Summary
Background
Laparoscopic Nissen fundoplication is considered the gold standard in surgical management of gastroesophageal reflux disease. Therefore, exhaustive scrutiny of the procedure is necessary. The aim of this study was to perform a complete and systematic literature review of laparoscopic Nissen fundoplication to summarize the evidence for safety and efficacy over time.
Methods
MEDLINE, Embase, CINAHL, the Cochrane Library, and Web of Science were searched for randomized controlled trials investigating intra- and postoperative outcomes at follow-ups between 4–6 weeks and 17 years.
Results
Among 1675 screened articles, 63 articles were identified comprising 40 trials with a total of 2619 participants. Intraoperative events included bleeding (2.9%), gastroesophageal injury/perforation (0.9%), and spleen injury/splenectomy (0.9%). One-year clinical follow-up presented the following: dysphagia (22.4%), heartburn or epigastric/sternal pain (15.1%), gas bloating (30.1%), and inability to vomit/belch (16.4%). These outcomes displayed a U-shaped curve with a minimum of symptoms at 1 year. At 10 years postoperatively, clinical outcomes deteriorated, demonstrating dysphagia (45.3%), heartburn or epigastric/sternal pain (30.9%), inability to vomit/belch (48.8%), and gas bloating (44.4%). Furthermore, the surgical benefit seems to dissipate at 17 years. At 1 and 10 years after surgery, reoperation rates were 6.7% and 16.3%, whereas proton pump inhibitor (PPI) use was at 12.3% and 23.3%, respectively.
Conclusion
The performance of Nissen fundoplication declines over time, as demonstrated by increased PPI medication usage for recurrent symptoms and an increased reoperation rate reaching a combined 39.6%, representing failures after 10 years. The complication rates are dominated by dysphagia, gas bloating, inability to belch/vomit, and/or recurrent reflux symptoms with heartburn.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
1.
This review of laparoscopic Nissen fundoplication (LNF) is the first to cover 63 articles representing 40 different randomized trials including 2619 patients and synthesizing both intra- and postoperative endpoints using specific follow-up timepoints to showcase the safety and performance of LNF from both a short- and long-term perspective, unlike previous reviews, which have generally combined different timepoints into postoperative follow-up.
-
2.
Publications based on single studies and especially retrospective studies often have lower-quality data and more missing patients compared to randomized studies, where both the financial resources and study efforts are higher. Therefore, a systematic review of only randomized articles increases the strength of the data.
-
3.
By scrutinizing the evidence from trials published over the past 25 years, this review was able to show that the performance of LNF declines over time, as shown by increased use of proton pump inhibitor (PPI) medication to manage recurrent symptoms and the increased complication rate leading to more reoperations. Furthermore, this review showcased that dysphagia and recurrent reflux symptoms seem to be the main causes of reoperation with LNF. In addition, it also became apparent that clinical outcomes deteriorate 10 years postoperatively and that the surgical benefit of LNF seems to dissipate at 17 years.
Introduction
Gastroesophageal reflux disease (GERD) results from reflux of gastric content into the esophagus, which may cause troublesome symptoms or complications [1]. Heartburn and regurgitation are typical symptoms of GERD, with esophagitis and Barrett’s esophagus as potential complications that develop over time [1]. Although there is regional variation in prevalence, GERD is a common condition worldwide, with more than a billion cases [2]. Furthermore, there are indications that the global burden is increasing [2].
Available treatment strategies include a spectrum of interventions such as lifestyle modifications, medical therapy, and anti-reflux surgery [1]. Indications for surgical treatment include persistent symptoms despite optimally dosed medical therapy or reluctance regarding long-term medication use [1]. Anti-reflux surgery comprises several techniques, but the current standard is laparoscopic fundoplication [3]. The most frequently employed technique, which is considered the gold standard, is laparoscopic Nissen fundoplication (LNF) [1, 3]. This involves a complete (360°) fundal wrap around the lower esophageal sphincter (LES) and, unsurprisingly, it is extensively reported in the literature [4,5,6,7,8,9,10].
LNF is generally viewed as a safe and effective treatment method for patients with GERD, although it is, as is any other procedure, associated with certain complications and side effects [3]. Furthermore, the evidence is inconclusive despite the plethora of literature on the matter [4,5,6,7,8,9,10]. To circumvent the disadvantages associated with LNF, other surgical options have been developed, such as the Toupet fundoplication technique that utilizes a more reserved 270° fundal wrap [3,4,5,6,7, 9, 10]. However, these alternatives have their own challenges in terms of balancing the respective benefits and harms, resulting in LNF’s maintained popularity [4,5,6, 8,9,10].
Amidst the wide range of published literature on LNF, questions remain regarding the effectiveness of the technique and the need for exhaustive scrutiny of the procedure that collates the available empirical evidence.
Objective
The aim of this study was to perform a systematic literature review to summarize the evidence regarding the long-term postoperative safety and performance of LNF in adults with GERD.
Methods
This systematic literature review was conducted by including elements of the review process outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [11]. The protocol was registered at www.researchregistry.com (Identification number: Reviewregistry1176). In this review, only data pertaining to LNF are presented, without any comparator treatment modalities. Since LNF is currently the most often conducted anti-reflux procedure globally, the purpose of this style of presentation is to enrich clinical knowledge with a specific focus on LNF safety and efficacy. Furthermore, although there are several systematic literature reviews that focus on LNF, the included studies in these reviews are not recent (i.e., not from within the past 10 years), and the additional information provided in our review may confirm or provide additional context based on the latest evidence.
Eligibility criteria
-
Study design: randomized controlled trial (RCT).
-
Participants: adults diagnosed with GERD.
-
Intervention: LNF to treat GERD.
-
Comparator: other surgical procedures, such as variations of LNF and open surgery, and medication for management of GERD.
-
Follow-up periods: short-term follow-up of 1 month, 6 weeks, and 6 months. Long-term follow-up of 1 year, 5 years, and ≥ 10 years.
-
Outcomes:
-
Intraoperative outcomes: splenic injury, splenectomy, gastroesophageal injury, perforation, liver injury, bleeding, infection, pneumothorax, other respiratory-related complications, conversion to open surgery, and death due to surgery.
