Abstract
Introduction
The American Society of Anesthesiologists (ASA) physical status classification system was developed as a simple categorization of patients’ physiological status that predicts the operative risk. Peroral endoscopic myotomy (POEM) is a less invasive alternative to surgical myotomy in achalasia. As such, POEM seems to be an appealing option for high-risk patients with achalasia. However, there are no studies which systematically analyzed the outcomes of POEM among patients with different ASA classes. Hence, we aimed to compare the safety and efficacy of POEM in patients with lower and higher ASA classes.
Methods
Medical records of all achalasia patients who underwent POEM at our institution between April 2014 and May 2019 were reviewed. Patients were categorized arbitrarily into two groups, lower ASA class (ASA I and II combined) and higher ASA class (ASA class III and IV combined). Demographic and procedural details, timed barium swallow (TBE), high-resolution esophageal manometry (HREM), pH study findings and Eckardt scores were compared between the two groups. Baseline characteristics were compared using Chi-square test and two-sample t-test for categorical and continuous variables, respectively.
Results
A total of 144 patients met our study criteria (lower ASA class, n = 44; and higher ASA class, n = 100). Patients in higher ASA class were significantly more obese and older. More patients in lower ASA class had prior Heller myotomy and more patients in higher ASA Class had prior botulinum toxin injections. Procedural parameters were similar in both groups. Procedural complications were infrequent and were also similar in the two groups. The length of stay, 30-day readmission rate, reflux symptoms and esophageal pH study findings were also comparable between the two groups. Treatment success was similar in both groups, 97.7% in lower ASA class versus 92% in higher ASA class (p = 0.19). At 2-month follow-up, both groups had significant improvement in HREM and TBE parameters.
Conclusion
POEM is a very safe and highly effective treatment option for achalasia patients with advanced ASA class similar to lower ASA class patients. POEM may be considered as the preferred choice for myotomy in these high-risk achalasia patients due to its low morbidity and high efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The natural orifice transluminal endoscopic surgery [1] (NOTES) led to emergence of peroral endoscopic myotomy (POEM) as an incision-less alternative to laparoscopic Heller myotomy (LHM) in achalasia. Large metanalyses [2,3,4,5] and a recent randomized controlled trail [6] have suggested similar or non-inferiority of POEM over LHM in achieving excellent esophageal drainage and palliation of symptoms in patients with achalasia. Based on these impressive results, POEM has now joined the main stream treatment armamentarium for achalasia including endorsement in some society guidelines [7, 8].
Multiple factors such as age, subtype of achalasia, coexisting comorbid conditions, body mass index (BMI), physical status, life expectancy are among the factors considered while selecting one treatment modality over another for achalasia patients. One such factor is the operative risk assessment, which plays a crucial role in estimating the post-procedural morbidity and mortality. There are various models for evaluating the preoperative anesthetic risk in patients undergoing invasive procedures [9]. Among them, the American Society of Anesthesiologists' physical status (ASA-PS) classification is one of the most widely accepted and universally validated scoring systems for predicting the operative risk [10]. This includes an effortless categorization of a patient's baseline health status, which thereby reflects the postoperative course and outcomes [11]. It consists of five classes (I–V), ranging from a normal healthy patient (class I) to a moribund patient who is not expected to survive (class V). The utility of the ASA-PS is to convey the risk associated with any procedure that requires anesthesia, with respect to the patient’s underlying systemic illnesses.
The ASA-PS has been reported to correlate with the anesthetic morbidity and peri-procedural outcomes in various surgical studies thus far. Nearly five decades ago, a landmark study by Vacanti et al. [12] suggested that increasing ASA-PS class is associated with higher morbidity and mortality after surgery. These findings were reaffirmed by another recent large multi-institutional cohort study that reported a strong association between higher ASA-PS and increased mortality within 48 h of administering an anesthetic, for both elective and emergent procedures [13]. As such, considering the high morbidity associated with a higher ASA class, it is a general tendency among clinicians to choose less invasive therapies for achalasia patients belonging to ASA class III and above.
