliable. This indication can improve the reliability of our platform.
The sensitivity and specificity were determined by comparing against a standard, commercially available isolation kit (QIAamp Viral RNA Mini kit, QIAGEN, Germany) obtained from the Microbiology and Immunology Laboratory of NCKU in Taiwan to verify that our developed system achieved comparable results.
3 Results and discussion
3.1 Characterization of the micropump
In this study, an integrated microfluidic chip was designed and fabricated for fast diagnosis and subtyping of influenza viruses. A suction-type micropump incorporated with a normally closed microvalve was adopted for precise liquid delivery such that the entire assay could be automated. The performance of the micropump is crucial for driving the liquid in the integrated microfluidic chip, as described in the previous sections. It is important to explore the relationship between the pumping rate and the applied air pressure when optimizing the operating conditions. Figure 5 shows the relationship between the pumping rate and the applied air pressure of the developed micropump when operated at −20, −25, −30, −40, −50, −60, −70, and −80 kPa, respectively. The pumping rate could be as high as 372.24 ± 15.95 μL/min, when actuated at a pressure of −70 kPa. Considering a reproducible pumping rate, the suction-type micropump was activated at a pressure of −50 kPa, corresponding to a pumping rate of 345.46 ± 11.14 μL/min in the subsequent experiments. Note that the error bars shown in Fig. 5 were obtained from three repeated measurements.
3.2 Selectivity test
In order to test the selectivity of the probe-conjugated magnetic beads, the specific nucleotide probes for infA/H1 (1.28 HAU), infA/H3 (1.28 HAU), and infB (1.28 HAU) were used for the extraction of viral RNA and hybridization with infA/H1 (lane 1), infA/H3 (lane 5), and infB (lane 9) strains, respectively, as shown in Fig. 6a. These experimental results demonstrated excellent selectivity to infA/H1, infA/H3, and infB with extremely high optical signals, 0.612 ± 0.027, 0.785 ± 0.013, and 1.112 ± 0.018 V, respectively. In addition, Fig. 6a also shows that the infA/H1 probe-conjugated beads incubated with infA/H3 and infB isolates (lanes 2 and lane 3) or infA/H3 probe-conjugated beads incubated with the infA/H1 and infB isolates (lane 4 and lane 6) or infB probe-conjugated beads incubated with the infA/H1 and infA/H3 isolates (lane 7 and lane 8) could not generate PCR products, as indicated by detection signals close to the negative control level (lane 2, lane 3, lane 4, lane 6, lane 7, lane 8, and NC were 0.194 ± 0.011, 0.201 ± 0.026, 0.199 ± 0.024, 0.186 ± 0.015, 0.194 ± 0.014, 0.212 ± 0.022, and 0.180 V ± 0.012, respectively). Note that the error bars shown here were obtained from three repeated measurements.
a Selectivity results for the microfluidic chip by using the optical detection module. b The length of the infA/H1, infA/H3, and infB detection genes were 249, 147, and 170 bp, respectively. The results showed that infA/H1, infA/H3, and infB probes were highly specific to subtyping of influenza viruses
In order to confirm the validity of the optical signals from the developed integrated chip, the RT-PCR products were also visualized by using gel electrophoresis on a 2 % agarose gel with ethidium bromide staining. Figure 6b shows a gel image of the PCR products amplified from the DNA transcribed from the total RNA that was extracted using the super-paramagnetic-bead-based method (Wang et al. 2012). The length of the detection genes for infA/H1, infA/H3, and infB were 249, 147, and 170 base pairs (bp), respectively. Note that lane L used a 100-bp DNA ladder marker and lane NC used ddH2O as a template. These results showed that the infA/H1, infA/H3, or infB probes provided a high selectivity for subtyping of influenza viruses and only the expected subtypes of samples were amplified successfully. No cross-reactivity was observed among infA/H1, infA/H3, and infB viruses, thus demonstrating high specificity by using the subtype-specific primers/probe.
