Summary
Background
Giant cell myocarditis and granulomatous myocarditis are rare diseases, leading to severe heart symptoms like tachyarrhythmia or atrial fibrillation with frequently fatal outcome. Typically, diagnosis is confirmed at necropsy or in explanted hearts, as the majority of cases remain clinically unrecognized.
Methods
Explanted heart specimens of 355 heart transplant recipients receiving cardiac transplantation between January 1994 and December 2011 were examined. Unexpected granulomatous myocarditis was found in the explanted hearts of three patients and giant cell myocarditis in four patients. We investigated preoperative and postoperative course and gross and histopathological findings of these two different disorders, which were thought to be the same disease for a long time.
Results
Preoperatively, both groups suffered from mild to severe symptoms of heart failure. Gross findings of resected heart specimens showed right and left ventricular hypertrophy. Histological examination revealed a left ventricular endomyocardial fibrosis and inflammation infiltrates including giant cells with the presence or absence of granulomas. All patients with granulomatous myocarditis are alive. Three patients suffering from giant cell myocarditis showed a complicated postoperative clinical course, one heart transplant recipient developed Guillain–Barré syndrome due to cytomegalovirus reactivation 6 months after heart transplantation, another patient died due to cerebral edema shortly after transplantation, and another one died because of myocardial and cerebral infarction after tricuspid valve replacement.
Conclusions
In consideration of the limitation of this study that a small number of patients were included, our results suggest that patients suffering from granulomatous myocarditis are older at heart transplantation and have a more favorable outcome compared with heart transplant recipients with giant cell myocarditis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Contrary to granulomatous myocarditis, which is mostly part of a systemic granulomatous disease (tuberculosis, sarcoidosis, or hypersensitivity reaction), giant cell myocarditis is a histopathological diagnosis, nearly impossible to verify by clinical examination preoperatively (Table 1).
Giant cell myocarditis is a rare and frequently fatal disorder, first described by Saltykow [1] in 1905 in a 37-year-old man dying suddenly after surgical drainage of an abscess. Until now, its etiology has not yet been fully elucidated. In the first half of twentieth century, borders between giant cell myocarditis and granulomatous myocarditis were not well defined, and names were used interchangeably leading sometimes to confusion. For differentiation, the presence of granulomas is the most important distinguishing mark.
Tesluk [2] was the first who separated the granulomatous lesions of sarcoidosis (Figs. 1 and 2) from a diffuse, nongranulomatous infiltrate, which he called giant cell myocarditis. The majority of giant cell myocarditis cases are clinically unrecognized, and primary diagnosis is confirmed at autopsy or in explanted heart specimens.
The cause of giant cell myocarditis is not known but often presumed to be autoimmune. A total of 20 % of cases of giant cell myocarditis occur in individuals with other inflammatory or autoimmune disorders (Table 2), especially inflammatory bowel disease [3–9]. Some authors hypothesize an autoimmune origin with correlation to myasthenia gravis, chronic lymphocytic thyroiditis, and giant cell myositis [10, 11]. The tumor most commonly associated with giant cell myocarditis is thymoma, especially the spindle cell type [12]. The occurrence of giant cell myocarditis has even been described after high-dose interleukin-2 treatment for lymphoma, maybe as a result of cytokine imbalance [13]. Besides the broad spectrum of diseases that may be accompanied by giant cell myocarditis, it must be considered that giant cell reaction can also occur after surgery (e.g., valve replacement or coronary artery bypass grafting). Suture material may initiate the immune system to build granulomas with surrounding giant cells, phagocyting the foreign material (Fig. 3).
Material and methods
A total of 355 female and male patients received heart transplantation at the Department of Cardiac Surgery of the Medical University Innsbruck between January 1994 and December 2011. Explanted hearts were sent to the Department of Pathology. Heart specimens were fixed with 4 % phosphate-buffered formalin, dehydrated, paraffin embedded, cut into 2-μm-thick slides, stained with hematoxilin and eosin, and reviewed by experienced pathologists. In this study, we investigated preoperative and postoperative course, gross morphological changes, and histopathological features of seven heart transplant recipients suffering from giant cell and granulomatous myocarditis.
