Abstract
Purpose
To describe tumor response and complications after selective ophthalmic arterial injection (SOAI) of melphalan for treatment of intraocular retinoblastoma.
Methods
A retrospective review of 17 eyes (12 patients) treated with SOAI of melphalan from January 2010 through December 2013 at Chang Gung Memorial Hospital.
Results
SOAI was successfully performed in 49 of 54 attempts. Six eyes underwent SOAI as the primary treatment and 11 eyes had previously been treated with other treatment modalities. Subsequent to SOAI, tumor regression was observed in 12 of 17 eyes, and vitreous seeding with complete or partial regression in ten of 15 eyes. Globe salvage was achieved in ten of 17 eyes, with three of four in group B and group C eyes, and seven of 13 in group D and group E eyes. Pancytopenia accompanied by neutropenic fever was observed in one case. Twelve eyes had local side effects, including lid edema (two eyes), third cranial nerve palsy (two eyes), sixth cranial nerve palsy (one eye), chorioretinal atrophy (six eyes), retinal arterial occlusion (three eyes), retinal detachment (one eye), and vitreous hemorrhage (seven eyes). Three cases with high-risk features, according to the histopathologic examination, had metastatic disease, and two of them died.
Conclusions
SOAI of melphalan is an effective treatment for intraocular retinoblastoma, achieving high globe salvage in cases of advanced disease, but can be associated with significant ocular complications. Repetitive SOAI with delayed enucleation could increase the risk of metastasis when used in high-risk cases. Therefore, clinicians should consider the benefits and potential risks and use this new technique with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinoblastoma, the most frequently occurring primary intraocular cancer [1], annually affects approximately 8.58 per million children under the age of 5 years in Taiwan [2]. Conducting the treatment for retinoblastoma is challenging, and numerous therapeutic modalities have been applied. Management of retinoblastoma includes enucleation, external beam radiotherapy (EBRT), systemic chemotherapy, and local treatments such as laser photocoagulation, thermotherapy, and cryotherapy. However, most of these therapies include certain limitations and unwanted complications [3, 4]. In the past, enucleation was a common form of management for patients with advanced retinoblastoma. Within the recent decade, numerous clinicians have sought to increase the possibility of preserving the eye and salvaging useful vision. Considering the long-term consequences of EBRT, multiagent systemic chemotherapy is currently the commonly used frontline management option for intraocular retinoblastoma, because it avoids the side effects caused by EBRT. Long-term toxicities, such as ototoxicity and nephrotoxicity, or secondary cancer, have been mentioned in the literature, but have rarely occurred [5, 6]. In 2004, Japanese investigators published studies describing a novel approach for delivering chemotherapeutic agents directly into the ophthalmic artery by occluding the distal flow in the internal carotid artery by means of balloon catheterization [7, 8]. Western specialized centers subsequently followed the progress of this new technique and reported high globe salvage rates and few local or systemic side effects [9–11]. Clinicians worldwide have used selective ophthalmic arterial injection (SOAI) and reported their own experiences. Therefore, we introduced SOAI into Taiwan and evaluated the tumor control, globe preservation rate, and complications of SOAI. Hence, we conducted a 4-year retrospective review to summarize our results of using SOAI on selected patients with newly diagnosed intraocular retinoblastoma and on those with refractory or relapsed retinoblastoma at Chang Gung Memorial Hospital, a tertiary referral hospital in Taiwan.
Patients and methods
All patients with ocular retinoblastoma treated with SOAI of melphalan at Chang Gung Memorial Hospital from January 2010 through December 2013 were included in this study. The study, which adhered to the tenets of the Declaration of Helsinki, was approved by the institutional review board of Chang Gung Memorial Hospital, which allowed retrieval of patient data and review of the medical information. The collected data included information on demographics, clinical findings, management, and treatment outcomes. All previous treatments for the eye as well as additional treatments during or after SOAI were recorded. All the patients underwent a comprehensive ocular examination under general anesthesia before SOAI and were assessed based on the International Classification of Retinoblastoma (ICRB) and Reese–Ellsworth classification. The clinical findings were recorded using fundus photography (RetCam camera; Clarity Medical Systems, Pleasanton, CA, USA). The patients and their families were informed of the possible risks and benefits of SOAI, and informed consent was obtained before each procedure.