3.3 Limit of detection of the integrated microfluidic system
In order to explore LOD of the developed microfluidic chip, three experiments were performed. Purified virus cultured in the laboratory was first used to test for the LOD. Four different concentrations of infA/H1 viruses, specifically lane 1 (1.28 HAU), lane 2 (0.128_HAU), lane 3 (0.0128 HAU), and lane 4 (0.00128 HAU), were loaded into the integrated microfluidic chip, as shown in Fig. 7a. The optical signals for the various infA/H1 concentrations were measured to be 0.576 ± 0.026, 0.513 ± 0.019, 0.346 ± 0.017, and 0.183 ± 0.016 V, respectively. Note that the signal for the negative control was around 0.180 ± 0.015 V. Note that the error bars shown here were obtained from three repeated measurements. Experimental results demonstrated that the detection limit of this microsystem was found to be a 102 dilution of 1.28 HAU of infA/H1 (0.0128 HAU). In order to confirm the validity of the optical signals from the developed integrated chip, Fig. 8a shows a gel image of the amplified PCR products for comparison. Note that the length of the infA/H1 detection gene was 249 bp and the lane L used a 50-bp DNA ladder marker. Lanes 1, 2, 3, and 4 were 1.28, 0.128, 0.0128, and 0.00128 HAU, respectively, and lane NC used ddH2O as a template.
Sensitivity results for the microfluidic chip by using the optical detection module; different concentrations of influenza A/H1, influenza A/H3, and influenza B viruses diluted from a sample with an initial concentration of 12.8 HAU/5 μL were tested. a A series of images of the magnetic complexes with different viral concentrations of influenza A/H1 when operated by the microfluidic chip, b optical signals from the detection of influenza A/H3 at different concentrations in the microfluidic chip, c optical signals from the detection of influenza B at different concentrations
Sensitivity results for the microfluidic chip by using slab-gel electrophoresis. a Gel image of the amplified PCR products; note that the length of the infA/H1 detection gene was 249 bp. b Gel image of the amplified PCR products. Note that the length of the infA/H3 detection gene was 147 bp. c Gel image of the amplified PCR products. Note that the length of infA/H1 was 147 bp
Similarly, four different concentrations of infA/H3 viruses, specifically lane 1 (1.28 HAU), lane 2 (0.128_HAU), lane 3 (0.0128 HAU), and lane 4 (0.00128 HAU), were loaded into the integrated microfluidic chip to test the LOD for InfA/H3, as shown in Fig. 7b. The optical signals from the infA/H3 samples were measured to be 0.732 ± 0.025, 0.678 ± 0.022, 0.479 ± 0.012, and 0.180 ± 0.018 V, respectively. Note that the signal from the negative control was around 0.174 ± 0.011 V. The error bars shown were obtained from three repeated measurements. These experimental results revealed that the LOD of the microsystem was a 102 dilution of 1.28 HAU (0.0128 HAU) for infA/H3. Similarly, in order to confirm the validity of the optical signals from the integrated chip, Fig. 8b shows a gel electrophoresis image of the amplified PCR products amplified for comparison. Note that the length of the infA/H3 detection gene was 147 bp and the lane L used a 50-bp DNA ladder marker. Lanes 1, 2, 3, and 4 were 1.28, 0.128, 0.0128, and 0.00128 HAU, respectively, and lane NC used ddH2O as a template.
In addition, five different concentrations of infB viruses, specifically lane 1 (1.28 HAU), lane 2 (0.128 HAU), lane 3 (0.0128 HAU), lane 4 (0.00128 HAU), and lane 5 (0.000128 HAU), were loaded into the integrated microfluidic chip to test the LOD, as shown in Fig. 7c. The optical signals for infB were measured to be 1.089 ± 0.023, 0.985 ± 0.083, 0.690 ± 0.015, 0.457 ± 0.092, and 0.185 ± 0.031 V, respectively. Note that the signal for the negative control was around 0.181 ± 0.042 V. The error bars shown were obtained from three repeated measurements. These experimental results demonstrated that the detection limit of the microsystem was a 103 dilution of 1.28 HAU for infB (0.00128 HAU). Again, in order to confirm the validity of the optical signals from the developed integrated chip, Fig. 8c shows a gel electrophoresis image of the amplified PCR products. Note that the length of the infB detection gene was 147 bp and the lane L used a 50-bp DNA ladder marker. Lanes 1, 2, 3, 4, and 5 were 1.28, 0.128, 0.0128, 0.00128, and 0.000128 HAU, respectively, and lane NC used ddH2O as a template.