-
Postoperative outcomes (short- and long-term follow-up): odynophagia, dysphagia, stenosis, gas bloating, vomiting, regurgitation, inability to vomit/belch, heartburn, epigastric/sternal pain, esophageal spasm, reoperation, reasons for reoperation, use of proton pump inhibitors (PPIs), percentage of overall time with pH < 4 on 24-hour monitoring, DeMeester score, LES pressure, endoscopy (for monitoring esophageal mucosal injury), Gastroesophageal Reflux Symptom Scale (GERSS), health-related quality of life (HRQOL), and the General Health Short Form 36 (GH-SF 36).
-
-
Context: clinical and community settings, regardless of geographical location.
-
Published full-text article in English.
Search strategy
Searches were conducted in MEDLINE (Ovid), Embase, CINAHL, the Cochrane Library, and Web of Science up until January 20, 2023. The search was performed by medical information experts from the Karolinska Institutet library. No limitations regarding publication dates were implemented. Reference lists of the selected eligible studies were manually searched for other relevant studies. See Appendix A for the detailed search strategy.
Selection of studies
Studies were selected via a thorough process facilitated by the program EndNote™ (Clarivate, Philadelphia, United States of America). First, duplicates were removed by EndNote’s built-in function. Second, titles and/or abstracts of the studies were screened by one reviewer (JH). Third, one reviewer (JH) assessed the eligibility of full-text articles using the eligibility criteria listed above. The study was considered the unit of interest and not each published article. Therefore, articles were collated if they originated from the same study.
Data extraction
An electronic data extraction form was developed and used to obtain data. Methods, LNF (intervention), participants, and outcomes in the LNF group were the focus. Data extraction was performed by one reviewer (JH). The template form as well as the data extracted and used are available upon request. If articles repeated results from the same study, they were compared, and data were extracted from only one of them.
Appraisal
Included studies were assessed using the Joanna Briggs Institute (JBI) critical appraisal tool for RCTs [12]. The appraisal was performed independently by two reviewers (JH and SD). Any disagreement was resolved through discussion until consensus was reached.
Data analysis
The objective of this review was to synthesize clinical evidence solely on LNF to understand the clinical safety and performance of this procedure. As previously stated, the comparator arms were not included. Therefore, the scope of this systematic literature review excluded any comparative analyses such as meta-analysis. Descriptive statistics were used to present the intraoperative, clinical, and objective postoperative results for patients treated with LNF. Dichotomous data were collated for intraoperative and postoperative clinical outcomes. If needed, the data were recalculated as the number of events or percentages. Summary results included only studies with reported outcome data and corresponding sample size. A subanalysis was performed on a subset of studies comparing 10- and 17-year follow-up, where patients acted as their own control. Postoperative PPI use and reoperation were combined to represent treatment failure. Continuous data were collated for objective postoperative outcomes and calculated as weighted averages. The weights were calculated according to each individual study’s sample size. Regarding the percentage of overall time with pH < 4, a normal value was defined as < 4.5% [13]. A DeMeester score of < 14.72 was defined as the normal value [13]. Stenosis and esophageal spasm were not reported in the included studies and several postoperative outcomes (i.e., LES pressure, endoscopy, GERSS, HRQOL, and GH-SF 36) were inconsistently reported for the selected follow-ups. These outcomes were subsequently not analyzed nor further reported in this systematic literature review. See Table B.1 for further details.
Results
Results of the search
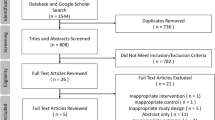
A total of 2524 records were identified through searching databases, of which 1675 were screened after removal of duplicates. During screening, 1572 records were excluded, and 103 full-text articles were assessed for eligibility. Eight additional records were identified through citation searching, of which seven were assessed for eligibility. In total, 63 articles (with data from 40 RCTs) met the inclusion criteria and were included [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76]. The flow diagram (Fig. 1) shows the work process for study selection and reasons for exclusion of full-text articles.
Included studies
Characteristics of included studies are summarized in Table 1. This systematic literature review included a total of 2619 participants treated with LNF. When presented, the study population was comprised of between 37% and 75% men, with a mean age of 42.9 to 59.1 years (median 42.5 to 52.0 years). The studies were conducted on five continents, mostly in Europe, and published between 1997 and 2022. Without further description, the comparator was one of the following: open Nissen fundoplication [14, 27, 29, 33, 36, 42, 74], laparoscopic Hill repair [19], laparoscopic anterior 90° fundoplication [57, 72], laparoscopic 120° anterior fundoplication [28], laparoscopic 180° anterior fundoplication [20, 25, 56, 65], laparoscopic 200 to 270° (Toupet) fundoplication [24, 35, 37, 40, 41, 44, 46, 55, 59, 60], robot-assisted LNF [32, 48, 49, 52], laparoscopic Lind fundoplication [39], a variation of LNF [22, 26, 34, 53, 54, 61, 69], or PPI therapy [15, 16, 45]. For the included studies with a variation of LNF, only one was considered as the intervention group and included in this review. The variations considered to be the comparator group and not presented in this review included LNF without division of short gastric vessels [22, 26, 61], LNF with crural closure using simple sutures and mesh hiatoplasty [34], additional prosthetic hiatal closure with a bougie [54], additional anterior hiatal closure [69], and LNF with suturing of the wrap to both diaphragmatic crura or to the body of the stomach [53]. In one study, the intervention group was divided into LNF with a 1.5- or 3‑cm wrap, but only data for participants receiving a 3-cm wrap were included [46, 47].
Intraoperative outcomes
All included studies presented results for at least one intraoperative outcome (Table 2). In total, 78 injuries and other complications occurred. Most were respiration-related complications (4.5%), followed by bleeding (2.9%). Furthermore, 39 cases (1.6%) required conversion to open surgery, reported by 37 articles. Gastroesophageal injury or perforation occurred in 0.9% of the subjects, reported by 17 articles. However, no deaths occurred during LNF surgery. As shown in Table 2, several outcomes were sporadically reported by the included studies, except for conversion to open surgery.
Postoperative outcomes
Heartburn and epigastric/sternal pain were combined into one outcome measure for the purposes of this review, which is referred to as “heartburn or epigastric/sternal pain” from this point on. Appendix B presents some results in more detail.