The SOAI procedure was performed under general anesthesia in the angiographic suite by neuroradiologists. The right femoral artery was punctured, and a 4-French (F) arterial sheath placed therein. Anticoagulation was obtained using liter bags of saline containing 10,000 U of heparin in a flush system. A 4-F (1.3-mm diameter) catheter was guided into the ipsilateral internal carotid artery. To visualize the eye and cerebral vasculature and choose the appropriate path for accessing the ophthalmic artery, serial arteriograms were taken. A 1.5-F microcatheter (Marathon Flow-Directed Micro Catheter; ev3 Neurovascular, Irvine, CA, USA) was subsequently inserted into the 4-F catheter to access the origin of the ophthalmic artery of the treated eye, and a confirmatory angiogram was taken. Melphalan (5 mg/20 mL) was administered through the microcatheter into the ophthalmic artery by slow infusion within 30 min. In patients with bilateral retinoblastoma who had both eyes treated in a single session, the contralateral ophthalmic artery was catheterized using the same technique and the procedure was repeated. After the procedure was completed, we withdrew the catheters, removed the femoral sheath, and accomplished hemostasis of the femoral artery by manual compression.
The patient was examined under general anesthesia 3–4 weeks after SOAI to evaluate the response, which was documented using fundus photography (RetCam camera). A subsequent session of SOAI was arranged for the patients according to the tumor response. If necessary, local treatments, including cryotherapy, transpupillary thermotherapy, and endolaser treatment were applied to localized lesions. Eyes exhibiting active vitreous seeding received an intravitreal injection of 5–10 μg/0.05 mL melphalan. Eyes with refractory tumors or persistent vitreous seeding were treated with EBRT or enucleation.
Results
Patient characteristics
Table 1 summarizes the characteristics of the 12 patients who received SOAI at Chang Gung Memorial Hospital within the study period. The mean patient age at diagnosis was 17.9 months (median 13, range 2–50). Of the 12 patients, five (41.7 %) had unilateral disease and seven (58.3 %) had bilateral disease. Of the seven bilateral cases, five had both eyes treated with SOAI; one had the opposite eye enucleated; and one had a relatively localized disease (ICRB group A), which was successfully treated with local treatment. Thus, 49 successful procedures of 54 SOAI trials were performed on 17 eyes, with a success rate of 90.7 %. In 1 procedure, the ophthalmic artery was accessed successfully through the middle meningeal artery, which provides collateral blood flow to the ophthalmic artery from the external carotid artery. Five procedures conducted on three patients were unsuccessful because of contrast reflux into the internal carotid artery and poor perfusion through the ophthalmic artery.
On the basis of the ICRB classification, the initial presentation included three group B eyes, one group C eye, one group D eye, and 12 group E eyes. The additional features of the 17 treated eyes at presentation included vitreous and subretinal seeding [14 eyes (82 %)], retinal detachment [RD; nine eyes (53 %)], iris neovascularization [two eyes (12 %)], and neovascular glaucoma [NVG; one eye (6 %)]. Six eyes were newly diagnosed cases and received SOAI as the primary treatment, whereas the other 11 eyes were refractory or relapsed eyes that had a previous history of systemic chemotherapy [11 eyes (65 %)], local treatment [five eyes (29 %)], intravitreal injection of melphalan [three eyes (18 %)], or EBRT [four eyes (24 %)]. Two patients with bilateral advanced disease had bilateral RD (group E) at the initial presentation, and two of the eyes underwent scleral buckling for persistent RD.