To convert the HAU values of virus samples to copy numbers, viral RNA was extracted from the virus samples, measured by a spectrophotometer, and calculated based on the established relationship (Witthaya et al. 2011). The extraction of total RNA from the virus samples was performed by using the QIAamp Viral RNA Mini kit (QIAGEN, Germany). The concentrations of the extracted total RNA were determined by a spectrophotometer (Beckman, DU530 UV/Vis, USA). The copy numbers of RNA were then calculated by the following formula (Kamol et al. 2008).
Initial concentrations of the three viruses (infA/H1, infA/H3, and infB) at 128 HAU were then calculated to be 1.6 × 108, 1.0 × 108, and 2.7 × 108 copies, respectively. Therefore, our HAU results can be converted to copy numbers. Experimental results for the LOD of infA/H1, infA/H3, and infB were measured to be 1.6 × 103, 1.0 × 103, and 2.7 × 102 copies, respectively. Our results showed acceptable LOD in comparison with many reports or kits (Boonsuk et al. 2008). Note that the previous studies (Payungporn et al. 2006; Li et al. 2006; Thontiravong et al. 2007; Zhang and Xing 2010) showed that the LODs of influenza diagnosis were between 10 and 104 copies by using purified viral RNA samples.
3.4 Diagnosis of influenza infections using clinical specimens
According to the aforementioned experimental conditions and the promising characterization results from the integrated microfluidic chip, clinical specimens were next tested. The microfluidic chip was designed with multiple detection regions, three positive tests, and one negative test. Ninety-two specimens were tested using the prototype microfluidic chips. The sensitivity and specificity were determined by comparing against gold standards (QIAamp Viral RNA Mini kit, QIAGEN, Germany) obtained from the Microbiology and Immunology Laboratory of NCKU in Taiwan and the Department of Pathology of NCKU Hospital in Taiwan to verify that our developed system achieved comparable results. Table 2 shows the summary of the infA/H1 test results. A sensitivity of 90 % and a specificity of 100 % were verified. Similarly, Table 3 shows the summary of the infA/H3 test results. A sensitivity of 91 % and a specificity of 100 % were verified. Table 4 shows the summary of the infB test results. A sensitivity of 90 % and a specificity of 100 % were verified accordingly. The entire experimental protocol was performed automatically within 60 min, and all the results showed that the developed microfluidic chip could detect clinical samples successfully with a high specificity and sensitivity. It therefore has several advantages when compared with the gold standard, including reduced consumption of biosamples (10 μL) and reagents (215 μL), automation, and a shorter time (within 60 min) for analysis. Note that the gold standard required 140 μL of biosamples and 2,810 μL of reagents and took about 100 min.
4 Conclusion
In this study, an integrated microfluidic system with the capability to automatically perform viral lysis, RNA extraction, a one-step RT-PCR process, and optical detection was successfully demonstrated. The RNA was successfully purified from viruses and clinical specimens utilizing the proposed magnetic-bead-based method within the microfluidic system. Compared to a conventional method (QIAamp Viral RNA Mini kit, QIAGEN, Germany) that required 100 min to perform the entire RNA isolation, nucleic acid amplification, and detection steps, our prototype microfluidic system could perform the entire process within 60 min. Moreover, the system performed the entire process automatically, making it less labor-intensive and greatly reducing the risk of contamination of the results or risk of infection to the operator. Furthermore, the subtyping of the influenza viruses could be realized on this developed system. In conclusion, our developed microfluidic system may provide a powerful alternative platform for fast diagnosis of influenza viruses.
