Abstract
Aims
To explore the association between known risk factors for diabetes and diabetes prevalence among disaggregated Asian American sub-ethnic groups and to highlight the importance of looking at data in disaggregated form.
Methods
Ten years of data collected by the California Health Interview Survey were pooled and analyzed. Logistic regression models, controlling for age, gender, and marital status, were used for the analysis. Comparisons were made among an aggregated sample of Asian Americans (N = 21,267) and a disaggregated sample of Asian Americans (i.e., Chinese, Japanese, Koreans, Filipinos, South Asians, and Vietnamese).
Results
Disaggregated data showed that Korean Americans who smoked had three times the odds of having diabetes compared to non-smoking Korean Americans [OR = 3.02 (95% CI 1.43, 6.39)]. High blood pressure puts both Japanese and Filipino Americans at twice the odds of having diabetes as those who do not have high blood pressure ([OR = 2.23 (95% CI 1.09, 4.54) and [OR = 2.82 (95% CI 1.82, 4.36)], respectively). Although close to 10% of Vietnamese Americans in the sample were current smokers, smoking status was not associated with diabetes.
Conclusions
The association between diabetes and known risk factors differ across Asian American sub-ethnic groups. Findings highlight the importance of disaggregated data and discourage a one-size-fits-all approach to diabetes care strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The National Diabetes Statistics Report indicated that 34.2 million Americans, approximately 1 in 10, have diabetes and 88 million, or 1 in 3 Americans, have pre-diabetes (Centers for Disease Control and Prevention [CDC] 2020). It is estimated that approximately 90–95% of the cases are type 2 diabetes (CDC 2019). High body mass index (BMI), high blood pressure, poor nutrition, physical inactivity, and smoking are some of the well-known risk factors for diabetes (Lindström and Tuomilehto 2003). More than half of those with diabetes are either current (21.6%) or former (36.4%) smokers, 68.4% have high blood pressure, defined as having blood pressure ≥ 140/90 mmHg or taking antihypertensive medication, and 89% had a BMI higher than the cut-off for normal body weight (CDC 2020).
Although Asian Americans have one of the lowest rates of diabetes when compared to African Americans and Hispanic/Latinos, approximately 2.3 million Asian Americans, age 18 years or older, have diabetes and about 0.7 million of these cases are undiagnosed based on 2018 estimates (CDC 2020). With a population size of 22.6 million people, Asian Americans make up roughly 7% of the total U.S. population (United States Census 2020) but an estimated 10% of Asian Americans have diabetes, a rate comparable to that of general Americans as reported by the National Diabetes Statistics Report.
Asian Americans
Asian Americans are a diverse group with rich, varied, and complex immigration histories and cultures that contrast the popular yet inaccurate image as a monolithic, homogeneous racial/ethnic group. Representing over 2100 languages from 48 countries, Asian Americans are indeed a culturally diverse minority group (Tran 2020). Each sub-ethnic group underwent unique experiences as they were establishing themselves in the U.S., leading to their individuality as Asian Americans and underlines the need to view their data in disaggregated form. The 1965 Immigration and Nationality Act, which eliminated the discriminatory national-origins quota law and created an immigration preference based upon a system of skills-based jobs and unifying individuals with their U.S.-based family members (Chishti et al. 2015; Hing 1993), and the Indochina Migration and Refugee Assistance Act of 1975, created to give refuge to over 130,000 refugees from Vietnam, Kampuchea, and Laos who fled communist governments (Taylor 2013; Võ 2000), leading to an influx of Vietnamese, Cambodian, and Laotians to the U.S., changed the overall make-up of Asian Americans from predominantly Chinese and Japanese to one that includes over 20 countries in East and Southeast Asia and the Indian subcontinent (Budiman and Ruiz 2021; Lee 2015). The U.S. Asian American population has grown from 1 million prior to 1965 to close to 23 million today (Budiman and Ruiz 2021). Although Asian Americans have long been part of America’s history, today’s Asian American population largely consist of either immigrants, refugees, and/or their U.S. born children. The exception are Japanese Americans, a majority U.S. born population, many of whom can trace their ancestry to the early Issei—first generation Japanese Americans who came to the U.S. during 1885–1924 (Ichioka 1988). The top six groups today in terms of population size in the U.S. are Chinese, Asian Indian (also referred to as South Asian), Filipino, Vietnamese, Korean, and Japanese (Budiman and Ruiz 2021).
