Abstract
Purpose
This study aimed to determine the role of preoperative shoulder ultrasonography (SUS) in detecting positional abnormalities of the long head of the biceps tendon (LHBT) and predicting subscapularis (SSC) tears in patients with rotator cuff injuries.
Methods
A total of 331 patients (365 shoulders) who had undergone arthroscopic shoulder surgery for the treatment of rotator cuff tears were included in the study. Their preoperative SUS and magnetic resonance imaging (MRI) findings were examined retrospectively to assess the presence of LHBT abnormalities at the bicipital groove. Using arthroscopic findings as the standard of reference, the sensitivity, specificity, and diagnostic accuracy of SUS and MRI were calculated for detection of LHBT malposition. Furthermore, the correlation between SSC rupture and preoperative LHBT condition was evaluated by MRI and SUS.
Results
LHBT malposition was preoperatively diagnosed with a sensitivity of 92%, specificity of 90%, and accuracy of 91% with SUS, and a sensitivity of 74%, specificity of 84%, and accuracy of 80% with MRI. Preoperative SUS was significantly superior to MRI in terms of sensitivity, specificity, and accuracy (p < 0.001 each). Further, the preoperative SUS LHBT findings could predict well the presence or absence of intraoperative SSC rupture (odds ratio: 1.73, p < 0.001).
Conclusion
SUS is a useful diagnostic modality for preoperative detection of LHBT malposition and prediction of SSC tears in patients with rotator cuff tears.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Shoulder pain in the region of the long head of the biceps tendon (LHBT) has been acknowledged for a long time [1]. Positional abnormalities in the LHBT have been recognized as a cause of pain. The presence of subscapularis (SSC) tendon rupture in the joint has also been identified. Diagnosing the pathophysiology of LHBT in patients with rotator cuff tears before surgery is vital for predicting SSC tears [2].
It has been widely accepted that magnetic resonance imaging (MRI) is essential for diagnosing rotator cuff tears; however, the diagnostic accuracy of MRI is poor for detecting malposition of the LHBT. Thus, preoperative MRI findings often differ with intraoperative findings [3].
Shoulder ultrasonography (SUS) is a simple method that enables anterior observation of regions near the bicipital groove and real-time dynamic observation during internal and external rotation. SUS is an excellent option for delineating soft tissues and can depict not only LHBT malposition but also hypertrophy and partial rupture due to inflammation and degeneration of tendons and their surrounding tissues.
To the best of our knowledge, no study has confirmed the higher accuracy of SUS in identification of LHBT malposition in comparison to MRI findings. This study aimed to evaluate the possible role of SUS in preoperative assessment of such lesions in patients with rotator cuff injuries and prediction of subscapularis tears.
Materials and methods
This retrospective study was performed at a single institution on 331 patients (365 shoulders) between July 2012 and May 2020. The study was approved by the Uda City Hospital Ethics Committee (R3UHRNo005), and informed consent was obtained from all the patients. The study was performed in accordance with the tenets of the Declaration of Helsinki.
We excluded patients who did not have preoperative MRI data. Patients with a painful rotator cuff tear underwent preoperative evaluation with MRI and SUS assessments at multiple time points before arthroscopic surgery for the treatment of rotator cuff tears was performed.
SUS was performed using an Arietta scanner (Hitachi) with a linear array transducer (7.2–18 MHz). SUS was performed by four medical technicians with 2–5 years of experience with SUS who were blinded to the clinical history.
As reported previously, the average accuracy rate of intraoperative findings was 80% for LHBT, 88% for SSP, 68% for ISP, and 71% for SSC in each of 20 patients who underwent examination for rotator cuff tears. No significant difference was found in diagnostic accuracy between the four technicians. It is considered that accuracy and reliability were maintained between the technicians.
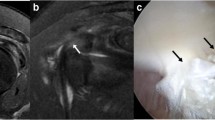
The LHBT lesions were classified into three categories, with the following definitions: Subluxation is defined as the medial displacement of the LHBT over the lesser tubercle, dislocation refers to complete deviation of the LHBT, and tear is indicated by the absence of tendon tissue within the bicipital groove without dislocation (Fig. 1). Furthermore, as a pathological finding of LHBT, color Doppler ultrasonography showed an increase in the number of micro-vessels around the inter-nodal sulcus. It also showed hypertrophy and partial rupture of the LHBT due to degeneration (Fig. 2).
