Abstract
Purpose
To investigate the changes in spherical equivalent and pupil response during near viewing in patients with intermittent exotropia (IXT) who have complaints of blurred vision or asthenopia from near viewing in daily life using a novel binocular wavefront aberrometer.
Study design
A cross-sectional study.
Methods
Ten IXT patients and ten healthy subjects wearing full-correction lenses at far sight (5 m) were instructed to fixate on a near target at 67 cm, which was then moved to 40 cm three times. Serial changes in the spherical equivalent (SE) refractive error (SE) were measured during this task using a laboratory-made open-field binocular Hartmann–Shack wavefront aberrometer and compared between patients and healthy subjects. In the IXT patients, regression analysis was performed between ∆SE and exodeviation angles, as measured by an alternate prism and cover test. Pupil-diameter and pupil-constriction ratios were also compared between patients and healthy subjects, and the correlation of constriction ratio with ∆SE was calculated for both groups.
Results
Compared to healthy subjects, IXT patients demonstrated significantly lower ∆SE of convergence (mean ± SD, 0.91 ± 0.26 D vs. 1.15 ± 0.19 D; P < 0.05) and divergence (0.93 ± 0.28 D vs. 1.16 ± 0.20 D; P < 0.05). Angle of exotropia was negatively correlated with ∆SE during far-sight and near-sight convergence and divergence (P < 0.05). Pupil-constriction ratio was also reduced in patients compared to healthy subjects (6.67% ± 3.31% vs. 11.9% ± 5.96%; P<0.05). Pupil-constriction ratio was positively correlated with ∆SE during convergence in both groups (P < 0.05).
Conclusion
Insufficient accommodation and pupil constriction during near viewing were observed in patients with IXT who had complaints of blurred vision or asthenopia from near viewing. These conditions might contribute to symptoms, such as fatigue, eye strain and impaired visual performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intermittent exotropia (IXT) is a common type of ocular misalignment (strabismus) in both children and adults [1,2,3]. Most adult patients experience discomfort associated with near work, such as study, and may also express cosmetic concerns [4]. The symptoms of IXT are variable, and can include headache, blurred vision, diplopia and eye fatigue, although few studies have compared the clinical characteristics of adult and pediatric IXT [4]. Numerous tasks in modern daily life require near vision, such as the use of computers, smartphones, tablets and other digital electronic devices. Intermittent exotropia patients may be unable to perform these activities efficiently, leading to asthenopia, fatigue, visual discomfort, blurred near vision or exodeviation.
Many studies have examined binocular vision impairments in IXT patients. In adults, decreased distant binocular visual acuity is observed due to greater demand on accommodation for controlling exodeviation [5, 6]. Reduced-distance stereoacuity in patients with IXT has also been associated with myopic shift and miosis, which occur when the visual system switches from monocular to binocular viewing conditions [7]. A significant myopic shift under binocular conditions is observed in IXT with a relatively large angle; thus, IXT patients rely on increased accommodation, and this in turn may induce eye strain and discomfort [7].
In IXT patients, therefore, binocular target fixation deteriorates. Moreover, greater effort to converge is required for near-target binocular fixation, especially if the angle of exodeviation is large [7]. However, no study has adequately examined dynamic changes in accommodation, convergence, and pupil constriction during near viewing among IXT patients [8,9,10,11,12]. Commercially available devices provide almost only monocular information on dynamic eye state, making it impossible to compare the dynamic state of both eyes simultaneously. Consequently, there is little information on how well an IXT patient can accommodate and converge in real-life situations. To overcome these limitations, we have developed a binocular open-view Hartmann–Shack wavefront sensor for measuring temporal variations of binocular accommodation and monochromatic aberrations [13, 14]. This instrument is also equipped with an infrared (IR) eye-gaze tracker to monitor pupil–corneal reflection and pupil diameter.
Methods
This study adhered to the Declaration of Helsinki and was approved by the institutional review board of Osaka University Medical School Hospital. The protocol was registered with the UMIN Clinical Trials Registry (UMIN 000005846) on June 24, 2011. Informed consent for participation and publication of anonymized data was obtained from all participants.