With over 2.3 million adult residents having been diagnosed with diabetes, 1.9 million of which is type 2 diabetes (California Department of Public Health 2020), California is home to roughly one-third of Asian Americans in the U.S. In fact, California has the largest number of Asian Americans according to the Pew Research Center (Budiman and Ruiz 2021). Asian Americans make up nearly 15% of California’s population at over 5.8 million, with approximately 27% Chinese, 22% Filipino, 14% Asian Indian/South Asian, 12% Vietnamese, 8% Korean, and 5% Japanese Americans (US Census Bureau 2016–2020).
Data disaggregation
Data disaggregation starting with the 2000 U.S. Census which separated Asian Americans and Pacific Islanders (Srinivasan and Guillermo 2000) have successfully been able to isolate unique disparities in these communities, catalyzing improvements in how services and programs are developed and delivered (Nguyen et al. 2013). Having disaggregated data helps researchers, health care providers, and policy makers fine tune cancer surveillance, screening, prevention, and treatment among Asian Americans and Pacific Islanders (Chen et al. 2004; Nguyen et al. 2014). It helps to isolate gaps and disparities in diverse issues such as tobacco use (Nguyen 2019), diabetes (Kanaya et al. 2011), victimization and delinquency (Le and Arifuku 2005), and academic/achievement gaps (Dolly Nguyen et al. 2015; Ngo and Sablan 2019)—all of which are important in better understanding the many facets of Asian American health.
Among Asian Americans alone, having disaggregated data means being able to look at the unique issues faced by Asian sub-ethnic groups, from the more populous groups such as the Chinese, Japanese, Vietnamese, and Filipinos, to the less populous groups, including Indonesians, Hmong, and Laotians. Collectively, Asian Americans are one of the most educated groups in the U.S.—more than half of Asian Americans (54%) age 25 years or older have a bachelor’s degree (National Center for Education Statistics [NCES] 2019). However, once separated into more specific sub-ethnic groups, the differences in educational attainment are quite alarming. Although a majority of Chinese, Korean, and Japanese American adults have a bachelor’s degree or higher (> 50%), only a small percentage of Bhutanese, Cambodians, Hmong, and Laotians have a bachelor’s degree (i.e., 10%, 16%, 18%, and 18%, respectively) (NCES 2019). Using data from the National Center for Health Statistics’ Multiple Cause of Death mortality files from 2003–2011, Hastings and colleagues (2015) identified different causes of death among several Asian American sub-ethnic groups. In their analysis, the team found that the leading cause of death among the collective Asian American group was cancer but once disaggregated, unique information emerged. Disaggregated data showed that heart disease was the leading cause of death among South Asian, Filipino, and Japanese men and that contrary to the information obtained from aggregated data, cancer is not the leading cause of death among South Asian women (Hastings et al. 2015).
The purpose of this paper is to identify the association between diabetes and the known risk factors for diabetes among Asian Americans and in doing so, differentiate the strengths of association between diabetes and the known risk factors across the top six Asian American sub-ethnic groups living in California. Ultimately, the results of this research will provide further evidence in support of data disaggregation, particularly among Asian Americans and health.
Methods
This study is a secondary analysis of health data from the California Health Interview Surveys (CHIS) collected and housed by UCLA’s Center for Health Policy Research. Conducted via telephone interviews, CHIS is the most comprehensive health survey in the state of California. Ten years (i.e., 2007–2016) of CHIS data were pooled, re-weighted, re-coded, and analyzed for this study.