Results
Histopathological examination of explanted heart specimens of the 355 heart transplant recipients revealed 4 cases of giant cell myocarditis and 3 cases of granulomatous myocarditis (Table 3).
None of these patients were transplanted due to the preoperative clinical diagnosis of giant cell or granulomatous myocarditis. The cause of transplantation was dilated cardiomyopathy (four patients), followed by ischemic heart disease (two patients) and solitary cardiac sarcoidosis without other organ involvement (one patient). Of the seven affected patients, one was female and six were male. Anamnestically, no autoimmune disorders were reported. Mean recipient age at transplantation was 45.5 ± 13.9 years in the giant cell myocarditis group (range, 35–66 years) and 52.7 ± 9.1 years in the granulomatous myocarditis group (range, 43–61 years). The median time of follow-up was 109.7 months (range, 3 days to 174 months).
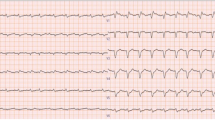
Preoperatively, all patients suffered from mild to severe symptoms of heart failure (New York Heart Association class II–IV). In two patients, ventricular tachycardia was present; one patient received an implantable cardioverter-defibrillator 1 year before heart transplantation. Electrocardiographic findings were suggestive of myocardial infarction in one patient, and two other male patients suffered from atrial fibrillation.
Left ventricular ejection fraction was significantly reduced in both groups and ranged between 10 and 35 %. Additionally, the mitral valve was involved in three patients showing signs of mild to severe valvular insufficiency, and two patients showed tricuspid valve involvement. Two patients received ventricular assist devices as bridge to transplantation.
Common aspects between giant cell and granulomatous myocarditis include extended fibrosis and right and left ventricular hypertrophy. The main gross finding in both groups was endomyocardial fibrosis mainly localized in the left ventricle and interventricular septum. Mean heart weight for the granulomatous myocarditis group was 433.3 ± 121.6 g (range, 313–527 g), and mean heart weight for the giant cell myocarditis group was 476.3 ± 84.4 g (range, 405–580 g).
Extended endomyocardial fibrosis, disrupted by more or less inflammatory infiltrates, mainly composed of lymphocytes, plasma cells, giant cells, and non-necrotizing or necrotizing granulomas, was the main histological finding in both groups. A causative organism could not be verified.
Postoperatively, four patients are currently alive, and three heart transplant recipients of the giant cell myocarditis group died. A male heart transplant recipient developed Guillain-Barré syndrome due to cytomegalovirus reactivation 8 months after cardiac transplantation and died due to sudden cardiac death after recovery from pneumonia 2 years postoperatively. One patient died due to cerebral edema 3 days after heart transplantation, and another heart transplant recipient died because of cerebral and myocardial infarction after tricuspid valve replacement 11 years after transplantation.
None of these seven patients showed granulomas or giant cell reaction in any of the routinely performed post-transplant endomyocardial biopsies. The highest rejection belonged to grade 1R (ISHLT 2004).
Discussion
In general, most patients with giant cell or granulomatous myocarditis suffer from nonspecific symptoms like chest pain, fatigue, ventricular arrhythmia, or heart block, and in several cases, initial symptoms can mimic those of acute myocardial infarction [14], with a usually more fulminant course in the case of giant cell myocarditis.
Giant cell myocarditis, an oftentimes lethal disease, is characterized by progressive congestive heart failure, frequently associated with refractory ventricular arrhythmia and rapid deterioration—the time period from onset of the first symptoms to severe heart failure and cardiogenic shock is usually only a few days or weeks. Men and women are equally affected, with an average age of 43 years at the time of symptom onset.
In the late 1980s and 1990s, the average time from the start of symptoms to death or transplantation was only 5 months, and many patients died before they could be listed for heart transplantation. Even now, the mean interval from the time of diagnosis to death or cardiac transplantation is still 6 months. Survival beyond 1 year without heart transplantation is uncommon. Recurrence in the native heart occurs up to 8 years after initial diagnosis.
