Abstract
Aims
Hypertension (HTN), diabetes mellitus (DM), and comorbidity are global health problems contributing to increased cardiovascular diseases (CVD). The demographic transition and urbanization have changed people’s lifestyles. This study aimed to examine the prevalence and associated factors of HTN, DM, and comorbidity in Bangladesh.
Methods
This study used Bangladesh Demographic Health Survey 2017–18 data. Bivariate analysis was taken to measure the associations, and multilevel modeling (binary logistic regression) was used to measure the effects.
Results
This study has found the prevalence of HTN, DM, and comorbidity at 28.01%, 10.27%, and 4.26%, respectively, among the adult population of Bangladesh. The older age groups, women, urban people with high BMI, unemployed, and non-manual working people have a higher prevalence of these diseases and comorbidity. The rapid increase of HTN, DM, and comorbidity must be prevented and controlled.
Discussion
Findings from this research can be used for policy formulation of public health to prevent and control HTN, DM, and comorbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of non-communicable diseases is increasing all over the world. Non-communicable diseases (NCDs) cost the lives of 41 million people annually, accounting for 71% of all deaths worldwide (WHO 2018), and that is projected by WHO to be 55 million in 2030 (WHO 2013). Low- and middle-income countries account for 77% of all NCD mortality (WHO 2018). NCDs were responsible for 7.9 million (55%) of the anticipated 14.5 million deaths in South-East Asia in 2008. Over the next decade, mortality from NCDs is expected to rise by 21%. Two of the fatal NCDs are CVD (CVD) and DM (DM) (WHO 2018). HTN is the most critical risk factor for nearly all CVDs (Kjeldsen 2018).
HTN is the medical term for elevated blood pressure (Messerli et al. 2007; Andreadis 2016; Beevers et al. 2014; Mills et al. 2020). Though there is a lot of development in medical science regarding the treatment of high blood pressure (Beevers et al. 2014; Andreadis 2016), the threat of HTN has increased a lot because the awareness and control of HTN remained low among people (Zhou et al. 2021; Rana et al. 2020; Messerli et al. 2007; Andreadis 2016; Beevers et al. 2014). HTN is associated with a greater risk of CVD becoming a significant cause of death worldwide, accounting for approximately 7 million yearly mortalities (Franklin and Wong 2013). HTN is linked to coronary heart disease (CHD), congestive heart failure (CHF), stroke, peripheral arterial disease (PAD), and chronic kidney disease problems (Lawes et al. 2004; Franklin and Wong 2013).
Diabetes is a chronic metabolic condition marked by high blood glucose levels (Wong and malik 2015; Holt and Kumar 2015). Long-term consequences such as CVD, blindness, renal failure, amputations, and stroke are important causes of morbidity and early death (Holt and Kumar 2015). Diabetes prevalence was expected to be 2.8% worldwide in 2000, with a projected increase to 4.4 % by 2030, resulting in a total of 366 million diabetes patients with a projection of 552 million in 2030 (Wong and malik 2015). In 2012, DM caused 1.5 million and 2.2 million mortality by increasing the prevalence of CVDs and other diseases (WHO 2016).
The global action plan for the prevention and control of NCDs 2013–2020 was taken with the vision to make “a world free of the avoidable burden of non-communicable diseases,” and one of the goals of the plan was to reduce the relative risk of early death from CVDs by 25% (WHO 2013). However, the increasing prevalence of HTN and DM did not help that progress. The burden of HTN and DM is higher in lower-middle-income countries (LMIC) (Mills et al. 2020; Zhou et al. 2021; WHO 2016).
Due to the demographic transition, Bangladesh has more adults than in the past few decades, so the risk of HTN and DM among people is increasing (Reddy 1996; WHO 2015). Bangladesh is also going through a nutritional transition and epidemiological nutrition, influencing the prevalence of non-communicable diseases (Mascie-Taylor 2012). A shift from the traditional diet to processed and fast food, a growing pattern of sedentary lifestyle because of improved socio-economic position, and less scope of physical activity because of unplanned urbanization are playing a role in the rise of HTN and DM in Bangladesh (Chowdhury et al. 2020; Fatema et al. 2017). According to the Ministry of Health and Family Welfare’s NCD risk factors survey from 2010, 95% of the population had at least one NCD. According to the World Health Organization (WHO), NCDs account for 52% of deaths in Bangladesh, and among them, CVDs alone were responsible for 27% of all fatalities. Bangladesh successfully reduced communicable diseases, but now the disease patterns shifted to non-communicable diseases, and HTN is a key factor (Karar et al. 2009; Mascie-Taylor 2012).
