Abstract
Aim
This study aimed to determine the predictors of fear-avoidance beliefs, pain, and disability indices in patients with chronic low back pain (LBP).
Subjects and Methods
A cross-sectional study was carried out on patients with chronic LBP attending the rheumatology outpatient clinics at Suez Canal University Hospital. Convenience sampling was used, and the main outcome measures were fear-avoidance beliefs, pain, and disability indices, which were measured using structured questionnaires.
Results
Mean age was 47 ± 13.4 years; mean body mass index (BMI) was 30.4 ± 5.47. Mean scores of the fear-avoidance belief questionnaire (FABQ)-total, FABQ-physical, FABQ-work, and Oswestry Disability Index (ODI) were 51.6 ± 16.1, 21.2 ± 5.8, 30.5 ± 11.4, and 42.35 ± 14.8, respectively, while median visual analog scale (VAS) score was 70 (50–80). There was a strong correlation among FABQ-total, VAS, and ODI; FABQ-P (r = 0.86, P < 0.01), FABQ-W (r = 0.96, P < 0.01), and ODI (r = 0.71, P < 0.01). According to multivariable linear regression analysis, the VAS scale (p = 0.01) and ODI (p < 0.01) were significantly associated with increased risk of FABQ-total. Similarly, FABQ-total (p < 0.01) was significantly associated with increased risk according to the ODI score.
Conclusions
A relationship was found among pain, disability, and fear-avoidance beliefs in patients with low back pain. Patients with a high level of fear of movement are more likely to have intense pain and disability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic lower back pain (LBP) is a common musculoskeletal disorder characterized by pain and discomfort for > 12 weeks in the posterior lumbar region between the 12th ribs and inferior gluteal folds (Chou et al. 2008).
Work loss and disability due to LBP affect approximately 16% and 34% of the general population, respectively (Ekman 2005).
A traditional biomedical model cannot illustrate the association between chronic pain and disability as it focuses on structural and biomechanical abnormalities. The biopsychosocial model is a better method to explain this because it includes psychological and social factors (Waddell 2004).
Many psychological factors such as fear, depression, anxiety, and a sense of helplessness often contribute to the development of chronic pain and associated disability (Samwel et al. 2006).
Fear leads to avoiding actual or perceived pain-generating physical activities, resulting in worsened performance and recovery after injury. Fear of pain is an important aspect of patients’ disability, which needs to be analyzed to achieve a successful outcome (Lundberg et al. 2011).
A fear-avoidance model (FAM) has been used to explain the development of pain experiences and behaviors. In this model, people evaluate their pain in relation to how it will affect the level of acquired fear and therefore subsequent avoidance of movement (Vlaeyen et al. 2001).
FAM proposes that during a musculoskeletal pain episode, anxiety and pain-related fear interact to determine whether an individual will resume normal activities (low psychological distress) or will avoid normal activities because of anticipation of increased pain and/or re-injuries (high psychological distress). The FAM suggests that high psychological distress is associated with poor clinical outcomes, potentially resulting in depressive symptoms, elevated pain intensity, greater physical impairments, and continued disability (Vlaeyen and Linton 2000).
This study aimed to determine the predictors of fear-avoidance beliefs, pain, and disability indices in patients with chronic LBP pain attending rheumatology outpatient clinics.
Methods
Design, setting, and time
This was a cross-sectional descriptive-analytic study. It was carried out between May 2018 and July 2018 in the rheumatology clinics of Suez Canal University Hospital.
Participants
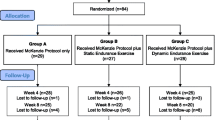
The study included 80 adult patients with chronic LBP. The sample size was calculated using the following formula (Dawson 2004):
Here, n = sample size, Zα/2 = 1.96 (the critical value that divides the central 95% of the Z distribution from the 5% in the tail), Zβ = 0.84 (the critical value that separates the lower 20% of the Z distribution from the upper 80%), and r = the correlation = 0.338 (Chung et al. 2013). The sample size was 66 cases. After adding a 20% dropout rate, it was 80 cases.
Inclusion criteria were: adult patients with chronic LBP were defined as those with pain and discomfort for > 12 weeks in the posterior lumbar region between the 12th ribs and inferior gluteal folds. Exclusion criteria were: patients with a recent history of trauma, structural deformity of the spine, previous or current cancer, pregnant women, and patients with mental or psychiatric disorders that might affect the reliability of their responses to the questionnaire.
Study tools
Data were collected using detailed history and clinical examination:
Personal history Age, gender, residence (rural or urban), occupation, smoking, and education level.