Results from the two earliest postoperative timepoints were collated into one period, i.e., 4 to 6 weeks after surgery. A summary of postoperative results is shown in Table 3 and presented more elaborately in Supplementary Table B.2. In total, 15 studies reported some result among 656 participants [14, 28, 34, 39, 48, 49, 52,53,54, 57, 60, 61, 69, 72, 75]. Postoperative events were common, particularly dysphagia (46.1%), gas bloating (32.5%), and heartburn or epigastric/sternal pain (31.9%).
At 6 months, some postoperative events decreased in frequency while others increased among the 584 available participants from 13 of the included studies [14, 22, 24, 32, 33, 39, 46, 53, 61, 65, 69, 72, 74]. These are shown in Table 3 and Supplementary Table B.3. The most common included gas bloating (32.2%), dysphagia (27.9%), and heartburn or epigastric/sternal pain (27.9%).
One year after surgery, 16 studies presented postoperative results among 656 participants [14, 20, 22, 24, 26,27,28, 34, 35, 39, 42, 47, 50, 52, 57, 73]. The results are shown in Table 3 and Supplementary Table B.4. In general, the overall percentage for each outcome had decreased in comparison to previous measurements. However, some outcomes were still relatively common, such as gas bloating (30.1%), dysphagia (22.4%), inability to vomit/belch (16.4%), and heartburn or epigastric/sternal pain (15.1%).
Results 5 years after operation were reported in nine studies among 504 participants [17, 25, 47, 58, 62, 66, 70, 73, 76]. The data exhibited an increase in the overall percentage for most outcomes, as shown in Table 3 and Supplementary Table B.5. Most participants complained about gas bloating (52.7%), inability to vomit/belch (39.8%), dysphagia (28.9%), and heartburn or epigastric/sternal pain (27.0%).
In six studies, 288 participants were successfully followed for 10 years after surgery and had postoperative results [23, 28, 30, 63, 67, 71]. Overall, most of the outcomes continued to increase in frequency at the 10-year follow-up (Table 3 and Supplementary Table B.6). Again, complication rates were substantial for inability to vomit/belch (48.8%), dysphagia (45.3%), gas bloating (44.4%), and heartburn or epigastric/sternal pain (30.9%; Table 3 and Supplementary Table B.6).
More than 10 years after the operation (range 12–20 years), only five studies reported results for a total of 238 participants [21, 31, 43, 64, 68]. The results are presented in Supplementary Table B.6. At this follow-up timepoint, there were substantial rates of dysphagia (55.7%), heartburn or epigastric/sternal pain (53.5%), and gas bloating (49.6%).
A summary of dysphagia and heartburn or epigastric/sternal pain at 10- and 17-year follow-ups with patients acting as their own control is presented in Table 4. These long-term postoperative clinical results were reported in three studies [30, 31, 63, 64, 67, 68]. Almost half of the participants complained about dysphagia 10 years after operation (50.3%) and around a third about heartburn or epigastric/sternal pain (31.6%). At 17 years after surgery with the same patient groups, substantially more participants suffered from dysphagia (65.1%) and heartburn or epigastric/sternal pain (53.5%).
Reoperation after LNF was reported in 21 of the 40 included studies [15, 19, 20, 22, 25, 28,29,30, 32, 37, 39, 41, 42, 45,46,47, 49, 50, 57, 58, 61,62,63, 65,66,67, 69,70,71,72,73,74, 76]. During both short- and long-term follow-up, reoperations were prevalent but to different extents (Table 5 and Supplementary Table B.7). The overall percentage of reoperations was 2.3% up to 4 to 6 weeks postoperatively, which increased to 6.7% up to 1 year postoperatively and to 16.3% up to 10 years postoperatively. The number of studies reporting reoperation differed for each follow-up, mostly presenting 1‑year results. Reoperations were mainly for two reasons: (prolonged) dysphagia and recurrent reflux symptoms. Several studies also reported reoperations due to hiatal hernia (including herniation of the wrap, incisional hernia, paraesophageal hiatal hernia, and recurrence of hiatal hernia).
Postoperative PPI medication use was presented in 18 studies, as shown in Table 5 and Supplementary Table B.8 [15, 17, 19, 21, 23, 25, 28,29,30, 37, 38, 42, 46, 47, 50, 51, 58, 62, 63, 66, 67, 70, 71, 73, 76]. PPI use was only reported in this review for follow-up periods ≥ 1 year. At 1 and 5 years after operation, there were similar rates for PPI use (12.3% and 11.9%, respectively), which increased to 23.3% at 10-year follow-up and to 23.5% at 12 to 15 years postoperatively.
When looking at the total failure rate, the most indicative figure is given by combining patient reoperations with PPI use (Table 5). Reoperations plus PPI use presented in 19.0% at 1 year postoperatively, with a similar rate after 5 years of 20.6%. However, 39.6% required PPIs and/or a reoperation after 10 years.
The percentage of total time with pH < 4 on 24-hour monitoring and DeMeester score were presented in seven studies for the 6‑month and 1‑year follow-ups [15, 22, 25, 33, 34, 42, 46]. However, the results were merged, as shown in Table 6. Regarding the percentage of total time with pH < 4, the weighted average of means was 3.3%, and the weighted average of means for the DeMeester score was 12.6. These average numbers are normal but represent high values for an average value of acid exposure. The number of failures was generally not disclosed.
Appraisal
The critical assessment is summarized in Supplementary Table B.9 and the query domains were mostly fulfilled in the included studies. However, multiple articles did not provide enough information, resulting in an unclear assessment for several domains. Out of the 40 studies included in this review, 10 studies did not fulfill three or more query domains [14,15,16,17,18,19, 22, 33, 41, 45, 51, 53].
Discussion
The purpose of this systematic literature review was to investigate the postoperative safety and performance of LNF in adult patients with GERD, since exhaustive scrutiny is lacking in the current evidence base. Out of the 1675 articles included following elimination of duplicates, 63 articles were selected, covering 40 different RCTs of LNF at various timepoints. These studies provided information on intraoperative and/or postoperative outcomes ranging from 4 weeks to more than 17 years postoperatively. Altogether, the studies included 2619 participants.