Bangladesh is facing a heavy burden of HTN and diabetes (Rahman et al. 2017a, b, c, 2015; Alam et al. 2014; Biswas et al. 2016). An analysis of studies from 1976 to 2019 showed that the prevalence of HTN grew by 0.51% every year (Chowdhury et al. 2020). The WHO’s “Non-Communicable Disease Risk Factor Survey Bangladesh 2010” identified an HTN prevalence of 17.9% among participants aged 25 and older (WHO 2011). Another meta-analysis of studies from 1994 to 2013 showed that DM increased by 0.27% and 0.47% yearly in urban and rural regions, respectively (Biswas et al. 2016). BDHS 2017–18 reported every 1 in 10 adults in Bangladesh with DM (NIPORT 2020). The rise in blood pressure (BP) and glucose level with ageing is a universal phenomenon (Baksi et al. 2009; Holt and Kumar 2015). HTN and DM were found in a higher proportion among Bangladeshi women than among men (Chowdhury et al. 2020; Rahman et al. 2017a, b, c; Islam et al. 2015; NIPORT 2020; Biswas et al. 2016). Bangladesh’s largest cities are heavily crowded, with little room for physical exercise; moreover, junk food is growing popular due to the ongoing change in dietary behavior. As a result, wealthy households in metropolitan regions have a larger proportion of overweight persons (Zahangir et al. 2017). Higher-educated people have higher odds of being hypertensive and diabetic in Bangladesh (Tareque et al. 2015; Rahman et al. 2017a, Talukder and Hossain 2020). The rich people in Bangladesh consume more food, are over-nourished, are more prone to be fat, perform less physically demanding work, and therefore have HTN (Tareque et al. 2015; Talukder and Hossain 2020). Industrial workers or day laborers are less prone to be hypertensive than government & non-government employees, business owners, farmers, agricultural workers, and other self-employed individuals (Rahman et al. 2017a).
People with higher BMI have a higher chance of getting HTN and DM in Bangladesh. Women, urban people, and higher educated and wealthy people have a higher chance of obesity, and it is also results in HTN and DM among them (Islam and Majumder 2012). BDHS 2017–18 reported across the eight divisions of Bangladesh that HTN among women aged 18 and older varies from 23% in Dhaka to 34% in Barisal. For men, the prevalence ranges from 21% in Mymensingh to 31% in Barisal (NIPORT 2020). The Dhaka division had the highest DM in men and women. The prevalence varies from 6.3 to 15.6 for men and 5% to 13.3% for women (NIPORT 2020).
This research will investigate the following research question – How do socioeconomic, demographic, lifestyle, and regional factors affect HTN, DM, and their comorbidity in Bangladesh in 2017?
This study is motivated to find out the socioeconomic, demographic factors, lifestyle, and regional factors provoking increasing HTN, DM, and comorbidity rate in Bangladesh, which will help the government and policymakers to understand the existing patterns of HTN, DM, and comorbidity in Bangladesh, to design evidence-based policies to prevent high rates of HTN, DM, and comorbidity and to reduce its bad effects on the Bangladeshi population.
Materials and methods
Data source
This research is based on Bangladesh Demographic Health Survey 2017–18 data. The most recent BDHS survey held in 2017–18 has been used to check the effects of the different factors on HTN, DM, and comorbidity. The National Institute of Population Research and Training (NIPORT) conducted the 2017–18 BDHS. The survey used a nationally representative sample that covered the whole population of Bangladesh’s noninstitutional housing units and followed a two-stage stratified sampling (NIPORT et al. 2020).
Dependent variable
Joint National Committee (JNC7) on the Prevention, Detection, Evaluation, and Treatment (2003) of High Blood Pressure classified HTN as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg. People taking medicine to lower BP are considered hypertensive, according to the BDHS program. Fasting glucose greater than or equal to 7.0 mmol/l is diabetes (WHO 2006). The joint existence of HTN and DM is comorbidity (Holt and Kumar 2015).