Variables of interest
Diabetes was assessed using the CHIS variable (AB22) linked to the question “Has a doctor ever told you have diabetes?” with possible responses “yes”, “no”, and “borderline or pre-diabetes”. This variable was dichotomized by combining the “yes” category with the “borderline or pre-diabetes” category as the latter category yielded less than 1.75% of the sample. Racial/ethnic group categories were formed using three CHIS variables: the current Office of Management and Budget/Department of Finance race designation (OMBSRREO), the Latin/Hispanic subtypes variable (LATIN9TP), and the Asian 9 subtypes variable (ASIAN9). The newly created race variable used for analysis included the categories non-Hispanic White, non-Hispanic Black, and Mexican as well as Chinese, Japanese, Korean, Filipino, South Asian, and Vietnamese, the top six largest Asian ethnic groups in terms of sample size. Mexican rather than Latinx was identified as a race/ethnic category because (1) the Hispanic/Latinx population in California is overwhelmingly Mexican American (approximately 75–80% of Hispanics/Latinx in our CHIS data sample were Mexican Americans) and (2) as researchers advocating for data disaggregation for Asian Americans, it would be negligent to justify disaggregating all Asians to sub-ethnic groups, but not the Hispanic/Latinx population. For comparisons with non-Hispanic White, Black, and Mexicans, an “all Asian” race category was created by combining Chinese, Japanese, Korean, Filipino, South Asian, Vietnamese, and other Asian groups. Age and body mass index (BMI) were treated as continuous variables. Marital status was divided into four categories (1 = married; 2 = living w/ partner; 3 = widowed/separated/divorced; 4 = never married). Current smoking and high blood pressure were dichotomized (yes/no response). Similar to diabetes, high blood pressure was based on a question that asked respondents if a doctor ever told them they have high blood pressure. Because data on dietary intake was limited for the 10-year pooled sample, weekly fast food consumption was used as a proxy for diet/nutrition in the analysis.
Statistical analysis
Statistical analyses included age-adjusted diabetes prevalence rates and descriptive statistics for non-Hispanic White, non-Hispanic Black, Mexicans, Asian Americans as an aggregate group, as well as stratified by six Asian sub-ethnic groups. CHIS data were age-standardized to the 2010 U.S. Census for comparison of diabetes prevalence rates among the groups. To identify the association between diabetes and the various known risk factors, we conducted logistic regression analysis (Cox 1958) using diabetes as the dichotomous outcome. All programming code and analyses were conducted with STATA statistical software version 14.0 (StataCorp 2015).
Missing data and response rates
Since CHIS is a telephone survey and participants are allowed to skip questions they do not want to answer, missing data do exist and have been imputed by the CHIS data team prior to distribution for secondary data analysis. Overall, missing data are low but more sensitive questions had higher rates of missing data (California Health Interview Survey [CHIS] 2020). Survey completion rates or response rates varied across the different years of data collection. CHIS report a median response rate of 39.2% in 2007 (CHIS 2009), 37.7% in 2009 (CHIS 2011), 35% in 2011–12 (CHIS 2014), 31.4% in 2013–14 (CHIS 2016), 25.7% in 2015–16 (CHIS 2017), and 12.2% in 2017–18 (CHIS 2019).
Results
The final sample size for this study was close to a quarter of a million Californians (n = 223,926). This sample consisted of 139,792 non-Hispanic Whites, 10,284 African Americans, 27,116 Mexican Americans, and 21,267 Asian Americans.
Table 1 provides a detailed look at the basic demographic characteristics of the overall sample as well as the aggregated Asian American sample and disaggregated Asian American sample (i.e., Chinese, Japanese, Korean, Filipino, South Asian, and Vietnamese). Chinese Americans made up the bulk of the Asian American sample at 29% (n = 6186), followed by Vietnamese Americans at 18% (n = 3865), and Korean Americans at 15% (n = 3173). Mean age for the overall sample was 55.60 years although the mean age varied across the different ethnic groups. Japanese Americans had the highest mean age at 62.48 years and South Asians were the youngest at 43.09 years. With the exception of South Asians, a majority (> 50%) of the sample were female. Most of these individuals were also married, except for African Americans. Using body mass index cutoffs specifically adjusted for Asian Americans (Hsu et al. 2015; Suzuki et al. 2007), the average BMI for all Asian groups/categorization ranged from within healthy range (18.5–22.9) to above healthy range normal (23.0–26.9). Among the Asian American sample, Japanese Americans had the highest rates of high blood pressure at 45.90% versus South Asians who had the lowest rates at 19.30%. Of the Asian American sample, smoking rates were highest among Vietnamese Americans at close to 10% and mean fast food consumption was highest among Filipino Americans at 1.53 times per week.
Compared to other minority groups, Asian Americans, as an aggregated group, had lower rates of age-adjusted diabetes (11.31% compared to 17.11% in Mexican Americans and 13.06% in African Americans), but once disaggregated, the data tells a different story. Filipino Americans had the highest rates of diabetes at 15.69%, a rate that is higher than that of African Americans (13.06%) and slightly lower than Mexican Americans (17.11%), who have the highest rate of diabetes among the entire sample. At 14.34%, diabetes rates among South Asians are also higher than that of African Americans. Vietnamese Americans and Chinese Americans had the lowest rates of diabetes at 8.33% and 8.74%, respectively, a value that is still higher than that of their White counterparts (7.20%) (Tables 1, 2 and 3).
