Abstract
The accuracy of attenuation coefficients and B-mode ultrasound for distinguishing between S0 (healthy, < 5% fat) and S1–3 (steatosis ≥ 5%) livers compared to a controlled attenuation parameter is unclear. This meta-analysis aimed to comprehensively assess the diagnostic performance of B-mode ultrasound imaging for evaluating steatosis of ≥ 5%. We searched the PubMed, Embase, and Web of Science databases for studies on the accuracy of B-mode ultrasound for differentiating S0 from S1–3 in adults with chronic liver disease. A bivariate random-effects model was performed to estimate the pooled sensitivity, specificity, positive (PLR) and negative likelihood ratios (NLR), and diagnostic odds ratios (DORs). Subgroup analyses by attenuation coefficient, conventional B-mode ultrasound findings, and B-mode ultrasound findings without semi-quantification methods were performed. Liver steatosis was scored as follows: S0, < 5%; S1, 5–33%; S2, 33–66%; and S3, > 66%. Nineteen studies involving 3240 patients were analyzed. The pooled sensitivity and specificity of B-mode ultrasound for detecting S1 were 0.70 (95% confidence interval [CI], 0.63–0.77) and 0.86 (95% CI 0.82–0.89), respectively. The pooled PLR, NLR, and DOR were 4.90 (95% CI 3.69–6.51), 0.35 (95% CI 0.27– 0.44), and 14.1 (95% CI 8.7–23.0), respectively. The diagnostic accuracy was better in patients with attenuation coefficients (area under the curve [AUC], 0.89; sensitivity, 0.75; specificity, 0.86) than in those with conventional B-mode findings (AUC, 0.80; sensitivity, 0.59; specificity, 0.83). In particular, the diagnostic value was better when the attenuation coefficient guided by B-mode ultrasound was utilized. To screen patients with steatosis of ≥ 5%, attenuation coefficient should be used.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatic steatosis is characterized by the accumulation of triacylglycerol-rich macrovesicular and/or microvesicular lipid droplets within the hepatocytes [1, 2]. Hepatic steatosis or fatty liver is defined as intrahepatic triacylglycerol of at least 5% of liver weight or 5% of hepatocytes containing lipid vacuoles [3, 4]. Non-alcoholic fatty liver disease (NAFLD) is becoming increasingly prevalent along with obesity and type 2 diabetes mellitus, and it is now the most common cause of chronic liver disease worldwide. The symptoms of NAFLD vary widely, from simple steatosis to non-alcoholic steatohepatitis [5, 6]. Untreated NAFLD may progress to more damaging conditions, including cirrhosis, hepatocellular carcinoma, and liver failure [7,8,9,10]. Controlled attenuation parameter (CAP), measured via transient elastography, has recently been endorsed as a noninvasive method for the detection and quantification of steatosis [11]. CAP has excellent diagnostic accuracy for diagnosing hepatic steatosis in patients with chronic liver disease [12,13,14]. Meanwhile, conventional abdominal B-mode ultrasound has been widely used to diagnose fatty liver (bright liver, hepato-renal contrast, deep attenuation, or vessel blurring). B-mode ultrasound has been shown to have an acceptable diagnostic accuracy of > 15–20% for detecting hepatic steatosis [15, 16]. However, its usefulness in identifying steatosis of ≥ 5% remains unclear.
A quantification method using attenuation coefficients has recently been utilized in B-mode ultrasound [17, 18]. Given that these B-mode imaging-guided attenuation coefficient methods are relatively new, only a few validation studies have been conducted. Thus, the diagnostic capability of B-mode ultrasound for detecting steatosis of ≥ 5% is controversial. There has been no evidence of accurately diagnosing steatosis of ≥ 5% using B-mode ultrasound. This meta-analysis aimed to comprehensively assess the diagnostic performance of B-mode ultrasound imaging for evaluating steatosis of ≥ 5%.