Consequently, patients with higher ASA class are less likely to undergo surgical myotomy in achalasia due to a perceived higher risk of complications. In addition to the remarkable efficacy, one of the significant advantages of POEM over LHM is its minimal invasiveness and lack of the traditional surgical operative risks as one would expect with a thoracic surgery like LHM. Based on these factors, one could assume POEM to be a safer choice in high-risk patients. However, there have been no studies thus far which evaluated the safety of POEM in achalasia patients belonging to different ASA classes. Hence, we aimed to compare the feasibility and outcomes of POEM among patients with lower and higher ASA classes.
Materials and methods
This study was approved by the Institutional Review Board at the Cleveland Clinic. We conducted a retrospective chart review of our prospective registry of all achalasia patients who underwent POEM at our institution between April 2014 and May 2019. A total of 144 patients were included and were divided into two arbitrary groups based on their ASA class: lower ASA group (ASA classes I and II combined) and higher ASA group (ASA classes III and IV combined). All included patients had high-resolution esophageal manometry (HREM), timed barium esophagram (TBE) performed before and 2 months after POEM along with an esophageal pH study as part of our standard clinical protocol. Patient demographics, prior treatments, pre, and 2 months post-treatment TBE and HREM parameters, 24 h esophageal pH study findings and Eckardt scores were compared between the two groups. Treatment success was defined as reduction of Eckardt score to ≤ 3. We performed POEM procedure, TBE, HREM and 24 h esophageal pH studies as per our institutional protocol as we described in our previous studies [14].
POEM procedure
All POEM procedures were performed under general anesthesia in an operating room using standard steps. The steps included (1) creation of a submucosal tunnel starting approximately 10–12 cm proximal to the LES (lower esophageal sphincter) and extending distally to about 2–4 cm onto the gastric side. This was typically performed on the anterior esophageal wall except in post-Heller patients in whom it was created on the posterior esophageal wall; (2) myotomy of the circular muscle fibers starting 3–4 cm distally from the mucosal entry site and 2–4 cm into the gastric wall; and (3) closure of the mucosal entry site using endoscopic clips. The next day, patients underwent a water-soluble contrast swallow radiograph to exclude transmural perforations. If the swallow study was unremarkable, patients were started on a clear liquid diet, discharged home, and were advised to advance diet gradually over the next 1–2 weeks.
HREM procedure
HREM was performed by using the following protocol: a 36-channel, solid-state catheter system with high-fidelity circumferential sensors at 1-cm intervals was advanced through the nasal canal (Sierra Scientific Instruments Inc., Los Angeles, CA, United States). Pressure data of 10- and 5-mL swallows of water were recorded and analyzed by using a dedicated computerized analysis system. All relevant parameters were analyzed according to the Chicago classification. Diagnostic criteria for achalasia were incomplete relaxation of LES (IRP > 15 mmHg) and aperistalsis of the esophageal body. Achalasia was classified into; type I if there was 100% aperistalsis without esophageal pressurization, type II if there was pan-esophageal pressurization > 30 mmHg in ≥ 20% of swallows and as type III when there were premature contractions in ≥ 20% of swallows.
TBE procedure
Patients were instructed to drink the maximum volume of dilute barium sulfate contrast (45% weight in volume) that they could tolerate without regurgitation or aspiration (between 100 and 250 mL) over 30–45 s. With the patient in an upright position, radiographs of the esophagus were taken at 1- and 5-min intervals after the last swallow. The height and width of the barium column were measured using a calibrated ruler and were recorded.
24-h esophageal pH study
Patients underwent a transnasal catheter-based 24-h pH study while staying off proton pump inhibitors (PPI) and other acid-reducing medications, 2 months after the POEM procedure. Abnormal pH study was defined as either DeMeester score > 14.72 or total abnormal acid exposure time > 5.5% (i.e., esophageal pH < 4 for greater than 5.5% of the time). We also looked at other pH study parameters, including abnormal esophageal acid exposure time (AET) in the post-prandial state (abnormal if > 6.8%), upright position (abnormal if > 8.2%), and supine position (abnormal if > 3%).
GERD symptoms and Eckardt scores
The presence or absence of GERD symptoms and Eckardt symptom scores were recorded at the time of clinical follow-up visits, typically 2 months after POEM.
ASA categorization
The ASA physical status classification system was used to assess the fitness of our patients prior to POEM [15]. The ASA class of the patients was documented by the anesthesia team prior to surgery as part of their standard documentation. It includes a six -category physical status classification system as follows: I—healthy person, II—mild systemic disease, III—severe systemic disease, IV—severe systemic disease that is a constant threat to life, V—a moribund person who is not expected to survive without the operation and VI—a declared brain-dead person whose organs are being removed for donor purposes.
