Abstract
Purpose
Our objective in this study was to assess the changes in medial gastrocnemius muscle (GCM) stiffness after botulinum toxin A (BTA) injection in children with cerebral palsy (CP) by using acoustic radiation force impulse (ARFI) elastography and to research the usability of this technique in clinical practice.
Materials and methods
Twenty-four spastic lower extremities of 12 children with CP were assessed. BTA injection treatment was applied to the medial GCM. Muscle stiffness was measured with the ARFI technique before the procedure and a month after the procedure. The patients were assessed with the modified Ashworth scale (MAS) in the physiotherapy department at about the same time. Shear wave velocity (SWV) values and MAS scores before and after the treatment were compared.
Results
Mean SWV values were measured as 3.20 ± 0.14 m/s before BTA and as 2.45 ± 0.21 m/s after BTA, and the difference between them was found to be statistically significant (p < 0.001). Mean MAS score (2.33 ± 0.70) after BTA decreased significantly when compared to the score before BTA (2.96 ± 0.62) (p = 0.001). SWV values positively correlated with MAS scores (ρ = 0.578, p = 0.003). The interobserver agreement expressed as interclass correlation coefficient (ICC) was 0.65 (95% CI 0.33–0.84, p < 0.001).
Conclusion
ARFI elastography for identifying structural changes that occur in the spastic muscle after BTA injection in children with CP can yield more valuable information with combined use of MAS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebral palsy (CP) is a term that describes muscle control deficiency that occurs as a result of damage in the brain. It is the most frequent upper motor neuron disease in childhood. Spastic CP is the most common type, seen in approximately 85% of children with CP. Due to spasticity, a great number of problems are seen in patients, such as locomotor disability, joint contractures, and difficulties in doing daily tasks. Because of these limiting effects, the main objective in treating children with CP is to decrease spasticity and to prevent the development of fixed contracture [1]. A botulinum toxin type A (BTA) injection, which is administered to spastic muscles during treatment, is a well documented, safe, frequently used, and effective treatment method [1–3]. The effect of BTA is to inhibit the release of acetylcholine in neuromuscular junctions. It causes temporary denervation in muscles [1]. The determination of medical and physical treatment efficacy and assessment of disease progression or regression in children with CP is possible only through the objective measurement of muscle stiffness. The modified Ashworth scale (MAS) is the most frequently used method in the assessment of spasticity in clinical practice and is applied by physicians or physiotherapists [4]. With this method, however, muscle tonus cannot be assessed objectively, and there is no standardization; moreover, it has a low level of reliability [5–7].
Ultrasound elastography is an imaging method that assesses the viscoelastic characteristics of tissues noninvasively. In ultrasound elastography, the basic principle is to measure the stiffness of tissues using a variety of technical approaches. In past years, a number of ultrasound elastography techniques have been developed, such as transient elastography, real-time elastography, and acoustic radiation force impulse (ARFI) elastography [8, 9]. ARFI elastography is a relatively new ultrasonographic method that shows quantitatively the degree of stiffness of tissues and lesions without the need for external compression [10]. Thus, it is a less operator-dependent technique. In this modality, a short-term (0.03–0.4 ms), high-powered (2.67 MHz frequency) acoustic compressive radiation force is applied to tissues instead of external compression. This applied force causes small displacements in the tissue (1–10 μm). In the horizontal plane, these translocations are called shear waves. Advanced ultrasound techniques can measure the speeds of these shear waves. In ARFI imaging, these speeds are given in m/s. Sheer wave velocity (SWV) is directly correlated with tissue stiffness. In general, greater SWV correlates with stiffer tissue [11]. In the literature, there are several reports of studies conducted using different ultrasonography techniques that assessed muscle stiffness in patients with CP by using ultrasound elastography [12–15]. However, there are few studies that have assessed muscle stiffness after BTA injection in children with spastic CP using ultrasound elastography [13, 15]. These studies have concluded that the combined use of ultrasound elastography with clinical scales can be useful in the assessment of spasticity.
The objective of our study was to assess the changes in medial gastrocnemius muscle (GCM) stiffness after BTA injection in children with spastic CP by using ARFI elastography and to research the usability of this technique in clinical practice. Our study is the first to evaluate the feasibility of the ARFI technique in children with spastic CP before and after BTA treatment.
Materials and methods
Participants
Twenty-four spastic lower extremities of 12 patients with CP (six girls, six boys, mean age 8.58 ± 2.48 years (age range 6–14), mean body weight 21.83 ± 5.13) were assessed. All the patients were diplegic. The inclusion criteria were: (1) within the age range of 6–15; (2) a diagnosis of spastic CP; (3) a muscle spasticity score greater than 1 according to the MAS scale; (4) did not receive a BTA injection in the last 6 months and (5) has not undergone a surgical procedure of the lower extremity. The exclusion criteria were: (1) presence of fixed ankle contracture and (2) previous lower extremity surgery. The study was approved by the Institutional Ethics Committee, and all parents provided written informed consent.