The overall number of anti-reflux surgeries (i.e., LNF) performed worldwide has decreased over recent decades, and LNF procedures are performed in limited numbers relative to the large acid reflux treatment field [3]. This is most likely due to the imbalance between symptom control and the occurrence of complications that has limited the number of patients referred for surgery by medical doctors and general practitioners [3]. One reason for the reduction in the number of Nissen procedures may be that approximately 40–50% of LNF patients suffered from an inability to belch or vomit and had gas bloating after 5 years, as noted in the Results section of the present review.
The results indicate that rather few complications and injuries occurred during surgery, estimated at 5.5% (n = 78), and no deaths occurred. A systematic review by Salman et al. indicated a slightly higher rate of perioperative events (7.5%) during LNF, but with similar types of complications except conversion to open surgery, which was omitted [6]. Another review by Broeders et al. reported no deaths associated with LNF surgery [10]. In our review, all but three included studies reported on the frequency of conversion to open surgery, which was required in 1.6% of the cases (n = 39). However, most of these conversions (64%) were reported in five studies [14, 29, 42, 61, 74]. These conversions were performed between 1992 and 2000, i.e., somewhat earlier than in the remainder of the studies. Overall, these operations were performed about a decade ago. Therefore, the presented intraoperative events may correlate with surgical skill.
The data show that the complication rates exhibit a U-shaped curve in general, with the best results occurring at 1 year after surgery. Such complications include dysphagia, vomiting, the inability to vomit/belch, and heartburn or epigastric/sternal pain (Table 3 and Fig. B.1a–d in Appendix B). Symptoms were present 4 to 6 weeks after surgery, with a decreasing trend after 6 months to the lowest amount at 1 year, followed by an increase again at 5 years that continued to 10 years or more postoperatively.
The U‑shaped curve of complication rates can be exemplified further by the two symptoms dysphagia and heartburn or epigastric/sternal pain.
Dysphagia is a well-known side effect related to compression of the food passageway that occurs with the Nissen wrap. At 4 to 6 weeks after surgery, 46.1% of participants presented with dysphagia, which reduced to 27.9% at 6 months and further decreased to 22.4% at 1 year. However, the dysphagia rate increased again to 28.9% after 5 years and even further to 45.3% after 10 years (Table 3 and Supplementary Table B.6). Additionally, the sub-analysis on patients acting as their own control showed a notable increase in the percentage of dysphagia, from 50.3% at 10 years to 65.1% at 17 years. Like the present results, Salman et al. displayed that 16.2% of participants had dysphagia 1 year after LNF surgery [6]. However, only 9.8% of the patients in that review had dysphagia > 12 months afterwards, a rate which is substantially lower than the results in our review (e.g., 22.4% at 1‑year follow-up). However, Broeders et al. reported that 13.5% of LNF patients had dysphagia ≽1 year after their surgery [9]. On the other hand, Du et al. showed that 40% of patients had dysphagia more than 5 years after LNF surgery [8], which is higher than in our results (28.9%). However, another review reported a dysphagia rate of 33% at 5‑year follow-up [10], in line with our results.
Heartburn or epigastric/sternal pain displayed a similar U‑shaped curve, whereby 31.9% of the participants presented with symptoms 4 to 6 weeks after surgery. At 6 months, 27.9% experienced these symptoms, a figure which decreased to 15.1% at 1‑year follow-up. However, this symptomology increased to 27.0% at 5 years and further to 30.9% at 10 years (Table 3 and Supplementary Table B.6). Furthermore, the summary of results at 10- and 17-year follow-ups with patients acting as their own control showed a notable increase in the rate of heartburn or epigastric/sternal pain to 31.6% at 10 years that progressed to 53.5% at 17 years. Broeders et al. reported that 6.3% of patients experienced heartburn at the 1‑year follow-up [10]. Our results are substantially higher (15.1%). In the same review by Broeders et al., the authors reported that 11.8% of patients had heartburn at the 5‑year follow-up [10]. Furthermore, Du et al. showed that 13.1% of patients had heartburn more than 5 years after LNF surgery [8]. These are considerably lower rates than we found (27.0% at 5 years and 30.9% at 10 years; Table 3 and Supplementary Table B.6). However, these previous reviews only included three studies for this endpoint, which might explain the differences in results. These outcomes are also related to how many of the failure patients were reoperated.
Gas bloating and regurgitation did not display a pattern that was appreciated as clearly, though the highest numbers of events occurred after 5 years and 10 years (52.7% and 18.3%, respectively). Previous research indicated that more than one third of LNF patients had gas bloating postoperatively [6], and another review reported 18% at the 1‑year follow-up [10]. Broeders et al. reported that 35.9% had gas bloating among LNF patients with at least 1 year of follow-up [9]. These results are in line with the present review’s results 1 year after LNF surgery (30.1%). Furthermore, a previous review reported that 48% experienced gas bloating after 5 years [10], which is similar to our 5‑year data (52.7%). In this review from the year 2013 by Broeders et al., 4.9% of patients reported regurgitation at the 1‑year follow-up [10], which is lower than our result (8.4%). We reported data from eight studies, whereas the previous review only provided data from three studies, which may explain the differing results.
Reoperations occurred throughout the entire study period and continued to increase with longer follow-up times, while PPI use was similar at 1 and 5 years after surgery, followed by a distinct increase after 10 years (Table 5 and Supplementary Tables B.6 and B.7). Whether PPI use is a suitable outcome for assessment may be scrutinized; however, it serves as an indication of the treatment effect [77]. Of note, around one fifth of the patients (19.0%) required reoperation and/or PPI use 1 year postoperatively, and more than one third (39.6%) required PPIs and/or reoperation after 10 years. Most studies reported that the reason for reoperation was due to dysphagia or recurrent reflux symptoms. This was expected based on the prevalent postoperative data and the U‑shaped curves displayed in this review. Evidence from a previous review indicated a similar rate of PPI use postoperatively (13.1%) [6]. Another review reported PPI use in 7.4% of LNF patients at the 1‑year follow-up and in 10% at the 5‑year follow-up [10]. On the contrary, we found higher rates of PPI use (12.3% and 11.9%, respectively). However, firstly, we based our results on eight studies compared to the two to three in the review by Broeders et al. [10]. Secondly, one needs to keep in mind that the number of PPI users depends on how many patients have been reoperated. The higher the reoperation rate, the lower the number of PPI users. This is why the combination of these two data points, as reported, is valuable. Postoperatively, Salman et al. showed that 4.5% needed reoperation, which is a lower rate than most postoperative rates presented in this review [6]. However, Salman et al. combined studies with follow-up periods ranging from 3 months to 15 years, which might explain the difference in rates. Another review by Broeders et al. from 2010 indicated that 7.0% of patients required reoperation after at least 1 year following LNF [9], which is similar to our results after 1 year (6.7%). Most other reviews included only a few studies, meanwhile, we included 17 studies. Furthermore, our inclusion of randomized studies provided more robust data that found lower reoperation rates if failure patients were kept on PPIs.