Statistical analysis
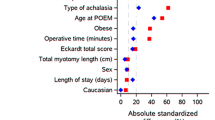
Continuous variables were presented as median (25th, 75th percentiles) and categorical variables as counts and frequency. Univariable analysis was performed to assess differences between the treatment groups. Two sample t-test was used to compare means and Kruskal–Wallis test was used to compare medians of continuous variables. Wilcoxon signed rank test was used to compare pre- and post-procedure median of continuous variables. Pearson’s Chi-square tests were used to compare categorical variables, and Fisher’s exact test was used for counts less than five. All statistical analyses were performed using R foundation for statistical computing (R version 3.5.3; Vienna, Austria), and a P value < 0.05 was considered as statistically significant.
Results
Baseline characteristics
A total of 144 patients were included in the final analysis, of which 100 patients belonged to higher ASA group (Class III–IV). Baseline patient characteristics are summarized in Table 1. The median age in the lower ASA group was 54 years (Quartile (Q)1–3: 19.8–73.0), while in the higher ASA group was 64.6 years (Q1–3: 25.2–87.4). A higher number of patients were ≥ 65 years in higher ASA group compared to the lower ASA group (50 vs. 15.9%, p = 0.0001). There were no significant differences in gender distribution between the two groups. Patients in higher ASA group had greater BMI (28.6 vs. 26.7 kg/m2, p = 0.034) compared to lower ASA patients. The mean follow-up duration was 2.6 months after POEM.
Achalasia characteristics
The distribution of achalasia subtypes and median integrated relaxation pressures (IRP) were similar in both groups (Table 1). Pre-POEM TBE parameters were also similar in the two groups. Patients in lower ASA group were more likely to have had prior Heller myotomy compared to the higher ASA group (36.4 vs. 12%, p = 0.0007). Conversely, patients in the higher ASA group had more prior botulinum toxin injections (29 vs. 11.4%, p = 0.022). The duration of the disease was similar between the lower and higher ASA patients (4 vs. 3 years, p = 0.71). The severity of symptoms as measured by Eckardt scores was also similar in both groups (Table 1).
POEM peri-procedural findings and adverse events
There were no significant differences in operative time (100 vs. 87 min, p = 0.08) and total myotomy length (9 vs. 9 cm, p = 0.47) between the lower and higher ASA groups, respectively. However, the lower ASA patients had a greater number of posterior myotomy performed than the higher ASA patients (36.4 vs. 12%, p = 0.0007), due to higher prior LHM in that group. The median length of stay was one day in both the lower and higher ASA groups (p = 0.06).
There was a significant difference in the number of post-procedural complications among patients in lower and higher ASA groups. Complications occurred in four patients in lower ASA (4/44, 9.1%) and one patient in higher ASA group. (1/ 100, (1%) (p = 0.015). Mucosal perforation occurred in a total of 3 patients (2 in lower ASA group and 1 in higher ASA group); 2 of these patients underwent endoscopic treatment with clips while 1 patient was treated conservatively with nasogastric tube placement due to the friable nature of the perforation from the effect of cautery precluding clip placement. One patient in the lower ASA group presented with delayed gastrointestinal bleeding from mucosal ulceration in lower esophagus. He underwent conservative treatment with delayed oral intake for 3–4 days. Another patient in the lower ASA group had a mucosal injury that did not require any intervention following the procedure. Subsequently, oral intake was initiated after mucosal healing was confirmed with upper endoscopy. There were no other adverse events or complications. Thirty-day readmissions were infrequent and were similar in the two groups (6.6 vs. 6%, p = 0.85).
Post-POEM findings
At 2 months, both groups had similar rates of treatment success, defined as an improvement of Eckardt score to ≤ 3 (97.7 vs. 92%, p = 0.19) (Table 2). Improvement in the TBE column height at 1 min was comparable between the lower and higher ASA groups (3.25 vs. 4.5 cm, p = 0.58). Similarly, the improvement in TBE column height at 5 min was also not significantly different between the two groups (4.55 vs. 4.15 cm, p = 0.91). There were similar improvements in LES-IRP in both lower and higher ASA groups (24.90 vs. 24.40 mmHg, p = 0.85). Post-POEM, greater number of patients in higher ASA group reported GERD symptoms compared to lower ASA patients, although not statistically significant (18 vs. 6.8%, p = 0.08). Abnormal DeMeester scores (> 14.72) were also not significantly different between the two groups (55.9 vs. 55.1%, p = 0.94). The improvements in Eckardt score and LES-IRP at 2 months post-POEM when compared to baseline are depicted in Figs. 1 and 2, respectively.