Independent variables
Age (18–29, 30–39, 40–49, 50–59, 60–69, 70–max), sex (female and male), wealth status (poorest, poorer, middle, richer, richest), employment status (employment, unemployed), job nature (non-manual, manual), educational attainment (no education & preschool, primary, secondary, higher), type of place of residence (urban, rural), BMI Asian cut-off (Underweight, Normal, Overweight or obese), and division (Barisal, Chittagong, Dhaka, Khulna, Mymensingh, Rajshahi, Rangpur, and Sylhet) are chosen as explanatory variables. A variable has been created, namely as job nature from the variable occupation and categorized into unemployed, manual (farming/agricultural work, poultry and cattle raising, home-based manufacturing, unskilled labor, factory work, blue-collar service, domestic servant), and non-manual (semi-skilled, professional/ technical, business, others). The Body Mass Index (BMI) for the Asian cut-off has been labeled as underweight for BMI <18.5, normal for BMI 18.5–22.9, and overweight for BMI≥ 23.
Statistical analysis
This study used statistical analysis to determine which factors are linked to HTN, DM, and comorbidity. Univariate and bivariate (chi-square test) analyses were conducted to check the association between the dependent and explanatory variables. After reviewing the association between the explanatory variable and dependent variable, this study has gone through a multilevel binary logistic model to determine the effects of different factors on HTN, DM, and comorbidity separately using the significant explanatory variables. Analyses were conducted using STATA version 16.
Results
Descriptive data
The youngest age group, 18–29, has the lowest prevalence of HTN (10.65%). The oldest age group 70–max is the most hypertensive (56.06%); 29.44% of the females are hypertensive, while 26.20% of males are hypertensive; 36.11% of people in the educational category no education, preschool are reported as hypertensive. From categories primary, secondary, and higher, 27.36%, 23.72%, and 23.45% of people are hypertensive, respectively; 31.84% of the unemployed, whereas 34.16% of people from the non-manual job and 23.36% from the manual job are hypertensive; 24.32% of people from the poorest quantile tend to be hypertensive. The richest quantile has the highest HTN prevalence (33.59%) among the categories; 29.13% of the urban people have HTN, while 27.59% of the rural people are hypertensive; 17.72% of people from the underweight category are hypertensive, the lowest among the BMI categories. However, the overweight or obese category tends to be more hypertensive (37.92%) than other categories; 33.43% of people in the Barisal division are hypertensive, the most hypertensive region in Bangladesh. In Mymensingh, 23.83% of people have HTN (Table 1).
The highest DM (16.56%) among age groups 50–59. Men (9.95%) are more prone to diabetes than women; 10.59% of people with primary education and 10.52% in higher education have DM. People from a non-manual job have a higher DM prevalence (15.23%) than other categories. The higher wealth quintiles have shown a higher prevalence of DM; 19.31% of people from the richest wealth quantile have diabetes; 14.04% of urban people have the disease. Overweight people have the highest DM prevalence (14.25%) compared with the other BMI categories. The capital Dhaka (15.09%), has the highest DM, whereas the Rangpur division has the lowest prevalence (5.73%). The older age groups showed a higher prevalence of comorbidity. The age group, 60–69, led to the highest 9.13% coexistence of HTN and DM; 4.10% of men and 4.39% of women suffered comorbidity. The no-education, preschool education category (4.62%) has the highest percentage of comorbidity. People from the non-manual job category (7.06% vs. 5.45% & 2.52%) suffered comorbidity, the highest among the job nature categories. Urban people (5.45% vs. 3.79%), rich people (1.90% poorest vs. 8.63% richest), people with high BMI (7.40% vs. 1.50%), and Chittagong division (5.46%) showed a higher prevalence of comorbidity. Those covariates which were found significant at 10% in the bivariate analysis were only considered in regression analysis.
