Abstract
Purpose
To evaluate the effectiveness of the orthokeratology (OK) lens slowing myopic progression compared with no intervention in pediatric eyes
Methods
A retrospective review of medical records was performed on 45 monocular myopic subjects 7 to 13 years of age who were treated with monocular ortho-k lens and followed-up for more than 12 months. The monocular myopia in the subjects’ eyes was -0.75 to -4.25 D (diopter), and near emmetropia in the contralateral and with-the-rule astigmatism no greater than -1.50 D. Axial elongation OU, reflecting the progression of myopia was measured at baseline using the same AL-Scan Optical Biometer and compared between the two eyes of each individual every six months for one year in all subjects and for two years in 9 subjects.
Results
After 12 months of lens wear, axial length had increased by 0.36 ± 0.23mm in the control eyes (P < 0.001) but showed far less change (+0.07 ± 0.21 mm) in the OK eyes (P = 0.038). The nine subjects followed-up for 2 years showed no axial length change (+0.16 ± 0.25 mm) in the OK eyes (P = 0.095) after 24 months and significant axial length growth (+0.38 ± 0.26 mm; P = 0.002) in the control eyes. Control eyes showed progressive axial length growth throughout the study compared with the one OK lens eye.
Conclusions
Using a contralateral eye study design, which prevented the influence of potential confounding factors, Effectiveness of the OK lens was proved. Myopic progression within a subject was excellent compared with no intervention
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of myopia is now a global concern. Approximately 25% of the world’s population has myopia, with an especially higher prevalence in Asia [1, 2]. Myopia is inconvenient because of the need to wear glasses or contact lenses. More seriously, it can also cause secondary ocular diseases, such as retinal detachment, myopic macular degeneration, and glaucoma. There is also a clear dose-response relationship with increased risks at higher degrees of myopia. Slowing myopic progression is important [3]. Interventions that have been attempted include multifocal lenses [4], multifocal contact lenses [5], timolol drops [6], atropine [7], and orthokeratology (OK).
Axial length increases in the majority of patients as myopia progresses. Thus, axial length can be utilized as an indicator of myopic progression [8]. OK lenses can more effectively control myopia than traditional single-vision spectacles by inhibiting axial elongation [9,10,11].
The effectiveness of OK lenses in inhibiting myopic progression has been described in children wearing an OK lens in one eye and a rigid gas permeable (RGP) lens in the contralateral eye [12]. The study results provide evidence that overnight, the OK lens inhibits axial eye growth and myopia progression to a larger extend, as compared with conventional RGP lenses.
Although this study was significant in comparing contralateral eyes, the control eyes may have been somewhat affected by the RGP lenses. To the best of our knowledge, there is only one case report of direct comparison of changes over time in an individual with an OK lens in one eye and the other eye unaided. In that report, conducted over a two-year period in an 11-year-old boy, there was an increase in axial length of 0.34 mm in the eye with no visual correction and 0.13 mm in the OK lens eye [13]. This study suggests the inhibitory effect of OK lens in an individual aided by monocular OK lens.
The purpose of the present study was to evaluate the effectiveness of the OK lens in children’s eyes compared with no intervention. To achieve this purpose, we included myopic-anisometropic patients who had a single myopic eye and a single nearly emmetropic eye. The main causes of anisometropia were corneal refractive power and ocular axial length [14, 15]. No other organic problems like corneal opacity, spherophakia, retinopathy of prematurity (ROP), and myelinated nerve fiber were evident in our patients.
Methods
This 24-month study used a retrospective, contralateral eye control design. The study conformed to the tenets of the Declaration of Helsinki (2008), and the research protocol and documentation received approval from the Saevit Eye Hospital Institutional Review Board.
Subjects
We obtained the pertinent data from the examination results in the medical records of children who came to our clinic for vision correction in only one myopic eye and who wore OK lenses on that single eye from 2013 to 2016. Our inclusion criteria specified age between 7 and 13 years at initial lens wearing.