Medical history related to low back pain Duration of low back pain, pain radiation, surgery, and medication.
Pain intensity was measured with the visual analog scale (VAS), which consists of a 1–100-mm line on which subjects place a mark representing their pain intensity between the left side, representing “no pain,” and the right side, representing “the worst pain imaginable.” The VAS is a reliable measure of pain. Its internal consistency measured by intraclass correlation coefficients (ICCs) was 0.97 (Bijur et al. 2001).
Fear-avoidance beliefs were assessed using a modified form of the FABQ, a 16-item, self-report scale, which focuses specifically on patient’s beliefs about how physical activity and work affect their pain. It consists of two subscales: FABQ-physical activity (FABQ-P) assesses attitudes and beliefs related to general physical activities (five items, range 0–30); FABQ-work (FABQ-W) assesses attitudes and beliefs related to occupational activities (eleven items, range 0–66). For both subscales, a low score indicates low fear-avoidance beliefs (Willims 2006). A reliable Arabic version is available and has been validated. The internal consistency of the Arabic version, measured by Cronbach’s alpha, is 0.73 (Alanazi et al. 2017).
The disability index of LBP was evaluated using the modified Oswestry Disability Index (ODI). The modified ODI is a ten-area questionnaire measuring pain and disability in individuals with LBP. These ten areas are pain intensity, personal care, lifting, walking, standing, sleeping, sex life, social life, and travel (Fairbank et al. 1980). A reliable Arabic version is available and has been validated. The internal consistency of the Arabic version, measured by Cronbach’s alpha, is 0.99 (Algarni et al. 2014).
Main variables were fear-avoidance beliefs, pain, and disability indices in patients with chronic LBP.
Statistical analysis
The results were analyzed using SPSS version 22. Both parametric and non-parametric tests were used for analysis, and normal distribution of the continuous data was checked using the Shapiro-Wilk test. For the descriptive statistics, normally distributed data were expressed by mean and standard deviation, and non-normally distributed data were presented as median and interquartile range. For inferential statistics, a correlation was explored among pain, disability, and the FABQ scores as well as the other variables using Pearson or Spearman tests. Multivariable linear regression analysis was used to assess predictors of FABQ-T, ODI, and VAS. P ≤ 0.05 was set as a criterion for establishing statistical significance.
Ethical considerations
The institutional review board (IRB) approved the study.
Results
The study was conducted on 80 patients with a response rate of 100%. Patients’ age was 47 ± 13.4 years old, and 54 (67.5%) were female. BMI was 30.4 ± 5.47 kg/m². Thirty-seven (46.3%) of the patients were unemployed. Median (range) LBP duration was 4 (2–7) years. Forty-nine (67.3%) patients had radiating pain, only 1 patient had a history of surgery, and 47 (58.8%) patients were on medications (Table 1).
The mean scores of FABQ total, FABQ-P, FABQ-W, and ODI were 51.6 ± 16.1, 21.2 ± 5.8, 30.5 ± 11.4, and 42.35 ± 14.8, respectively, while the median VAS was 70 (50–80) (Table 2).
Regarding the correlation among FABQ, VAS, and ODI, FABQ-P (r = 0.86, P < 0.01), FABQ-W (r = 0.96, P < 0.01), and ODI (r = 0.71, P < 0.01) showed a significant strong correlation with FABQ-total, while VAS (r = 0.5, P = 0.017) showed positive significant moderate correlation with FABQ-total. Regarding correlation between the ODI scale and other variables, FABQ-P (r = 0.64, P < 0.01), FABQ-W (r = 0.66, P < 0.01), and VAS (r = 0.51, P < 0.01) showed significant moderate correlation with ODI (Table 3).
Multivariable linear regression analysis was used to assess predictors of FABQ-total: R² = 0.513, where 51.3% of the variability of FABQ-total can be explained by this linear model. The VAS scale and ODI were statistically significant independent positive predictors of FABQ-total, where, for every 10-point increase in the VAS scale, there is a 2.46-point increase in the FABQ-total score. Also, for every 10-point increase in the ODI score, there is a 5.39-point increase in the FABQ-total score (Table 4).
Multivariable linear regression analysis was used to assess predictors of the ODI score. R2 = 0.577, where 57.7% of the variability of ODI can be explained by this linear model. FABQ-total was a statistically significant independent positive predictor of the ODI score (P < 0.01), where, for every 10-point increase in FABQ-total, there is a 4.68-point increase in the ODI score. Otherwise, no other factors significantly affected the ODI score (Table 5).