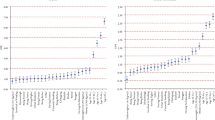
From Table 2, binary logistic regression following random intercept models has been used in three different models. People in the older age groups are more likely to have NCDs compared with the 18–29 age groups while controlling other variables. The odds ratio continues to increase with age. Age group 70–max has a 17.09 times higher chance (CI 13.898–21.014, p < 0.01) to have HTN, 50–59 has 4.769 (CI 3.764–6.042, p < 0.01) times higher risk to have diabetes and 70–max has 24.334 (CI 14.86–39.848, p < 0.01) higher chance to have both diseases than age group 18–29. Females have a 32.4% higher chance (CI 1.18–1.417, p < 0.01) of being hypertensive than males. Rural people have a 0.2% higher chance (CI 0.893–1.125) of having HTN, a 3.3% lower chance (0.821–1.139) of having diabetes, and a 4.6% (CI 1.166–1.867) higher chance to have the comorbidity than Urban people. The primary education category has a 6.4% (CI 0.943–1.199) chance of having HTN. The non-manual category from job nature showed a higher possibility of having HTN (OR 1.096, CI 0.935–1.286), diabetes (OR 1.08, CI 0.867–1.345), and comorbidity (OR 1.287, CI 0.953–1.738). As people become wealthier, they are more likely to develop HTN, diabetes, and comorbidity. Richest quantile has 38.6% higher odds (CI 1.161–1.655, p < 0.01) to be hypertensive, 145.8% higher risks (CI 1.889–3.198, p < 0.01) to have diabetes and 222.2% higher risk (CI 2.197–4.724, p < 0.01) to have both diseases.
People with overweight or obese category have 248.6% higher odds (OR 3.486, CI 3.008–4.039, p < 0.01) to be hypertensive, 106.1% higher odds (OR 2.061, CI 1.645–2.58, p < 0.01) to have diabetes and 305.6% higher odds (OR 4.056, CI 2.738–6.008, p < 0.01) to have both than underweight individuals. People from Rangpur have 79.1% higher odds (OR 1.791, CI 1.463–2.194, p < 0.01) to have HTN, 55% lower odds (OR 0.45, CI 0.334–0.608, p < 0.01) to have diabetes, and Mymensingh have 25.1% lower odds (OR 0.749, CI 0.509–1.102) to have both than the people of Dhaka. People of Sylhet have 39.8% higher odds to have HTN compared to the Dhaka division and 32% lower odds to have diabetes compared to the Dhaka.
Discussion
This is the first study to explore how socioeconomic, demographic, lifestyle, and regional factors affect HTN, DM, and their comorbidity in Bangladesh using multilevel modeling. With ageing, the vascular system, metabolic disorders, and many other biological changes happen, which trigger HTN and DM (Harvey et al. 2015; Suastika et al. 2012). The findings of this study were consistent with those of other studies (Rahman et al. 2017a; Islam et al. 2015; Chowdhury et al. 2020 Hanif et al. 2021; Talukder and Hossain 2020) in terms of the ageing process’s increased risk of HTN and DM. The life expectancy in Bangladesh is growing, and the population is ageing due to the demographic transition (Islam and Biswas 2014). Therefore, in the coming decades, Bangladesh will have many elderly patients with hypertension and diabetes.
Women in Bangladesh have higher risks of being hypertensive, diabetic, and both diseases, which supports the previous studies (Chowdhury et al. 2020; Rahman et al. 2017a, b, c; Islam et al. 2015; Talukder and Hossain 2020; Kibria 2021). A large portion of Bangladeshi women are homemakers (Gosoniu et al. 2008), and due to modern life and household activities become easier. Urban women in Bangladesh have a very limited scope of physical activity (Khan and Kraemer 2009). Though Bangladesh has improved significantly in reducing gender discrimination, women still lack proper health awareness (Rahman et al. 2017b). These problems lead to decreased physical activity and obesity, making people more susceptible to these illnesses.
There are no available studies on the effects of manual and non-manual jobs on HTN and DM in Bangladesh. Non-manual jobs have more impact than manual to have these diseases and comorbidity because non-manual workers are more physically inactive than manual workers. Rahman et al. (2017a) found that among manual workers, the prevalence is lower than in the professional category (government employee, non-government employee, business owner, farmer, agricultural worker, and other self-employed), which I mentioned as non-manual.