Association between diabetes and known risk factors
Among the aggregated Asian American group, no association existed between smoking and diabetes. As expected, those with high blood pressure and increasing body mass index had higher odds of having diabetes (OR = 2.51, 95% CI 2.01, 3.15) and (OR = 1.08, 95% CI 1.06, 1.10), respectively. Among non-Hispanic Whites and Mexicans, sex, age, never married, smoking, high blood pressure, and BMI were all associated with diabetes. Similar to Asian Americans, age, high blood pressure, and BMI were related to diabetes among African Americans.
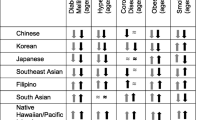
Disaggregated data among the Asian American group showed that the risk factors for diabetes varied among the six Asian American sub-ethnic groups. For Chinese Americans, age, marital status (i.e., never married), high blood pressure, and body mass index were significantly associated with diabetes. More specifically, increasing age and body mass index plus high blood pressure are risk factors for having diabetes among Chinese Americans but never marrying is a protective factor against diabetes (OR = 0.48 [0.24, 0.99]). Among Japanese Americans and Filipino Americans, age, high blood pressure, and body mass index were associated with diabetes. Most interestingly, having high blood pressure puts both of these groups at more than twice the odds of having diabetes as those who do not have high blood pressure (OR = 2.23 [1.09, 4.54] for Japanese Americans and OR = 2.82 [1.82, 4.36] for Filipino Americans). Although close to 10% of Vietnamese Americans in the sample were current smokers, smoking was not associated with diabetes, but age, marital status (i.e., never married), and high blood pressure were associated with diabetes. Among Korean Americans, age, marital status (i.e., living with a partner and never married), smoking, and body mass index were statistically significantly associated with diabetes. In fact, among Korean Americans, those who were current smokers had three times the odds of having diabetes compared to those who did not smoke (OR = 3.02 [1.43, 6.39]). Among South Asians, age, marital status (i.e., never married), and body mass index were associated with diabetes. In all cases, marital status, more specifically not being married, was protective against diabetes. Although Filipino Americans had high rates of weekly fast food consumption, no associations were seen between diabetes and fast food consumption among them or any other Asian American sub-ethnic groups.
Conclusion
Aggregated data masked the many nuances in regard to diabetes rates and related risk factors among Asian Americans in this sample. Using disaggregated data and looking specifically at sub-ethnic Asian American groups better quantifies diabetes rates among specific Asian Americans and also better isolates diabetes risk factors that are unique to each specific group. Our findings support the need for looking at data in disaggregated form and corroborates with previous research studies that have identified unique health challenges among Asian Americans. Looking at disaggregated data from over 2 million adult members of Kaiser Permanente in Northern California, Karter and colleagues, in the DISTANCE study, found high rates of diabetes among Filipino Americans and South Asian Americans being masked by lower rates among Chinese Americans and other ethnic groups (Karter et al. 2013). Additional evidence suggests high rates of diabetes particularly among Filipino Americans (Fuller-Thomson et al. 2017; Gomez et al. 2004). A cross-sectional survey conducted in Houston, Texas, found high prevalence of diabetes among Filipino Americans and suggests that Filipinos Americans are at a higher risk of developing diabetes than non-Hispanic Whites (Cuasay et al. 2001). It is important to note, however, that although Filipino Americans have one of the highest rates of diabetes among Asian Americans, people in the Philippines do not necessarily have one of the highest rates of diabetes in Asia (Ramachandran et al. 2012). Possible reasons for high rates of diabetes among Filipino Americans include high consumption of fat and meat (Vargas 2018) and adoption of western lifestyles (Araneta 2019). Among Chinese Americans, diet, reduced physical activity, and access to health care may be linked to diabetes (Varma et al. 2006) while low health literacy is a barrier to care post diagnosis (Leung et al. 2014). Medically underserved Chinese Americans are at an increased risk for diabetes and complications from diabetes because of poverty, limited English proficiency, and lack of culturally and linguistically tailored care (Ivey et al. 2012). Although national level data describes something different, the Agency for Healthcare Research and Quality (AHRQ) reported that Korean Americans have higher diabetes rates than non-Hispanic Whites (Islam et al. 2013). A combination of changes in diet, environment, physical activity, living arrangements, social relationships, and mental health are linked to diabetes among Korean Americans (Kim et al. 2015). Overall, existing evidence suggests a need to examine specific sub-ethnic groups in health research since Asian Americans should not be treated as one homogeneous group.