Abbreviations
- bp:
-
Base pairs
- CNC:
-
Computer-numerical-control
- cDNA:
-
Complementary DNA
- ddH2O:
-
Double-distilled water
- dUTP:
-
Deoxyuridine triphosphate
- EMVs:
-
Electromagnetic valves
- HA:
-
Hemagglutinin
- HAU:
-
Hemagglutinin unit
- infA/H1:
-
Influenza A/H1
- infA/H3:
-
Influenza A/H3
- infB:
-
Influenza B
- LOD:
-
Limit of detection
- MEMS:
-
Micro-electro-mechanical systems
- NA:
-
Neuraminidase
- NP:
-
Nucleoprotein
- PCR:
-
Polymerase chain reaction
- PDMS:
-
Polydimethylsiloxane
- PMMA:
-
Polymethylmethacrylate
- RNA:
-
Ribonucleic acid
- RNAse:
-
Ribonuclease
- RT:
-
Reverse transcription
- RT-PCR:
-
Reverse-transcription polymerase chain reaction
- SOIV:
-
Swine-origin influenza virus
- TE:
-
Thermoelectric
References
Akin A, Wu CC, Lin TL (1998) A comparison of two RNA isolation methods for double-stranded RNA of infectious bursal disease virus. J Virol Methods 74:179–184
Alexander DJ, Assaad F, Bachmann PA, Bögel K, Chu H, Easterday BC, Hannoun CM, Kaplan MM, Laver WG, Ottis K, Romvary JJ, Scholtissek C, Shortridge KF, Slepuskin AN, Tumova B, Webster RG (1981) The ecology of influenza viruses: a WHO memorandum. Bull World Health Organ 59(6):869–873
Atmar RL, Baxter BD, Dominguez EA, Taber LH (1996) Comparison of reverse transcription-PCR with tissue culture and other rapid diagnostic assays for detection of type A influenza virus. J Clin Microbiol 34(10):2604–2606
Auroux PA, Iossifidi D, Reyes DR, Manz A (2002) Micro total analysis systems. 2. Analytical standard operations and applications. Anal Bioanal Chem 74:2637–2652
Boonsuk P, Payungporn S, Chieochansin T, Samransamruajkit R, Amonsin A, Songserm T, Chaisingh A, Chamnanpood P, Chutinimitkul S, Theamboonlers A, Poovorawan Y (2008) Detection of influenza virus types A and B and type A subtypes (H1, H3, and H5) by multiplex polymerase chain reaction. Tohoku J Exp Med 215(3):247–255
Cao QF, Meng YP, Sun Y (2003) An effective quick method for total RNA extraction in Malus. J Agric Biotechnol 11(4):428–429
Chambers TM, Shortridge KF, Li PH, Powell DG, Watkins KL (1994) Rapid diagnosis of equine influenza by the Directigen FLU-A enzyme immunoassay. Vet Rec 135(12):275–279
Chirgwin JM, Przybyla AE, MacDonald RJ, Rutter WJ (1979) Isolation of biologically active ribonucleic acid from sources enriched in ribonuclease. Biochemistry 18:5294–5299
Choi JW, Ahn CH, Bhansali S, Henderson HT (2000) A new magnetic bead-based, filterless bio-separator with planar electromagnet surfaces for integrated bio-detection systems. Sens Actuators B Chem 68:34–39
Chomczynski P (1993) A reagent for the single-step simultaneous isolation of RNA, DNA and proteins from cell and tissue samples. Biotechniques 15:532–537
Chomczynski P, Mackey K (1995) Short technical report. Modification of the TRIZOL reagent procedure for isolation of RNA from Polysaccharide-and proteoglycan-rich sources. Biotechniques 19(6):942–945
Cox NJ, Subbarao K (2000) Global epidemiology of influenza: past and present. Annu Rev Med 51:407–421
Faix DJ, Sherman SS, Waterman SH (2009) Rapid-test sensitivity for novel swine-origin influenza A (H1N1) virus in humans. New Engl J Med 361:728–729
Gavin P, Thomson RB Jr (2003) Review of rapid diagnostic tests for influenza. Clin Appl Immunol Rev 4(3):151–172