This research has found that wealthy people are at high risk of HTN, diabetes, and comorbidity. Wealth is associated with education and the type of place of residence. A higher percentage of educated and rich people reside in the urban areas of Bangladesh (BBS 2019). The dietary habit and lifestyles of wealthy people in urban areas could be a reason for this. The results support the claim of (Rahman et al. 2017a), 2015; Talukder and Hossain 2020), and some other studies that the risk of HTN increases the wealthier one gets.
BMI has a significant impact on these diseases. The nutritional transition is influencing the BMI level of people, which is very alarming for Bangladesh’s HTN, diabetes, and comorbidity outlook (Al Muktadir et al. 2019). Results regarding obesity support the evidence from (Rahman et al. 2017a; Talukder and Hossain 2020) that increased BMI causes a higher risk.
HTN, DM, and comorbidity are disproportionately distributed among Bangladesh’s different divisions. This study found the prevalence of these NCDs is associated with divisions. The socio-economic developments of Bangladesh have an unequal distribution throughout the country, which could be a reason for the disproportionate distribution of HTN.
The HTN status among the clusters shows some similarity (though the amount is small) because the socio-economic variables in a cluster have some similarities. Thus, there is a spatial effect, and it is affecting the HTN scenario. The impact of urban–rural residence, education, and employment status reveal insignificance.
Conclusion
Bangladesh needs to renovate its health system to combat HTN and diabetes. The grass-root level health service providers such as community clinics should provide treatment for these NCDs so that the vulnerable groups can avoid the unfortunate consequences. Strengthening community clinics with the equipment for checking and treating these diseases could help people prevent the problem. As these diseases are silent killers, the government should encourage people to do routine checkups of blood pressure and blood glucose level. HTN and diabetes-related health education should be addressed on the school-level syllabus so that individuals can be aware of these silent-killer diseases from a young age. Establishing fully equipped and active NCD corners in every government hospital is necessary. A collective effort is required to prevent the complications that arise from these diseases. This includes public health awareness, print and electronic media, collaborations between communities, and government-supported healthy policies to reduce population morbidity and death gradually.
Data availability
The data set used in this study is available at https://dhsprogram.com/data/dataset/Bangladesh_Standard-DHS_2017.cfm?flag=0.
References
Al Muktadir MH, Islam MA, Amin MN, Ghosh S, Siddiqui SA, Debnath D et al (2019) Nutrition transition–Pattern IV: Leads Bangladeshi youth to the increasing prevalence of overweight and obesity. Diabetes Metab Syndrome: Clin Res Rev 13(3):1943–1947. https://doi.org/10.1016/j.dsx.2019.04.034
Alam DS, Chowdhury MAH, Siddiquee AT, Ahmed S, Niessen LW (2014) Awareness and control of hypertension in Bangladesh: follow-up of a hypertensive cohort. BMJ open 4(12):e004983. https://doi.org/10.1136/bmjopen-2014-004983
Andreadis, E. A. (2016). Hypertension: a growing threat. Hypertension and Cardiovascular Disease, 1–17
Baksi AJ, Treibel TA, Davies JE, Hadjiloizou N, Foale RA, Parker KH et al (2009) A meta-analysis of the mechanism of blood pressure change with aging. J Am College Cardiol 54(22):2087–2092. https://doi.org/10.1016/j.jacc.2009.06.049
Bangladesh Bureau of Statistics (2019) Report on Bangladesh Sample Vital Statistics 2018. BBS, Dhaka
Beevers DG, Lip GYH, O’Brien ET (2014) The prevalance and causes of HTN in ABC of HTN (6th edition). John Wiley & Sons, Incorporated, p 1-9. https://ebookcentral.proquest.com/lib/soton-ebooks/reader.action?docID=1819338&ppg=1 [Accessed 25 September 2021]