Ultrasonic view of the long head of the biceps tendon (LHBT) with relation to the bicipital groove. a Normal anatomy of the LHBT in the bicipital groove, b Subluxation of the LHBT ( →) over the lesser tubercle, c Dislocation of the LHBT with complete deviation from the bicipital groove distal LHBT ( →), d Tear ( →) of the LHBT
Preoperative MRI was performed to assist the orthopedic surgeon in the surgical planning of rotator cuff repair. MRI was performed using a 3.0 Tesla MR, and T2-weighted radial images were examined for the appearance of LHBT malposition in cross-sectional imaging axial views. Cases where the LHBT could not be identified were classified as rupture. Subluxation was defined as the medial displacement of the LHBT in the bicipital groove over the lesser tubercle, dislocation referred to complete deviation, and rupture referred to absence of LHBT in the bicipital groove along with hypertrophic or edematous changes (Fig. 3).
Magnetic resonance imaging of the long head of the biceps tendon (LHBT) with relation to the bicipital groove. a Normal anatomy of the LHBT in the bicipital groove, b Subluxation of the LHBT over the lesser tubercle, c Dislocation of the LHBT with complete deviation from the bicipital groove, d Tear of the LHBT
In the study, comparisons were made between: (1) conformance of the intraoperative arthroscopic findings (Fig. 4) with the preoperative MRI and SUS findings for LHBT and (2) the predictive powers of preoperative MRI and SUS findings of LHBT malposition for predicting SSC tears.
Statistical analysis
Statistical analyses were performed using EZR ver. 1.54 (Easy R, Saitama, Japan). Multivariate analysis was performed to determine the sensitivity and specificity of the preoperative MRI and SUS findings based on the intraoperative findings of SSC rupture and LHBT lesions. A p value of 0.05 was considered statistically significant.
Results
There were 331 patients (181 males and 150 females) with rotator cuff tears included in this study. Their mean age was 65 years (range 18–90 years), mean duration of illness was 13 months (range 1–132 months), and postoperative mean observation period was 18 months (range 6–40 months).
Sensitivity
Of the 365 shoulders examined, 120 (33%) were diagnosed with positional LHBT abnormalities on diagnostic arthroscopy (Table 1). Of these, 84 cases showed abnormalities during both preoperative SUS and MRI, and 26 cases showed preoperative SUS abnormalities alone with normal MRI findings. However, four cases showed abnormalities on the preoperative MRI with normal SUS findings, and six cases showed normal preoperative investigative findings on SUS and MRI.
Specificity
Of the 245 shoulders (67%) that were diagnosed as normal on diagnostic arthroscopy (Table 2), 194 had normal preoperative findings on both SUS and MRI, 28 showed normal preoperative SUS findings and abnormalities on MRI, 12 showed normal preoperative MRI findings with abnormalities on SUS, and 11 showed abnormalities on both preoperative SUS and MRI.
The concordance of diagnostic arthroscopy with the preoperative findings of LHBT subluxation, dislocation, and tear is represented by a sensitivity of 92%, specificity of 90%, and accuracy of 91% for SUS, and a sensitivity of 74%, specificity of 84%, and accuracy of 80% for MRI (Table 3). The concordance of intraoperative findings with preoperative SUS and MRI findings was compared, and a significant difference was found in sensitivity, specificity, and accuracy in diagnosis (p < 0.001, respectively).
SUS and MRI findings of LHBT (Table 4)
As a result of comparing SUS and MRI findings in LHBT pathologies, abnormal LHBT findings were found with SUS in 212 cases (58%) and with MRI in 157 cases (43%). Hypertrophy/edema (SUS includes color Doppler) was detected in 86 cases (41%) and 30 cases (19%) with SUS and MRI, respectively. Subluxation was diagnosed in 85 cases (40%) and 80 cases (50%) with SUS and MRI, respectively. Dislocation was diagnosed in four cases (2%) with SUS and in three cases (2%) with MRI. Ruptures were found in 37 cases (17%) with SUS and in 44 cases (28%) with MRI. There was a significant difference between SUS and MRI findings (p < 0.001).