Limitations
Several limitations should be noted when reviewing the results of this analysis. First, the data used for this study was collected only among California residents and thus may not be generalizable to Asian Americans living in other parts of the U.S. CHIS is an extensive survey and can be time-consuming thus only a specific subset of individuals may have provided their data. Since data was collected over 10 years and pooled, there are some issues with missing data and the effects of time (e.g., the sample in 2006 may be different from the sample in 2016). Lastly, because we chose to pool 10 years of data and analyze it post hoc, the types of items on the CHIS over the span of 10 years was out of our control and thus we had to use whatever items were available for the 10-year time period as proxies for other behaviors (e.g., fast food consumption in place of dietary intake/behaviors).
Implications
The findings from this study highlight the importance of viewing data on a disaggregated level. More specifically, the authors of this manuscript encourage researchers, practitioners, and public health professionals to utilize disaggregated data in decision making surrounding Asian Americans and their health because we have seen and proven with data that they are not homogeneous. We encourage health professionals to develop more targeted approaches to prevention and management of diabetes among this diverse population.
Availability of data and material
The data underlying this article is part of the California Health Interview Survey and accessed from the University of California Los Angeles’ Center for Health Policy Research [https://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx]. Public Use Data Files can be obtained directly from the Center for Health Policy Research. Confidential Data files used for this secondary analysis may be shared upon reasonable requests.
References
Araneta MR (2019) Engaging the ASEAN diaspora: type 2 diabetes prevalence, pathophysiology, and unique risk factors among Filipino migrants in the United States. Journal of the ASEAN Federation of Endocrine Societies 34(2):126
Budiman A, Ruiz NG (2021a) Key facts about Asian Americans, a diverse and growing population. Retrieved from https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-americans/
California Department of Public Health (2020) Chronic Disease Control Branch: COVID-19 and Diabetes. Retrieved from https://www.cdph.ca.gov/Programs/CCDPHP/DCDIC/CDCB/pages/diabetesprevention.aspx
California Health Interview Survey (2009) CHIS 2007 methodology series: report 4 – response rates. UCLA Center for Health Policy Research, Los Angeles
California Health Interview Survey (2011) CHIS 2009 methodology series: report 4 – response rates. UCLA Center for Health Policy Research, Los Angeles
California Health Interview Survey (2014) CHIS 2011–2012 methodology series: report 4 – response rates. UCLA Center for Health Policy Research, Los Angeles
California Health Interview Survey (2016) CHIS 2013–2014 methodology series: report 4 – response rates. UCLA Center for Health Policy Research, Los Angeles
California Health Interview Survey (2017) CHIS 2015–2016 methodology series: report 4 – response rates. UCLA Center for Health Policy Research, Los Angeles
California Health Interview Survey (2019) CHIS 2017–2018 methodology series: report 4 – response rates. UCLA Center for Health Policy Research, Los Angeles
California Health Interview Survey (2020) CHIS 2019 methodology series: report 1 – sample design. UCLA Center for Health Policy Research, Los Angeles
CDC (2019) Type 2 diabetes. Retrieved from https://www.cdc.gov/diabetes/basics/type2.html
CDC (2020) National diabetes statistics report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services, pp 12–15. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Chen JY, Diamant AL, Kagawa-Singer M, Pourat N, Wold C (2004) Disaggregating data on Asian and Pacific Islander women to assess cancer screening. Am J Prev Med 27(2):139–145. https://doi.org/10.1016/j.amepre.2004.03.013
Chishti M, Hipsman F, Ball I (2015) Fifty years on, the 1965 Immigration and Nationality Act continues to reshape the United States. Retrieved from
Cox DR (1958) The regression analysis of binary sequences. J Roy Stat Soc: Ser B (methodol) 20(2):215–232. https://doi.org/10.1111/j.2517-6161.1958.tb00292.x