The most important inclusion criterion of the children included in the data analysis was that one myopic eye had to have an uncorrected visual acuity lower than 20/25 and no organic problem other than refractive error. The contralateral eye also had to have an uncorrected visual acuity of 20/25 or better so that no correction was needed. Our refractive criteria were myopia in one eye at the spherical equivalent of between -0.75 D (diopter) and -4.25 D, and near emmetropia or very mild myopia/hyperopia in the contralateral eye of between -0.75 D, and +0.625 D.
The children included had with-the-rule astigmatism no greater than -1.50 D, no one had against-the rule or oblique astigmatism; monocular corrected distance visual acuity was no worse than 20/20 OU; no active inflammatory ocular surface diseases; no near or distance strabismus; no previous use of rigid contact lenses, no spectacles other than single-vision, no other myopia control modalities such as multifocal soft contact lens, atropine, and adequate capability to complete the lens care protocol of inserting, removing, cleaning, rinsing, and storing the lenses with or without parents’ help. Subjects were excluded if the myopic refractive error in their control eyes exceeded -0.75 D in spherical equivalent refraction (SER) or the non-corrected visual acuity (NCVA) in their control eyes ever dropped below 20/25 for any reason.
Procedure
Before the subjects began wearing the lenses, we measured their axial length, NCVA, best-corrected visual acuity (BCVA), both cycloplegic and non-cycloplegic manifest refractions, corneal topography, and corneal curvature using autokeratometry.
The OK lenses (Ortho-K LK Lens; Lucid Korea) were spherical four-zone lenses made of gas-permeable lens material (Boston XO). All subjects were fitted for the lens in the myopic eye by a certified ophthalmic technician based on the manufacturer’s instructions.
Subsequently, the lenses were dispensed to the patients. They were advised to wear the lenses in their myopic eye for at least eight consecutive hours every night and told that they needed to follow a specified cleaning procedure every time they removed the lenses.
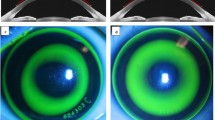
All patients underwent ocular examinations including slit lamp examination, NCVA, BCVA, non-cycloplegic manifest refraction, and corneal curvature assessment by automatic keratometry one day, two weeks and three months following initial lens setting, and then at six-month intervals over two years. We measured axial length and performed corneal topography before and six months after the lens wear. Corneal topography was performed only in the lens-wearing eye, but all other examinations were performed OU. All data were measured in individual subjects, but for convenience, the data on the OK lens eyes were defined as the OK lens group, and the data for the naked eyes were defined as the control group.
At every visit, we conducted slit lamp assessments and used sodium fluorescein dye under cobalt blue lighting to determine the corneal surface integrity. In addition to coming for their regular checkups, the children were instructed to visit whenever any ocular symptoms occurred. Whenever any abnormal symptoms, such as photophobia, redness, eye pain, or tearing, occurred, we had the children stop wearing the OK lens for an average of one month and, if the symptoms were severe, the subjects received the appropriate treatment. The children could not start wearing the lenses again until they had completely recovered because lens wearing may worsen cases of keratitis. Whenever infective keratoconjunctivitis developed in the control eye, the OK lens use was t halted.
When patients had NCVA < 20/25 or SER < -0.50 D despite wearing the OK lenses for more than eight hours of sleep and regular checkup visits, We performed corneal topography to confirm that lens centration was desirable. If there were no problems on corneal topography, we had the children revisit after two or more consecutive weeks of lens wear; if the results were the same after two weeks even when the children had sufficiently followed the instructions, they were excluded from the data analysis.
Measurement techniques
Axial length
We used the AL-Scan Optical Biometer (Nidek) to measure axial length. This noncontact instrument is based on infrared interferometry principles and measures the distance in millimeters from the apex of the anterior corneal surface to the retinal pigment epithelium. We took six measurements of axial length at each measurement session and averaged them; the axial length measurements were taken from the same optical biometer each time by the same masked examiner.
Corneal topography
All subjects underwent imaging with a Keratograph® 4 (Oculus) on the OK lens eye before they began wearing the lenses and then at every six-month visit. All measurements were taken by a trained optometrist or contact lens optician and took approximately 30 s; the instruments were calibrated by the manufacturers immediately prior to the study. On each measurement occasion, three topographic maps were captured for each eye and the mean values for the variables of interest were calculated. The variable of interest was corneal asphericity (Q).
