Abstract
The advantages of magnetoencephalography (MEG) in the field of epilepsy are numerous; just like electroencephalography (EEG), MEG is able to noninvasively measure epilepsy-specific information (i. e., the brain activity) independent of blood flow with a very high temporal resolution in the order of milliseconds. Thanks to its unique sensitivity to tangential sources, it gives the full picture when combined with EEG. It allows for accurate source imaging and shows a high sensitivity for neocortical sources. In this article, the technique and its clinical impact are reviewed.
Zusammenfassung
Die Magnetenzephalographie (MEG) bietet für die Anwendung in der Epileptologie verschiedene Vorteile. Ähnlich wie die Elektroenzephalographie (EEG) kann die MEG epilepsieassoziierte Muster der Hirnaktivität nichtinvasiv messen, unabhängig vom Blutfluss und mit einer sehr hohen zeitlichen Auflösung im Bereich von Millisekunden. Aufgrund der einzigartigen Sensitivität für tangentiale Quellen liefert sie in Kombination mit der EEG ein umfassendes Bild. Sie ermöglicht eine genaue Quellenanalyse und verfügt dabei über eine hohe Sensitivität für neokortikale Quellen. Der vorliegende Artikel beschreibt das Verfahren und fasst den Einfluss auf die klinische Praxis zusammen.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Physiology of cerebral potentials and MSI technique
Magnetoencephalography (MEG) has become an accepted clinical tool that can directly and noninvasively measure the magnetic fields produced by the brain. These fields are perpendicular to the electrical signals arising from the apical dendrites from pyramidal neurons orientated in parallel in the cortex [7]. The apical dendrites are orientated differently according to their position in the gyri and sulci. While MEG is selectively sensitive for sources that are tangentially orientated, i. e., mainly on the banks of the sulci, electroencephalography (EEG) is mainly sensitive for radially orientated sources (to a lesser extent to tangential sources), i. e., mainly on the top of the gyri [19].
The neuromagnetic fields are very small (10−15 T) and decrease in strength over the distance they cross (Biot–Savart law). Therefore, specific conditions and hardware are needed to record them. Firstly, environmental magnetic noise is reduced by a magnetic shielded room and secondly superconducting quantum interference devices (SQUIDs) imbedded in liquid helium (He) are used to pick up the small signals. Today, whole-head MEG systems are available with over 300 sensors imbedded in a helmet.
Despite the costs, MEG is advancing thanks to its more accurate and less complex source localization compared with EEG. MEG is therefore often referred to as magnetic source imaging (MSI).
MSI requires two “problems” to be solved: the “forward” and “inverse” problems. To solve the forward problem, a head model is required. In the case of EEG signals, the head model has to take into account the different conductivities of the tissues involved as well as the head geometry and the anisotropy of the white matter tracts and the skull because electrical signals are conducted differently through the cerebrospinal fluid, white or gray matter, bone, skull, etc. This results in a “patient-specific realistic multilayer head model,” which requires complex computations. As a result of the insensitivity of the magnetic field for the different conductivities and anisotropy, a “spherical one-layer head model” based on the patient’s individual magnetic resonance imaging (MRI) can be used for MSI.
Solving the inverse problem is based on modeling the sources responsible for producing signals within the brain cortex measured with the EEG electrodes or MEG SQUIDs. The inverse problem has no unique solution. MEG has advantages over EEG in estimating the inverse problem as the number of sensors may exceed 300 and radial sources can be excluded owing to the selective sensitivity of MEG for the tangential sources. The solution of the inverse problem is often represented by an equivalent current dipole (ECD), representing the source as a dipole being the center of gravity; however, other modeling techniques exist (such as minimum norm estimation [MNE], beamforming, SAM[synthetic aperture magnetometry]-kurtosis algorithm etc.), and most clinical data available today are based on ECD modeling [7].