Materials and methods
Ethics
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses of Diagnostic Test Accuracy Studies (PRISMA-DTA) [19]. The review was registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42021255110).
Literature search
Studies on the diagnostic characteristics of B-mode ultrasound for quantifying liver steatosis with histology as the reference standard were extracted from the PubMed, Embase, and Web of Science databases until May 15, 2021. Only English-language manuscripts published or accepted by a peer-reviewed journal between January 2000 and May 2021 were included in the meta-analysis. Study results published only in abstract form were not considered. The final query for PubMed was: “(fatty liver) AND ((ultrasound) AND (attenuation)) NOT (Children)) NOT (review)) AND ((biopsy)” [All Fields] AND 2000/1/1:2021/5/15[Date–Entry]. An analogous query was used for Web of Science.
Selection criteria
Eligible studies were identified according to the following criteria: (1) the diagnostic accuracy for steatosis (≥ 5%) in adults with chronic liver disease; (2) liver biopsy was performed; (3) sufficient data were provided to calculate the true positive (TP), false-positive (FP), false-negative (FN), and true-negative (TN) rates of ultrasound findings for hepatic steatosis of ≥ 5%; and (4) at least 50 patients were evaluated to obtain good reliability. Only articles available in full text and written in English were included. Duplicate publication, animal studies, and ex vivo studies were excluded.
Data extraction and quality assessment
Two reviewers independently extracted the data and evaluated the quality of the included studies, with disagreements resolved by consensus. The following data were retrieved: first author, publication year, location, study design, technique of ultrasound, the number of patients, age, sex, body mass index (BMI), and the duration between ultrasound and liver biopsy. TP, FP, FN, and TN were directly extracted or calculated. The quality of the studies was assessed by two reviewers according to the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool [20].
Statistical analysis
The diagnostic accuracy of B-mode ultrasound attenuation was evaluated according to the summary sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), positive predictive value (PPV), negative predictive value (NPV), and diagnostic odds ratio (DOR) with corresponding 95% confidence intervals (CI) calculated using the bivariate random-effects model. Then, the hierarchical summary receiver-operating characteristic (HSROC) curve and the area under the curve (AUC) were calculated. Heterogeneity was evaluated using the Cochrane Q-test and the Higgins inconsistency index (I2), with p < 0.05 or I2 > 50% considered to indicate substantial heterogeneity [21, 22].
Sensitivity analysis was restricted to patients with chronic viral liver disease. Univariate meta-regression analysis and subgroup analysis were also performed to explore possible sources of heterogeneity. The covariates included the following: (1) measurement technique (attenuation coefficient vs. conventional B-mode findings), (2) number of patients (≥ 150 vs. < 150), (3) BMI (≥ 26 vs. < 26 kg/m2), (4) publication date (2000–2009 vs. 2010–2021), and (5) the duration between liver biopsy and ultrasound (≥ 30 vs. < 30 days). The findings of steatosis observed using conventional B-mode ultrasound were defined as follows: bright liver [23], hepato-renal contrast [23], deep attenuation [23], or vascular blurring [23]. Fagan plots were used to assess the clinical utility of ultrasound findings for diagnosing hepatic steatosis. Publication bias was assessed using Deeks’ funnel plot, with a p value of < 0.1 for the slope coefficient suggesting significant asymmetry. All statistical analyses were performed using the “midas” and “metandi” modules of Stata version 15.0 (Stata Corp, College Station, TX, USA).
Results
Search results and study characteristics
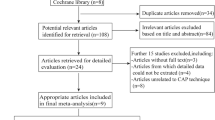
A total of 304 articles were initially analyzed. After removing 40 duplicates and 264 irrelevant studies, 43 studies were further evaluated. Of these, 24 studies were excluded after a full-text review, because they were of undesirable article type, were not diagnostic accuracy studies, were not relevant to chronic liver disease, included a small sample size (< 50 participants), had insufficient data (TP, FP, TN, and FN not reported or could not be calculated), and not written in the English language. Ultimately, 19 articles involving 3240 patients were analyzed [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. The study selection flowchart is presented in Fig. 1. The detailed characteristics of the 19 studies are summarized in Table 1.