Cardiac magnetic resonance imaging and endomyocardial biopsy can be helpful in making the correct diagnosis and ensuring that timely adequate treatment is administered, but sampling error remains a significant limitation to the diagnostic accuracy of the endomyocardial biopsy [15]. Usually, four to six biopsy samples are routinely analyzed during a diagnostic procedure, but a negative result without any evidence of granulomas does not automatically exclude giant cell or granulomatous myocarditis because of the patchy pattern of both diseases.
Whereas the treatment of granulomatous myocarditis commonly consists of drugs used for the underlying disease (corticosteroids for sarcoidosis, three- and fourfold drug combination with rifampicin, ethambutol, and isoniacid for tuberculosis, methotrexat and gold for rheumatic disease, and antihistamines for hypertensitivity disease), the rapidly progressive course of giant cell myocarditis requires immediate therapeutic intervention, including standard pharmacologic therapy for congestive heart failure, tachyarrhythmias, heart block, and secondary hepatic and renal insufficiency.
Since the first report of the Multicenter GCM Study Group [14], the recommended treatment has been the triple combination of cyclosporine, prednisone, and azathioprine. Exceptionally, other immunosuppressive drugs like mycophenolate mofetil, methotrexate, or the T-cell antibody muromonab can be added or substituted for other agents [16].
The combined treatment with immunosuppressants improves the poor prognosis, and yield a median survival time of 12 months compared with 3 months for untreated affected patients. Nevertheless, some patients require mechanical circulatory support or heart transplantation within 1 year [17].
The implantation of a temporary or permanent pacemaker, an implantable cardiac defibrillator, intra-aortic balloon pumps, or ventricular assist devices to bridge the time until heart transplantation may be necessary. Although a bridge to transplant concept is unavoidable in most cases, in general, the time period to transplantation is short and ranges from a few days to weeks.
Transplantation remains an effective therapy for patients suffering from giant cell myocarditis, yielding a 5-year survival rate of 71 % despite a 20–25 % risk of recurrence in the allograft, with an usually fulminant clinical course and sometimes even fatal outcome [14, 18–20]. It has been estimated that one-third of the 25 % of recurrences may be lethal [21, 22].
Histologically, three phases of giant cell myocarditis (acute, healing, and healed) have been described and may coincide within a single heart. The acute phase usually consist of typically multifocal necrosis and widespread mixed inflammatory infiltrate composed of numerous multinucleated macrophagic giant cells, lymphocytes, histiocytes, plasma cells, and eosinophils. The healing phase consists of granulation tissue and collagen with macrophagic and myogenic giant cells and occasional lymphocytes. The histiogenesis of the giant cells is still discussed controversially. Maybe the derivation of giant cells is related to the type or phase of injury or the nature of the response evoked.
Although giant cell myocarditis is associated with autoimmune genesis in 20 % of patients, none of our patients suffered from additional autoimmune disease. In our study, patients with giant cell myocarditis were younger at heart transplantation than those with granulomatous myocarditis. None of our patients suffered from recurrence of giant cell or granulomatous myocarditis, and none of the surviving transplant recipients showed signs of severe allograft rejection in post-transplant endomyocardial biopsies. Three of the four patients suffering from giant cell myocarditis showed a complicated postoperative clinical course, and two of them died shortly after transplantation. In contrast, all three granulomatous myocarditis patients are currently alive.
Gross findings of explanted hearts did not significantly differ between the granulomatous myocarditis and the giant cell myocarditis group. Right and left ventricular hypertrophy and more or less expanded endomyocardial fibrosis were present in both groups. Because myocardial involvement in giant cell myocarditis is usually extensive, hearts of patients with acute clinical presentations are typically dilated with flaccid ventricular walls. The cut surface of the myocardium contains pale areas, which correspond to areas of intense inflammation. Scarring is not characteristic of the acute disease but may appear in hearts of patients with longer survival.
On the first sight, a relevant limitation of our study is the small number of patients in both groups, the giant cell myocarditis group and the granulomatous myocarditis group, but maybe this study can add some information to the course of both diseases. In general, the lack of data concerning long-term management of giant cell and granulomatous myocarditis patients highlights the need for continuing multicenter collaborative clinical and pathological investigations.