MSI indications in epilepsy
Typically, epilepsy patients undergo the MEG recording in supine position lasting in European centers about 90 min (range, 60–420 min) and are encouraged to fall asleep during the acquisition [28]. In the recorded MEG data, different features are used to study the disease and more specifically to localize the epileptogenic zone as precisely as possible.
The value of interictal MSI
As a result of the acquisition circumstances, the most common feature measured with MEG is the interictal epileptiform discharge (IED) rather than the seizure. Depending on the localization of the so-called irritative zone, sensitivity to detect IEDs with MEG differs but is feasible in about three quarter of patients [21, 23]. Studies comparing IED on simultaneously recorded scalp EEG and MEG show the complementarity between the two techniques. In more than 50% of patients, IED can be identified on both scalp EEG and MEG, in 7% of patients only EEG shows IED, and in 18% only MEG shows IED. In 21% of patients, no spikes can be recorded with any of the two modalities. Interestingly, it was shown that 47% of patients who did not show spikes on scalp EEG did have spikes during 1 h of MEG recording [12].
Studies comparing ECoG with simultaneous MEG have shown that all MEG spikes had subdural counterparts, whereas 56% of the spikes recorded on ECoG were shown on MEG. However, for lateral neocortical, insular, intrasylvian, and (frontal) interhemispheric foci, this rate rose to 90% of spikes [20, 21]. With similar studies it was shown that in neocortical epilepsy, MEG picks up IED that extend no more than 3–4 cm2 of activated lateral frontal neocortex on subdural electrodes, up to 6 cm2 for more basal frontal and temporal neocortex, whereas other studies showed that scalp EEG only detects IED when 10 cm2 is activated [19, 26]. However, these studies did not use high-density EEG.
Diagnostic accuracy and added value
In neocortical cases, the current presurgical evaluation is not sufficient. The inclusion of MEG can be important as MEG is more sensitive for neocortical sources compared with deep sources.
Various studies have focused on frontal lobe epilepsy (FLE) as scalp EEG is often unable to detect interictal or ictal activity due to fast propagation, muscle activity, etc., whereas MEG can [18, 20]. The insular cortex is the second region that often causes difficulties in the current presurgical work-up. Several studies reported on the superiority of MEG over other techniques in the work-up of insular cases and confirmed this with intracranial monitoring [2, 17].
Although MEG seems more sensitive for neocortical sources, studies have confirmed that mesial temporal spikes can also be detected by MEG and can add crucial information [11]. In this case the orientation rather than the localization is important for distinguishing between mesial and lateral temporal lobe epilepsy. Vertical or horizontal MEG spikes in the anterior temporal pole indicate a higher chance of mesial temporal onset [11, 12].
Patients with nonlesional neocortical epilepsy represent the most difficult group within the presurgical evaluation as only 35% are rendered seizure free following epilepsy surgery [27]. MEG can serve as a guide to identify very subtle lesions or to plan intracranial implantation in these cases (see later). If focal MEG clusters can be found they are definitely valuable in decision-making in these cases. In this difficult patient group, MEG was compared with other presurgical investigations and the intracranial gold standard. MEG lateralizes correctly in 86% of cases compared with 78% for ictal video-EEG monitoring (VEM), 70% for FDG-PET (fluorodeoxyglucose-positron emission tomography), and 57% for ictal SPECT (single photon emission computed tomography). MEG and ictal VEM identified the correct lobe in 65% of cases, FDG-PET in 57% of cases, and ictal SPECT in 52% of cases [10].
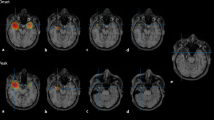
Besides the important role of MEG in nonlesional cases, it is also of important value in lesional cases. Focal cortical dysplasia (FCD), for example, is a highly and intrinsically epileptogenic lesion often causing intractable epilepsy treatable with epilepsy surgery. MRI can identify these lesions by showing blurring of the gray–white matter, cortical thickening, and abnormal signs in the white matter; however, the lesions might also be very subtle or even microscopic and not visible on optimal imaging. Owing to their intrinsic epileptogenicity, MEG plays an important role in the delineation of their extent and in predicting the outcome following resection [31]. Itabashi and colleagues concluded in their study on patients with very subtle and initially overlooked FCD that MEG-guided a posteriori review of MRI should become clinical practice [8].