The 19 original articles included eight prospective studies, ten retrospective studies, and one cross-sectional study. The quality assessment results are presented in Fig. 2. Risk-of-bias analysis showed that four studies were high risk for flow and timing because of the long duration between ultrasound and liver biopsy. Most studies were identified as low risk for bias and applicability concerns, with all of the studies satisfying four or more of the seven total domains. Deeks’ plot showed that there was no potential publication bias (p = 0.68 for all patients, p = 0.24 for the patients with attenuation coefficients, and p = 0.97 for the patients with conventional B-mode ultrasound) (Fig. 3).
Diagnostic accuracy of B-mode ultrasound for the detection of mild steatosis
In all patients, the pooled sensitivity and specificity of B-mode ultrasound for detecting S1 were 0.70 (95% CI 0.63–0.77) and 0.86 (95% CI 0.82–0.89), respectively (Table 2). The pooled PLR, NLR, and DOR were 4.90 (95% CI 3.69–6.51), 0.35 (95% CI 0.27– 0.44), and 14.1 (95% CI 8.7–23.0), respectively. Figure 4a shows the HSROC curve, with an AUC of 0.87 (95% CI 0.82–0.91).
Meanwhile, the diagnostic accuracies according to the attenuation coefficient and conventional B-mode findings were as follows. The attenuation coefficient group showed better diagnostic accuracy (sensitivity, specificity, PPV, NPV, PLR, NLR, DOR, and AUC) than the conventional B-mode findings group (Table 2; Fig. 4b, c). In the conventional B-mode ultrasound group, semi-quantification methods were performed to diagnose the steatosis grade in three studies [36, 37, 40]. By quantifying the level of echogenicity, the hepato-renal contrast index was calculated. Thus, we analyzed the impact of the exclusion of semi-quantification methods on the diagnostic value of conventional B-mode ultrasound. Conventional B-mode findings that included only non-quantification methods had low diagnostic value (Table 2, Fig. 4d). The forest plots are presented in Figs. 5 and 6.
No heterogeneity was found in the attenuation coefficient group (Fig. 5). The pooled sensitivity and specificity of attenuation coefficients for detecting mild steatosis were 0.75 (95% CI 0.70–0.79) and 0.86 (95% CI 0.82–0.90), respectively (Fig. 5). The pooled sensitivity and specificity of conventional B-mode ultrasound for detecting mild steatosis were 0.69 (95% CI 0.57–0.79) and 0.85 (95% CI 0.79–0.89). There were heterogeneities in both sensitivity and specificity in the conventional B-mode ultrasound group (Fig. 6).
Clinical utility of B-mode ultrasound for hepatic steatosis in suspected fatty liver patients
Among patients with suspected hepatic steatosis, the PLR and NLR in those with S1 steatosis were 4.90 and 0.35, respectively (Fagan plot analysis). In this subset of patients with a 25% pre-test probability (based on clinical suspicion), a positive B-mode finding achieved a 62% probability of correct diagnosis, and a negative B-mode value achieved a 10% probability of incorrect diagnosis. When the pre-test probability (based on clinical suspicion) was set to 50%, a positive B-mode finding yielded an 83% probability of correct diagnosis, and a negative B-mode result yielded a 26% probability of incorrect diagnosis. When the pre-test probability (based on clinical suspicion) was set to 75%, a positive B-mode value showed a 94% probability of correct diagnosis, and a negative B-mode value showed a 51% probability of incorrect diagnosis.