Biswas T, Islam A, Rawal LB, Islam SMS (2016) Increasing prevalence of diabetes in Bangladesh: a scoping review, Public Health, Volume 138(2016) P4-11, ISSN 0033-3506, https://doi.org/10.1016/j.puhe.2016.03.025
Chowdhury MZI, Rahman M, Akter T, Akhter T, Ahmed A, Shovon MA et al (2020) Hypertension prevalence and its trend in Bangladesh: evidence from a systematic review and meta-analysis. Clin Hypertension 26:1–19. https://doi.org/10.1186/s40885-020-00143-1
Fatema K, Hossain S, Natasha K, Chowdhury HA, Akter J, Khan T, Ali L (2017) Knowledge attitude and practice regarding diabetes mellitus among nondiabetic and diabetic study participants in Bangladesh. BMC Public Health 17(1):1–10. https://doi.org/10.1186/s12889-017-4285-9
Franklin SS, Wong ND (2013) Hypertension and cardiovascular disease: contributions of the Framingham Heart Study. Global heart 8(1):49–57
Gosoniu GD, Ganapathy S, Kemp J, Auer C, Somma D, Karim F, Weiss MG (2008) Gender and socio-cultural determinants of delay to diagnosis of TB in Bangladesh, India and Malawi [Special section on gender and TB]. Int J Tuberculosis Lung Disease 12(7):848–855(8)
Hanif AAM, Hasan M, Khan MSA, Hossain MM, Shamim AA, Mitra DK et al (2021) Prevalence and associated factors of insufficient physical activity among elderly people in Bangladesh: a nationally representative cross-sectional study. BMJ Open Sport Exercise Med 7(3):e001135. https://doi.org/10.1136/bmjsem-2021-001135
Harvey A, Montezano AC, Touyz RM (2015) Vascular biology of ageing—implications in hypertension. J Mol Cell Cardiol 83:112–121. https://doi.org/10.1016/j.yjmcc.2015.04.011
Holt T, Kumar S (2015) ABC of diabetes. Wiley, New York
Islam A, Biswas T (2014) Health system in Bangladesh: challenges and opportunities. Am J Health Res 2(6):366–374. https://doi.org/10.11648/j.ajhr.20140206.18
Islam AK, Majumder AA (2012) HTN in Bangladesh: a review. Indian Heart J 64(3):319–323. https://doi.org/10.1016/S0019-4832(12)60096-0 [Accessed 12 September, 2021]
Islam SMS, Mainuddin AKM, Islam MS, Karim MA, Mou SZ, Arefin S, Chowdhury KN (2015) Prevalence of risk factors for hypertension: a cross-sectional study in an urban area of Bangladesh. Global Cardiol Sci Pract 2015(4). https://doi.org/10.5339/gcsp.2015.43
Karar AZ, Alam N, Streatfield KP (2009) Epidemiological transition in rural Bangladesh, 1986-2006. Glob Health Action 19(2). https://doi.org/10.3402/gha.v2i0.1904
Khan MMH, Kraemer A (2009) Factors associated with being underweight, overweight and obese among ever-married non-pregnant urban women in Bangladesh. Singapore Med J 50(8):804
Kibria GMA (2021) Prevalence and factors associated with diabetes among Bangladeshi adults: an analysis of demographic and health survey 2017–18. Diabetes Epidemiol Manag 2:100012, ISSN 2666-9706. https://doi.org/10.1016/j.deman.2021.100012
Kjeldsen SE (2018) HTN and cardiovascular risk: general aspects. Pharmacol Res 129(2018):95–99. https://doi.org/10.1016/j.phrs.2017.11.003
Lawes CMM, Hoorn SV, Law MR, Elliott P, MacMahon S, Rodgers A (2004) High blood pressure. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL (eds) Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors, vol 2. WHO, Geneva, pp 281–389
Mascie-Taylor N (2012) Is Bangladesh going through an epidemiological and nutritional transition? Coll Antropol 36(4):1155–1159
Messerli FH, Williams B, Ritz E (2007) Essential HTN. Lancet 370(9587):P91–P603, ISSN 0140-6736. https://doi.org/10.1016/S0140-6736(07)61299-9
Mills KT, Stefanescu A, He J (2020) The global epidemiology of HTN. Nat Rev Nephrol 16:223–237. https://doi.org/10.1038/s41581-019-0244-2
National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International (2020) Bangladesh Demographic and Health Survey 2011; NIPORT, Mitra and Associates, and ICF International: Dhaka, Bangladesh; Calverton, MD, USA
Rahman MM, Gilmour S, Akter S, Abe SK, Saito E, Shibuya K (2015) Prevalence and control of HTN in Bangladesh: a multilevel analysis of a nationwide population-based survey. J Hypertens 33:465–472