In the case of cavernoma, the epilepsy is caused by the associated mass effect, gliosis, and hemosiderin. Therefore, the tissue adjacent to the lesion, rather than the cavernoma itself, exhibits hyperexcitability. In these patients, MEG helps to delineate the extent of the resection beyond the cavernoma. In cases of multiple cavernoma, MEG will probably “only” reveal the complexity of the case and contribute to the decision about further invasive work-up or rejection [24].
Localizing accuracy
Over the past 20 years, many studies investigated the role of MEG within the presurgical evaluation and compared the MEG results with the gold standard available, i. e., seizure outcome following resection and/or invasive recording.
Only a few are reported here: Stefan et al. performed a retrospective study including 455 cases and concluded that MEG identified the correct lobe in 89% of cases and added information in 33% and crucial information in 10% [23]. Knowlton et al. reported on a positive predictive value (PPV) of MSI for seizure localization of 82–90% depending on whether it was computed against intracranial recording alone or in combination with surgical outcome [13]. Knowlton et al. showed that a highly localized MSI result was significantly associated with seizure-free outcome [14]. Based on a retrospective analysis of the value of MEG performed at Cleveland between 2009 and 2012, Vadera et al. found that when preoperative MEG studies were fused with postoperative MRI, for 30 of 65 patients the MEG cluster was located within the resection cavity, for 28 of 65 completely outside the cavity, and for seven of 65 partially within; they showed a significantly improved likelihood of seizure freedom with complete clusterectomy in patients with localization outside the temporal lobe [30]. Englot et al. reported on 132 surgical cases. They concluded that a concordant and specific MEG result predicted seizure freedom with an odds ratio (OR) of 5.11 [5].
In 2008 Lau et al. systematically reviewed the literature and concluded that large randomized clinical trials were needed as at that time insufficient evidence was available to support the relationship between the use of MEG in surgical planning and seizure-free outcome after epilepsy surgery [15] Besides the fact that this review received a lot of critics for methodological misunderstandings, today the number of studies comparing the MEG result with postoperative outcome has only increased and the evidence for its value in the presurgical evaluation became only more established, so the need for a new systematic review is clear.
Therapeutic impact and added value
Various studies evaluated how the inclusion of MEG in the decision-making process changed patient management (Table 1). Overall, the studies concluded that adding MEG to the presurgical protocol changes management in 1/5–1/3 patients (depending on the inclusion level; [9, 14, 25, 29]).
Guidance of invasive video-EEG monitoring
An important role for MEG in the work-up is the optimal planning of intracranial recording since the implantation scheme is crucial. Knowlton showed this elegantly in his study including all patients planned for intracranial implantation. In this group, in 23% pf patients the MEG result resulted in extra electrode coverage and in 39% of these cases these extra electrodes involved the seizure onset [14]. Agirre-Arrizubieta compared patients who underwent MEG before their implantation with electrodes with a control group that underwent intracranial implantation without MEG. The MEG group consisted of more complex patients; however, no differences in successful implantations were found, suggesting that MEG contributes toward identifying the ideal implantation site when standard methods fail [1]. However, a randomized study would be the only way to prove this; nevertheless, the value of MEG in patient work-up is already established making randomization unethical.
The value of ictal MSI
Apart from IEDs, epilepsy is characterized by the occurrence of seizures and to date the ictal onset zone (SOZ) has always been considered the closest approximation of the epileptogenic zone. However, the recording of seizures during MEG acquisitions is difficult because the sessions are generally rather short (mean of 90 min [4]) and movement can cause problems for recording good signal quality. Still, the value of magnetic seizure activity has been described by different authors. The recording of ictal activity can be a coincidence or planned/anticipated for.