In patients with suspected hepatic steatosis based on attenuation coefficients, the PLR and NLR in those with S1 steatosis were 5.66 and 0.28, respectively (Fagan plot). In this subset of patients with a 25% pre-test probability (based on clinical suspicion), a positive B-mode finding had a 64% probability of correct diagnosis, and a negative B-mode value revealed a 9% probability of incorrect diagnosis. When the pre-test probability (based on clinical suspicion) was set to 50%, a positive B-mode finding yielded an 84% probability of correct diagnosis, and a negative B-mode result yielded a 23% probability of incorrect diagnosis. When the pre-test probability (based on clinical suspicion) was set to 75%, a positive B-mode value showed a 94% probability of correct diagnosis, and a negative B-mode value showed a 47% probability of incorrect diagnosis.
In patients suspected of having hepatic steatosis based on B-mode ultrasound findings, the PLR and NLR among those with S1 steatosis were 4.48 and 0.37, respectively (Fagan plot). In this subset of patients with 25% pre-test probability (based on clinical suspicion), a positive B-mode finding revealed a 62% probability of correct diagnosis, and a negative B-mode value revealed a 11% probability of incorrect diagnosis. When the pre-test probability (based on clinical suspicion) was set to 50%, a positive B-mode finding yielded an 83% probability of correct diagnosis, and a negative B-mode finding yielded a 26% probability of incorrect diagnosis. When the pre-test probability (based on clinical suspicion) was set to 75%, a positive B-mode value showed a 94% probability of correct diagnosis, and a negative B-mode value showed a 52% probability of incorrect diagnosis.
Results of meta-regression and subgroup analysis
Univariate meta-regression showed that the sample size, method of ultrasound, BMI, publish year, and duration between liver biopsy and ultrasound were associated with the heterogeneity. B-mode ultrasound showed better performance in the diagnosis of a large sample size, attenuation coefficient, BMI > 25 kg/m2, recently reported paper, and short time between biopsy and ultrasound. The details of the subgroup analysis are presented in Table 3.
Discussion
The accuracy of attenuation coefficients and B-mode ultrasound for diagnosing hepatic steatosis is yet to be fully elucidated. The results of this meta-analysis indicate that B-mode ultrasound performed using current techniques has a good accuracy for detecting 5% steatosis (S1), with the AUC reaching 87%. In particular, when attenuation coefficients are utilized, the AUC for the diagnosis of S1 reached 89%, while the AUC was 0.80 for conventional B-mode ultrasound.
Hepatic steatosis is defined as intrahepatic fat of at least 5% of hepatocytes. The degree of steatosis in liver biopsies is usually assessed through a morphological semiquantitative approach in which the histopathologist uses a four-grade scale. However, Franzen et al. reported that semiquantitative evaluation overestimates the degree of steatosis in liver biopsies, with 5% of hepatocytes corresponding to only a small percentage of the total area. This meta-analysis primarily investigated whether a small percentage of fat area in tissue specimens could be diagnosed using current ultrasound imaging methods. CAP, which is based on the properties of ultrasonic signals acquired using transient elastography, is currently widely used to diagnose hepatic steatosis [11]. Some meta-analysis studies have reported that CAP is a promising noninvasive test for diagnosing mild hepatic steatosis [14, 43]. Petroff et al. recently reported the diagnostic accuracy of CAP in 2346 patients with mild steatosis [14]. CAP was found to be a reliable method to distinguish S0 from S1–3 in patients with NAFLD, with an AUC of 0.807, sensitivity of 0.790, and specificity of 0.740.
Apart from CAP, B-mode ultrasound findings and attenuation parameters have also been used to diagnose hepatic steatosis. A meta-analysis by Hernaez et al. [44] showed that B-mode findings allowed for reliable and accurate detection of moderate-to-severe steatosis (S2 and S3). B-mode ultrasound images can be improved. For example, new ultrasound machines have lower signal attenuation and generate clearer intrahepatic echo images. However, the diagnostic accuracy of B-mode ultrasound for mild steatosis (S1) has not been established. Although there have been studies on its diagnostic capability for mild steatosis [34,35,36, 39], to our knowledge, no meta-analysis has been performed to analyze attenuation coefficients guided by B-mode ultrasound. Previous studies also had a small sample size [24,25,26,27,28,29,30, 38].