Despite pH monitoring being considered the gold standard modality for diagnosis of GERD [13], the frequency of 24-hour pH monitoring test failure was generally not reported in the included studies. Instead, only the weighted average results were presented, demonstrating normal values for acid exposure 6 to 12 months after surgery [13]. These average numbers were normal but occupy the higher end of normal limits in terms of acid exposure. However, due to the invasive nature of most objective measurements, it was expected that only a couple of these outcomes were possible for inclusion in evidence synthesis. Like the results presented in this review, previous research indicates a normal percentage of time with pH < 4 and normal DeMeester scores following LNF on average, albeit with results in the upper end of the normal result range [4, 6, 10].
The results of this review indicate that side effects and complications were present during both short- and long-term follow-up after LNF. In general, the clinical postoperative results suggested that following surgery, it took about 1 year before patients achieved maximally optimal results. Nevertheless, worsening of the rates of symptoms and complications continued for more than 10 years afterwards.
Appraisal indicated that most of the studies fulfilled the domains stated in the JBI critical appraisal tool [12]. However, critical information was missing from multiple articles, causing speculation of the evidence to some extent. The omission of information cannot be fully explained by the journals’ restrictions; for instance, word limit restrictions are one such consideration.
Strengths and limitations
To only include RCTs is a strength of this study, since the review was spared from inherent methodological issues associated with observational studies. Numerous subjective and objective outcomes were studied, enabling a more thorough perspective of the procedure. This was further enhanced by including both short- and long-term specific follow-up timepoints. The appraisal was performed by two independent reviewers, thus ensuring a rigorous assessment of the studies included. Descriptive statistics were utilized for all statistical analyses, since to test hypotheses in our setting would extensively use the same data on a repeated basis, resulting in redundant hypothesis testing. We could have used, e.g., Bonferroni corrections to resolve that, but adding complexity to the analysis where there are missing data (e.g., Table B.3) could make the analysis opaque from a statistical point of view. The only feasible solution would be to make the claim that the missing data are missing at random, and even if that does apply to some studies, it certainly does not for all. As a result, we chose not to perform a more in-depth statistical analysis in this review.
We also acknowledge some limitations. Mainly, our choice to focus solely on LNF and not include the comparator arm(s) is a limitation, as an analysis of comparative evidence between LNF and other treatment options was not conducted, although this may provide objective information to help in clinical decision-making. We failed to synthesize several outcomes (Table B.1), which highlights the lack of evidence in published studies pertaining to LNF. There were slight variations of the LNF technique that may potentially affect generalizability. However, the included trials described the surgical procedures to various degrees, with different levels of detail, making categorization insufficient. Further, we were limited by the inconsistency in endpoint reporting. For instance, 16 studies provided data at the 1‑year follow-up, but only four trials presented odynophagia results (Table B.4). Additionally, 24-hour pH monitoring results were combined for the 6‑ and 12-month follow-ups, which slightly reduced resolution and context. However, this outcome was surprisingly infrequent and was therefore deemed the best option. Some portions of the systematic literature review were conducted by one reviewer, although double-checked, which may affect the syntheses and robustness.
Conclusion
Although LNF is considered the gold standard in anti-reflux surgery and has been a recurrent research topic for many decades, a complete review of the literature has not been comprehensively performed. The safety profile presented in this systematic literature review demonstrates a limited number of serious surgical complications and a reasonable number of reoperations. The performance of LNF varies over time, with an increasing number of patients taking PPIs and most symptoms presenting as a U-shaped curve with the lowest rates at 1 year. Complication rates were substantially higher at 5 years, whereby participants from nine randomized trials presented with gas bloating (52.7%), inability to vomit/belch (39.8%), dysphagia (28.9%), and heartburn or epigastric/sternal pain (27.0%). The available postoperative data up to 17 years indicate that the performance of Nissen fundoplication dissipates in the long term. Several reported events could, at least partly, be attributed to the compression of the food passageway that is associated with the fundal wrap technique of Nissen fundoplication.
The complications and adverse events indicate an unmet need, where newer treatment options may contribute to reducing the treatment gaps. Surgeons and patients should take this review into consideration when selecting treatment for gastroesophageal reflux disease.
References
Bredenoord AJMD, Pandolfino JEMD, Smout AJPMP. Gastro-oesophageal reflux disease. Lancet. 2013;381(9881):1933–42.
Nirwan JS, Hasan SS, Babar ZU, Conway BR, Ghori MU. Global Prevalence and Risk Factors of Gastro-oesophageal Reflux Disease (GORD): Systematic Review with Meta-analysis. Sci Rep. 2020;10(1):5814.
Yadlapati R, Hungness ES, Pandolfino JE. Complications of antireflux surgery. Am J Gastroenterol. 2018;113(8):1137–47.
Amer MA, Smith MD, Khoo CH, Herbison GP, McCall JL. Network meta-analysis of surgical management of gastro-oesophageal reflux disease in adults. Br J Surg. 2018;105(11):1398–407.
Markar S, Andreou A, Bonavina L, Florez ID, Huo B, Kontouli KM, et al. UEG and EAES rapid guideline: Update systematic review, network meta-analysis, CINeMA and GRADE assessment, and evidence-informed European recommendations on surgical management of GERD. United European Gastroenterol J. 2022;10(9):983–98.
Salman MA, Salman A, Shaaban HE, Alasmar M, Tourky M, Elhaj MGF, et al. Nissen Versus Toupet Fundoplication For Gastro-oesophageal Reflux Disease, Short And Long-term Outcomes. A Systematic Review And Meta-analysis. Surg Laparosc Endosc Percutan Tech. 2023;33(2):171–83.