Procedure
Botulinum toxin A (BTA) (Botox, Allergan, Inc., CA, USA) injections were administered to the spastic medial GCM of all children. The dose of BTA (200–300 units) was adjusted according to the degree of spasticity in each patient. The injections were given by an experienced physical therapist. No side effects or complications were observed after the injections. Muscle stiffness was measured with the ARFI technique before the procedure and in the first month after the procedure. At the same time, patients’ spasticities were assessed, scored between 0 and 5, and recorded by a physical therapist using a modified Ashworth scale (MAS) (0 = normal, 5 = extreme resistance) [4]. For statistical purposes, a score of 1 was considered as 1, while a score of 1+ was regarded as 2 and so on up to a score of 4, which was regarded as 5 [16].
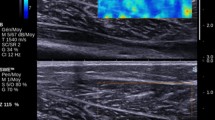
Ultrasound elastography examinations of the patients were made with ARFI elastography (Acuson S2000; Siemens Medical Solutions, Mountain View, CA, USA) using a linear probe (9L4). A virtual touch tissue quantification (VTQ) application was chosen for the quantitative assessment of tissue stiffness. ARFI measurements of the patients were taken within the same day by a radiologist with 4 years of ultrasound elastography experience who was blind to the MAS scores of the patients. All subjects were scanned on an examination platform in the prone position with their feet hanging over the edge of the table to prevent GCM contractions. Both axial and longitudinal plane medial GCM were evaluated with B-mode ultrasound before elastography measurements, and the transducer was placed on the medial GCM parallel to the long axis of the muscle by applying minimal compression (as much as the weight of the probe) (Fig. 1). For SWV measurements, a region of interest (ROI) cursor was placed at the mid-point of the GCM’s largest circumference (Fig. 2). The ROI box used for ARFI measurements has a standard size of 0.5 cm2. SWV values are seen on the screen as m/s (meters per second). Five measurements were made for each muscle, and the mean values of these were used for analysis. For SWV, the range was 0–9 m/s. When the measurements were erroneous, “x.xx” was seen on the screen, and the measurements were repeated until valid values were found.
For interobserver agreement assessment, another radiologist with 2 years of US elastography experience assessed five patients chosen randomly. The assessments of both radiologists were made on the same day.
Statistical analysis
Statistical analyses were performed with SPSS 18.0 for Windows. Data were presented as a mean ± standard deviation (SD), as a median (min–max), and as a frequency (%). The Shapiro–Wilk test was used to analyze the normal distribution assumption of the quantitative outcomes. To compare two dependent groups, we used the paired t test for normally distributed data and the Wilcoxon signed-rank test for non-normal data. The Spearman rank correlation test was used for the determination of correlations. A p value less than 0.05 was considered to be statistically significant. The interclass correlation coefficient (ICC) was used to examine the agreement between the measurements as follows: poor agreement, ICC < 0.40; fair to good agreement, ICC = 0.40–0.75; and excellent agreement, ICC > 0.75.
Results
SWV values and MAS degrees obtained before and after treatment were compared. The assessment is summarized in Table 1.
Before BTA, 5 (20.8%) out of 24 extremities were measured as MAS score 2, 15 (62.5%) were measured as MAS score 3, and 4 (16.7%) were measured as MAS score 4. After BTA, one (4.2%) out of 24 extremities was measured as MAS score 1, 16 (66.7%) were measured as MAS score 2, 5 (20.8%) were measured as MAS score 3, and 2 (8.3%) were measured as MAS score 4 (Table 1; Fig. 2). The average MAS score values were 2.96 ± 0.62 before BTA and 2.33 ± 0.70 after BTA, and the difference between them was statistically significant (p = 0.001) (Table 1). The average SWV values were 3.20 ± 0.14 before BTA and 2.45 ± 0.21 after BTA, and the difference between them was statistically significant (p < 0.001) (Table 1; Fig. 3). The SWV values positively correlated with MAS score (ρ = 0.578, p = 0.003). The interobserver agreement expressed as ICC was 0.65 (95% CI 0.33–0.84, p < 0.001).
Discussion
One of the most important problems in monitoring children with CP is the lack of suitable measuring tools for the assessment of the efficiency of interventions and treatment methods for muscle spasticity in clinical practice. Clinical measurements can give some information; however, these are subjective. ARFI elastography is a technique that can measure muscle stiffness noninvasively and objectively, and it can indirectly inform us about muscle spasticity and can help us to evaluate the efficiency of the treatments in these children.