The first ictal MEG studies were performed with only a few channels or multichannel hemispherical MEG recordings combined with foramen ovale electrodes. Further ictal MEG studies showed that at seizure onset the signal-to-noise ratio (SNR) for dipole analysis may be too low or that artifacts obscure the seizure onset in some patients. In some successfully localized cases it was demonstrated that the ictal source localization was superior to interictal MEG and that there was a good correlation with invasively recognized seizure onset [4]. Continuous ictal head movement measurement later was also used for correction of movement artifacts in the study of Fujiwara et al. [6]. Here, instead of dipole analysis, short time Fourier transformation rhythm analysis was performed. In 63% of cases, concordant lobar interictal and ictal source localizations existed, the source of the ictal localization was closer than the interictal to the seizure onset zone defined by invasive EEG. Ictal MEG provided clear source localizations even if interictal MEG spikes were bilateral or missing. If interictal spikes were recorded as bilateral, then ictal recordings showed unilateral seizure activity. A comparison of interictal and ictal source localization was made by Medvedovsky [16]. In this study, the interictal MEG had a high sensitivity (95%) and moderate specificity (75%), while ictal MEG had high sensitivity (96%) and specificity (90%) in predicting SOZ localization on the lobe level in 12 patients with both ictal and interictal signals. Badier et al. compared SEEG epileptogenicity index, source localization using dipoles, and linearly constrained minimum variance (LCMV; a beamformer technique). It was found that source localization methods performed on rhythmic patterns could localize the epileptogenic zone as validated by SEEG. In terms of concordance, LCMV was superior to ECD [3].
Finally, it was shown that ictal MEG helped to convert drug-resistant epilepsy patients unsuitable for surgery or planned for phase II monitoring into candidates suitable for surgery; moreover, it resulted in favorable outcomes for those who were operated on, in other words ictal MEG changed the patient management of these difficult-to-manage refractory epilepsy patients [22].
Limitations
MEG clearly also holds some limitations:
-
Not only is reimbursement limited or lacking in many countries, but also the number of clinical MEG centers is still rather low, making the inclusion of MEG in the presurgical evaluation still not possible for all patients.
-
The presence of metal implants can cause artifacts blurring the physiological signals. Nevertheless, today software is able to reduce these artifacts significantly in most patients enabling interpretation of the data.
-
Negative MEG recording, i. e., when no IED and/or seizures could be recorded during the MEG acquisition, pose a problem for about one quarter of patients. Therefore alternative features are more and more often being studied. Not only slow activity but also fast activity has recently gained interest as well as network analysis such as, for example, spike-independent resting-state analysis (beyond the scope of this review).
-
Just like all results within the presurgical evaluation, MEG should always be combined with the results of the other investigations and all results need to be interpreted with caution before the team can decide upon the next step. No unique test is available to guide surgery and/or intracranial implantation on its own.
Practical conclusion
Who to refer for MEG:
-
Patients with normal scalp EEG can be referred for MEG since both techniques are to be considered complementary.
-
In patients with normal MRI and a focal MEG result, the MRI needs to be reviewed with the additional MEG information available to screen for subtle and originally missed lesions.
-
In patients with semiology or other noninvasive testing suggestive of frontal, intrasylvian, or insular seizure onset, MEG might be superior to EEG in identifying the irritative zone.
-
In the case of clear lesions, the MEG result might help to delineate the resection beyond the visible abnormality.
-
For patients planned for intracranial recording, MEG can be of benefit to optimally plan the implantation and overcome the sampling bias.
-
Ictal MEG can give additional information to interictal MEG and is possible in cases with a high likelihood of seizure recording.