Gijs MAM (2004) Magnetic bead handling on-chip: new opportunities for analytical applications. Microfluid Nanofluid 1:22–40
Grodzinski P, Liu R, Yang J, Ward MD (2004) Microfluidic system integration in sample preparation chip-sets-a summary. In: Proceedings of the 26th annual international conference of the IEEE EMBS, pp 2615–2618
Hawkins TL, O’Connor-Morin T, Roy A, Santillan C (1994) DNA purification and isolation using a solid-phase. Nucleic Acids Res 22(21):4543–4544
Hindiyeh M, Levy V, Azar R, Varsano N, Regev L, Shalev Y, Grossman Z, Mendelson E (2005) Evaluation of a multiplex real-time reverse transcriptase PCR assay for detection and differentiation of influenza viruses A and B during the 2001–2002 influenza season in Israel. J Clin Microbiol 43(2):589–595
Huang Y, Mather EL, Bell JL, Madou M (2002) MEMS-based sample preparation for molecular diagnostics. Anal Bioanal Chem 372:49–65
Hurt AC, Baas C, Deng YM, Roberts S, Kelso A, Barr IG (2009) Performance of influenza rapid point-of-care tests in the detection of swine lineage A (H1N1) influenza viruses. Influenza Other Respi Viruses 3(4):171–176
Johnson NP, Mueller J (2002) Updating the accounts: global mortality of the 1918–1920. Spanish influenza pandemic. Bull Hist Med 76(1):105–115
Jungell-Nortamo A, Syvänen AC, Luoma P, Söderlund H (1988) Nucleic acid sandwich hybridization: enhanced reaction rate with magnetic microparticles as carriers. Mol Cell Probes 2(4):281–288
Kamol S, Sunchai P, Thaweesak C, Rujipat S, Alongkorn A, Thaweesak S, Arunee C, Pornchai C, Salin C, Apiradee T, Yong P (2008) Typing (A/B) and subtyping (H1/H3/H5) of influenza A viruses by multiplex real-time RT-PCR assays. J Virol Methods 152:25–31
Li JH, Tang CH, Song CY, Chen MJ, Feng ZY, Pan YJ (2006) A simple, rapid and effective method for total RNA extraction from Lentinula edodes. Biotechnol Lett 28(15):1193–1197
Li SK, Lin CH, Chen YT, Lee LH, Liu HJ (2008) Development of a reliable assay protocol for identification of diseases (RAPID)-bioactive amplification with probing for detection of avian reovirus. J Virol Methods 149(1):35–41
Lien KY, Liu CJ, Lin YC, Kuo PL, Lee GB (2009) Extraction of genomic DNA and detection of single nucleotide polymorphism genotyping utilizing an integrated magnetic bead-based microfluidic platform. Microfluid Nanofluid 6:539–555
Liu CJ, Lien KY, Weng CY, Shin JW, Chang TY, Lee GB (2009) Magnetic-bead-based microfluidic system for ribonucleic acid extraction and reverse transcription processes. Biomed Microdevices 11:339–350
Matsuzaki Y, Katsushima N, Nagai Y, Shoji M, Itagaki T, Sakamoto M, Kitaoka S, Mizuta K, Nishimura H (2006) Clinical features of influenza C virus infection in children. J Infect Dis 193(9):1229–1235
McCalla SE, Ong C, Sarma A, Opal SM, Artenstein AW, Tripathi A (2012) A simple method for amplifying RNA targets (SMART). J Mol Diagn 14(4):328–335
Medina RA, Garcia-Sastre A (2011) Influenza A viruses: new research developments. Rev Microbiol 9:590–603
Payungporn S, Chutinimitkul S, Chaisingh A, Damrongwantanapokin S, Buranathai C, Amonsin A, Theamboonlers A, Poovorawan Y (2006) Single step multiplex real-time RT-PCR for H5N1 influenza A virus detection. J Virol Methods 1131:143–147
Siavashi MR, Taherkhani H, Rezaei K, Deligani MRR, Assmar M (2005) Comparison of Dot-ELISA and sandwich ELISA diagnostic tests in detection of human hydatidosis. Iran Biomed J 9(2):91–94