ARFI imaging is a relatively recent ultrasound elastography technology. It enables the noninvasive and quantitative assessment of the elastic characteristics of tissues. Unlike conventional elastography techniques, this method provides an opportunity to assess without the need for external compression, and thus it is less operator-dependent [17]. Recently, there has been an increase in the number of studies that show the efficiency and benefits of the ARFI technology method in clinical practice [11, 18, 19].
In the medical literature, there are few reports of elastography studies before and after treatment in spastic patients, and these studies have been conducted using the strain elastography technique, which is a semi-quantitative method. In the case of the strain elastography technique, soft tissues are more deformed and stiff tissues are less deformed with external compression, and this information is color-coded on the screen. Tissue elasticity is indicated by colors, and the average intensity of color pixels is used. Park and Kwon used this method in their study; in the assessment before and after BTA, they found a decrease in red pixel intensity, which is an indicator of muscle stiffness in the assessment, 4 weeks after BTA injection [15]. Boyaci et al. showed that red pixel intensity was higher in a group with CP when compared with a control group, and that intensity decreased 4 weeks after treatment [13]. In a study conducted with spastic biceps brachii muscles of stroke patients, Askin et al. showed that strain index values decreased significantly after BTA injection [20]. However, there is only one study in the literature, conducted by Cho et al., which assesses spastic muscles with ARFI [21]. Cho et al. assessed the spastic lower extremity muscles of early cervical spinal cord injury (SCI) patients with the ARFI technique and found differences between spastic SCI patients, nonspastic SCI patients, and normal controls.
Our study is the first to assess the intrinsic muscle stiffness before and after BTA treatment by using the ARFI technique in children with spastic CP, which is an upper motor neuron disease. The results of our study showed a significant decrease in SWV values after treatment, and SWV values were found to be correlated with MAS scores. However, while there was no change in the MAS scores of some patients after BTA treatment, there was a minimal increase in SVW values. This may be due to the ineffectiveness of BTA treatment depending on various factors (e.g., BTA dose, injection failure, individual subcutaneous fat tissue thickness) in these patients. In histopathological studies conducted with children with CP, an increase was found in collagen content, while a decrease was shown in sarcomeres, and MAS was found to be significantly correlated with the total collagen amount [15, 22, 23]. Since ARFI elastography can assess the structural changes in tissues quantitatively, increased collagen amounts in spastic muscles can be demonstrated indirectly using this technique. The ARFI technique is a less user-dependent technique, and with this technique, the stiffness in muscles can be expressed numerically. This technique can measure the degree of stiffness in spastic muscles indirectly with SWV values. Thus, it provides more objective data to the clinician in the assessment and follow-up of these patients.
Similar to previous studies in the literature, all children were in a prone position during the US examinations, with their feet in the neutral position and feet to the edge of the table to prevent GCM contractions in our study [12, 15]. Lee et al. showed that the SWV was found to increase in the medial GCM with increased ankle position, joint torque, and fascicle strain in their study [14]. However, they compared the medial GCM of the more-affected limb with that of the less-affected limb in patients with unilateral CP, and status before and after BTA treatment was not compared. Our study is the first study to evaluate intrinsic muscle stiffness before and after BTA treatment in CP patients with ARFI, which is a new method. However, in future studies, it would be more appropriate to measure the stiffness of the muscle at the phasic phase to identify the severity of the spasticity for understanding the causes of abnormal movement and for guiding treatment planning.
Our study has some limitations. As mentioned above, measurement of muscle stiffness in the neutral position alone can be regarded as a limitation in terms of the use of ARFI SWV values in treatment follow-up. The number of cases is relatively small. Also, a short-term assessment was made (4 weeks later). Long-term assessment results will be more useful for clinicians; therefore, long-term follow-up studies are required.
Conclusion
In conclusion, we assessed structural changes in the medial GCM after BTA injection in children with spastic CP by using ARFI elastography. ARFI elastography is a valuable method that shows muscle stiffness in children with spastic CP with objective numerical values, and its combined use with MAS in the treatment planning and treatment efficiency of these patients can yield more useful results.
References
Kerr Graham H, Selber P. Musculoskeletal aspects of cerebral palsy. J Bone Jt Surg Br. 2003;85:157–66.
Cosgrove AP, Corry IS, Graham HK. Botulinum toxin in the management of the lower limb in cerebral palsy. Dev Med Child Neurol. 1994;36:386–96.
Langdon K, Blair E, Davidson SA, et al. Adverse events following botulinum toxin type A treatment in children with cerebral palsy. Dev Med Child Neurol. 2010;52:972–3.
Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–7.
Yam WK, Leung MS. Interrater reliability of Modified Ashworth Scale and Modified Tardieu Scale in children with spastic cerebral palsy. J Child Neurol. 2006;21:1031–5.
Mutlu A, Livanelioglu A, Gunel MK. Reliability of ashworth and modified ashworth scales in children with spastic cerebral palsy. BMC Musculoskelet Disord. 2008;9:44.
Numanoğlu A, Günel MK. Intraobserver reliability of modified Ashworth scale and modified Tardieu scale in the assessment of spasticity in children with cerebral palsy. Acta Orthop Traumatol Turc. 2012;46:196–200.
Ruan Z, Zhao B, Qi H, et al. Elasticity of healthy Achilles tendon decreases with the increase of age as determined by acoustic radiation force impulse imaging. Int J Clin Exp Med. 2015;15:1043–50.
Brandenburg JE, Eby SF, Song P, et al. Ultrasound elastography: the new frontier in direct measurement of muscle stiffness. Arch Phys Med Rehabil. 2014;95:2207–19.
Fahey BJ, Nightingale KR, Nelson RC, et al. Acoustic radiation force impulse imaging of the abdomen: demonstration of feasibility and utility. Ultrasound Med Biol. 2005;31:1185–98.
Nightingale K. Acoustic radiation force impulse (ARFI) imaging: a review. Curr Med Imaging Rev. 2011;7:328–39.
Kwon DR, Park GY, Lee SU, et al. Spastic cerebral palsy in children: dynamic sonoelastographic findings of medial gastrocnemius. Radiology. 2012;263:794–801.
Boyaci A, Tutoglu A, Boyaci N, et al. Changes in spastic muscle stiffness after botulinum toxin A injections as part of rehabilitation therapy in patients with spastic cerebral palsy. NeuroRehabilitation. 2014;35:123–9.
Lee SMS, Gaebler-Spira D, Zhanga LQ, et al. Use of shearwave ultrasound elastography to quantify muscle properties in cerebral palsy. Clin Biomech. 2016;31:20–8.
Park GY, Kwon DR. Sonoelastographic evaluation of medial gastrocnemius muscles intrinsic stiffness after rehabilitation therapy with botulinum toxin a injection in spastic cerebral palsy. Arch Phys Med Rehabil. 2012;93:2085–9.
Picelli A, Dambruoso F, Bronzato M, et al. Efficacy of therapeutic ultrasound and transcutaneous electrical nerve stimulation compared with botulinum toxin type A in the treatment of spastic equinus in adults with chronic stroke: a pilot randomized controlled trial. Top Stroke Rehabil. 2014;21:S8–16.
Nightingale KR, McAleavey SA, Trahey GE. Shear wave generation using acoustic radiation force: in vivo and ex vivo results. Ultrasound Med Biol. 2003;29:1715–23.
Friedrich-Rust M, Wunder K, Kriener S, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology. 2009;252:595–604.
Palmeri ML, Wang MH, Rouze NC, et al. Noninvasive evaluation of hepatic fibrosis using acoustic radiation force-based shear stiffness in patients with nonalcoholic fatty liver disease. J Hepatol. 2011;55:666–72.
Aşkın A, Kalaycı ÖT, Bayram KB, et al. Strain sonoelastographic evaluation of biceps muscle intrinsic stiffness after botulinum toxin-A injection. Top Stroke Rehabil. 2016;23:1–6.
Cho KH, Nam JH. Evaluation of stiffness of the spastic lower extremity muscles in early spinal cord injury by acoustic radiation force impulse imaging. Ann Rehabil Med. 2015;39:393–400.
Booth CM, Cortina-Borja MJ, Theologis TN. Collagen accumulation in muscles of children with cerebral palsy and correlation with severity of spasticity. Dev Med Child Neurol. 2001;43:314–20.
Smith LR, Lee KS, Ward SR, et al. Hamstring contractures in children with spastic cerebral palsy result from a stiffer extracellular matrix and increased in vivo sarcomere length. J Physiol. 2011;589:2625–39.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no commercial associations or sources of support that might pose a conflict of interest.
Ethical statement
The study was approved by the Medical Ethics Committee of the University Hospital, and all subjects provided written informed consent.
About this article
Cite this article
Ceyhan Bilgici, M., Bekci, T., Ulus, Y. et al. Quantitative assessment of muscle stiffness with acoustic radiation force impulse elastography after botulinum toxin A injection in children with cerebral palsy. J Med Ultrasonics 45, 137–141 (2018). https://doi.org/10.1007/s10396-017-0780-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-017-0780-y