Treatment outcomes
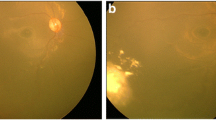
Table 2 presents the treatment course and outcomes. Each eye received one to six sessions of SOAI (mean 2.88, median 3). Subsequent to SOAI, tumor regression was observed in 12 eyes (71 %). Four eyes exhibited no regression and the tumor size increased after the procedure. One eye had a hazy cornea caused by NVG, and the condition could not be evaluated comprehensively after SOAI. In the eyes with vitreous seeding, three eyes exhibited complete regression, seven eyes exhibited partial regression, and four eyes displayed no prominent response to SOAI. Figure 1 shows a representative case before and after treatment. Eleven of the 17 eyes received concurrent treatments during or after SOAI, including local treatment [six eyes (35 %)], adjuvant systemic chemotherapy [two eyes (12 %)], and intravitreal injection of melphalan [five eyes (29 %)]. Five eyes (29 %) received EBRT because of advanced disease or persistent vitreous seeding. Seven eyes required enucleation. The indications for enucleation included NVG, vitreous hemorrhage obscuring tumor visualization, and tumor progression. For the enucleated eyes that underwent histopathologic examination, we observed no viable tumor in two eyes, viable tumors confined to the retina in two eyes, and high-risk features for metastasis (choroid and optic nerve invasion) in three eyes. These three patients exhibited metastasis to the central nervous system, and two patients died despite having undergone chemotherapy after enucleation.
Response to selective ophthalmic arterial injection (SOAI) for retinoblastoma. (a) A 1-year-old patient with bilateral retinoblastoma, who had previously received systemic chemotherapy, had a large, partially regressed tumor on the temporal side, with disc traction and a retinal tear in the right eye. (b) Multiple midperipheral tumors were present in the left eye. (c, d) After three doses of SOAI, complete regression of the tumors in both eyes was observed. Retinal arterial occlusion accompanied by a pale disc and diffuse chorioretinal atrophy occurred in the right eye (c)
All patients had a median follow-up of 22 months (mean 21.3, range 5–43). Globe salvage was achieved in ten of 17 eyes (59 %), comprising four of the six newly diagnosed eyes (67 %) and six of the 11 refractory or relapsed eyes (55 %). Among the eyes that were spared enucleation, three of four (75 %) were from groups B and C, and seven of 13 (54 %) were from groups D and E. One eye initially contained a single solitary tumor (group B), but continued to progress, and vitreous seeds occurred before SOAI. Despite treatment with multiple therapies, the progression continued and the eye was eventually enucleated.
Because of their young age, most of the patients did not undergo a formal visual acuity measurement. Vision was followed up according to the family report and the response to light, fixation, and following an object. Patient 4, who had initially presented with group-D disease, exhibited the best corrected visual acuity of 0.9 and a stable condition at the final follow-up examination.
Complications
Table 2 summarizes the complications experienced by each patient after SOAI. No life-threatening or severe systemic complications occurred, such as stroke, cerebral infarction, or sepsis. Pancytopenia accompanied by neutropenic fever was observed 15 days after the third SOAI treatment in patient 3. The patient was admitted to hospital and blood transfusion was required. No patient developed secondary neoplasms during the follow-up period.