Andreou A, Watson DI, Mavridis D, Francis NK, Antoniou SA. Assessing the efficacy and safety of laparoscopic antireflux procedures for the management of gastroesophageal reflux disease: a systematic review with network meta-analysis. Surg Endosc. 2019;34(2):510–20.
Du X, Wu J‑M, Hu Z‑W, Wang F, Wang Z‑G, Zhang C, et al. Laparoscopic Nissen (total) versus anterior 180° fundoplication for gastro-esophageal reflux disease: A meta-analysis and systematic review. Medicine. 2017;96(37):e8085‑e.
Broeders JA, Mauritz FA, Ali AU, Draaisma WA, Ruurda JP, Gooszen HG, et al. Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg. 2010;97(9):1318–30.
Broeders JA, Roks DJ, Ali AU, Watson DI, Baigrie RJ, Cao Z, et al. Laparoscopic anterior 180-degree versus nissen fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis of randomized clinical trials. Ann Surg. 2013;257(5):850–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;.
JBI. Critical appraisal tool. Checklist for randomized controlled trials. 2020. https://mcusercontent.com/b7a3429cdeb2d9125de40e149/files/a27aefa1-64d9-a671-abb9-8a62285ff0da/JBI_Checklist_for_RCTs_archive_2020.docx..
Streets CG, DeMeester TR. Ambulatory 24-hour Esophageal pH Monitoring: Why, When, and What to Do. J Clin Gastroenterol. 2003;37(1):14–22.
Ackroyd R, Watson DI, Majeed AW, Troy G, Treacy PJ, Stoddard CJ. Randomized clinical trial of laparoscopic versus open fundoplication for gastro-oesophageal reflux disease. Br J Surg. 2004;91(8):975–82.
Anvari M, Allen C, Marshall J, Armstrong D, Goeree R, Ungar W, et al. A randomized controlled trial of laparoscopic nissen fundoplication versus proton pump inhibitors for treatment of patients with chronic gastroesophageal reflux disease: One-year follow-up. Surg Innov. 2006;13(4):238–49.
Attwood S, Lundell L, Hatlebakk J, Eklund S, Junghard O, Galmiche J, et al. Medical or surgical management of GERD patients with Barrett’s esophagus: the LOTUS trial 3‑year experience. J Gastrointest Surg. 2008;12(10):1646–54.
Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD the LOTUS randomized clinical Trial. JAMA. 2011;305(19):1969–77.
Hatlebakk JG, Zerbib F, Varannes SBD, Attwood SE, Ell C, Fiocca R, et al. Gastroesophageal acid reflux control 5 years after antireflux surgery, compared with long-term eomeprazole therapy. Clin Gastroenterol Hepatol. 2016;14(5):678–85.
Aye R, Swanstrom L, Kapur S, Buduhan G, Dunst C, Knight A, et al. A randomized multiinstitution comparison of the laparoscopic Nissen and Hill repairs. Ann Thorac Surg. 2012;94(3):951–7.
Baigrie R, Cullis S, Ndhluni A, Cariem A. Randomized double-blind trial of laparoscopic Nissen fundoplication versus anterior partial fundoplication. Br J Surg. 2005;92(7):819–23.
Roks D, Broeders J, Baigrie R. Long-term symptom control of gastro-oesophageal reflux disease 12 years after laparoscopic Nissen or 180° anterior partial fundoplication in a randomized clinical trial. Br J Surg. 2017;104(7):852–6.
Blomqvist A, Dalenback J, Hagedorn C, Lonroth H, Hyltander A, Lundell L. Impact of complete gastric fundus mobilization on outcome after laparoscopic total fundoplication. J Gastrointest Surg. 2000;4(5):493–500.
Mardani J, Lundell L, Lönroth H, Dalenbäck J, Engström C. Ten-year results of a randomized clinical trial of laparoscopic total fundoplication with or without division of the short gastric vessels. Br J Surg. 2009;96(1):61–5.
Booth MI, Stratford J, Jones L, Dehn TCB. Randomized clinical trial of laparoscopic total (Nissen) versus posterior partial (Toupet) fundoplication for gastro-oesophageal reflux disease based on preoperative oesophageal manometry. Br J Surg. 2008;95(1):57–63.
Cao Z, Cai W, Qin M, Zhao H, Yue P, Li Y. Randomized clinical trial of laparoscopic anterior 180degree partial versus 360degree Nissen fundoplication: 5‑year results. Dis Esophagus. 2012;25(2):114–20.
Chrysos E, Tzortzinis A, Tsiaoussis J, Athanasakis H, Vasssilakis J, Xynos E. Prospective randomized trial comparing Nissen to Nissen-Rossetti technique for laparoscopic fundoplication. Am J Surg. 2001;182(3):215–21.
Chrysos E, Tsiaoussis J, Athanasakis E, Zoras O, Vassilakis J, Xynos E. Laparoscopic vs open approach for Nissen fundoplication. A comparative study. Surg Endosc. 2002;16(12):1679–84.
Djerf P, Montgomery A, Hallerbäck B, Håkansson H, Johnsson F. One- and ten-year outcome of laparoscopic anterior 120° versus total fundoplication: a double-blind, randomized multicenter study. Surg Endosc. 2016;30(1):168–77.
Draaisma WA, Rijnhart-de JHG, Broeders IA, Smout AJ, Furnee EJ, Gooszen HG. Five-year subjective and objective results of laparoscopic and conventional Nissen fundoplication: a randomized trial. Ann Surg. 2006;244(1):34–41.
Broeders J, Rijnhart-de JH, Draaisma W, Bredenoord A, Smout A, Gooszen H. Ten-year outcome of laparoscopic and conventional nissen fundoplication: randomized clinical trial. Ann Surg. 2009;250(5):698–706.
Oor J, Roks D, Broeders J, Hazebroek E, Gooszen H. Seventeen-year outcome of a randomized clinical trial comparing laparoscopic and conventional Nissen fundoplication: a plea for patient counseling and clarification. Ann Surg. 2017;266(1):23–8.
Draaisma WA, Ruurda JP, Scheffer RC, Simmermacher RK, Gooszen HG, Rijnhart-de JHG, et al. Randomized clinical trial of standard laparoscopic versus robot-assisted laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease. Br J Surg. 2006;93(11):1351–9.