References
Agirre-Arrizubieta Z, Thai NJ, Valentin A, Furlong PL, Seri S, Selway RP, Elwas RD, Alarcon G (2014) The value of MEG to guide electrode implantation in epilepsy. Brain Topogr 27(1):197–2017
Ahmed R, Otsubo H, Snead C, Donner E, Widjaja E, Ochi A, Drake JM, Rutka JT (2017) Diagnostic evaluation and surgical management of pediatric insular epilepsy utilizing magnetoencephalography and invasive EEG monitoring. Epilepsy Res 140:72–81
Badier JM, Bénar CG, Woodman M et al (2016) Ictal magnetic source. imaging in presurgical assessment. Brain Topogr 29:182–192
Eliashiv DS, Elsas SM, Squires K, Fried I, Engel J Jr (2002) Ictal magnetic source imaging as a localizing tool in partial epilepsy. Neurology 59:1600–1610
Englot DJ, Nagarajan SS, Imber BS, Raygor KP, Honma SM, Mizuiri D, Mantle M, Knowlton RC, Kirsch HE, Chan EF (2015) Epileptogenic zone localization using magnetoencephalography predicts seizure freedom in epilepsy surgery. Epilepsia 56(6):949–958
Fujiwara H, Greiner H, Hemasilpin N et al (2012) Ictal MEG onset source localization compared to intracranial EEG and outcome: improved epilepsy presurgical evaluation in paediatrics. Epilepsy Res 99(3):214–224
Hämäläinen M et al (1993) Magnetoencephalography—theory, instrumentation, and applications to noninvasive studies of the working human brain. Rev Mod Phys 65(2):414–495
Itabashi H, Jin K, Iwasaki M, Okumura E, Kanno A, Kato K, Tominaga T, Kawashima R, Nakasato N (2014) Electro- and magneto-encephalographic spike source localization of small focal cortical dysplasia in the dorsal peri-rolandic region. Clin Neurophysiol 125(12):2358–2363
Ito T, Otsubo H, Shiraishi H, Yagyu K, Takahashi Y, Ueda Y, Takeuchi F, Takahashi K, Nakane S, Kohsaka S, Saitoh S (2015) Advantageous information provided by magnetoencephalography for patients with neocortical epilepsy. Brain Dev 37(2):237–242
Jeong W, Chung CK, Kim JS (2012) Localization value of magnetoencephalography interictal spikes in adult nonlesional neocortical epilepsy. J Korean Med Sci 27(11):1391–1397
Kaiboriboon K, Nagarajan S, Mantle M, Kirsch HE (2010) Interictal MEG/MSI in intractable mesial temporal lobe epilepsy: spike yield and characterization. Clin Neurophysiol 121(3):32531
Kharkar S, Knowlton R (2015) Magnetoencephalography in the presurgical evaluation of epilepsy. Epilepsy Behav 46:19–26
Knowlton RC (2006) The role of FDG-PET, ictal SPECT, and MEG in epilepsy surgery evaluation. Epilepsy Behav 8(1):91–101
Knowlton RC, Razdan SN, Limdi N, Elgavish RA, Killen J, Blount J, Burneo JG, Ver Hoef L, Paige L, Faught E, Kankirawatana P, Bartolucci A, Riley K, Kuzniecky R (2009) Effect of epilepsy magnetic source imaging on intracranial electrode placement. Ann Neurol 65(6):716–723
Lau M, Yam D, Burneo JG (2008) A systematic review on MEG and its use in the presurgical evaluation of localization-related epilepsy. Epilepsy Res 79(2-3):97–104
Medvedovsky M (2015) Academic Dissertation. Helsinki
Mohamed IS, Gibbs SA, Robert M, Bouthillier A, Leroux JM, Khoa Nguyen D (2013) The utility of magnetoencephalography in the presurgical evaluation of refractory insular epilepsy. Epilepsia 54(11):1950–1959
Mu J, Rampp S, Carrette E, Roessler K, Sommer B, Schmitt FC, De Tiège X, Hamer H, Boon P, Pauli E, Bluemcke I, Zhou D, Buchfelder M, Stefan H (2014) Clinical relevance of source location in frontal lobe epilepsy and prediction of postoperative long-term outcome. Seizure 23(7):553–559