Conclusion
Giant cell myocarditis and granulomatous myocarditis are two different disorders, both characterized by worsening heart failure with a more fulminant course for giant cell myocarditis patients. Heart transplantation may be required for end-stage heart failure, but transplantation does not necessarily protect from recurrence of the disease.
In conclusion, our results suggest, in accordance with previously published studies, that giant cell myocarditis is a disease that affects younger persons and is characterized by poorer clinical outcome after cardiac transplantation and more severe post-transplant complications in comparison with granulomatous myocarditis. However, future studies are required to elucidate the pathogenetic, clinical, and therapeutic implications of our results.
Disclosure
This article was not supported by any fund. Informed consent was obtained from all patients for being included in the study. The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
C. Steger, D. Höfer, and H. Antretter declare that there is no conflict of interest.
References
Saltykow S. Über diffuse Myokarditis. Arch Pathol Lab Med Anat. 1905;182:1.
Tesluk H. Giant cell versus granulomatous myocarditis. Am J Clin Pathol. 1956;26:1326–33.
Klein BR, Hedges TR, 3rd, Dayal Y, Adelman LS. Orbital myositis and giant cell myocarditis. Neurology. 1989;39:988–90.
de Jongste MJ, Oosterhuis HJ, Lie KI. Intractable ventricular tachycardia in a patient with giant cell myocarditis, thymoma and myasthenia gravis. Int J Cardiol. 1986;13:374–8.
Burke JS, Medline NM, Katz A. Giant cell myocarditis and myositis. Associated with thymoma and myasthenia gravis. Arch Pathol. 1969;88:359–66.
Kloin JE. Pernicious anemia and giant cell myocarditis. New association. Am J Med. 1985;78:355–60.
McKeon J, Haagsma B, Bett JH, Boyle CM. Fatal giant cell myocarditis after colectomy for ulcerative colitis. Am Heart J. 1986;111:1208–9.
Weidhase A, Grone HJ, Unterberg C, Schuff-Werner P, Wiegand V. Severe granulomatous giant cell myocarditis in Wegener’s granulomatosis. Klin Wochenschr. 1990;68:880–5.
Ariza A, López MD, Mate JL, Curós A, Villagrasa M, Navas-Palacios JJ. Giant cell myocarditis: monocytic immunophenotype of giant cells in a case associated with ulcerative colitis. Hum Pathol. 1995;26:121–3.
Ruis J, Yebra M, Sánches-Vegazo I, Ramos MP, Lacoma F, Gea JC. Giant cell myocarditis: a systemic disease? Apropos a case. Med Clin (Barc). 1993;101:459–61.
Schmid KO. Granulomatous giant cell polymyositis and myocarditis in benign thymoma. Verh Dtsch Ges Pathol. 1965;49:248–53.
Davies MJ, Pomerance A, Teare RD. Idiopathic giant cell myocarditis—a distinctive clinic-pathological entity. Br Heart J. 1975;37:192–5.
Truica CI, Hansen CH, Garvin DF, Meehan KR. Idiopathic giant cell myocarditis after autologous hematopoietic stem cell transplantation and interleukin-2 immunotherapy: a case report. Cancer. 1998;83:1231–6.
Cooper LT, Jr., Berry GJ, Shabetai R. Idiopathic giant cell myocarditis—natural history and treatment. Multicenter Giant Cell Myocarditis Study Group Investigators. N Engl J Med. 1997;336:1860–6.
Magnani JW, Dec GW. Myocarditis: current trends in diagnosis and treatment. Circulation. 2006;113:876–90.
Kandolin R, Lehtonen J, Salmenkivi K, Räisänen-Sokolowski A, Lommi J, Kupari M. Diagnosis, treatment, and outcome of giant-cell moycarditis in the era of combined immunosuppression. Circ Heart Fail. 2013;6:15–22.
Kindermann I, Barth C, Mahfoud F, Ukena C, Lenski M, Yilmaz A, Klingel K, Kandolf R, Sechtem U, Cooper LT, Böhm M. Update on myocarditis. J Am Coll Cardiol. 2012;59:779–92.
Cooper LT, Jr., ElAmm C. Giant cell myocarditis. Diagnosis and treatment. Herz. 2012;37:632–6.