Multivariable linear regression analysis was used to assess predictors of VAS: R2 = 0.298, where 29.8% of the variability of VAS can be explained by this linear model. FABQ-total was a statistically significant independent positive predictor of VAS (P = 0.015), where for every 10-point increase in FABQ-total, there is a 3.48-point increase in the VAS score. Otherwise, no other factors significantly affected the VAS score (Table 6).
Discussion
Multivariable linear regression analysis showed that the FABQ-T score was significantly associated with high ODI and VAS scores. This shows that disability is strongly associated with how individuals interpret their pain.
This result shows that chronic pain does not necessarily lead to disability, and how the individual perceives the pain is most important. In line with this result, regression analysis was used in a study on 184 chronic low back pain patients to test the role of both self-efficacy and fear-avoidance beliefs in mediating the relationship between pain and disability. Both were found to mediate the effects of pain intensity on disability at the onset of chronic low back pain (Costa et al. 2011). Similarly, Nava-Bringas et al. (2017) found that the total FABQ score was a determinant of disability evaluated with the Roland Morris Questionnaire.
The present study showed that the FABQ-total score was 51.6 ± 16.1. This high score can be explained by the increased degrees of pain and disability among our subjects represented by a median VAS score of 70 (IQR 50–80) and mean ODI score of 42.35 ± 14.8.
This score was close to the results of the study by Chung et al. (2013), which reported a mean score of 39.2 ± 11, and the study by de Moraes Vieira et al. (2014), which reported a mean of 42 ± 11.5. However, it was not consistent with the results of the study by Guclu et al. (2012), which reported a mean of 29.47 ± 13.44. A possible explanation for this inconsistency is the high degrees of pain and disability among our subjects.
Regarding the FAB-physical activity score, our study reported a mean score of 21.2 ± 5.8, which was not consistent with the results of the study by Chung et al. (2013) in which the mean FAB-physical activity score was 15.6 ± 4.8, and the results of the study by Guclu (2012) and colleagues, which reported a mean FAB-physical activity score of 14.57 ± 6.25. The high mean age of our subjects (47.7 ± 13.4 years) might have affected the degree of physical activity compared with the lower mean age of other studies.
Regarding the FAB-work score, we reported a mean score of 30.5 ± 11.4, which was similar to the results of the study by Chung et al. (2013), which reported a mean score of 24.1 ± 7.7. However, it was different from the study of Guclu et al. (2012), which reported a mean score of 15.19 ± 9.69. This inconsistency could be explained by the higher percentage of unemployed subjects in our sample with 46.3%.
In the current study, we reported the degree of disability using the Oswestry Disability Index (ODI) with a mean score among our subjects of 42.35 ± 14.8. These results were different from those of the study by Chung (2013) and colleagues in which the mean ODI score was 32.5 ± 12.2. This could be explained by our rather old population with a high mean age (47.7 ± 13.4 years). Besides, the high BMI (30.4 ± 5.47) as well as the severity of pain manifested, as represented with high VAS scores [70 (IQR 50–80)], might have negatively influenced the degree of disability.
There was a significant positive correlation between fear-avoidance beliefs of patients, as measured by FABQs, and both pain, as measured by the VAS score, and disability, as presented by the ODI Index. The increased disability score in patients with high FABQ scores was expected, as patients prefer to limit their movements, fearing pain.
These findings were consistent with the results from previous studies; for example, in another cross-sectional study on 80 chronic low back pain patients, Nava-Bringas (2017) and colleagues found a positive correlation between functional disability, measured by the Roland-Morris scale, and high FABQ scores. These correlations were found with the total score as well as with the physical activity and work subscales. In a similar study assessing the relationship between physical capacity and fear-avoidance beliefs in patients with chronic low back pain, Lee et al. reported that there was a significant correlation between the measures of physical capacity and the FABQ-W. Additionally, they found an increase in pain intensity related to higher scores on the FABQ-P, leading to less activity, which further contributes to the severity of pain (Lee and Park 2017). Also, another study on 55 patients reported that the ODI score showed a significant correlation with FABQ-W (r = 0.376, P = 0.005), FABQ-total (r = 0.338, P = 0.011), and VAS (r = 0.494, P = 0.000) (Chung et al. 2013).
Based on the results of our multivariate analysis, this study suggests screening for fear-avoidance beliefs in patients with low back pain may be useful to identify patients at risk of psychosocial problems as well as pain intensity and physical impairment. Patients with high fear of movement are more likely to have intense pain and disability; therefore, the focus of the therapy for these patients should be to desensitize them about performing movements and increase their exercise.