Refractive error
Cycloplegic manifest refraction was performed on the children before they began wearing the OK lenses on their myopic eyes; we induced the cycloplegia 20 min before refraction with 1% cyclopentolate eye drops (Cyclogyl® Eye Drops; Alcon Pharmaceutical Co.). Three of the drops were administered at five-minute intervals. Non-cycloplegic manifest refraction was performed during every follow-up visit.
Autokeratometry
Mean flat and steep K were measured using an ARK-1 auto-refractor/keratometer (Nidek) OU at every visit. We automatically obtained five measurements from each eye and averaged them on each measurement occasion.
Statistical analyses
Extracted data were imported into a database. Statistical analyses were conducted using SPSS software ver. 18.0 (SPSS Inc.). All data were distributed normally (Kolmogorov-Smirnov test, P > 0.05) and are presented as the mean ± standard deviation. Baseline sphere, cylinder, spherical equivalent refractive error, and axial length were compared between the two study groups using independent-samples t tests.
Changes in SER error and axial length were assessed over time using repeated-measures ANOVAs with one within-subject factor (visits: baseline, 6, 12, and 24 months) and one between-subject factor (treatment modality: OK lens or none), including evaluating the contributions of each factor and their interactions.
We measured the differences between visits (i.e., pre-OK vs. post-OK) using a paired t test or Wilcoxon signed rank test depending on normality of data distribution. P < 0.05 was considered to be statistically significant.
Results
We reviewed the data of 75 patients who used the monocular OK lenses. Within 12 months, 15 showed myopic progression in the control eye (SER > -0.75). These children were instructed to wear either binocular OK lenses or single-vision glasses. There were no severe complications such as bacterial or amoebic keratitis. Eight children were unable to adapt to lens wear. Three had recurrent contact lens related allergic reaction and stopped wearing their lenses. They were treated with anti histamine eye drops and steroid eye drops. All three cases were cured without sequelae such as corneal opacity. Four were lost to follow-up.
Ultimately, we reviewed the data on 45 subjects (90 eyes), 29 girls and 16 boys. Among the children who wore the OK lenses, all slept with their lenses for at least eight hours every night and achieved unaided visual acuity of 20/25 or better during two-week follow-up visits. The subjects wore monocular OK lenses without a lens change for at least 12 months, with nine patients who had worn OK lenses for over 24 months and had regular follow-up during which they also wore the same lenses for the 24 months.
The baseline biometric data for the OK lens and no-lens eyes obtained immediately before the children began wearing the lenses are presented in Table 1. Average sphere diopter, SER error, and axial length at baseline were statistically different between the OK lens and control groups (all P < 0.001), but there were no differences in cylinder diopter between the two groups (P = 0.354).
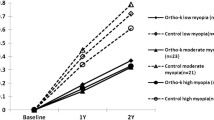
Axial length
Table 2 presents the baseline axial lengths in the OK lens and control groups. In the OK lens group, the initial axial length was 24.19 ± 0.82 mm. After one year it was 24.26 ± 0.79 mm (P = 0.038). In the control group, the axial length increased from 23.50 ± 0.68 mm to 23.82 ± 0.70 mm (P < 0.001) and axial length elongation over one year was different between the two groups (P < 0.001) (Fig. 1).
The OK lens can mechanically reduce the axial length. Therefore, we compared the axial elongation between 6 and 12 months after treatment. In the OK lens group, the axial length elongation was +0.09 ± 0.17 mm (P = 0.001) and the control group showed more axial length elongation as long as +0.17 ± 0.15 mm (P < 0.001) between 6 and 12 months.
Box’s test of equality of covariance matrices revealed that the observed covariance matrices of the dependent variables were equal across groups (P = 0.036).
The repeated-measures (for baseline, 6 months, 12 months) ANOVAs revealed significant within-group increases in axial length over time (P < 0.001), and the within-group time-varying changes in the two groups differed as well (P < 0.001). In addition, the between-group efficacy differed between the two groups (P =0.001).