Cooper LT, Jr., Berry GJ, Rizeq M, Schroeder JS. Giant cell myocarditis. J Heart Lung Transplant. 1995;14:394–401.
Moloney ED, Egan JJ, Kelly P, Wood AE, Cooper LT, Jr. Transplantation for myocarditis: a controversy revisited. J Heart Lung Transplant. 2005;24:1103–10.
Cooper LT, Jr. Giant cell myocarditis: diagnosis and treatment. Herz. 2000;25:291–8.
Nieminen MS, Salminen US, Taskinen E, Heikkila P, Partanen J. Treatment of serious heart failure by transplantation in giant cell myocarditis diagnosed by endomyocardial biopsy. J Heart Lung Transplant. 1994;13:543–5.
Theaker JM, Gatter KC, Brown DC, Heryet A, Davies MJ. An investigation into the nature of giant cells in cardiac and skeletal muscle. Hum Pathol. 1988;19:974–9.
Shariff S, Straatman L, Allard M, Ignaszewski A. Novel associations of giant cell myocarditis: two case reports and a review of the literature. Can J Cardiol. 2004;20:557–61.
Schumann C, Faust M, Gerharz M, Ortmann M, Schubert M, Krone W. Autoimmune polyglandular syndrome associated with idiopathic giant cell myocarditis. Exp Clin Endocrinol Diabetes. 2005;113:302–7.
Frustaci A, Cuoco L, Chimenti C, et al. Celiac disease associated with autoimmune myocarditis. Circulation. 2002;105:2611–8.
Nash CL, Panaccione R, Sutherland LR, Meddings JB. Giant cell myocarditis, in a patient with Crohn’s disease, treated with etanercept—a tumour necrosis factor-alpha antagonist. Can J Gastroenterol. 2001;15:607–11.
Kilgallen CM, Jackson E, Bankoff M, Salomon RN, Surks HK. A case of giant cell myocarditis and malignant thymoma: a postmortem diagnosis by needle biopsy. Clin Cardiol. 1998;21:48–51.
Kon T, Mori F, Tanji K, Miki Y, Kimura T, Wakabayashi K. Giant cell polymyositis and myocarditis associated with myasthenia gravis and thymoma. Neuropathology. 2013;33:281–7.
Tanahashi N, Sato H, Nogawa S, Satoh T, Kawamura M, Shimoda M. A case report of giant cell moycardits and myositis observed during the clinical course of invasive thymoma associated with myasthenia gravis. Keio J Med. 2004;53:30–42.
Sato H, Iwasaki E, Nogawa S, Suzuki S, Amano T, Fukuuchi Y, et al. A patient with giant cell myocarditis and myositis associated with thymoma and myasthenia gravis. Rinsho Shinkeigaku. 2003;43:496–9.
Ibi T, Sahashi K. Myasthenia gravis, giant cell polymyositis and cardiomyositis associated with thymoma. Ryoikibetsu Shokogun Shirizu. 2001;36:344–6.
Tomimoto H, Akiguchi I, Kameyama M, Haibara H, Kitaichi M. Giant cell myositis and myocarditis associated with myasthenia gravis and thymoma—an autopsy case. Rinsho Shinkeigaku. 1985;25:688–93.
Bourgeois-Droin C, Sauvanet A, Lemarchand F, De Roquancourt A, Cottenot F, Brocheriou C. Thymoma associated with myasthenia, erythroblastopenia, myositis and giant cell myocarditis. One case (author’s transl). Nouv Presse Med. 1981;10:2097–8.
Leib ML, Odel JG, Cooney MJ. Orbital polymyositis and giant cell myocarditis. Ophthalmology. 1994;101:950–4.
Lind-Ayres MR, Abramowsky C, Mahle WT. Pediatric giant cell myocarditis and orbital myositis. Pediatr Cardiol. 2009;30:510–2.
Kollmeier M, Brodhun M, Sliwka U, Sigusch H, Witte OW, Heide G. Diplopia and cardiogenic shock. Nervenarzt. 2006;77:187–8.
Sasaki H, Yano M, Kawano O, Hikosaka Y, Fujii Y. Thymoma associated with fatal myocarditis and polymyosisit in a 58-year-old man following treatment with carboplatin and paclitaxel: a case report. Oncol Lett. 2012;3:300–2.