Subjects
Ten patients with IXT reporting gradually blurred vision or asthenopia from near viewing in daily life were recruited at Osaka University Hospital between April 2014 and April 2016. Patients were included if they were able to fully participate in the examinations and cooperate with binocular wavefront-sensor measurements. Patients with amblyopia or ocular diseases were excluded. All patients were examined by experienced orthoptists.
Patients included seven men and three women of mean age (±standard deviation [SD]) 20.1 ± 5.74 years (range, 13–29 years). Best-corrected visual acuity (BCVA) was 1.0 or better OU in all patients. The angle of exotropia was measured by an alternate prism cover test (APCT) at 5 m and 30 cm. Patients with exodeviation at least 12 ∆ at distance or near determined by APCT were included. The mean angle was 13.9 ± 9.46∆ exotropia (range, 2−35∆) at 5 m and 22.3 ± 8.46∆ exotropia (range, 10−35∆) at 30 cm. The right eye was dominant in four subjects and the left eye in six as determined by the Miles test. The average spherical equivalent (SE) refractive error of the dominant eye was −3.88 ± 2.57 D (range, −8.25 to −0.25 D) measured by an autorefractor. A Titmus stereo test (Stereo Optical Inc.) indicated that the stereoacuity of all patients was 60 seconds of arc or better (classified as ‘good’).
We also examined ten normal subjects, who did not complain of blurred vision or asthenopia from near viewing in daily life, all were without any eye diseases except for the refractive error. Eye position in these subjects was either orthophoric or slight exophoric determined by alternative cover–uncover tests. These subjects included four men and six women (mean age, 24.7 ± 5.41 years; range, 13−32 years). The right eye was dominant in four subjects and the left eye in six. The average SE refractive error was −2.73 ± 1.85 D (range, −5.38 to 0.0 D) (Table 1).
Measurement of binocular spherical equivalent and pupil diameter during vergence
The SE was measured using a laboratory-made binocular Hartmann–Shack wavefront aberrometer (Topcon Corp) (Fig. 1a, b). Details are described elsewhere [13, 14]. Briefly, this instrument automatically measures and records sequential wavefront aberrations for 3.5 seconds at a sampling rate of 30 Hz (Fig. 1a, b). The diameter of each lenslet is 200 lumen (lm) and the focal length is 5 mm, allowing approximately 250–260 sample points in the Hartmann image within a 4-mm diameter pupil. It is equipped with an eye-gaze tracker using infrared light to monitor the pupil and corneal reflection. The distance between the center of the pupil and the corneal reflection was measured by a camera focused on the anterior segment of the eye. A calibration procedure was performed before each experimental trial. The subject, who wore full correction lenses at 5 m, was instructed to look at a calibration plate that consisted of eight horizontal targets placed 2 cm apart and located 50 cm in front of the eye. We confirmed that all subjects demonstrated binocular convergence when fixating on a target located 67 cm from the corneal surface.
Schematic view of the binocular Hartmann–Shack wavefront aberrometer. (a, b) An in-house aberrometer was used to measure the spherical equivalent (SE) and angle of vergence under natural near-viewing conditions. (c, d) A visual target (a 2 cm white asterisk on a blackboard) was set 67 cm in front of the eyes and moved to 40 cm (range of 1.0 MA) three times at 0.5 MA/second
Wavefront measurements were made in a darkened room through a natural pupil while subjects wore their full correction lenses. Subjects were instructed to fixate with both eyes on a target (a 2 cm white asterisk on a blackboard) 67 cm in front. During fixation, the target moved from 67 cm to 40 cm [range of 1 meter angle (MA)] in front of the eyes and then returned to 67 cm at 0.5 MA/second (Fig. 1c, d). This cycle was repeated three times for each subject. Four measurements were taken, and SE was analyzed quantitatively in the central 4 mm diameter of the pupil by expanding the set of Zernike polynomials using customized software developed in our laboratory. The SE was measured OU simultaneously every 33.3 milliseconds for 3.5 seconds (total of 106 samples per eye).
The longitudinal diameter of the pupil, which was not affected by the eye deviation, was also measured in real time with a camera during convergence. The baseline pupil diameter (mm) was defined as the mean over 1.0 second during fixation on the target at 67 cm before the task, and minimal pupil diameter (mm) was defined as the smallest pupil size during constriction. Four measurements were taken, and the waves were analyzed. The pupillary constriction ratio (%) was defined as the difference between the baseline and minimum diameter divided by the baseline pupil diameter, and the pupil constriction time (in seconds) as the time between initiation and peak pupillary constriction.