Nine subjects’ follow-up for two years showed no axial length change (+0.16 ± 0.25 mm) in the OK eyes (P = 0.095) after 24 months and significant axial length growth (+0.38 ± 0.26 mm) in the OK eyes (P = 0.002) (Table 3).
Refractive error
Considering that the baseline SER value in the OK lens group was -1.56 ± 0.78 D and the 12-month SER values was +0.03 ± 0.41 D, there was a significant hyperopic shift (correction of myopia) after six months (P < 0.001) and 12 months (P < 0.001) of OK lens wear (Table 4). The control group showed continuous axial length elongation, indicating that the SER was statistically significantly different from baseline (P < 0.001) based on the myopic progression from -0.21 ± 0.33 D to -0.65 ± 0.50 D after 12 months.
Table 3 summarizes the data on the nine of 45 patients who wore the monocular lenses for the last 24 months. The effects of the monocular OK lens were also excellent in the patients who received relatively long follow-up.
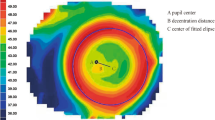
Corneal topography
In Table 5, we summarize the topographic variables of interest at 12 and 24 months of follow-up in the OK lens group. After 12 months of OK lens wear, there was a significant decrease or flattening of flat and steep keratometry (both P < 0.001) compared with baseline. We also observed a significant positive shift in Q value (toward oblate) after 12 and 24 months (both P < 0.05).
These data demonstrate clinically significant changes from baseline in flat and steep K values, and Q in the OK lens-wearing eyes only, confirming that an OK effect was achieved during overnight wear of the reverse geometry lenses during the follow-up period.
Discussion
The myopic population is growing, and secondary degeneration due to myopia, such as retinal detachment, myopic macular degeneration, and glaucoma, are often irreversible [3]. Therefore, preventing myopia progression is a worldwide concern, and it is necessary to determine the most effective methods to accomplish this. In this study, axial length elongation in the children who wore the monocular OK lens over 12 months was definitively less in their lens eyes than in their naked eyes (P < 0.001).
The mechanism by which OK lenses might control myopia is still under debate. The most strongly supported hypothesis is based on the animal studies by Smith et al. [16] who demonstrate that the peripheral retina has a greater influence on axial eye growth in the developing eye than was previously appreciated. Inducing hyperopic defocus in the peripheral retina in animal models induces axial eye growth and the development of myopia, whereas myopic defocus in the peripheral retina reduces eye growth and hyperopia [17].
Many studies have compared and reported the effectiveness of OK lenses and other treatments. For example, Swarbrick et al. [12] report an increase in axial length of 0.09 ± 0.09 mm in a control group that wore RGP lens and no change in their OK lens group over a one-year period. Zhu et al. [18] report that the increase in axial length after one year was 0.16 ± 0.17 mm in an OK group and 0.39 ± 0.21 mm in a control group that wore glasses. Pauné et al. [19] also report one-year axial length increase of 0.15 ± 0.10 mm in an OK group and 0.26 ± 0.15 mm in a control group that wore soft radial refractive gradient contact lenses. Although these studies did vary in patient demographics such as initial age, race/ethnicity, study period, and method of treatment in the control group, the conclusions are nearly identical that the OK lens was more successful in controlling myopia than other treatments, either physical and medical.
However, these studies suggest that there is an uncontrolled variable called “inter-subject difference” as well as the differences in the baseline between individuals who did and did not wear the OK lens. At the same time, it is likely that during the follow-up periods the two groups will almost never live in exactly the same environment. Chan et al. [20] tried to compare axial length changes of genetically identical twins with same amount of near activities, one of whom was aided by a single vision lens glass (SVLs) and the other treated with orthokeratology. The report overall change in axial length of 0.52 mm (OD) and 0.70 mm (OS) in the twin with the OK lens, and 0.77 mm (OD) and 0.82 mm (OS) in the twin with SVLs. Even though genetic differences had been ruled out, environmental differences still could not be.
However, using a contralateral eye study design prevented the influence of potential confounding factors. It is very important to see the changes in biometry over time with nearly all variables controlled. Our study is the first to satisfy this requirement.