Morrissey RP, Rana JS, Luthringer DJ, Cheng V, Czer LS, Philip K, Kass R, Schwarz ER. Case of fulminant giant-cell myocarditis associated with polymyositis, treated with a biventricular assist device and subsequent heart transplantation. Heart Lung. 2011;40:340–5.
Isobe K, Gocho K, Kaburaki K, Sugino K, Akasaka Y, Homma S. An autopsied case of giant cell myocarditis and myositis associated with invasive thymoma. Nihon Kokyuki Gakkai Zasshi. 2010;48:432–8.
Roberts WC, Kehoe JA, Carpenter DF, Golden A. Cardiac valvular lesions in rheumatoid arthritis. Arch Intern Med. 1968;122:141–6.
Kennedy LJ, Jr., Mitchinson MJ. Giant cell arteritis with myositis and myocarditis. Calif Med. 1971;115:84–7.
Benisch BM, Josephson M. Subacute (giant cell) thyreoiditis and giant cell myocarditis in patient with carcinoma of lung. Chest. 1973;64:764–5.
McCrea PC, Childers RW. Two unusual cases of giant cell myocarditis associated with mitral stenosis and with Wegener’s syndrome. Br Heart J. 1964;26:490–8.
Hales SA, Theaker JM, Gatter KC. Giant cell myocarditis associated with lymphoma: an immunocytochemical study. J Clin Pathol. 1987;40:1310–3.
Helliwell TR, Edwards RH. Giant cell myocarditis associated with lymphoma. J Clin Pathol. 1988;41:598–9.
Glennon PE, Petersen ME, Sheppard MN. Fatal giant cell myocarditis after resection of a thymoma. Heart. 1996;75:531–2.
Koul D, Kanwar M, Jefic D, et al. Fulminant giant cell myocarditis and cardiogenic shock: an unusual presentation of malignant thymoma. Cardiol Res Pract. 2010;2010:185896.
Ishikawa H, Kaneko H, Watanabe H, Takagi A, Ming ZW. Giant cell myocarditis in association with drug-induced skin eruption. Acta Pathol Jpn. 1987;37:639–44.
Daniels PR, Berry GJ, Tazelaar HD, Cooper LT. Giant cell myocarditis as a manifestation of drug hypersensitivity. Cardiovasc Pathol. 2000;9:287–91.
Kossovsky N, Cole P, Zackson DA. Giant cell myocarditis associated with silicone. An unusual case of biomaterials pathology discovered at autopsy using x-ray energy spectroscopic techniques. Am J Clin Pathol. 1990;93:148–52.
Laufs H, Nigrovic PA, Schneider LC, et al. Giant cell myocarditis in a 12-year-old girl with common variable immunodeficiency. Mayo Clin Proc. 2002;77:92–6.
Gillie I, Fox H. Mitral stenosis together with a giant cell myocarditis limited to the left atrium. J Clin Pathol. 1968;21:750–2.
Rabson AB, Schoen FJ, Warhol MJ, Mudge GH, Collins JJ, Jr. Giant cell myocarditis after mitral valve replacement: case report and studies of the nature of giant cells. Hum Pathol. 1984;15:585–7.
Steger CM, Hager T, Antretter H, et al. Cardiac sarcoidosis mimicking arrhythmogenic right ventricular dysplasia. BMJ Case Rep. 2009;2009. pii: bcr08.2009.2204. doi:10.1136/bcr.08.2009.2204.
Steger CM, Antretter H, Höfer D. Guillain-Barré syndrome due to CMV reactivation after cardiac transplantation. Case Rep Cardiol. 2012;2012:Article ID 506290.
Steger CM, Antretter H, Höfer D. Cardiac involvement in muscular dystrophies leading to heart transplantation. Eur Surg. 2013;45:245–50.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steger, C., Höfer, D. & Antretter, H. Giant cell and granulomatous myocarditis necessitating cardiac transplantation: clinical, gross, and histopathological findings. Eur Surg 46, 209–215 (2014). https://doi.org/10.1007/s10353-014-0269-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-014-0269-5