Data analysis
Data are expressed as mean ± SD. We collected measurements of SEs and pupil diameters from dominant eyes both in IXT patients and normal subjects. All statistical analyses were conducted using JMP ver.13.0 (SAS Institute). The significance level was set at P < 0.05 (two tailed) for all tests. Mean changes in SE (∆SE) and pupil diameter were compared between IXT patients and healthy subjects by independent sample t-tests after confirming that data sets were normally distributed according to the Kolmogorov-Smirnov normal test. The relationships between ∆SE and alternate prism cover test and pupil constriction ratio were evaluated by linear regression.
Results
Accommodation measurements using the in-house wavefront aberrometer
All subjects demonstrated binocular convergence and divergence during the task, and three parameters (SE, pupil diameter, and eye positions) were completely recorded, although some subjects blinked and some patients with IXT diverted their non-dominant eyes; however, they did not observe the target monocularly.
Figure 2 shows representative SE responses, pupil diameter responses, and eye positions (right eye: blue; left eye: red line) for a normal subject and an IXT patient. Patients exhibited higher-amplitude irregular fluctuations during baseline recording. None of the patients exhibited a deviation that could not be tracked by the aberrometer during the visual-fixation task. In both groups, waveforms consisted of three negative (N1-N3) and four positive peaks (S1−S4). To evaluate SE and pupil diameter changes, waves were divided into two phases, convergence and divergence, and the average changes in S1-N1, S2-N2, and S3-N3 during the convergence phase and the average changes in S2-N1, S3-N2, and S4-N3 during the divergence phase were measured. We also determined the peak to peak times (for example, S1 to N1) as the response durations.
Representative spherical equivalent (SE), pupil diameter, and eye position changes in a normal subject and an IXT patient. Responses of spherical equivalent (SE) in a normal subject (left column) and an IXT. patient (right column) (right eye: blue; left eye: red line) during near viewing (a). Responses of pupil diameter in a normal subject (left column) and an IXT patient (right column) during near viewing (b). Baseline SE and pupil diameter were more irregular (fluctuating) in the IXT patient. There were three negative peaks (N1−N3) and four positive peaks (S1−S4) in all waves. Changes in eye positions in a normal subject (left column) and an IXT patient (right column) during near viewing (c)
Lower ∆SEs of convergence and divergence in IXT patients
Figure 3 shows ∆SEs of the dominant eyes during convergence and divergence. The mean ∆SE of convergence was significantly lower in IXT patients compared to normal subjects (0.91 ± 0.26 D vs. 1.15 ± 0.19 D; P = 0.0289) (Fig. 3a, Table 2). Similarly, mean ΔSE of divergence was significantly lower in IXT patients (0.93 ± 0.28 D vs. 1.16 ± 0.20 D; t-test P = 0.0477) (Fig. 3b, Table 2). On the other hand, there was no significant difference in baseline SE of the dominant eye during binocular fixation on the target at 67 cm between IXT patients and normal subjects (−1.04 ± 0.30 D vs. −1.20 ± 0.36 D) (Fig. 3c). There were also no significant differences in ∆SE durations of convergence and divergence between IXT patients and normal subjects (Table 2).
Spherical equivalent changes (∆SEs) during convergence and divergence in IXT patients and normal subjects. The ∆SE values during convergence (a) and divergence (b) were significantly smaller in IXT patients than normal subjects. On the other hand, there was no significant difference in mean baseline SE of the dominant eye between IXT patients and normal subjects (c). a. Convergence: * P = 0.0289 by t-test, b. Divergence: ** P = 0.0477 by t-test
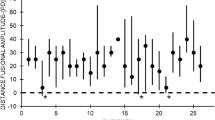
Relationship between eye exodeviation and ∆SE in IXT patients
The angle of exotropia was negatively correlated with ∆SE during vergence for both far and near sight (far-sight exotropia: convergence: P = 0.0184; divergence: P = 0.0074; near-sight exotropia: convergence: P = 0.0403; divergence: P = 0.0284). Thus, ∆SE tended to decrease with greater angle of exotropia (Fig. 4).