Correlation between SSC tear and preoperative LHBT condition according to SUS and MRI findings (Table 5)
Of the 365 shoulders, 184 shoulders (51%) showed no SSC tendon tears on diagnostic arthroscopy (Table 5). This included 48 (26%) cases that were diagnosed with abnormal LHBT on preoperative MRI and 136 (73%) cases with normal LHBT findings. Conversely, the 184 shoulders included 72 (40%) cases with abnormal LHBT findings on preoperative SUS and 112 (60%) cases with normal LHBT findings. The remaining 181 shoulders (49%) were diagnosed with SSC tendon tears on diagnostic arthroscopy. Of these, 109 and 140 cases had abnormal LHBT findings on MRI and SUS, respectively. In contrast, 72 and 41 cases had normal LHBT findings on MRI and SUS, respectively.
On multivariate analysis, the preoperative SUS findings showed a significant difference regarding the presence or absence of intraoperative SSC rupture (odds ratio 1.73, p < 0.001), while the MRI findings showed no significant difference (odds ratio: 1.34) (Table 6).
Discussion
The LHBT starts from the upper part of the glenohumeral joint and the labrum, passes through the inter-nodal groove from the rotator interval (RI) in the shoulder joint, and is extra-articular [4]. The LHBT is thought to act as an upper braking mechanism for the head of the humerus. In the RI, the biceps reflection pulley is formed by the joint capsule, coracohumeral ligament (CHL), superior glenohumeral ligament (SGHL), supraspinatus tendon (SSP), and subscapularis tendon (SSC). The pulley provides a stabilizing mechanism for the LHBT [1], and damage to its constituents causes anterior shoulder joint pain by inducing LHBT instability and inflammation. It is considered that LHBT function can predict instability of the LHBT. The LHBT is thought to be involved in the pain associated with rotator cuff tears. The stabilization mechanism of the LHBT brachii involves not only the bony element of the inter-nodal groove, but also the upper end of the inner wall of the inter-nodal groove. It is composed of the nodular top of the subscapular muscle and the inner bundle of the brachial ligament. The tendon-like tissue supports the LHBT from the inter-nodal groove to the supraclavicular nodule of the scapula from the inferior medial side and acts as a pulley to change the direction [1].
However, since the LHBT in the shoulder joint has a large three-dimensional phase change, it is difficult to detect lesions with MRI because of the partial volume effect. We also cannot depict intra-shoulder lesions with SUS. However, SUS can depict soft tissues in the internal groove.
Shoulder dysfunction is a common complication of the musculoskeletal system in the elderly. This is often due to rotator cuff tears and osteoarthritis of the shoulder. Asymptomatic rotator cuff tears are common in the elderly.
We conducted a retrospective study on the assumption that SSC damage due to damage to the stabilization mechanism can be predicted by observing LHBT malposition associated with painful rotator cuff tears and LHBT function.
For successful treatment of rotator cuff tears, examination of the presence of LHBT lesions and the pathological condition is crucial. LHBT lesions can have various etiologies, such as trauma, sports injuries, and chronic diseases. However, LHBT lesions associated with rotator cuff tears are most likely caused by degeneration, chronic minor trauma, and impingement, rather than acute trauma [5].
Although MRI is the gold standard for diagnosing rotator cuff tears [3], LHBT lesions may often be missed, and preoperative and intraoperative findings may differ [3, 5,6,7]. Morgan et al. reported difficulty in analyzing malposition of the LHBT in the bicipital groove using MRI and computed tomography [6]. Unlike MRI, SUS has no risk of radiation exposure, and dynamic motion can be easily observed. Therefore, SUS is considered to be an excellent method for delineating subluxation/dislocation of the LHBT, which may change depending on the position of the shoulder joint.
Our results showed relatively high sensitivity (92%), specificity (90%), and accuracy (91%) in detecting abnormal LHBT on preoperative SUS, which were higher than those of preoperative MRI (sensitivity 74%, specificity 84%, accuracy 80%). Hence, it can be inferred that preoperative LHBT malposition can be better detected with SUS than MRI.
A significant difference was observed in SUS and MRI findings of the LHBT (p < 0.001). According to the findings, hypertrophy/edema was more commonly diagnosed with SUS (n = 86, 41%) than with MRI (n = 30, 19%). This is because the average age of patients included in this study was 65 years old, and they had painful rotator cuff tears that may be attributed to degenerative changes due to aging.