Simonsen L, Clarke MJ, Williamson GD, Stroup DF, Arden NH, Schonberger LB (1997) The impact of influenza epidemics on mortality: introducing a severity index. Am J Public Health 87(12):1944–1950
Smith AB, Mock B, Meleau R, Colarusso P, Willis DE (2003) Rapid detection of influenza A and B viruses in clinical specimens by Light Cycler real time RT-PCR. J Clin Virol 28(1):51–58
Smith GJ, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, Ma SK, Cheung CL, Raghwani J, Bhatt S, Peiris JS, Guan Y, Rambaut A (2009) Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 459(7250):1122–1125
Thontiravong A, Payungporn S, Keawcharoen J, Chutinimitkul S, Wattanodorn S, Damrongwatanapokin S, Chaisingh A, Theamboonlers A, Poovorawan Y, Oraveerakul K (2007) The single-step multiplex reverse transcription- polymerase chain reaction assay for detecting H5 and H7 avian influenza A viruses. Tohoku J Exp Med 211(1):75–79
Vasoo S, Stevens J, Singh K (2009) Rapid antigen tests for diagnosis of pandemic (swine) influenza A/H1N1. Clin Infect Dis 49:1090–1093
Vilkner T, Janasek D, Manz A (2004) Micro total analysis systems. Recent developments. Anal Chem 76:3373–3385
Wang CH, Lien KY, Hung LY, Lei HY, Lee GB (2012) Integrated microfluidic system for multiple subtyping of influenza virus by using molecular diagnosis approach. Microfluid Nanofluid 13(1):113–123
Webster RG, Bean WJ, Gorman OT (1992) Evolution and ecology of influenza-A virus. Rev Microbiol 56(1):152–179
Weng CH, Lien KY, Yang SY, Lee GB (2011a) A suction-type, pneumatic microfluidic device for liquid transport and mixing. Microfluid Nanofluid 10:301–310
Weng CH, Lien KY, Yang SY, Lee GB (2011b) A suction-type, pneumatic microfluidic device for liquid transport and mixing. Microfluid Nanofluid 10:301–310
Witthaya P, Piyathida P, Jarika M, Yong P, Sunchai P (2011) Molecular detection and subtyping of human influenza A virus based on multiplex RT-PCR assay. Int Res J Biotech 2(5):085–092
Yang YN, Hsiung SK, Lee GB (2009) A pneumatic micropump incorporated with a normally closed valve capable of generating a high pumping rate and a high back pressure. Microfluid Nanofluid 6:823–833
Zhang C, Xing D (2010) Single-molecule DNA amplification and analysis using microfluidics. Chem Rev 110:4910–4947
Zheng HJ, Tao ZH, Cheng WF, Piessens WF (1990) Comparison of dot-ELISA with sandwich ELISA for the detection of circulating antigens in patients with bancroftian filariasis. Am J Trop Med Hygiene 42:546–549
Zhu X, Yu W, McBride R, Li Y, Chen LM, Donis RO, Tong S, Paulson JC, Wilson LA (2012) Hemagglutinin homologue from H17N10 bat influenza virus exhibits divergent receptor-binding and pH-dependent fusion activities. Proc Natl Acad Sci 110(4):1458–1463
Acknowledgments
The authors would like to thank the National Science Council in Taiwan for financial support (NSC101-2120-M-007-014). Partial financial support from the Towards a World-Class University Project is also greatly appreciated.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Tai, CH., Tsai, YC., Wang, CH. et al. An integrated microfluidic platform for rapid detection and subtyping of influenza viruses from clinical samples. Microfluid Nanofluid 16, 501–512 (2014). https://doi.org/10.1007/s10404-013-1249-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10404-013-1249-y