Some environmental factors like excessive near work could have accelerated myopic progression of some children in our study. Although all environmental factors of subjects could not be assessed by tools like a questionnaire, the two eyes of each subject were in the same environment during the same period of time, whether that involved near work or not. So, it is meaningful that with different interventions (one with OK lens and one untreated) each of the two eyes changed differently.
In addition, our study compared the axial growth rate in the two eyes of each of the same subjects with and without OK lens. Because we utilized the same subject’s two eyes for the study and the control conditions, we could use paired statistics to significantly reduce the required number of subjects while retaining statistical power. Furthermore, because of the contralateral eye study design, we did not need concern ourselves with balance between the treatment and control eyes.
In our study, the one-year axial length increase of 0.07 ± 0.21 mm in the OK group and 0.36 ± 0.23 mm in the control group was a stronger inhibitory effect than previous studies. Although we cannot explain these differences, they do strongly support the positive effect that orthokeratology can achieve.
When the children with monocular myopia visited our clinic, the axial lengths in their myopic eyes were significantly greater than the lengths in their contralateral eyes (P < 0.001). We recommended wearing monocular OK lenses based on previous studies that inhibiting axial elongation can prevent progression of myopia.
Deng et al. [21] report that, for most subjects in the COMET (Correction of Myopia Evaluation Trial) cohort in children with myopic anisometropia, during the period of fast progression and eventual stabilization myopia and axial length progressed at similar rates in both the myopic and emmetropic eyes.
Thus, it is justifiable to analyze the differences over time in axial length in myopic eyes wearing OK lenses and naked emmetropic eyes even when subjects have myopic anisometropia and aniso-axial length at baseline [21]. In our study, the OK lens group showed less axial elongation than the control group, confirming the effectiveness of OK lenses. Previous studies of myopia control using OK lenses have used either glasses or soft contact lenses as the control condition [12, 18, 19].
There is a moral problem with performing monocular myopia correction for research purposes in children with bilateral myopia. In addition, the children may not have binocular visual balance, which can lead to nonspecific symptoms including dizziness and stereopsis impairment if they have monocular correction. As such, it is practically difficult to see the “true” effects of the OK lens by having subjects wear a monocular OK lens in one eye but nothing in the contralateral eye.
However, in our study, children with monocular myopia were able to wear the OK lenses only in their myopic eyes. Their satisfaction increased with the use of the monocular OK lenses and we were able to compare the OK lenses with the no-intervention control eyes.
In humans, corneal reshaping after OK lens wear can induce myopic defocus on the peripheral retina with a flatter central curvature and steeper peripheral curvature design [22, 23]. In other words, apparent shortening of axial length early in OK lens wear may reflect the contribution of OK-induced central corneal thinning, combined with choroidal thickening or recovery owing to reduced or neutralized myopiogenic stimuli in the eye growth of myopic children [12]. Chen et al. [24] also report that the changes in axial length were significantly correlated with the changes in choroidal thickness in the OK lens group. We speculate that this may be the mechanism that underlies the myopia control effects of OK lens wear.
In conclusion, our study adds to previous findings that OK lenses retard axial elongation, and it is more meaningful because our use of OK lens and no-intervention (control) groups confirmed the sole effect of the OK lenses by using both eyes of each individual. Certain limitations exist in the present study since this is retrospective study with unavoidable selection bias, so additional prospective studies with more participants are necessary.
References
Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR, et al. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol. 2004;122:495–505.
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in china: a randomized clinical trial. JAMA. 2015;314:1142–8.
Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739–48.
Li SM, Ji YZ, Wu SS, Zhan SY, Wang B, Liu LR, et al. Multifocal versus single vision lenses intervention to slow progression of myopia in school-age children: a meta-analysis. Surv Ophthalmol. 2011;56:451–60.
Li SM, Kang MT, Wu SS, Meng B, Sun YY, Wei SF, et al. Studies using concentric ring bifocal and peripheral add multifocal contact lenses to slow myopia progression in school-aged children: a meta-analysis. Ophthalmic Physiol Opt. 2017;37:51–9.