In this study, the AUC in the total population was higher than that in previous CAP reports [14]. Despite using the same principle, attenuation coefficients guided by B-mode ultrasound had an even better AUC than CAP. The attenuation coefficients guided by B-mode can be measured while checking the B-mode image. Given that measurement by TE is based on M- and A-mode imaging, it is influenced by the respiratory status, size of the liver, and experience of the operator. It has already been reported that the accuracy of stiffness measurement is higher when B-mode is utilized [45]. The same applies to the attenuation coefficients guided by B-mode ultrasound.
Previous studies have shown an NAFLD prevalence rate of approximately 25% [23, 46, 47]. In this study, post-test probabilities were calculated using the Fagan plot. When the pre-test probability was set to 25%, B-mode findings showed high accuracy for ruling out fatty liver. This indicates the importance of paying attention to patients with a low level of attenuation coefficients or without conventional B-mode findings. Meanwhile, if obese patients are evaluated, positive findings are crucial as most of them have fatty liver. Patients with positive B-mode findings can be considered to have fatty liver. Interestingly, regarding the diagnosis of mild steatosis, B-mode findings had diagnostic accuracy inferior to that of attenuation coefficients. However, the post-test probability of B-mode was not inferior to that of attenuation coefficients. This may be the rationale for the recent improvements in ultrasound machines, and these improvements may indicate that the conventional B-mode ultrasound may also be useful in obese patients.
Meanwhile, HSROC analysis showed a wide variability in B-mode ultrasound. Forest plots indicated heterogeneity for both sensitivity and specificity in the conventional B-mode ultrasound. In subgroup analysis, a large sample size, attenuation coefficients, BMI < 25 kg/m2, recent publication year (from 2010), and duration between biopsy and ultrasound were better for diagnostic accuracy when mild steatosis was diagnosed. Although funnel plots showed no publication bias, clinical studies have to include a large sample size. Enrolling patients with BMI < 25 kg/m2 may lower the proportion of those with fatty liver. Moreover, when older studies were analyzed, B-mode ultrasound had insufficient diagnostic performance. Attenuation coefficients had better diagnostic value than conventional B-mode ultrasound with non-quantification methods. Conventional B-mode ultrasound had lower pooled sensitivity, indicating that it has insufficient diagnostic capability for ruling out S0. Thus, attenuation coefficients should be used to distinguish S0 from S1–3, with this method being reliable.
This study had some limitations. First, there have been only a few reported studies on attenuation coefficients guided by B-mode ultrasound to date. More high-quality studies are needed to establish the diagnostic value of attenuation coefficients. Second, there were few recent studies that analyzed conventional B-mode. We will perform another meta-analysis when more studies become available. Third, a few clinical trials have compared attenuation coefficients with other tests (CAP or magnetic resonance imaging). Comparative studies are needed to establish the accuracy and usefulness of attenuation coefficients. Fourth, the diagnostic ability of attenuation coefficients was not evaluated between different ultrasound devices as data from only a limited number of participants were included and, therefore, they were insufficient to perform this sub-analysis. When more papers are published in the future, we would like to re-analyze this aspect.
Conclusion
Conventional B-mode ultrasound has sufficient diagnostic capability for steatosis ≥ 5%. In particular, attenuation coefficients guided by B-mode ultrasound are reliable and reproducible.
References
Cohen JC, Horton JD, Hobbs HH. Human fatty liver disease: old questions and new insights. Science. 2011;332:1519–23.
You M, Arteel GE. Effect of ethanol on lipid metabolism. J Hepatol. 2019;70:237–48.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Bedossa P. Pathology of non-alcoholic fatty liver disease. Liver Int. 2017;37:85–9.
Brunt EM, Kleiner DE, Wilson LA, et al. Neuschwander-Tetri BA, NASH Clinical Research Network. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology. 2011;53:810–20.
Adams LA, Lymp JF, St Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–21.
Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31.