Cuasay LC, Lee ES, Orlander PP, Steffen-Batey L, Hanis CL (2001) Prevalence and determinants of type 2 diabetes among Filipino-Americans in the Houston, Texas metropolitan statistical area. Diabetes Care 24(12):2054–2058. https://doi.org/10.2337/diacare.24.12.2054
Dolly Nguyen BM, Hoa Nguyen M, Teranishi RT, Hune S (2015) The hidden academic opportunity gaps among Asian Americans and Pacific Islanders: What disaggregated data reveals in Washington State. https://files.eric.ed.gov/fulltext/ED573771.pdf
Fuller-Thomson E, Roy A, Chan KT-K, Kobayashi KM (2017) Diabetes among non-obese Filipino Americans: findings from a large population-based study. Can J Public Health, 108(1):e36-e42. https://doi.org/10.17269/CJPH.108.5761
Gomez SL, Kelsey JL, Glaser SL, Lee MM, Sidney S (2004) Immigration and acculturation in relation to health and health-related risk factors among specific Asian subgroups in a health maintenance organization. Am J Public Health 94(11):1977–1984. https://doi.org/10.2105/ajph.94.11.1977
Hastings KG, Jose PO, Kapphahn KI, Frank AT, Goldstein BA, Thompson CA, Eggleston, K, Cullen MR, Palaniappan LP (2015) Leading causes of death among Asian American subgroups (2003–2011). PloS one 10(4):e0124341. https://doi.org/10.1371/journal.pone.0124341
Hing BO (1993) Making and remaking Asian America through immigration policy. Stanford Press, Palo Alto
Hsu WC, Araneta MRG, Kanaya AM, Chiang JL, Fujimoto W (2015) BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care 38(1):150–158. https://doi.org/10.2337/dc14-2391
Ichioka Y (1988) The Issei: The world of the first generation Japanese immigrants, 1885–1924. Free Press, New York
Islam NS, Zanowiak JM, Wyatt LC, Chun K, Lee L, Kwon SC, Trinh-Shevrin C (2013) A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J Community Health 38(6):1030–1041. https://doi.org/10.1007/s10900-013-9711-z
Ivey SL, Tseng W, Kurtovich E, Weir RC, Liu J, Song H, . . . Hubbard A (2012) Evaluating a culturally and linguistically competent health coach intervention for Chinese-American patients with diabetes. Diabetes Spectrum, 25(2):93–102. https://doi.org/10.2337/diaspect.25.2.93
Kanaya AM, Adler N, Moffet HH, Liu J, Schillinger D, Adams A, Ahmed AT, Karter AJ (2011) Heterogeneity of diabetes outcomes among asians and pacific islanders in the US: the diabetes study of northern california (DISTANCE). Diabetes Care, 34(4):930–937. https://doi.org/10.2337/dc10-1964
Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, Kanaya AM (2013) Elevated rates of diabetes in Pacific Islanders and Asian subgroups: the Diabetes Study of Northern California (DISTANCE). Diabetes Care 36(3):574–579. https://doi.org/10.2337/dc12-0722
Kim MT, Kim KB, Huh B, Nguyen T, Han HR, Bone LR, Levine D (2015) The effect of a community-based self-help intervention: Korean Americans with type 2 diabetes. Am J Prev Med 49(5):726–737
Le TN, Arifuku I (2005) Asian and Pacific Islander youth victimization and delinquency: A case for disaggregate data. Amerasia J 31(3):29–42. https://doi.org/10.17953/amer.31.3.y1483q3v35045255
Lee C (2015) Family reunification and the limits of immigration reform: Impact and legacy of the 1965 Immigration Act. Paper Presented at the Sociological Forum. https://doi.org/10.1111/socf.12176
Leung AYM, Bo A, Hsiao H-Y, Wang SS, Chi I (2014) Health literacy issues in the care of Chinese American immigrants with diabetes: a qualitative study. BMJ Open 4(11):e005294
Lindström J, Tuomilehto J (2003) The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 26(3):725–731. https://doi.org/10.2337/diacare.26.3.725
NCES (2019) Indicator 27 Snapshot: Attainment of a Bachelor's or Higher Degree for Racial/Ethnic Subgroups. Retrieved from https://nces.ed.gov/programs/raceindicators/indicator_RFAS.asp
Ngo F, Sablan J (2019) Southeast Asian and Pacific Islander student progression through community college: a disaggregated transcript analysis. Teach Coll Rec 121(8):1–32. https://doi.org/10.1177/016146811912100807
Nguyen AB (2019) Disaggregating Asian American and Native Hawaiian and other Pacific Islander (AANHOPI) adult tobacco use: findings from wave 1 of the population assessment of Tobacco and Health (PATH) Study, 2013–2014. J Racial Ethn Health Disparities 6(2):356–363. https://doi.org/10.1007/s40615-018-00532-1