Discussion
This study evaluated the safety and efficacy of POEM in achalasia patients and showed that it is very safe with similar and high success rates in both lower and higher ASA class patients. POEM was highly efficacious in achieving symptom relief along with remarkably low peri-procedural adverse events in both the groups. Improvement in TBE parameters and LES-IRP on esophageal manometry following POEM was also comparable in the two groups.
Treatment of achalasia is aimed at palliation of symptoms by relieving LES pressure, since there is no cure. Among the available options, LHM and POEM have emerged as preferred and popular treatments to relieve the lower esophageal sphincter pressure effectively [3]. Since its introduction in 2010, numerous studies have demonstrated the efficacy of the endoscopic incision-less myotomy (POEM) in a wide variety of achalasia patients [16,17,18,19,20]. A recent multicenter randomized controlled trial by Werner et al. [6] in 221 patients with achalasia suggested that POEM was non-inferior to LHM in achieving technical success and symptomatic relief at a 2-year follow-up. The main drawback of POEM is the associated higher risk of clinically relevant GERD when compared with LHM [3, 20, 21]. However, many studies have also suggested complete subjective and objective resolution of GERD following POEM with the use of acid-reducing proton pump inhibitors [5, 20,21,22]. Additionally, the long-term clinical consequences of this pathologic acid reflux following POEM are also incompletely understood [23,24,25]. Based on these observations, many experts across the globe recommend POEM as an effective therapy for achalasia [7, 8].
The preoperative evaluation for achalasia patients routinely includes a pre-anesthetic assessment to gauge the patients coexisting comorbid conditions, perioperative risk, and readiness for the planned procedure. The ASA-PS classification is commonly used by clinicians, anesthesiologists, and surgeons to define a patient's overall health status. Although the ASA-PS was not primarily devised to evaluate operative risk, it is still widely used for this purpose. Studies have shown that a higher ASA-PS is associated with an increased rate of perioperative complications, total length of hospital stay, unforeseen hospital or ICU admissions and even higher mortality following ambulatory surgery [26,27,28,29,30,31,32]. ASA-PS also correlates well with the Charlson Comorbidity Index and the Revised Cardiac Risk Index, the other well-validated scoring systems used for functional status evaluation before surgery [26, 32]. Thus, it a general tendency of surgeons to prefer less invasive options like medical therapies or endoscopic options such as botulinum toxin or pneumatic dilation for achalasia patients with higher ASA class. This hypothesis corroborates with our analysis as great majority of patients with a higher ASA class were either untreated or had simple endoscopic treatments such as botulinum toxin injections. Only 12% underwent prior LHM in higher ASA class group compared to 36.4% in the lower ASA group. Strikingly, even the recent randomized controlled trial comparing the efficacy of endoscopic (POEM) and surgical myotomy (LHM) included fairly healthy individuals with limited information on the patient's baseline comorbid conditions or ASA classification (6). As such, ours is the first study to analyze the risk and benefit of POEM in the high-risk patients belonging to higher ASA class in comparison to the healthier lower ASA class patients.
Multiple studies including a recent meta-analysis suggested a notable age difference among patients undergoing POEM as compared to LHM with patients in the POEM groups being significantly older than those in the LHM groups [33,34,35,36,37]. Although, there are no studies that directly evaluated the efficacy of LHM and POEM in achalasia patients with higher ASA class, the reported disparity in age and coexisting comorbid conditions among patients being referred for POEM and LHM, suggests a general tendency of physicians to offer less invasive treatments to patients who are older and belonging to higher ASA class. Our study findings also corroborated that observation, since the patients in higher ASA group were significantly older than lower ASA group (64.6 vs. 54 years, p = 0.004). It is also interesting to note that majority of the patients in our study belonged to higher ASA group compared to lower ASA class (100 vs. 44 patients). Although, there was no formal treatment protocol/strategy at our institution regarding selecting patients for either LHM or POEM based on ASA class, there might be a selection bias towards opting for POEM in higher ASA class patients.