Kumar R, Priyadarshi RN, Anand U. Non-alcoholic fatty liver disease: growing burden, adverse outcomes and associations. J Clin Transl Hepatol. 2020;8:76–86.
Mantovani A, Scorletti E, Mosca A, et al. Complications, morbidity and mortality of nonalcoholic fatty liver disease. Metabolism. 2020;111S:154170.
Haflidadottir S, Jonasson JG, Norland H, et al. Long-term follow-up and liver-related death rate in patients with non-alcoholic and alcoholic related fatty liver disease. BMC Gastroenterol. 2014;14:166.
Sasso M, Beaugrand M, de Ledinghen V, et al. Controlled attenuation parameter (CAP): a novel VCTE™ guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36:1825–35.
Imajo K, Kessoku T, Honda Y, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology. 2016;150:626–37.
Eddowes PJ, Sasso M, Allison M, et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1717–30.
Petroff D, Blank V, Newsome PN, et al. Assessment of hepatic steatosis by controlled attenuation parameter using the M and XL probes: an individual patient data meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:185–98.
Lupsor M, Badea R. Imaging diagnosis and quantification of hepatic steatosis: is it an accepted alternative to needle biopsy? Rom J Gastroenterol. 2005;14:419–25.
Bintintan A, Chira RI, Bintintan VV, et al. Value of hepatic elastography and Doppler indexes for predictions of esophageal varices in liver cirrhosis. Med Ultrason. 2015;17:5–11.
Tamaki N, Koizumi Y, Hirooka M, et al. Novel quantitative assessment system of liver steatosis using a newly developed attenuation measurement method. Hepatol Res. 2018;48:821–8.
Fujiwara Y, Kuroda H, Abe T, et al. The B-mode image-guided ultrasound attenuation parameter accurately detects hepatic steatosis in chronic liver disease. Ultrasound Med Biol. 2018;44:2223–32.
McInnes MDF, Moher D, Thombs BD, et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319:388–96.
Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Guyatt GH, Oxman AD, Kunz R, et al. Rating the quality of evidence—inconsistency. J Clin Epidemiol. 2011;64:1294–302.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Hamaguchi M, Takeda N, Kojima T, et al. Identification of individuals with non-alcoholic fatty liver disease by the diagnostic criteria for the metabolic syndrome. World J Gastroenterol. 2012;18:1508–16.
Kuroda H, Fujiwara Y, Abe T, et al. Two-dimensional shear wave elastography and ultrasound-guided attenuation parameter for progressive non-alcoholic steatohepatitis. PLoS ONE. 2021;16:e0249493.
Sugimoto K, Moriyasu F, Oshiro H, et al. The role of multiparametric US of the liver for the evaluation of nonalcoholic steatohepatitis. Radiology. 2020;296:532–40.
Lee DH, Cho EJ, Bae JS, et al. Accuracy of two-dimensional shear wave elastography and attenuation imaging for evaluation of patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2021;19:797–805.
Dioguardi Burgio M, Ronot M, Reizine E, et al. Quantification of hepatic steatosis with ultrasound: promising role of attenuation imaging coefficient in a biopsy-proven cohort. Eur Radiol. 2020;30:2293–301.
Bae JS, Lee DH, Lee JY, et al. Assessment of hepatic steatosis by using attenuation imaging: a quantitative, easy-to-perform ultrasound technique. Eur Radiol. 2019;29:6499–507.
Tada T, Iijima H, Kobayashi N, et al. Usefulness of attenuation imaging with an ultrasound scanner for the evaluation of hepatic steatosis. Ultrasound Med Biol. 2019;45:2679–87.
Koizumi Y, Hirooka M, Tamaki N, et al. New diagnostic technique to evaluate hepatic steatosis using the attenuation coefficient on ultrasound B mode. PLoS ONE. 2019;14:e0221548.