Two eyes developed transient lid edema combined with forehead redness and conjunctiva congestion. Patient 1 suffered from right third cranial nerve palsy after the final (third) SOAI session, and patient 3, from left third and sixth cranial nerve palsy after the second SOAI session. The extraocular movement and ptosis recovered completely within 1–2 months. Patient 3 then received another three courses of SOAI, and no cranial nerve palsy occurred. Seven eyes were observed to have vitreous hemorrhage in the follow-up examination under general anesthesia. Of these patients, one gradually resolved, and three had accompanying NVG. Five of these patients required enucleation. Patient 5 received scleral buckling for the left eye and the retina was attached before SOAI, but RD was observed after the procedure. No break was observed after careful examination, and the RD was possibly caused by vitreoretinal traction. Retinal arterial occlusion was observed by fundoscopy in three eyes. Of those three eyes, two exhibited diffuse arterial occlusion with a pale disc and prominent chorioretinal atrophy, and one had retinal arterial occlusion over the inferior branch. Six patients experienced chorioretinal atrophy. Five of them exhibited diffuse attenuation of the choroidal vessels with retinal pigment epithelium (RPE) loss, and one presented with only sector changes in the inferior area.
Discussion
Selective ophthalmic arterial injection has recently gained considerable attention because of positive reports indicating that it provides effective tumor control with globe salvage and few side effects [11, 12]. In our case series, we observed a 59 % globe salvage rate and a 71 % tumor response rate when SOAI was applied as a component of multimodal therapy. Patients with newly diagnosed disease exhibited a slightly higher rate of globe preservation than did those with refractory or relapsed disease. However, we noted significant local adverse events during follow-up. Three patients had metastatic disease, and two of them died because of direct invasion of the central nervous system.
Reviewing the literature, we found different chemotherapy agents and doses used for SOAI and numerous additional therapies. After a relatively long-term follow-up, Gobin et al. [10] reported that 70 % of their patients who received SOAI combined with other treatment modalities were spared the need to undergo enucleation or EBRT. They excluded eyes with NVG or suspected optic nerve invasion. They used multiple drugs for SOAI, including melphalan, topotecan, carboplatin, and methotrexate. They also routinely performed cryotherapy or laser ablation for all tumors before SOAI. Suzuki et al. [12] reported 408 eyes treated with balloon catheter and melphalan between 1988 and 2007. Most of their cases were initially treated with EBRT or chemotherapy. Fifty eyes, mainly bilateral cases, were treated with SOAI as the primary treatment. The globe salvage rate was similar to that of our series. They reported that more than half of the eyes without macular involvement maintained a visual acuity > 0.5.
For patients with advanced disease, even aggressive multimodal therapy results in a high rate of treatment failure, and EBRT or enucleation is eventually required [13, 14]. Most of our cases [13 of 17 (76 %)] had advanced group D or group E disease. With the aid of SOAI, we achieved a globe salvage rate of 54 % for the advanced cases. Six cases with group E disease required enucleation because of the limited response to SOAI involving progression or recurrence (n = 5) and NVG with vitreous hemorrhage obscured fundus visualization (n = 1). In our series, although the main tumors typically responded positively to SOAI, vitreous seeding remained a challenge in the treatment of advanced intraocular retinoblastoma. Most of the patients with vitreous seeding [ten of 14 (71 %)] exhibited partial or no prominent regression after SOAI. We cannot describe the response of subretinal seeding accurately because numerous concurrent treatments were used; however, we observed subretinal fluid absorption with regressed subretinal seeding in most of the cases. Previous studies have indicated that vitreous seeding is not quite responsive to SOAI [12]. By applying SOAI combined with other treatment modalities, Shields et al. [15] reported a 67 % rate of successful control of vitreous seeds. For eyes with both vitreous and subretinal seeding, Abramson et al. [16] reported a globe salvage rate of 80 % in treatment-naive eyes and of 54 % in eyes that had received prior treatments during a 2-year follow-up. In the case series reported by Vajzovic et al. [17], three of 12 eyes (25 %) with vitreous seeds that were treated with SOAI received enucleation because of tumor recurrence. A histopathologic examination of the enucleated eyes revealed viable vitreous seeds, which thus represented a limited response to SOAI [18]. Kim et al. [19] reported similar findings for two enucleated eyes after failure of SOAI; the eyes had received melphalan doses as high as 8 mg per treatment.