This is the first study to analyze the risk and benefit of POEM in the high-risk patients belonging to higher ASA class in comparison to the healthier lower ASA class patients. The important health care outcomes such as operative time, hospital length of stay and 30-day readmission rate and mortality were not significantly different among our patients with higher and lower ASA classes. Interestingly, the peri- and post-procedural adverse events such as gas-related complications, mucosal injury or perforation were comparable between patients belonging to higher and lower ASA class. The incidence of GERD as measured by the total abnormal acid exposure time on 24-h study was also similar in both groups. However, there was a trend toward higher number of patients reporting GERD symptoms in high ASA group compared to low ASA group, but it did not reach statistical significance (18 vs. 6.8%, p = 0.08), likely due to small sample size.
All the POEM procedures in this study were performed by only two providers, minimizing the variations in technical expertise and experience between operators. Despite being a retrospective study, both the groups in our study were similar with regard to clinical, radiological, and manometric findings, arguing against a wide variation in the severity of achalasia. All our manometric tracings were reported based on the current Chicago classification version 3.0 and limits era-based confounding. We found no significant difference in the occurrence of GERD between the two study groups despite using an AET cut-off of > 4.5% [38] for reporting clinically relevant GERD, which is quite lower than the recommended threshold by the Lyon consensus (AET value of > 6%) [39].
This study has some limitations. The retrospective nature of this study often carries the risk of inherent bias as it is often challenging to capture accurate information through a mere chart review. Importantly, the median follow-up duration of our study was relatively short, and long-term outcomes are yet to be explored in these high-risk patients. Some relevant results, such as adverse events, may not be recorded entirely in a retrospective study. This study was conducted in a tertiary care center with high expertise in POEM procedures. Our study subjects represent a typical patient population seen at tertiary care centers with higher percentage of patients with one or more previous treatments for achalasia and longer duration of illness. Thus, our results may not be widely applicable to smaller institutions that are in the initial stages of performing POEM. Lastly, although it would be ideal to compare outcomes of POEM vs. LHM in both lower and higher ASA class patients, we do not have that data and it is beyond the scope of this study.
Our study adds to the growing body of literature that POEM in highly effective and safe in various achalasia patients. Our study demonstrated excellent outcomes after POEM with a significant reduction in symptom scores and esophageal obstruction (as measured by manometry and barium swallow) even in the high-risk population (ASA class III and above). However, our results do highlight a need for more long-term randomized prospective comparison of POEM and LHM in patients with higher ASA class to definitively establish the efficacy of one over another in these high-risk patients. This will most likely necessitate a multicenter approach owing to the rarity of achalasia and a lower number of patients with higher ASA class undergoing invasive procedures.
References
Arulampalam T, Patterson-Brown S, Morris AJ, Parker MC. Natural orifice transluminal endoscopic surgery. Ann R Coll Surg Engl. 2009;91(6):456–9. https://doi.org/10.1308/003588409X464487.
Marano L, Pallabazzer G, Solito B, et al. Surgery or peroral esophageal myotomy for Achalasia: A systematic review and meta-analysis. Med (United States). 2016;95(10):e3001.
Schlottmann F, Luckett DJ, Fine J, Shaheen NJ, Patti MG. Laparoscopic Heller Myotomy Versus Peroral Endoscopic Myotomy (POEM) for Achalasia: a systematic review and meta-analysis. Ann Surg. 2018;267(3):451–60. https://doi.org/10.1097/SLA.0000000000002311.
Hungness ES, Sternbach JM, Teitelbaum EN, Kahrilas PJ, Pandolfino JE, Soper NJ. Per-oral endoscopic myotomy (POEM) after the learning curve: durable long-term results with a low complication rate. Ann Surg. 2016;264(3):508–15. https://doi.org/10.1097/SLA.0000000000001870.
Hernández-Mondragón OV, Solórzano-Pineda OM, González-Martínez M, Blancas-Valencia JM. Gastroesophageal reflux disease after peroral endoscopic myotomy: short-term, medium-term, and long-term results. Rev Gastroenterol Mex. 2020;85(1):4–11. https://doi.org/10.1016/j.rgmx.2019.04.001.
Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic Achalasia. N Engl J Med. 2019;381(23):2219–29. https://doi.org/10.1056/NEJMoa1905380.
Inoue H, Shiwaku H, Iwakiri K, et al. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018;30(5):563–79. https://doi.org/10.1111/den.13239.
Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020;91(2):213-227.e6. https://doi.org/10.1016/j.gie.2019.04.231.
Moonesinghe SR, Mythen MG, Das P, Rowan KM, Grocott MPW. Risk stratification tools for predicting morbidity and mortality in adult patients undergoing major surgery: qualitative systematic review. Anesthesiology. 2013;119(4):959–81. https://doi.org/10.1097/ALN.0b013e3182a4e94d.
Doyle DJ, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). StatPearls Publishing; 2018. http://www.ncbi.nlm.nih.gov/pubmed/28722969. Accessed 16 Mar 2020.
Prause G, Offner A, Ratzenhofer-Komenda B, Vicenzi M, Smolle J, Smolle-Jü Ttner F. Comparison of Two Preoperative Indices to Predict Perioperative Mortality in Non-Cardiac Thoracic Surgery1997; vol 11. https://academic.oup.com/ejcts/article-abstract/11/4/670/350170. Accessed 5 Apr 2020.
Vacanti CJ, VanHouten RJ, Hill RC. A statistical analysis of the relationship of physical status to postoperative mortality in 68,388 cases. Anesth Analg. 49(4):564–566. http://www.ncbi.nlm.nih.gov/pubmed/5534668. Accessed 30 Apr 2020.
Hopkins TJ, Raghunathan K, Barbeito A, et al. Associations between ASA Physical Status and postoperative mortality at 48 h: a contemporary dataset analysis compared to a historical cohort. Perioper Med. 2016. https://doi.org/10.1186/s13741-016-0054-z.
Sanaka MR, Hayat U, Thota PN, et al. Efficacy of peroral endoscopic myotomy vs other Achalasia treatments in improving esophageal function. World J Gastroenterol. 2016;22(20):4918–25. https://doi.org/10.3748/wjg.v22.i20.4918.
Doyle DJ, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). StatPearls Publishing; 2018. http://www.ncbi.nlm.nih.gov/pubmed/28722969. Accessed 12 Oct 2020
Stavropoulos SN, Desilets DJ, Fuchs KH, et al. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80(1):1–15. https://doi.org/10.1016/j.gie.2014.04.014.
Greenleaf EK, Winder JS, Hollenbeak CS, Haluck RS, Mathew A, Pauli EM. Cost-effectiveness of per oral endoscopic myotomy relative to laparoscopic Heller myotomy for the treatment of achalasia. Surg Endosc. 2018;32(1):39–45. https://doi.org/10.1007/s00464-017-5629-3.
Li QL, Wu QN, Zhang XC, et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc. 2018;87(6):1405-1412.e3. https://doi.org/10.1016/j.gie.2017.10.031.
Nabi Z, Ramchandani M, Chavan R, et al. Per-oral endoscopic myotomy for achalasia cardia: outcomes in over 400 consecutive patients. Endosc Int Open. 2017;05(05):E331–9. https://doi.org/10.1055/s-0043-105517.
Awaiz A, Yunus RM, Khan S, Memon B, Memon MA. Systematic review and meta-analysis of Perioperative Outcomes of Peroral Endoscopic Myotomy (POEM) and Laparoscopic Heller Myotomy (LHM) for Achalasia. Surg Laparosc Endosc Percutaneous Tech. 2017;27(3):123–31. https://doi.org/10.1097/SLE.0000000000000402.
Repici A, Fuccio L, Maselli R, et al. GERD after per-oral endoscopic myotomy as compared with Heller’s myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc. 2018;87(4):934-943.e18. https://doi.org/10.1016/j.gie.2017.10.022.
Nabi Z, Reddy DN, Ramchandani M. Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc. 2018;87(1):4–17. https://doi.org/10.1016/j.gie.2017.09.029.
Hopkins J, Switzer NJ, Karmali S. Update on novel endoscopic therapies to treat gastroesophageal reflux disease: a review. World J Gastrointest Endosc. 2015;7(11):1039. https://doi.org/10.4253/wjge.v7.i11.1039.
