Abstract
A case of perforated multiple gastric duplication cysts is presented. One of the gastric duplication cysts without perforation was seen on ultrasonography (US) with the following specific findings of gastric duplication cysts: a five-layered appearance, fold-like structures in the wall, and blood supply from the gastroepiploic artery. Other cysts with perforation presented with irregular and thin walls with a lack of the “double-wall sign” on US. These characteristic findings may be specific to perforated multiple gastric duplication cysts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric duplication cysts are rare and represent only 4% of all duplication cysts of the alimentary tract [1]. Although the cysts are commonly solitary and located along the great curvature of the stomach, multiple gastric duplication cysts or perforated duplication cysts are rare and have been reported only in a few case reports [2–6]. Furthermore, the ultrasonographic findings in this case, i.e., a five-layered appearance with fold-like structures in the wall, have not been reported previously.
Case report
A 9-month-old female infant presented with a several-day history of increasing episodes of vomiting and diarrhea. She was transferred to our hospital with suspected ileus and/or colitis. On physical examination, there were no palpable masses or tenderness. Body temperature was 37.6°C. Laboratory data revealed abnormal levels of white blood cells [14 × 103/μl (normally less than 9.8 × 103/μl)], CRP [0.3 mg/dl (normally less than 0.2 mg/dl)], and heamoglobin [8.3 g/dl (normally more than 15.2 g/dl)], and normal serum amylase.
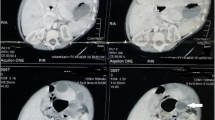
Contrast-enhanced 64-slice CT revealed an egg-shaped oval mass with target-like enhancement located near the greater curvature of the stomach (Fig. 1). The ascites spread around the stomach, and free air was not seen in the peritoneal cavity. According to the CT findings, a duplication cyst, Meckel’s diverticulum, or intussusception was suspected.
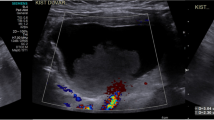
Ultrasonographic examination was performed using a Logiq 7 (GE Healthcare, Hino, Tokyo, Japan) with a 5.0- to 9.0-MHz linear probe (9L) and a 5.0- to 13.0-MHz linear probe (M12L). Ultrasonography (US) showed an oval cystic mass with a wall of 9 mm thickness beside the stomach (Fig. 2a). The cyst wall was contiguous with the gastric wall through the low echoic layer and consisted of five layers with a fold-like structure as follows: inner hyperechoic layer, hypoechoic thin layer, hyperechoic layer, hypoechoic thick layer, and outer hyperechoic layer (Fig. 2b, c). Color Doppler ultrasonography (CDUS) revealed tortuous vessels in the thick wall supplied by the gastroepiploic artery (Fig. 2d). Retrospectively, two other cystic masses with irregular walls were detected on the gastric antrum (Fig. 3a). A hyperechoic lesion and fluid collection with a fluid-fluid level spread around the stomach and oval cystic mass (Fig. 3b).
a A B-mode image produced using a 9L probe (9 MHz) shows an oval cystic mass with a wall 9 mm thick beside the stomach. b The cyst wall is contiguous with the stomach wall. c A B-mode image scanned using a M12L probe (12 MHz) clearly reveals the cystic wall consisting of five layers with a fold-like structure: an inner hyperechoic layer, a hypoechoic thin layer, a hyperechoic layer, a hypoechoic thick layer, and an outer hyperechoic layer. d CDUS shows tortuous vessels in the thick wall supplied by the gastroepiploic artery
An upper gastrointestinal series showed only a smooth compression at the great curvature side of the gastric antrum without communication between the gastric and cystic lumens (Fig. 4).
Although the preoperative diagnosis was gastric duplication, the reason why the ascites spread around the stomach as an acute peritonitis was unknown. Because of the patient’s aggravated symptoms of infection, cystectomy and abscess drainage were performed.
At surgery, not only an oval cystic mass (9 mm in diameter), but also two other cystic masses were found around the stomach. The cysts with thickened walls, which could be preoperatively detected, were shown to arise from the gastric antrum and to be contiguous with gastric serousal and muscular walls. The two other cysts with irregular and thin walls were not preoperatively detected. They had perforations to the peritoneal cavity. In addition, the omentum and inflammatory ascites covered these cysts and the gastric antrum.