Rahman M, Williams G, Al Mamun A (2017a) Gender differences in HTN awareness, antihypertensive use and blood pressure control in Bangladeshi adults: findings from a national cross-sectional survey. J Health Popul Nutr 36(1):23
Rahman M, Zaman M, Islam J et al (2017b) Prevalence, treatment patterns, and risk factors of HTN and pre-HTN among Bangladeshi adults. J Hum Hypertens 32(5):334–348
Rahman MM, Akter S, Jung J, Rahman MS, Sultana P (2017c) Trend, projection, and appropriate body mass index cut-off point for diabetes and HTN in Bangladesh. Diabetes Res Clin Pract 126:43–53. https://doi.org/10.1016/j.diabres.2017.01.008. Accessed 25th September, 2021
Rana J, Oldroyd J, Islam MM, Tarazona-Meza CE, Islam RM (2020) Prevalence of hypertension and controlled hypertension among United States adults: evidence from NHANES 2017-18 survey. Int J Cardiol Hypertension 7:100061. https://doi.org/10.1016/j.ijchy.2020.100061
Reddy KS (1996) HTN control in developing countries: generic issues. J Hum HTN 10:33–38
Suastika K, Dwipayana P, Semadi MS, Kuswardhani RT (2012) Age is an important risk factor for type 2 DM and CVDs. In: Glucose tolerance. IntechOpen. https://doi.org/10.5772/52397. [Accessed 20 July 2022]
Talukder A, Hossain MZ (2020) Prevalence of DM and its associated factors in Bangladesh: application of two-level logistic regression model. Sci Rep 10, 10237. https://doi.org/10.1038/s41598-020-66084-9 [Accessed 20 June, 2022]
Tareque MI, Koshio A, Tiedt AD, Hasegawa T (2015) Are the rates of HTN and diabetes higher in people from lower socioeconomic status in Bangladesh? Results from a nationally representative survey. PloS one 10(5):e0127954. https://doi.org/10.1371/journal.pone.0127954 [Accessed 22 September, 2021]
Wong ND, Malik S (2015) Diabetes and Cardiovascular Disease: Evaluation. Prevention & Management, JP Medical Ltd
World Health Organization (2013) Follow-up to the Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. Sixty-sixth World Health Assembly, Agenda item, p 13
World Health Organization (2011) Non-communicable disease risk factor survey Bangladesh 2010. WHO, Dhaka
World Health Organization (2016) Global report on diabetes. WHO, France Available from: https://apps.who.int/iris/handle/10665/204871
World Health Organization (WHO) (2006) Definition and diagnosis of DM and intermediate hyperglycemia: report of a WHO/IDF consultation. WHO, Geneva
World Health Organization (WHO) (2015) Global status report on non-communicable diseases 2014. WHO, Geneva
World Health Organization (WHO) (2018) World health statistics 2018: monitoring health for the SDGs World Health Organization, Geneva
Zahangir MS, Hasan MM, Richardson A, Tabassum S (2017) Malnutrition and non-communicable diseases among Bangladeshi women: an urban–rural comparison. Nutrition Diabetes 7(3):e250–e250. https://doi.org/10.1038/nutd.2017.2
Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA et al (2021) Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 398(10304):957–980. https://doi.org/10.1016/S0140-6736(21)01330-1
Acknowledgments
We would like to thank Bangladesh Bureau of Statistics (BBS) and Bangladesh Demographic and Health Survey (BDHS) 2017–18 for providing us nationally representative data.
Author information
Authors and Affiliations
Contributions
MRH developed the study concepts and MRH, MMI, and FMN analyzed the data. MRH, MMI, FMN, MA, and MAA drafted the manuscript. All authors read, critically reviewed, and approved the final version of the paper.
Corresponding author
Ethics declarations
Ethical considerations
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not required.
Informed consent
Not applicable for this study.
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hasan, M.R., Islam, M.M., Noor, F.M. et al. Analyzing hypertension and diabetes mellitus status among Bangladeshi adults: evidence from Bangladesh Demographic Health Survey (BDHS) 2017–18 data. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-01987-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-01987-1