Regarding vitreous seeding, possible causes of the limited effect of SOAI include the avascular characteristic of the vitreous cavity and poor penetration of the chemotherapeutic agents [15, 19]. Resistance to single-agent chemotherapy may also be a concern. Two cases in our series exhibited prominent tumor regression and a stable condition after the initial three to four courses of SOAI. We repeated two courses of SOAI because of tumor regrowth accompanied by seed recurrence. The effects appeared to be limited and the disease continued to progress (Fig. 2). These two eyes were eventually enucleated. Although the ideal dose and number of SOAI sessions were not effectively identified, we discovered that most tumors demonstrated the greatest response after approximately three sessions of SOAI, and the procedure may be less effective if repeated more than three times. We treated the cases that exhibited limited response and persistent vitreous seeds with other treatment modalities, including intravitreal injection of melphalan or EBRT.
Limited response to selective ophthalmic arterial injection (SOAI) for recurrent retinoblastoma. (a) A 2-year-old patient with retinoblastoma, who had previously received systemic chemotherapy, presented with a partially regressed tumor near the disc and another active tumor at 3 o’clock with some vitreous seeds in the left eye. (b) Subsequent to four doses of SOAI, the tumors and seeds regressed. (c) Three months later, tumor regrowth was detected near the disc with recurrence of subretinal and vitreous seeds. (d) After two repeated doses of SOAI and administration of intravitreal injection of melphalan, two enlarged tumors were observed near the disc with an increased number of subretinal and vitreous seeds, and complicated with vitreous hemorrhage
Three of the cases had bilateral disease and metastasis to the central nervous system, and two of those cases died. One patient presented with tumor recurrence, and another two refractory cases had received aggressive multimodal treatments before SOAI. Patients 5 and 6 resisted all treatment modalities including EBRT and chemotherapy, and after treatment with SOAI, the disease continued to progress, ultimately leading to enucleation. One enucleated eye from each patient revealed choroid and optic nerve invasion, which represent the high-risk features of metastasis [20, 21]. High-risk features are frequently associated with advanced retinoblastoma. More than 10 % of the cases in group D and more than 50 % of those in group E exhibited at least one high-risk feature [22]. High-risk features are difficult to predict in newly diagnosed cases, even when magnetic resonance imaging is used, and are most effectively defined by histopathologic examination of the enucleated eye [23, 24]. SOAI for treatment of advanced retinoblastoma should be applied with caution, because it may be insufficient for treating remote subclinical metastatic disease. Patients with very advanced disease, such as suspected invasion to optic nerve, should be excluded. Resistance to single-agent chemotherapy and incomplete response to vitreous seeding should also be a concern. In our series, enucleation was unacceptable for some parents, especially in the bilateral advanced cases. Repeated SOAI to preserve the eyeball with delayed enucleation could increase the risk of extraocular extension or mask the histopathologic findings as a result of inaccurate staging [5, 25, 26]. Enucleation remains unpreventable for certain cases with advanced retinoblastoma [27].
We observed certain short-term local effects after SOAI, including lid edema with congestion, forehead redness, and cranial nerve palsy, which previous studies have also mentioned [17, 28–31]. These transient side effects disappeared completely within 1–2 months. We observed chorioretinal atrophy, which presented slowly and persisted in six of the 17 eyes (35 %) in our series. This result was similar to that reported by Muen et al. [29], who observed chorioretinal atrophy in seven of 15 cases (47 %). Shields et al. [28] also observed RPE mottling in nine of 17 cases (52 %), five of which slowly evolved into choroidal atrophy. The cause of chorioretinal atrophy is unclear. Possible causes may be the direct cytotoxic effect of melphalan on the choroidal vascular bed or the RPE [29, 32 ]. The diffuse and homogeneous changes also suggest its relation to the toxic effects of chemotherapy [28].