Oishi M et al (2002) Epileptic spikes: magnetoencephalography versus simultaneous electrocorticography. Epilepsia 43(11):1390–1395
Ossenblok P, de Munck JC, Colon A, Drolsbach W, Boon P (2007) Magnetoencephalography is more successful for screening and localizing frontal lobe epilepsy than electroencephalography. Epilepsia 48(11):2139–2149
Paulini A, Fischer M, Rampp S, Scheler G, Hopfengärtner R, Kaltenhäuser M, Dörfler A, Buchfelder M, Stefan H (2007) Lobar localization information in epilepsy patients: MEG—a useful tool in routine presurgical diagnosis. Epilepsy Res 76(2-3):124–130
Ramanujam B, Bharti K, Viswanathan V et al (2017) Can ictal-MEG obviate the need for phase II monitoring in people with drug-refractory epilepsy? A prospective observational study. Seizure 45:17–23
Stefan H, Hummel C, Scheler G, Genow A, Druschky K, Tilz C, Kaltenhäuser M, Hopfengärtner R, Buchfelder M, Romstöck J (2003) Magnetic brain source imaging of focal epileptic activity: a synopsis of 455 cases. Brain 126(pt11):2396–2405
Stefan H, Scheler G, Hummel C, Walter J, Romstöck J, Buchfelder M, Blümcke I (2004) Magnetoencephalography (MEG) predicts focal epileptogenicity in cavernomas. J Neurol Neurosurg Psychiatr 75(9):1309–1313
Sutherling WW, Mamelak AN, Thyerlei D, Maleeva T, Minazad Y, Philpott L, Lopez N (2008) Influence of magnetic source imaging for planning intracranial EEG in epilepsy. Neurology 71(13):990–996
Tao JX, Ray A, Hawes-Ebersole S, Ebersole JS (2005) Intracranial EEG substrates of scalp EEG interictal spikes. Epilepsia 46(5):669–676
Téllez-Zenteno JF, Hernández Ronquillo L, Moien-Afshari F, Wiebe S (2010) Surgical outcomes in lesional and non-lesional epilepsy: a systematic review and meta-analysis. Epilepsy Res 89(23):310–318
De Tiege X, Lundqvist D, Beniczky S, Seri S, Paetau R (2017) Current clinical magnetoencephalography practice across Europe: are we closer to use MEG as an established clinical tool. Seizure 50:53–59
De Tiège X, Carrette E, Legros B, Vonck K, Op de Beeck M, Bourguignon M, Massager N, David P, Van Roost D, Meurs A, Lapere S, Deblaere K, Goldman S, Boon P, Van Bogaert P (2012) Clinical added value of magnetic source imaging in the presurgical evaluation of refractory focal epilepsy. J Neurol Neurosurg Psychiatr 83(4):417–423
Vadera S, Jehi L, Burgess RC, Shea K, Alexopoulos AV, Mosher J, Gonzalez-Martinez J, Bingaman W (2013) Correlation between magnetoencephalography-based “clusterectomy” and postoperative seizure freedom. Neurosurg Focus 34(6):E9
Wilenius J, Medvedovsky M, Gaily E, Metsähonkala L, Mäkelä JP, Paetau A, Valanne L, Paetau R (2013) Interictal MEG reveals focal cortical dysplasias: special focus on patients with no visible MRI lesions. Epilepsy Res 105(3):337–348
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Carrette has received refunding for travel and registration costs and Prof. Stefan has received honoraria and travel reimbursement for lectures.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Carrette, E., Stefan, H. Magnetic source imaging. Z. Epileptol. 31, 192–196 (2018). https://doi.org/10.1007/s10309-018-0186-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10309-018-0186-x