Limitations of the study
Since this is a cross-sectional study, it is difficult to ascertain causation and to establish the causal relationship between factors associated with fear-avoidance belief. Inclusion criteria included the patients who agreed to participate, which may cause volunteer bias; also, the study was carried out in rheumatology clinics, which could cause selection bias as many patients with low back pain may seek other levels of care with a different presentation of study factors, affecting the generalizability of the results.
Conclusion
This study suggests that there is a considerable relationship among pain severity, FABQ scores, and functional disability. Screening for fear-avoidance beliefs in patients with LBP can be useful for the identification of patients at risk of psychosocial problems and physical impairment. Patients who are very afraid of movement are more likely to have intense pain and disability; therefore, the focus of the therapy for these patients should be to desensitize them about performing movements and increase their exercise capabilities.
References
Alanazi F, Gleeson P, Olson S, Roddey T (2017) Translation and validation of the Arabic version of the fear-avoidance beliefs questionnaire in patients with low Back pain. Spine 42(7):411–416
Algarni AS, Ghorbel S, Jones JG, Guermazi M (2014) Validation of an Arabic version of the Oswestry index in Saudi Arabia. Ann Phys Rehabil Med 57(10):653–663
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for the measurement of acute pain. Acad Emerg Med 8:1153–1157
Chou R, Qaseem A, Snow V (2008) Low Back pain guidelines panel. Diagnosis and treatment of low back pain for the clinical efficacy assessment Subcommittee of the American College of physicians. Am Pain Soc Ann Intern Med 148(3):247–248
Chung EJ, Hur YG, Lee BH (2013) A study of the relationship among fear-avoidance beliefs, pain, and disability index in patients with low back pain. J Exerc Rehabil 9(6):532–535
Costa LDCM, Maher CG, McAuley JH, Hancock MJ, Smeets RJEM (2011) Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. Eur J Pain 15(2):213–219
Dawson B (2004) Trapp RG basic & clinical biostatistics (4th ed). LANGE Basic Sci
De Moraes Vieira ÉB, De Góes SM, Damiani LP, De Mattos Pimenta CA (2014) Self-efficacy and fear avoidance beliefs in chronic low back pain patients: coexistence and associated factors. Manag Nurs 15(3):593–602
Ekman M, Johnell O, Lidgren L (2005) The economic cost of low back pain in Sweden in 2001. Acta Orthop 76:275–284
Fairbank JC, Couper J, Davies JB, O'Brien JP (1980) The Oswestry low-back pain disability questionnaire. Physiotherapy 66(8):271–273
Guclu DG, Guclu O, Ozaner A, Senormanci O, Konkan R (2012) The relationship between disability, quality of life and fear-avoidance beliefs in patients with chronic low back pain. Turk Neurosurg 22(6):724–731
Lee J, Park S (2017) The relationship between physical capacity and fear-avoidance beliefs in patients with chronic low back pain. J Phys Ther Sci 29(10):1712–1714
Lundberg M, Grimby-Ekman A, Verbunt J, Simmonds MJ (2011) Pain-related fear: a critical review of the related measures. Pain Res Treat 494196
Nava-Bringas TI, Macías-Hernández SI, Vásquez-Ríos JR, Coronado-Zarco R, Miranda-Duarte A, Cruz-Medina E, Arellano-Hernández A (2017) Fear-avoidance beliefs increase the perception of pain and disability in Mexicans with chronic low back pain. Rev Bras Rheumatol 57(4):306–310
Samwel HJ, Ever AW, Crul BJ, Kraaimaat FW (2006) The role of helplessness, fear of pain, and passive pain-coping in chronic pain patients. Clin J Pain 22:245–251
Vlaeyen JW, Linton SJ (2000) Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 85:317–332
Vlaeyen J, De Jong J, Geilen M, Heuts PH, Van Breukelen G (2001) Graded exposure in vivo in the treatment of pain-related fear: a replicated single-case experimental design in four patients with chronic low back pain. Behav Res Ther 39:151–166
Waddell G (2004) The biopsychosocial model. In: Waddel G (ed) The back pain revolution. Churchill Livingston, Edinburgh, pp 265–282
Williams E (2006) Fear Avoidance Behavior Questionnaire. Aus J Physiot 52:149
Acknowledgments
the research team would like to acknowledge all the participants and the health care team in the rheumatology clinics for their cooperation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were following the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salama, H.M., Reda, N., El Shahaly, M. et al. Predictors of fear-avoidance belief, pain, and disability index in patients with chronic low back pain attending rheumatology outpatient clinics. J Public Health (Berl.) 30, 417–422 (2022). https://doi.org/10.1007/s10389-020-01296-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-020-01296-x