The association of SSC rupture and subluxation/dislocation of the LHBT is well established [8, 9]. Regarding open shoulder surgery in previous reports, SSC ruptures were considered to be a relatively rare rupture, accounting for only 10.5–21% of all rotator cuff tears. In recent years, advances in arthroscopic surgery have made it possible to observe the pathology in detail, and it has been reported that the frequency of SSC rupture is 19–49.4% [8,9,10,11,12,13,14,15,16]. In our study, SSC rupture was observed in 49% of rotator cuff injuries.
SSC rupture most often occurs on the articular surface and primarily involves the superior portion; hence, the caudal portion is not often damaged with its rupture [17]. Retraction of the tendon is consequently minimal [17]. Moreover, scar tissue subsequently develops over the ruptured area, thereby covering it. As a consequence, the tendon appears intact upon visualization on MRI [18, 19]. Furthermore, the diagnostic ability of MRI for SSC rupture is inferior to that for supraspinatus tendon rupture [15, 18,19,20]. Narasimhan et al. reported that direct visualization of the articular surface in SSC rupture is difficult even on SUS (sensitivity 39%) [21].
We considered the SSC to be involved in stabilizing LHBT motion. The SSC plays a role as a pulley to suppress the dislocation of the LHBT; therefore, incomplete rupture or damage of the SSC can lead to dislocation [22]. In this study, in the presence of SSC tears, the LHBT showed subluxation in 62 cases (45%). In contrast, a study reported that even in the presence of a subscapularis muscle injury, 10% of cases did not present pulley lesions [23]. We inferred that SSC rupture can be predicted when subluxation of the LHBT is observed because the SSC together with the CHL and SGHL reportedly forms a pulley to suppress LHBT dislocation. In our study, we found that the LHBT condition on SUS remained intact in 41 patients (23%) in the presence of SSC tears. Therefore, subscapularis rupture is not necessarily a subluxation of the LHBT. However, the subscapularis muscle together with the CHL and SGHL reportedly forms a pulley that suppresses dislocation of the LHBT [24]. Hence, SSC rupture can be inferred if LHBT malposition occurs upon dynamic observation under SUS.
The preoperative detection of LHBT abnormalities associated with SSC tears was analyzed and was considered to be significant in the case of SUS; hence, LHBT findings of SUS may have strong clinical implications in indicating the presence of SSC rupture [22, 25]. Further, extra-articular pathology is difficult to diagnose with preoperative MRI, and this may be altered using SUS preoperatively for diagnosis. More studies are required to clarify the association between preoperative LHBT lesions associated with rotator cuff tears and postoperative changes in the LHBT.
This study had some limitations. In cases of shoulder contracture, SUS is not suitable for anterior observation near the bicipital groove and dynamic observation by external rotation. In cases of shoulder osteoarthritis, the rotator cuff is visualized with difficulty as the head of the humerus head is significantly deformed. When a significant amount of muscle is infiltrated with fat, the ultrasonic beam is scattered, thus limiting the clinical utility of SUS assessment. As a consequence, SUS findings may become incompatible with preoperative findings.
Conclusion
Patients who underwent arthroscopic rotator cuff repair were preoperatively assessed with MRI and SUS. In diagnosing LHBT malposition, SUS was superior to MRI in terms of sensitivity, specificity, and accuracy. Further, SSC rupture and abnormal LHBT findings on SUS showed a significant correlation, suggesting that SUS can strongly predict SSC rupture preoperatively.
Change history
15 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10396-022-01212-8
References
Boileau P, Ahrens PM, Hatzidakis AM. Entrapment of the long head of the biceps tendon: the hourglass biceps—a cause of pain and locking of the shoulder. J Shoulder Elbow Surg. 2004;13:249–57.
Arai R, Mochizuki T, Yamaguchi K, et al. Functional anatomy of the superior glenohumeral and coracohumeral ligaments and the subscapularis tendon in view of stabilization of the long head of the biceps tendon. J Shoulder Elbow Surg. 2010;19:58–64.
Rol M, Favard L, Berhouet J. Diagnosis of long head of biceps tendinopathy in rotator cuff tear patients: correlation of imaging and arthroscopy data. Int Orthop. 2018;42:1347–55.
Nakata W, Katou S, Fujita A, et al. Biceps pulley: normal anatomy and associated lesions at MR arthrography. Radiographics. 2011;31:791–810.
Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9:382–5.
Morag Y, Jacobson JA, Miller B, et al. MR imaging of rotator cuff injury: what the clinician needs to know. Radiographics. 2006;26:1045–65.