Pupil constriction ratio and duration during convergence in IXT patients and normal subjects
Compared to healthy controls, IXT patients exhibited lower-pupil constriction ratios (6.67% ± 3.31% vs. 11.9% ± 5.96%; t-test P = 0.0256) (Fig. 5a, Table 3); however, there were no significant differences in pupil-constriction times and baseline pupil diameters between IXT patients and normal subjects (Fig. 5b, c; Table 3).
Pupil-constriction ratio and duration during convergence in IXT patients and normal subjects. The pupil-constriction ratio (a) during convergence was significantly smaller in IXT patients than in normal subjects, while there was no significant difference in pupil-constriction time (b) and baseline pupil diameter (c) of the dominant eye between groups. * P = 0.0109 by t-test
Relationship between pupil constriction ratio and convergent ∆SE in IXT patients and normal subjects
Pupil-constriction ratio was positively correlated with ∆SE during convergence in both IXT patients and normal subjects (IXT: P = 0.0128; normal subjects: P = 0.0364) (Fig. 6). Therefore, pupil-constriction ratio increased with the extent of accommodation.
Relationship between pupil-constriction ratio and ∆SE in IXT patients and normal subjects. Pupil-constriction ratio was positively correlated with ∆SE during convergence in both groups (blue: IXT patients: P = 0.0128; red: normal subjects: P = 0.0364), confirming an association between pupil-constriction ratio and accommodation
Discussion
Using our in-house open-field binocular Hartmann–Shack wavefront aberrometer, we demonstrated a measurable deficit in accommodation (∆SE) in IXT patients compared to healthy controls during binocular near viewing. A larger angle of exotropia was associated with smaller changes in SE during vergence, suggesting that this deficit gets worse with more severe eye misalignment. Pupil-constriction ratio during binocular near viewing was also deficient in IXT patients compared to normal subjects. Collectively, these results suggest that insufficient accommodation and pupil constriction are the causes of the visual discomfort, fatigue, eye strain, and impaired visual performance observed n IXT patients.
Insufficient accommodation in IXT patients during near viewing
Significantly reduced accommodation of the dominant eye during binocular near viewing was observed in IXT patients (Fig. 3c). On the other hand, Horwood et al. report that increased vergence demand to control intermittent distance exotropia for near vision also drives significantly increased accommodation [15]. Intermittent exotropia patients bear greater accommodative loads during binocular viewing of a near target [7, 9]. Thus, IXT patients require excessive accommodation to maintain single binocular vision when focusing on a near target. Our results are different from those reports for the following reasons. When patients were fixating on a near target with both eyes before the start of the task, accommodative loads induced by convergence may have been applied, thereby reducing residual accommodation capacity during the task. The negative correlation between angle of exotropia and ∆SE during vergence (Fig. 4) suggests that accommodative loads increase with IXT severity.
Decrease of pupil constriction ratio during convergence in IXT patients
We also observed significantly reduced pupil-constriction ratios in IXT patients, and a positive correlation between the pupil-constriction ratio and ∆SE in both IXT patients and normal subjects. To the best of our knowledge, no previous studies have described dynamic changes of pupil response in IXT patients during near viewing or the relationship between pupil-constriction ratio and ∆SE. This result also suggests that accommodative loads induced by convergence may have been applied before the start of the task, thereby reducing residual pupil constriction during the task. These results thus suggest that poor binocular near viewing (insufficient accommodation and pupil constriction) in patients with IXT who complained about eye fatigue or blurred vision at near works might stem from excessive accommodative loads by convergence before the task, although we are aware that there was no difference in the baseline SE before the task between IXT patients and healthy subjects. In this study, all patients wore full correction lenses at 5 m under binocular condition; therefore, there were fewer chances of developing phoria myopia, resulting in no difference in the baselines of SE and pupil diameter.