Vascular insults, such as vessel stenosis or occlusion, may occur following SOAI and may contribute to ischemic changes in the choroid and retina. Vajzovic et al. [17] observed one case of Purtscher-like retinopathy resulting from embolization. Shields et al. [28] reported four cases complicated with ophthalmic artery occlusion after SOAI that had presented as central retinal arterial occlusion, branch retinal arterial occlusion, or choroidal atrophy. Subsequent histopathology reports on enucleated eyes revealed choroidal and retinal atrophy caused by vascular compromise. They also observed unexpected intravascular foreign material within the thrombi of the ciliary artery, intrachoroidal vessels, and central retinal vessels, or within the regressed tumor, which may have been related to embolization events [33]. In our series, three eyes exhibited retinal arterial occlusion combined with chorioretinal atrophy. The implication of chorioretinal atrophy and vessel occlusion may be profound in certain patients, particularly in bilateral advanced cases.
In our series, seven eyes had complications associated with vitreous hemorrhage after SOAI. Six of these eyes were advanced group E cases; the other eye, classified as having group B disease, initially progressed and revealed a vitreous hemorrhage with limited regression after SOAI was administered. Five of the seven eyes ultimately underwent enucleation. Previous studies have reported vitreous hemorrhage after SOAI in 13–27 % of advanced cases, most of which required enucleation [17, 29, 30, 34]. Our results presented a higher rate of vitreous hemorrhage. Four eyes received multiple treatments before SOAI, including EBRT. Three cases exhibited vitreous hemorrhage accompanied by NVG. Although the exact mechanism of vitreous hemorrhage is unknown, the cause may be related to ischemic retina with fragile neovascularization and the toxicity of chemotherapeutic agents [34]. Muen et al. [29] reported that three cases previously treated with EBRT experienced severe vitreous hemorrhage after SOAI. They suggested that SOAI could disturb the choroidal vascular system and exacerbate radiation angiopathy. Vitreous hemorrhage is a serious complication, particularly in advanced cases with the possibility of progression, and persistent vitreous hemorrhage that obscures fundus visualization indicates enucleation.
Our study has several limitations, including its small sample size and retrospective characteristic, and the association of SOAI with other concurrent therapies. We could not accurately evaluate the effect of SOAI on intraocular retinoblastoma on its own. However, previous studies on retinoblastoma treatment have been limited by similar shortcomings. Although our data revealed the treatment results and complications, further follow-up is necessary to evaluate the long-term effects of SOAI.
In conclusion, we have demonstrated that SOAI of melphalan is a successful globe-salvage therapy in treating advanced intraocular retinoblastoma when combined with other treatment modalities. Rare systemic complications were observed in this series, and significant ocular toxic effects that were occasionally vision-threatening were discovered. Despite the effective tumor control of SOAI, we suggest using this new therapy with caution for advanced cases, particularly for patients with high-risk features and potential for metastasis. The increased risk of metastasis resulting from repetitive SOAI with delayed enucleation could threaten the patient’s life. EBRT could be considered as a globe-salvage method for advanced cases with profound vitreous seeding, and enucleation continues to be a life-saving technique for the treatment of advanced intraocular retinoblastoma.
References
Kivela T. The epidemiological challenge of the most frequent eye cancer: retinoblastoma, an issue of birth and death. Br J Ophthalmol. 2009;93:1129–31.
Chen YH, Lin HY, Hsu WM, Lee SM, Cheng CY. Retinoblastoma in Taiwan: incidence and survival characteristics from 1979 to 2003. Eye (London). 2010;24:318–22.
Shields CL, Shields JA. Intra-arterial chemotherapy for retinoblastoma: the beginning of a long journey. Clin Exp Ophthalmol. 2010;38:638–43.
Abramson DH. Super selective ophthalmic artery delivery of chemotherapy for intraocular retinoblastoma: ‘chemosurgery’. The first Stallard lecture. Br J Ophthalmol. 2010;94:396–9.