Microscopic examination revealed that the thickened wall consisted of five layers similar to normal gastric layers (mucosa, muscularis mucosa, submucosa, muscle, and serosa) without perforation (Fig. 5a). In the other thin walls, ectopic pancreatic tissue and perforation were detected. Finally, the patient was diagnosed as having multiple gastric duplication cysts with perforation into the peritoneal cavity (Fig. 5b).
a Resected specimen shows the cut surface of the cysts. The thickened wall arises from the gastric antrum and resembles gastric mucosa with a fold-like structure (arrow). The two other cysts with irregular and thin walls have a perforation to the peritoneal cavity (arrowheads). b Microscopic examination reveals that the thickened wall consisted of five layers like a normal gastric layer (mucosa, muscularis mucosa, submucosa, muscle, and serosa) without perforation (H&E). c In other thin walls with perforation, ectopic pancreatic tissue is detected (H&E)
Discussion
Enteric duplication can occur anywhere in the gastrointestinal tract. The most common site is the ileum, so gastric duplication cysts are rare. US is the most specific imaging modality for diagnosis of enteric duplication cysts due to its ability to reveal the gastrointestinal signature of the cysts. Well described in the literature is the “double-wall” or “muscular rim” sign, which refers to the appearance of a cyst mimicking the gastrointestinal tract with an echogenic inner margin corresponding to mucosa surrounded by a hypoechoic rim of tissue representing the smooth muscle layer [7]. Identification of this sign on US has been regarded as characteristic of an enteric duplication cyst [8–12]. The presence of these two layers helps to exclude other cystic masses such as mesenteric or omental cysts, choledochal cysts, ovarian cysts, and pancreatic pseudocysts [13]. The double-wall sign, however, is not always specific for enteric duplication. Cheng et al. [14] reported cases of lesions mimicking enteric duplication cysts, such as mesenteric cysts and cystic teratomas. They mentioned that ultrasonographic visualization of the split hypoechoic muscularis propria layer or identification of all five layers increases the specificity in making the ultrasonographic diagnosis of a duplication cyst. In the present case, the five layers of the cyst wall, specific to enteric duplication cysts, could be preoperatively visualized by using US.
In abdominal US, this five-layered appearance is currently considered diagnostic of the gastrointestinal tract wall, as the alternating hyperechoic and hypoechoic layers roughly correspond to the anatomical structure from the endoluminal aspect: boundary echo plus mucosa, muscularis mucosa, submucosa, muscle, and serosa, respectively [15]. Although findings of a five-layered structure of gastrointestinal duplication cysts have been reported [10, 16], to the best of our knowledge, this is the first report of the sonographic features of the five-layered structure in a gastric duplication cyst. We correlated the ultrasonographic finding of a five-layered appearance with the pathological finding (Fig. 6a, b). Although there was a little mismatch between the ultrasonographic and pathologic findings with regard to the thickness of each layer, the alternating hyperechoic and hypoechoic layers of the gastric duplication cyst roughly corresponded to the anatomical structure from the endoluminal aspect: boundary echo plus mucosa, muscularis mucosa, submucosa, muscle, and serosa, respectively, as in a previous report about jejunal duplication cyst [10]. Also, US clearly revealed that the gastric duplication was contiguous with the gastric wall through the fourth hypoechoic layer corresponding to the muscle layer. Although endoscopic ultrasonographic findings of a gastric duplication cyst adjacent to the fourth layer of the stomach wall have been reported [17], in the present case, findings of the gastric duplication cyst adjacent to the fourth layer of the stomach wall could be clearly obtained with abdominal US. The fold-like structure of the cyst wall may be a finding specific to gastric duplication cysts. Furthermore, a common blood supply for gastric duplication cysts via the gastroepiploic artery has been frequently reported [18, 19]. In the present case, this blood supply was preoperatively depicted using CDUS.
Ultrasonographic pathologic correlation of thickened gastric duplication cyst with five-layered appearance. a B-mode image. 1 inner hyperechoic layer, 2 hypoechoic thin layer, 3 hyperechoic layer, 4 hypoechoic thick layer, 5 outer hyperechoic layer. b Microscopic specimen. 1 boundary echo plus mucosa, 2 muscularis mucosa, 3 submucosa, 4 muscle, 5 serosa
Gastric duplication cysts usually manifest as palpable masses in early infancy. Peptic ulcer formation, pancreatitis, and perforation with peritonitis, as in the present case, are other known complications. The perforation of a gastric duplication is either secondary to the development of a gastric ulcer or due to the pressure of accumulation of secretions of hydrochloric acid and enzymes continuously produced by the inner lining of the gastric mucosa and probably also by pancreatic tissue. In the present case, gastric duplication cysts with perforation had a small amount of ectopic pancreatic tissue in the cyst wall. Perforation of a solitary gastric duplication cyst into the peritoneal cavity has been reported. However, to the best of our knowledge, perforation of multiple gastric duplication cysts has been reported in only one case report [6], so this condition is extremely rare.
Unfortunately, small duplication cysts with perforation could not be preoperatively detected, although a large gastric duplication cyst without perforation was preoperatively diagnosed. Only one case report concerning the sonographic findings of perforation of duplication cysts has been published [6]. This paper reported that the presence of internal echoes, the heterogeneity of the surrounding mass, and the presence of a small amount of free peritoneal fluid in Morrison’s pouch, in conjunction with the double cystic wall (as in the present case), are suggestive of perforated duplication cysts of the alimentary system. In the present case, US preoperatively revealed dirty ascites with a fluid-fluid level corresponding to inflammatory fluid collection and a high-echoic lesion corresponding to the omentum covering the perforation site. However, a perforated gastric duplication was not present with a large gastric duplication cyst but was present with other small cysts. US retrospectively showed irregular walls with a lack of a “double-wall sign” at a small part of the perforated gastric duplication.