Franzén T, Anderberg B, Wirén M, Johansson K. Long-term outcome is worse after laparoscopic than after conventional Nissen fundoplication. Scand J Gastroenterol. 2005;40(11):1261–8.
Granderath F, Schweiger U, Kamolz T, Asche K, Pointner R. Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg. 2005;140(1):40–8.
Guérin E, Bétroune K, Closset J, Mehdi A, Lefèbvre J, Houben J, et al. Nissen versus Toupet fundoplication: results of a randomized and multicenter trial. Surg Endosc. 2007;21(11):1985–90.
Heikkinen TJ, Haukipuro K, Koivukangas P, Sorasto A, Autio R, Södervik H, et al. Comparison of costs between laparoscopic and open Nissen fundoplication: a prospective randomized study with a 3-month followup. J Am Coll Surg. 1999;188(4):368–76.
Håkanson BS, Lundell L, Bylund A, Thorell A. Comparison of laparoscopic 270° posterior partial fundoplication vs total fundoplication for the treatment of gastroesophageal reflux disease: a randomized clinical trial. JAMA Surg. 2019;154(6):479–86.
Analatos A, Hakanson BS, Ansorge C, Lindblad M, Lundell L, Thorell A. Clinical Outcomes of a Laparoscopic Total vs a 270degree Posterior Partial Fundoplication in Chronic Gastroesophageal Reflux Disease: A Randomized Clinical Trial. JAMA Surg. 2022;157(6):473–80.
Khan MA, Smythe A, Globe J, Stoddard CJ, Ackroyd R. Randomized controlled trial of laparoscopic Nissen versus Lind fundoplication for gastro-oesophageal reflux disease. Scand J Gastroenterol. 2009;44(3):269–75.
Koch O, Kaindlstorfer A, Antoniou S, Asche K, Granderath F, Pointner R. Laparoscopic Nissen versus Toupet fundoplication: objective and subjective results of a prospective randomized trial. Surg Endosc. 2012;26(2):413–22.
Koch OO, Kaindlstorfer A, Antoniou SA, Luketina RR, Emmanuel K, Pointner R. Comparison of results from a randomized trial 1 year after laparoscopic Nissen and Toupet fundoplications. Surg Endosc. 2013;27(7):2383–90.
Laine S, Rantala A, Gullichsen R, Ovaska J. Laparoscopic vs conventional Nissen fundoplication—A prospective randomized study. Surg Endosc. 1997;11(5):441–4.
Salminen P, Hurme S, Ovaska J. Fifteen-year outcome of laparoscopic and open Nissen fundoplication: a randomized clinical trial. Ann Thorac Surg. 2012;93(1):228–33.
Laws H, Clements R, Swillie C. A randomized, prospective comparison of the Nissen fundoplication versus the Toupet fundoplication for gastroesophageal reflux disease. Ann Surg. 1997;225(6):647–53.
Mahon D, Rhodes M, Decadt B, Hindmarsh A, Lowndes R, Beckingham I, et al. Randomized clinical trial of laparoscopic Nissen fundoplication compared with proton-pump inhibitors for treatment of chronic gastro-oesophageal reflux. Br J Surg. 2005;92(6):695–9.
Mickevičius A, Endzinas Ž, Kiudelis M, Jonaitis L, Kupčinskas L, Maleckas A, et al. Influence of wrap length on the effectiveness of Nissen and Toupet fundoplication: A prospective randomized study. Surg Endosc. 2008;22(10):2269–76.
Mickevicius A, Endzinas Z, Kiudelis M, Jonaitis L, Kupcinskas L, Pundzius J, et al. Influence of wrap length on the effectiveness of Nissen and Toupet fundoplications: 5‑year results of prospective, randomized study. Surg Endosc. 2013;27(3):986–91.
Morino M, Pellegrino L, Giaccone C, Garrone C, Rebecchi F. Randomized clinical trial of robot-assisted versus laparoscopic Nissen fundoplication. Br J Surg. 2006;93(5):553–8.
Müller-Stich B, Reiter M, Wente M, Bintintan V, Köninger J, Büchler M, et al. Robot-assisted versus conventional laparoscopic fundoplication: short-term outcome of a pilot randomized controlled trial. Surg Endosc. 2007;21(10):1800–5.
Müller-Stich B, Reiter M, Mehrabi A, Wente M, Fischer L, Köninger J, et al. No relevant difference in quality of life and functional outcome at 12 months’ follow-up—a randomised controlled trial comparing robot-assisted versus conventional laparoscopic Nissen fundoplication. Langenbecks Arch Surg. 2009;394(3):441–6.
Lang F, Huber A, Kowalewski KF, Kenngott HG, Billmann F, Billeter AT, et al. Randomized controlled trial of robotic-assisted versus conventional laparoscopic fundoplication: 12 years follow-up. Surg Endosc. 2022;36(8):5627–34.
Nakadi I, Mélot C, Closset J, DeMoor V, Bétroune K, Feron P, et al. Evaluation of da Vinci Nissen fundoplication clinical results and cost minimization. World J Surg. 2006;30(6):1050–4.
Paranyak M, Patel R, Grubnyk V, Grubnik V. Influence of Wrap Fixation Technique on the Results of Fundoplication. Surg Laparosc Endosc Percutan Tech. 2021;31(6):663–8.
Patterson EM, Herron DM, Hansen PD, Ramzi N, Standage BA, Swanstrom LL. Effect of an esophageal bougie on the incidence of dysphagia following Nissen fundoplication: A prospective, blinded, randomized clinical trial. Arch Surg. 2000;135(9):1055–62.
Qin M, Ding G, Yang H. A clinical comparison of laparoscopic nissen and toupet fundoplication for gastroesophageal reflux disease. J Laparoendosc Adv Surg Tech A. 2013;23(7):601–4.
Raue W, Ordemann J, Jacobi CA, Menenakos C, Buchholz A, Hartmann J. Nissen versus Dor fundoplication for treatment of gastroesophageal reflux disease: a blinded randomized clinical trial. Dig Surg. 2011;28(1):80–6.
Spence GM, Watson DI, Jamiesion GG, Lally CJ, Devitt PG. Single center prospective randomized trial of laparoscopic Nissen versus anterior 90 degrees fundoplication. J Gastrointest Surg. 2006;10(5):698–705.