Soresi M, Giannitrapani L, Florena AM, et al. Reliability of the bright liver echo pattern in diagnosing steatosis in patients with cryptogenic and HCV-related hypertransaminasaemia. Clin Radiol. 2009;64:1181–7.
de Moura AA, Cotrim HP, Barbosa DB, et al. Fatty liver disease in severe obese patients: diagnostic value of abdominal ultrasound. World J Gastroenterol. 2008;14:1415–8.
Perez NE, Siddiqui FA, Mutchnick MG, et al. Ultrasound diagnosis of fatty liver in patients with chronic liver disease: a retrospective observational study. J Clin Gastroenterol. 2007;41:624–9.
Ballestri S, Nascimbeni F, Baldelli E, et al. Ultrasonographic fatty liver indicator detects mild steatosis and correlates with metabolic/histological parameters in various liver diseases. Metabolism. 2017;72:57–65.
Kelly EM, Feldstein VA, Etheridge D, et al. Sonography predicts liver steatosis in patients with chronic hepatitis B. J Ultrasound Med. 2017;36:925–32.
Zelber-Sagi S, Webb M, Assy N, et al. Comparison of fatty liver index with noninvasive methods for steatosis detection and quantification. World J Gastroenterol. 2013;19:57–64.
Webb M, Yeshua H, Zelber-Sagi S, et al. Diagnostic value of a computerized hepatorenal index for sonographic quantification of liver steatosis. Am J Roentgenol. 2009;192:909–14.
Petzold G, Lasser J, Rühl J, et al. Diagnostic accuracy of B-Mode ultrasound and hepatorenal Index for graduation of hepatic steatosis in patients with chronic liver disease. PLoS ONE. 2020;15:e0231044.
Lee SS, Park SH, Kim HJ, et al. Non-invasive assessment of hepatic steatosis: prospective comparison of the accuracy of imaging examinations. J Hepatol. 2010;52:579–85.
Lee JY, Kim KM, Lee SG, et al. Prevalence and risk factors of non-alcoholic fatty liver disease in potential living liver donors in Korea: a review of 589 consecutive liver biopsies in a single center. J Hepatol. 2007;47:239–44.
Crum-Cianflone N, Dilay A, Collins G, et al. Nonalcoholic fatty liver disease among HIV-infected persons. J Acquir Immune Defic Syndr. 2009;50:464–73.
Chen CH, Lin ST, Yang CC, et al. The accuracy of sonography in predicting steatosis and fibrosis in chronic hepatitis C. Dig Dis Sci. 2008;53:1699–706.
Pu K, Wang Y, Bai S, et al. Diagnostic accuracy of controlled attenuation parameter (CAP) as a non-invasive test for steatosis in suspected non-alcoholic fatty liver disease: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19:51.
Hernaez R, Lazo M, Bonekamp S, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54:1082–90.
Tanaka T, Hirooka M, Koizumi Y, et al. Development of a method for measuring spleen stiffness by transient elastography using a new device and ultrasound-fusion method. PLoS ONE. 2021;16:e0246315.
Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
Eguchi Y, Hyogo H, Ono M, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol. 2012;47:586–95.
Funding
This work was supported in part by the Japan Society for the Promotion of Science KAKENHI (Grant Number 21K07701 to M.H., and Grant Number 21K08008 to Y.H.).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MH, YK, KS, and YN. The first draft of the manuscript was written by MH, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Masashi Hirooka, Yohei Koizumi, Kotaro Sunago, Atsushi Yukimoto, Yoshiko Nakamura, Kana Hirooka, Takao Watanabe, Osamu Yoshida, Yoshio Tokumoto, Masanori Abe, and Yoichi Hiasa declare no conflicts of interest.
Ethical statement
An ethical statement is not required as it a review article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hirooka, M., Koizumi, Y., Sunago, K. et al. Efficacy of B-mode ultrasound-based attenuation for the diagnosis of hepatic steatosis: a systematic review/meta-analysis. J Med Ultrasonics 49, 199–210 (2022). https://doi.org/10.1007/s10396-022-01196-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-022-01196-5