The management of a symptomatic duplication is surgical. It is commonly recommended that infants presenting with a subclinical intestinal duplication discovered incidentally undergo surgery for prevention of future complications due to obstruction or perforation. The muscularis of the cysts arises from and is contiguous with the muscularis of the stomach, but the mucosa of the cyst usually does not communicate with the gastric lumen. In the present case, there was no communication between the gastric lumen and the duplication cysts, including the cyst with perforation visualized by the upper gastrointestinal series. Therefore, when severe inflammation and/or dirty ascites are detected in patients with duplication cysts with or without free air in the peritoneal cavity, the possibility of perforation at other duplication cysts should be considered because of the lack of communication between the gastric lumen and duplication cysts.
In summary, a case of multiple gastric duplication cysts with perforation was reported. Ultrasonographic examination was the specific imaging modality that not only clearly revealed the five-layered appearance with a fold-like structure specific to gastric duplication, but also revealed a lack of wall layering and revealed the spread of heterogeneous fluid collection in the complicating perforation.
References
Faerber EN, Balsara R, Vinocur CD, de Chadarevian JP. Gastric duplication with hemoptysis: CT findings. Am J Roentgenol. 1993;161:1245–6.
Queizan A, Hernandez F, Rivas S, Herrero F. Prenatal diagnosis of gastric triplication. Eur J Pediatr Surg. 2006;16:52–4.
Bisset GS, Towbin RB. Pediatric case of the day. Multiple duplication cysts. Radiographics. 1986;6:917–20.
Karnak I, Ocal T, Senocak ME, Tanyel FC, Buyukpamukcu N. Alimentary tract duplications in children: report of 26 years’ experience. Turk J Pediatr. 2000;42:118–25.
Sutcliffe J, Munden M. Sonographic diagnosis of multiple gastric duplication cysts causing gastric outlet obstruction in a pediatric patient. J Ultrasound Med. 2006;25:1223–6.
Koumanidou C, Montemarano H, Vakaki M, Pitsoulakis G, Savvidou D, Kakavakis K. Perforation of multiple gastric duplication cysts: diagnosis by sonography. Eur Radiol. 1999;9:1675–7.
Segal SR, Sherman NH, Rosenberg HK, et al. Ultrasonographic features of gastrointestinal duplications. J Ultrasound Med. 1994;13:863–70.
Kangarloo H, Sample WF, Hansen G, Robinson JS, Sarti D. Ultrasonic evaluation of abdominal gastrointestinal tract duplication in children. Radiology. 1979;131:191–4.
Moccia WA, Astacio JE, Kaude JV. Ultrasonographic demonstration of gastric duplication in infancy. Pediatr Radiol. 1981;11:52–4.
Simonovsky V. Jejunal duplication cyst displaying peristalsis and a five-layered appearance of the wall: a preoperative ultrasound diagnosis. Eur Radiol. 1996;6:153–5.
Barr LL, Hayden CK Jr, Stansberry SD, Swischuk LE. Enteric duplication cysts in children: are their ultrasonographic wall characteristics diagnostic? Pediatr Radiol. 1990;20:326–8.
Richards DS, Langham MR, Anderson CD. The prenatal sonographic appearance of enteric duplication cysts. Ultrasound Obstet Gynecol. 1996;7:17–20.
Carty HML, Higham J, Crawford SF. Paediatric ultrasound. 1 edn ed. London: Greenwich Medical Media Ltd; 2001. p. 61–71.
Cheng G, Soboleski D, Daneman A, Poenaru D, Hurlbut D. Sonographic pitfalls in the diagnosis of enteric duplication cysts. Am J Roentgenol. 2005;184:521–5.
Kimmey MB, Martin RW, Haggitt RC, Wang KY, Franklin DW, Silverstein FE. Histologic correlates of gastrointestinal ultrasound images. Gastroenterology. 1989;96:433–41.
Royal SA, Hedlund GL, Kelly DR. Ileal duplication cyst. Am J Roentgenol. 1994;163:98.
Takahara T, Torigoe T, Haga H, et al. Gastric duplication cyst: evaluation by endoscopic ultrasonography and magnetic resonance imaging. J Gastroenterol. 1996;31:420–4.
Knight J, Garvin PJ, Lewis E Jr. Gastric duplication presenting as a double esophagus. J Pediatr Surg. 1983;18:300–1.
De la Torre Mondragon L, Daza DC, Bustamante AP, Fascinetto GV. Gastric triplication and peritoneal melanosis. J Pediatr Surg. 1997;32:1773–5.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s10396-010-0290-7
About this article
Cite this article
Marugami, N., Hirai, T., Yamashita, N. et al. A case of perforated multiple gastric duplication cysts with five-layered appearance on ultrasonography. J Med Ultrasonics 38, 47–51 (2011). https://doi.org/10.1007/s10396-010-0282-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-010-0282-7