Watson DI, Devitt PG, Smith L, Jamieson GG. Anterior 90° partial vs Nissen fundoplication—5 Year follow-up of a single-centre randomised trial. J Gastrointest Surg. 2012;16(9):1653–8.
Strate U, Emmermann A, Fibbe C, Layer P, Zornig C. Laparoscopic fundoplication: Nissen versus Toupet two-year outcome of a prospective randomized study of 200 patients regarding preoperative esophageal motility. Surg Endosc. 2008;22(1):21–30.
Wang B, Zhang W, Liu S, Du Z, Shan C, Qiu M. A Chinese randomized prospective trial of floppy Nissen and Toupet fundoplication for gastroesophageal disease. Int J Surg. 2015;23(Pt A)):35–40.
Watson DI, Pike GK, Baigrie RJ, Mathew G, Devitt PG, Britten-Jones R, et al. Prospective double-blind randomized trial of laparoscopic Nissen fundoplication with division and without division of short gastric vessels. Ann Surg. 1997;226(5):642–52.
O’Boyle CJ, Watson DI, Jamieson GG, Myers JC, Game PA, Devitt PG. Division of short gastric vessels at laparoscopic nissen fundoplication: a prospective double-blind randomized trial with 5‑year follow-up. Ann Surg. 2002;235(2):165–70.
Yang H, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG. Randomized trial of division versus nondivision of the short gastric vessels during laparascopic Nissen fundoplication—10-year outcomes. Ann Surg. 2008;247(1):38–42.
Kinsey-Trotman SP, Devitt PG, Bright T, Thompson SK, Jamieson GG, Watson DI. Randomized trial of division versus nondivision of short gastric vessels during Nissen fundoplication: 20-year outcomes. Ann Surg. 2018;04:4.
Watson DI, Jamieson GG, Pike GK, Davies N, Richardson M, Devitt PG. Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg. 1999;86(1):123–30.
Ludemann R, Watson D, Jamieson G, Game P, Devitt P. Five-year follow-up of a randomized clinical trial of laparoscopic total versus anterior 180 degrees fundoplication. Br J Surg. 2005;92(2):240–3.
Cai W, Watson D, Lally C, Devitt P, Game P, Jamieson G. Ten-year clinical outcome of a prospective randomized clinical trial of laparoscopic Nissen versus anterior 180( degrees ) partial fundoplication. Br J Surg. 2008;95(12):1501–5.
Rudolph-Stringer V, Bright T, Irvine T, Thompson SK, Devitt PG, Game PA, et al. Randomized Trial of Laparoscopic Nissen vs. Anterior 180 Degree Partial Fundoplication—Late Clinical Outcomes at 15–20 years. Ann Surg. 2020;.
Watson DI, Jamieson GG, Devitt PG, Kennedy JA, Ellis T, Ackroyd R, et al. A prospective randomized trial of laparoscopic Nissen fundoplication with anterior vs posterior hiatal repair. Arch Surg. 2001;136(7):745–51.
Wijnhoven BP, Watson DI, Devitt PG, Game PA, Jamieson GG. Laparoscopic Nissen fundoplication with anterior versus posterior hiatal repair: long-term results of a randomized trial. Am J Surg. 2008;195(1):61–5.
Chew C, Jamieson G, Devitt P, Watson D. Prospective randomized trial of laparoscopic Nissen fundoplication with anterior versus posterior hiatal repair: late outcomes. World J Surg. 2011;35(9):2038–44.
Watson DI, Jamieson GG, Lally C, Archer S, Bessell JR, Booth M, et al. Multicenter, prospective, double-blind, randomized trial of laparoscopic nissen vs anterior 90° partial fundoplication. Arch Surg. 2004;139(11):1160–7.
Nijjar RS, Watson DI, Jamieson GG, Archer S, Bessell JR, Booth M, et al. Five-year follow-up of a multicenter, double-blind randomized clinical trial of laparoscopic Nissen vs anterior 90 degrees partial fundoplication. Arch Surg. 2010;145(6):552–7.
Wenner J, Nilsson G, Oberg S, Melin T, Larsson S, Johnsson F. Short-term outcome after laparoscopic and open 360 degrees fundoplication. A prospective randomized trial. Surg Endosc. 2001;15(10):1124–8.
Nilsson G, Larsson S, Johnsson F. Randomized clinical trial of laparoscopic versus open fundoplication: evaluation of psychological well-being and changes in everyday life from a patient perspective. Scand J Gastroenterol. 2002;37(4):385–91.
Nilsson G, Wenner J, Larsson S, Johnsson F. Randomized clinical trial of laparoscopic versus open fundoplication for gastro-oesophageal reflux. Br J Surg. 2004;91(5):552–9.
Wijnhoven BPL, Wijnhoven BPL, Lally CJ, Lally CJ, Kelly JJ, Kelly JJ, et al. Use of Antireflux Medication After Antireflux Surgery. J Gastrointest Surg. 2008;12(3):510–7.
Acknowledgements
The author would like to thank Magdalena Svanberg, Susanne Gustafsson, and Anders Wändahl from the Karolinska University Library for their help with the systematic search for relevant records.
Funding
This work was supported by Implantica, Zug, Switzerland (research grant number K952211103), providing full ownership to the Karolinska Institutet, Stockholm, Sweden, to content, including data analysis and publishing at any time regardless of the results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The work was conducted from 2017 to 2023, of which the main work was conducted during the years 2017–2018. During this period, the primary researcher (J. Hoffsten) was not an employee of the funding company but employed at the Karolinska Institutet. The authors J. Hoffsten (since 2020) and S. Das (since 2023) are consultants at the funding company and affiliated with the Karolinska Institutet. J. Zehetner, S.F. Schoppmann, and J.C. Lipham declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Johanna Hoffsten and Shuchesmita Das are no longer at the Karolinska Institutet, although this is the institution at which they conducted most of the study.
Appendices
Appendix A
Search strategy
Appendix B
Supplementary tables and figures
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zehetner, J., Hoffsten, J., Das, S. et al. Looking back on a gold standard: a systematic literature review of laparoscopic Nissen fundoplication as an anti-reflux treatment option. Eur Surg (2024). https://doi.org/10.1007/s10353-024-00836-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10353-024-00836-z