Shields CL, Kaliki S, Rojanaporn D, Al-Dahmash S, Bianciotto CG, Shields JA. Intravenous and intra-arterial chemotherapy for retinoblastoma: what have we learned? Curr Opin Ophthalmol. 2012;23:202–9.
Rizzuti AE, Dunkel IJ, Abramson DH. The adverse events of chemotherapy for retinoblastoma: what are they? Do we know? Arch Ophthalmol. 2008;126:862–5.
Yamane T, Kaneko A, Mohri M. The technique of ophthalmic arterial infusion therapy for patients with intraocular retinoblastoma. Int J Clin Oncol. 2004;9:69–73.
Suzuki S, Kaneko A. Management of intraocular retinoblastoma and ocular prognosis. Int J Clin Oncol. 2004;9:1–6.
Abramson DH, Dunkel IJ, Brodie SE, Marr B, Gobin YP. Superselective ophthalmic artery chemotherapy as primary treatment for retinoblastoma (chemosurgery). Ophthalmology. 2010;117:1623–9.
Gobin YP, Dunkel IJ, Marr BP, Brodie SE, Abramson DH. Intra-arterial chemotherapy for the management of retinoblastoma: four-year experience. Arch Ophthalmol. 2011;129:732–7.
Abramson DH, Dunkel IJ, Brodie SE, Kim JW, Gobin YP. A phase I/II study of direct intraarterial (ophthalmic artery) chemotherapy with melphalan for intraocular retinoblastoma: initial results. Ophthalmology. 2008;115:1398–404, 1404.e1.
Suzuki S, Yamane T, Mohri M, Kaneko A. Selective ophthalmic arterial injection therapy for intraocular retinoblastoma: the long-term prognosis. Ophthalmology. 2011;118:2081–7.
Shields CL, Honavar SG, Meadows AT, Shields JA, Demirci H, Naduvilath TJ. Chemoreduction for unilateral retinoblastoma. Arch Ophthalmol. 2002;120:1653–8.
Shields CL, Honavar SG, Meadows AT, Shields JA, Demirci H, Singh A, et al. Chemoreduction plus focal therapy for retinoblastoma: factors predictive of need for treatment with external beam radiotherapy or enucleation. Am J Ophthalmol. 2002;133:657–64.
Shields CL, Bianciotto CG, Jabbour P, Ramasubramanian A, Lally SE, Griffin GC, et al. Intra-arterial chemotherapy for retinoblastoma: report No. 1, control of retinal tumors, subretinal seeds, and vitreous seeds. Arch Ophthalmol. 2011;129:1399–406.
Abramson DH, Marr BP, Dunkel IJ, Brodie S, Zabor EC, Driscoll SJ, et al. Intra-arterial chemotherapy for retinoblastoma in eyes with vitreous and/or subretinal seeding: 2-year results. Br J Ophthalmol. 2012;96:499–502.
Vajzovic LM, Murray TG, Aziz-Sultan MA, Schefler AC, Wolfe SQ, Hess D, et al. Supraselective intra-arterial chemotherapy: evaluation of treatment-related complications in advanced retinoblastoma. Clin Ophthalmol. 2011;5:171–6.
Vajzovic LM, Murray TG, Aziz-Sultan MA, Schefler AC, Fernandes CE, Wolfe SCQ, et al. Clinicopathologic review of enucleated eyes after intra-arterial chemotherapy with melphalan for advanced retinoblastoma. Arch Ophthalmol. 2010;128:1619–23.
Kim J, Do H, Egbert P. Enucleated eyes after failed intra-arterial infusion of chemotherapy for unilateral retinoblastoma: histopathologic evaluation of vitreous seeding. Clin Ophthalmol. 2011;5:1655–8.
Shields CL, Shields JA, Baez KA, Cater J, De Potter PV. Choroidal invasion of retinoblastoma: metastatic potential and clinical risk factors. Br J Ophthalmol. 1993;77:544–8.