This study has several limitations. We collected measurements of SEs and pupil diameters from dominant eyes only of both the IXT patients and normal subjects because of the possibility that nondominant eyes were slightly exodeviated during the task and could not be measured exactly. Although our device could record both eyes’ positions during the task in all subjects, in patients with IXT the nondominant eyes were slightly exodeviated; it was also possible that the eye position of nondominant eyes could not be measured precisely and, therefore, we did not quantitatively analyze the changes in MA during the task. Only a small number of participants were included, and IXT patients were myopic but not hyperopic, although group differences reached statistical significance. Nonetheless, a larger-scale study including IXT patients who have hyperopia as well as myopia is required to verify our conclusions.
Our open-field binocular Hartmann–Shack wavefront aberrometer revealed insufficient accommodation in patients with IXT who complained about eye fatigue or blurred vision at near works. This deficit may account for the observed visual discomfort, fatigue, asthenopia, and impaired visual performance experienced by IXT patients in daily tasks requiring near viewing. We also propose that this device could be used to measure the dynamics of binocular vision in strabismus patients during daily life. Further investigation is needed to determine the interactions among accommodation, vergence, and pupil constriction in strabismus patients for the design of appropriate therapies.
References
Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia: a population-based study. Ophthalmology. 2005;112:104–8.
Mohney BG, Huffaker RK. Common forms of childhood exotropia. Ophthalmology. 2003;110:2093–6.
Jung JW, Lee SY. A comparison of the clinical characteristics of intermittent exotropia in children and adults. Korean J Ophthalmol. 2010;24:96–100.
Lee SY, Oh JS, Kim SJ. The clinical characteristics and surgical results in the intermittent exotropia more than 15 years of age. J Korean Ophthalmol Soc. 1997;36:1056–63.
Walsh LA, Laroche GR, Tremblay F. The use of binocular visual acuity in the assessment of intermittent exotropia. J AAPOS. 2000;4:154–7.
Ahn SJ, Yang HK, Hwang JM. Binocular visual acuity in intermittent exotropia: role of accommodative convergence. Am J Ophthalmol. 2012;154:981–6.
Shimojyo H, Kitaguchi Y, Asonuma S, Matsushita K, Fujikado T. Age-related changes of phoria myopia in patients with intermittent exotropia. Jpn J Ophthalmol. 2009;53:12–7.
Chirre E, Prieto P, Artal P. Dynamics of the near response under natural viewing conditions with an open-view sensor. Biomed Opt Express. 2015;6:4200–11.
Ha SG, Jang SM, Cho YA, Kim SH, Song JS, Suh YW. Clinical exhibition of increased accommodative loads for binocular fusion in patients with basic intermittent exotropia. BMC Ophthalmol. 2016;16:77.
Horwood AM, Riddell PM. The use of cues to convergence and accommodation in naïve, uninstructed participants. Vis Res. 2008;48:1613–24.
Prieto PM, Vargas-Martín F, Goelz S, Artal P. Analysis of the performance of the Hartmann–Shack sensor in the human eye. J Opt Soc Am A. 2000;17:1388–98.
Hampson KM, Chin SS, Mallen EAH. Binocular Shack–Hartmann sensor for the human eye. J Mod Opt. 2007;55:703–16.
Kobayashi M, Nakazawa N, Yamaguchi T, Otaki T, Hirohara Y, Mihashi T. Binocular open-view Shack–Hartmann wavefront sensor with consecutive measurements of near triad and spherical aberration. Appl Opt. 2008;47:4619–26.
Kanda H, Kobayashi M, Mihashi T, Morimoto T, Nishida K, Fujikado T. Serial measurements of accommodation by open-field Hartmann–Shack wavefront aberrometer in eyes with accommodative spasm. Jpn J Ophthalmol. 2012;56:617–23.
Horwood AM, Riddell PM. Evidence that convergence rather than accommodation controls intermittent distance exotropia. Acta Ophthalmol. 2012;90:e109–17.
Acknowledgements
The authors would like to thank Enago (http://www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
T. Morimoto, None; H. Kanda, None; M. Hirota, None; K. Nishida, None; T. Fujikado, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Takeshi Morimoto
About this article
Cite this article
Morimoto, T., Kanda, H., Hirota, M. et al. Insufficient accommodation during binocular near viewing in eyes with intermittent exotropia. Jpn J Ophthalmol 64, 77–85 (2020). https://doi.org/10.1007/s10384-019-00695-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-019-00695-2