Saw SM, Gazzard G, Au Eong KG, Tan DT. Myopia: attempts to arrest progression. Br J Ophthalmol. 2002;86:1306–11.
Song YY, Wang H, Wang BS, Qi H, Rong ZX, Chen HZ. Atropine in ameliorating the progression of myopia in children with mild to moderate myopia: a meta-analysis of controlled clinical trials. J Ocular Pharmacol. 2011;27:361–8.
Huang J, Wen D, Wang Q, McAlinden C, Flitcroft I, Chen H, et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology. 2016;123:697–708.
Si JK, Tang K, Bi HS, Guo DD, Guo JG, Wang XR. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci. 2015;92:252–7.
He M, Du Y, Liu Q, Ren C, Liu J, Wang Q, et al. Effects of orthokeratology on the progression of low to moderate myopia in Chinese children. BMC ophthalmol. 2016;16:126.
Sun Y, Xu F, Zhang T, Liu M, Wang D, Chen Y, et al. Orthokeratology to control myopia progression: a meta-analysis. PloS One. 2015;10:e0124535.
Swarbrick HA, Alharbi A, Watt K, Lum E, Kang P. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology. 2015;122:620–30.
Cheung SW, Cho P, Fan D. Asymmetrical increase in axial length in the two eyes of a monocular orthokeratology patient. Vision Res. 2004;81:653–6.
Hashemi H, Khabazkhoob M, Emamian MH, Shariati M, Abdolahi-nia T, Fotouhi A. All biometric components are important in anisometropia, not just axial length. Br J Ophthalmol. 2013;97:1586–91.
Zeng J, Cui Y, Li J, Xie W, Li Z, Zhang L, et al. Correlation of axial length and corneal curvature with diopter in eyes of adults with anisometropia. Int J Clin Exp Med. 2015;8:13639–43.
Smith EL 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49:2386–92.
Liu Y, Wildsoet C. The effect of two-zone concentric bifocal spectacle lenses on refractive error development and eye growth in young chicks. Invest Ophthalmol Vis Sci. 2011;52:1078–86.
Zhu MJ, Feng HY, He XG, Zou HD, Zhu JF. The control effect of orthokeratology on axial length elongation in Chinese children with myopia. BMC ophthalmol. 2014;14:141.
Paune J, Morales H, Armengol J, Quevedo L, Faria-Ribeiro M, Gonzalez-Meijome JM. Myopia control with a novel peripheral gradient soft lens and orthokeratology: a 2-year clinical trial. Biomed Res Int. 2015;2015:507572.
Chan KY, Cheung SW, Cho P. Orthokeratology for slowing myopic progression in a pair of identical twins. Cont Lens Anterior Eye. 2014;37:116–9.
Deng L, Gwiazda J, Manny RE, Scheiman M, Weissberg E, Fern KD, et al. Limited change in anisometropia and aniso-axial length over 13 years in myopic children enrolled in the correction of myopia evaluation trial. Invest Ophthalmol Vis Sci. 2014;55:2097–105.
Kang P, Swarbrick H. Peripheral refraction in myopic children wearing orthokeratology and gas-permeable lenses. Optom Vis Sci. 2011;88:476–82.
Lyu Byul, Hwang Kyu Yeon, Kim Sun Young, Kim Su Young, Na Kyung Sun. Effectiveness of toric orthokeratology in the treatment of patients with combined myopia and astigmatism. Korean J Ophthalmol. 2016;30:434–42.
Chen Z, Xue F, Zhou J, Qu X, Zhou X. Effects of orthokeratology on choroidal thickness and axial length. Optom Vis Sci. 2016;93:1064–71.
Acknowledgments
None.
Funding
The authors have no financial or proprietary interest in any of the materials or methods discussed in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
M. Na, None; A. Yoo, None.
About this article
Cite this article
Na, M., Yoo, A. The effect of orthokeratology on axial length elongation in children with myopia: Contralateral comparison study. Jpn J Ophthalmol 62, 327–334 (2018). https://doi.org/10.1007/s10384-018-0573-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-018-0573-x