Shields CL, Shields JA, Baez K, Cater JR, De Potter P. Optic nerve invasion of retinoblastoma: metastatic potential and clinical risk factors. Cancer. 1994;73:692–8.
Wilson MW, Qaddoumi I, Billups C, Haik BG, Rodriguez-Galindo C. A clinicopathological correlation of 67 eyes primarily enucleated for advanced intraocular retinoblastoma. Br J Ophthalmol. 2011;95:553–8.
Wilson MW, Rodriguez-Galindo C, Billups C, Haik BG, Laningham F, Patay Z. Lack of correlation between the histologic and magnetic resonance imaging results of optic nerve involvement in eyes primarily enucleated for retinoblastoma. Ophthalmology. 2009;116:1558–63.
Eagle RC Jr. High-risk features and tumor differentiation in retinoblastoma: a retrospective histopathologic study. Arch Pathol Lab Med. 2009;133:1203–9.
Wilson MW, Haik BG, Dyer MA. Superselective intraophthalmic artery chemotherapy: what we do not know. Arch Ophthalmol. 2011;129:1490–1.
Levin MH, Gombos DS, O’Brien JM. Intra-arterial chemotherapy for advanced retinoblastoma: is the time right for a prospective clinical trial? Arch Ophthalmol. 2011;129:1487–9.
Shields CL, Shields JA. Retinoblastoma management: advances in enucleation, intravenous chemoreduction, and intra-arterial chemotherapy. Curr Opin Ophthalmol. 2010;21:203–12.
Shields CL, Bianciotto CG, Jabbour P, Griffin GC, Ramasubramanian A, Rosenwasser R, et al. Intra-arterial chemotherapy for retinoblastoma: report No. 2, treatment complications. Arch Ophthalmol. 2011;129:1407–15.
Muen WJ, Kingston JE, Robertson F, Brew S, Sagoo MS, Reddy MA. Efficacy and complications of super-selective intra-ophthalmic artery melphalan for the treatment of refractory retinoblastoma. Ophthalmology. 2012;119:611–6.
Thampi S, Hetts SW, Cooke DL, Stewart PJ, Robbins E, Banerjee A, et al. Superselective intra-arterial melphalan therapy for newly diagnosed and refractory retinoblastoma: results from a single institution. Clin Ophthalmol. 2013;7:981–9.
Venturi C, Bracco S, Cerase A, Cioni S, Galluzzi P, Gennari P, et al. Superselective ophthalmic artery infusion of melphalan for intraocular retinoblastoma: preliminary results from 140 treatments. Acta Ophthalmol. 2013;91:335–42.
Munier FL, Beck-Popovic M, Balmer A, Gaillard MC, Bovey E, Binaghi S. Occurrence of sectoral choroidal occlusive vasculopathy and retinal arteriolar embolization after superselective ophthalmic artery chemotherapy for advanced intraocular retinoblastoma. Retina. 2011;31:566–73.
Eagle RC Jr, Shields CL, Bianciotto C, Jabbour P, Shields JA. Histopathologic observations after intra-arterial chemotherapy for retinoblastoma. Arch Ophthalmol. 2011;129:1416–21.
Peterson EC, Elhammady MS, Quintero-Wolfe S, Murray TG, Aziz-Sultan MA. Selective ophthalmic artery infusion of chemotherapy for advanced intraocular retinoblastoma: initial experience with 17 tumors. J Neurosurg. 2011;114:1603–8.
Conflicts of interest
S. J. Ong, None; A. -N. Chao, None; H. -F. Wong, None; K. -L. Liou, None; L. -Y. Kao, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ong, S.J., Chao, AN., Wong, HF. et al. Selective ophthalmic arterial injection of melphalan for intraocular retinoblastoma: a 4-year review. Jpn J Ophthalmol 59, 109–117 (2015). https://doi.org/10.1007/s10384-014-0356-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-014-0356-y