Familiari P, Greco S, Gigante G, et al. Gastroesophageal reflux disease after peroral endoscopic myotomy: analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc. 2016;28(1):33–41. https://doi.org/10.1111/den.12511.
Shiwaku H, Inoue H, Sasaki T, et al. A prospective analysis of GERD after POEM on anterior myotomy. Surg Endosc. 2016;30(6):2496–504. https://doi.org/10.1007/s00464-015-4507-0.
Sankar A, Johnson SR, Beattie WS, Tait G, Wijeysundera DN. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth. 2014;113(3):424–32. https://doi.org/10.1093/bja/aeu100.
Gupta PK, Gupta H, Sundaram A, et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation. 2011;124(4):381–7. https://doi.org/10.1161/CIRCULATIONAHA.110.015701.
Han K, Kim HL, Pantuck AJ, Dorey FJ, Figlin RA, Belldegrun AS. Use of American Society of Anesthesiologists physical status classification to assess perioperative risk in patients undergoing radical nephrectomy for renal cell carcinoma. Urology. 2004;63(5):841–6. https://doi.org/10.1016/j.urology.2003.12.048 (discussion 846–7).
Skaga NO, Eken T, Søvik S, Jones JM, Steen PA. Pre-injury ASA physical status classification is an independent predictor of mortality after trauma. J Trauma. 2007;63(5):972–8. https://doi.org/10.1097/TA.0b013e31804a571c.
Vacanti CJ, VanHouten RJ, Hill RC. A statistical analysis of the relationship of physical status to postoperative mortality in 68388 cases. Anesth Analg. 1970;49(4):564–6 (Accessed 10 Apr 2020).
Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77(2):217–22. https://doi.org/10.1093/bja/77.2.217.
Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–9. https://doi.org/10.1161/01.CIR.100.10.1043.
Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of Perioperative Outcomes between Peroral Esophageal Myotomy (POEM) and Laparoscopic Heller Myotomy. J Gastrointest Surg. 2013;17(2):228–35. https://doi.org/10.1007/s11605-012-2030-3.
Zhang Y, Wang H, Chen X, et al. Per-Oral Endoscopic Myotomy versus Laparoscopic Heller Myotomy for Achalasia. Med (United States). 2016. https://doi.org/10.1097/MD.0000000000002736.
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL. A comparative study on comprehensive, objective outcomes of laparoscopic heller myotomy with Per-Oral Endoscopic Myotomy (POEM) for achalasia. Ann Surg. 2014;259(6):1098–103. https://doi.org/10.1097/SLA.0000000000000268.
Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, Denham W. Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach. Surg (United States). 2013;154(4):893–900. https://doi.org/10.1016/j.surg.2013.04.042.
Khashab MA, Kumbhari V, Tieu AH, et al. Peroral endoscopic myotomy achieves similar clinical response but incurs lesser charges compared to robotic heller myotomy. Saudi J Gastroenterol. 2017;23(2):91–6. https://doi.org/10.4103/1319-3767.203360.
Boeckxstaens GE, Annese V, Des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364(19):1807–16. https://doi.org/10.1056/NEJMoa1010502.
Prakash Gyawali C, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: The Lyon Consensus. Gut. 2018;67(7):1351–62. https://doi.org/10.1136/gutjnl-2017-314722.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Madhusudhan R Sanaka, Dr. Pravallika Chadalavada, Dr. Fahrettin Covut, Dr. Rajat Garg, Dr. Prashanthi Thota, Dr. Scott Gabbard, Dr. Mohammad Alomari, Dr. Sudish Murthy, and Dr. Siva Raja have no conflicts of interest or financial ties to disclose pertinent to this article.
Ethical Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on Human experimentation and with the Helsinki declaration of 1964 and later versions. This retrospective study was approved by the Institutional Board Review of Cleveland Clinic.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript has not been published and is not under consideration for publication elsewhere. However, the preliminary data was accepted in abstract form for a poster presentation at the Digestive Disease Week, DDW 2020 conference (May 2nd–5th, 2020 | Chicago, Illinois).
Rights and permissions
About this article
Cite this article
Sanaka, M.R., Chadalavada, P., Covut, F. et al. Peroral endoscopic myotomy is equally safe and highly effective treatment option in achalasia patients with both lower and higher ASA classification status. Esophagus 18, 932–940 (2021). https://doi.org/10.1007/s10388-021-00840-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-021-00840-2