Taylor SA, Newman AM, Nguyen J, et al. Magnetic resonance imaging currently fails to fully evaluate the biceps-labrum complex and bicipital tunnel. Arthroscopy. 2016;32:238–44.
Kowalczuk M, Kohut K, Sabzevari S, et al. Proximal long head biceps rupture: a predictor of rotator cuff pathology. Arthroscopy. 2018;34:1166–70.
Hanusch BC, Makaram N, Utrillas-Compaired A, et al. Biceps sheath fluid on shoulder ultrasound as a predictor of rotator cuff tear: analysis of a consecutive cohort. J Shoulder Elbow Surg. 2016;25:1661–7.
Shi LL, Mullen MG, Freehill MT, et al. Accuracy of long head of the biceps subluxation as a predictor for subscapularis tears. Arthroscopy. 2015;31:615–9.
Deutsch A, Altchek DW, Veltri DM, et al. Traumatic tears of the subscapularis tendon. Clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med. 1997;25:13–22.
Flury MP, John M, Goldhahn J, et al. Rupture of the subscapularis tendon (isolated or in combination with supraspinatus tear): when is a repair indicated? J Shoulder Elbow Surg. 2006;15:659–64.
Kreuz PC, Remiger A, Erggelet C, et al. Isolated and combined tears of the subscapularis tendon. Am J Sports Med. 2005;33:1831–7.
Kim TK, Rauh PB, McFarland EG. Partial tears of the subscapularis tendon found during arthroscopic procedures on the shoulder: a statistical analysis of sixty cases. Am J Sports Med. 2003;31:744–50.
Garavaglia G, Ufenast H, Taverna E. The frequency of subscapularis tears in arthroscopic rotator cuff repairs: a retrospective study comparing magnetic resonance imaging and arthroscopic findings. Int J Shoulder Surg. 2011;5:90–4.
Lafosse L, Jost B, Reiland Y, et al. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89:1184–93.
Adams CR, Schoolfield JD, Burkhart SS. Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy. 2010;26:1427–33.
Pfirrmann CW, Zanetti M, Weishaupt D, et al. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology. 1999;213:709–14.
Tung GA, Yoo DC, Levine SM, et al. Subscapularis tendon tear: primary and associated signs on MRI. J Comput Assist Tomogr. 2001;25:417–24.
Foad A, Wijdicks CA. The accuracy of magnetic resonance imaging and magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy. 2012;28:636–41.
Narasimhan R, Shamse K, Nash C, et al. Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop. 2016;40:975–9.
Sakurai G, Ozaki J, Tomita Y, et al. Incomplete tears of the subscapularis tendon associated with tears of the supraspinatus tendon: cadaveric and clinical studies. J Shoulder Elbow Surg. 1998;7:510–5.
Godenèche A, Nové-Josserand L, Audebert S, et al. Relationship between subscapularis tears and injuries to the biceps pulley. Knee Surg Sports Traumatol Arthrosc. 2017;25:2114–20.
Bennett WF. Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of “hidden” rotator interval lesions. Arthroscopy. 2001;17:173–80.
Toshiaki A, Itoi E, Minagawa H, et al. Cross-sectional area of the tendon and the muscle of the biceps brachii in shoulders with rotator cuff tears: a study of 14 cadaveric shoulders. Acta Orthop. 2005;76:509–12.
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yoshiko Fujiwara, Syuichi Yamamoto, Yumi Kato, Shimpei Kurata, Shuhei Fujii, Kazuya Inoue, Takashi Inoue, Takamitsu Mondori, Yoshiyuki Nakagawa, and Yasuhito Tanaka declare that they have no conflicts of interest.
Ethical statement
All procedures were in accordance with the ethical standards imposed by the Uda City Hospital Ethics Committee (R3UHRNo005), as well as the principles of the Declaration of Helsinki (1964) and its later amendments.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The Publisher regrets the following error in figure 1 where the label of the figure was published incorrectly. The correct figure is given in this correction.
About this article
Cite this article
Fujiwara, Y., Yamamoto, S., Kato, Y. et al. Usefulness of ultrasound in diagnosing long head of the biceps tendon malposition in patients with rotator cuff tears. J Med Ultrasonics 49, 289–295 (2022). https://doi.org/10.1007/s10396-022-01200-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-022-01200-y