Nguyen AB, Chawla N, Noone A-M, Srinivasan S (2014) Disaggregated data and beyond: future queries in cancer control research. AACR. https://doi.org/10.1158/1055-9965.EPI-14-0387
Nguyen B-MD, Nguyen MH, Nguyen T-LK (2013) Advancing the Asian American and Pacific Islander data quality campaign: data disaggregation practice and policy. Asian American Policy Rev 24:55. Retrieved from https://libproxy.csun.edu/login?url=https://www.proquest.com/scholarly-journals/advancing-asian-american-pacific-islander-data/docview/1786882319/se-2
Ramachandran A, Snehalatha C, Shetty AS, Nanditha A (2012) Trends in prevalence of diabetes in Asian countries. World J Diabetes 3(6):110
Srinivasan S, Guillermo T (2000) Toward improved health: disaggregating Asian American and Native Hawaiian/Pacific Islander data. Am J Public Health 90(11):1731. https://doi.org/10.2105/2Fajph.90.11.1731
StataCorp (2015) Stata Statistical Software: Release 14. College Station, TX: StataCorp LP
Suzuki M, Murashima M, Hoerr SL & with the WHO Expert Consultation Panel (2007) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Nutr Diet 64:157–163
Taylor KB (2013) Indochina migration and refugee assistance act (1975). In C E Cortés, M A A m e (Ed.) (Eds.), Multicultural America: a multimedia encyclopedia, vol. 1. Sage, London, pp 1190–1191
Tran C (2020) Multifaceted: the cultural diversity of Asian America. Retrieved from https://www.kcet.org/shows/asian-americans/multifaceted-the-cultural-diversity-of-asian-america
US Census (2020) Asian American and Pacific Islander Heritage Month: May 2020. Retrieved from https://www.census.gov/newsroom/facts-for-features/2020/aian.html
US Census Bureau (2016–2020) American Community Survey 5-Year Estimates
Vargas P (2018) Dietary intake and obesity among Filipino Americans in New Jersey. J Environ Public Health, 2018
Varma R, Wen G, Jiang X, Hsu C, Torres M, Klein R, Azen SP, McKean-Cowdin R, Chinese American Eye Study Group (2016) Prevalence of diabetic retinopathy in adult Chinese American individuals: the Chinese American Eye Study. JAMA Ophthalmology 134(5):563–569
Võ LT (2000) The Vietnamese American experience: from dispersion to the development of post-refugee communities. In: Wu JY-WS, Song M (eds) Asian American studies: a reader. Rutgers University Press, New Brunswick, pp 290–305
Acknowledgements
The authors would like to acknowledge and thank the University of California Los Angeles’ Center for Health Policy Research and California State University, Northridge.
Funding
This research is supported through a grant from the National Institute of Minority Health and Health Disparities, National Institutes of Health R15 Academic Research Enhancement Award (Grant Number: 1R15MD011666-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMHD. Additional support for this research was funded by the National Institute of General Medical Sciences (NIGMS) BuildingInfrastructure Leading to Diversity (BUILD) Initiative, grant numbers TL4GM118977, UL1GM118976, and RL5GM118975. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIGMS.
Author information
Authors and Affiliations
Contributions
Patchareeya Pumpuang Kwan, Role: Writing – Original draft, Writing – Review and Editing.
Jonathan Watts, Role: Data curation, Methodology, Formal analysis.
Jamie Michelle Prudencio, Role: Writing – Review and Editing, Visualization.
Lawrence Chu, Role: Data curation, Methodology, Funding acquisition.
Danielle Erika Co, Role: Formal analysis, Writing – Review and Editing.
Edith Chen, Role: Conceptualization, Funding acquisition, Writing – Review and Editing.
Corresponding author
Ethics declarations
Ethics approval
The research presented here has been reviewed by the Institutional Review Board at California State University, Northridge. Based on the review, the Committee for Protection of Human Subjects has determined that the research referenced below does not meet the standards for generalizable human subjects research per 45 CFR 46, Sect. 102(e)(1).
Consent to participate
N/A
Consent for publication
N/A
Conflicts of interest
There are no conflicts of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kwan, P.P., Watts, J., Prudencio, J.M. et al. Differences in diabetes risk factors among Asian Americans. J Public Health (Berl.) 32, 1–8 (2024). https://doi.org/10.1007/s10389-022-01779-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-022-01779-z