Abstract
Purpose
Congenital central hypoventilation syndrome (CCHS) and rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD) are rare disorders of autonomic regulation with risk for disrupted neurocognitive development. Our aim is to summarize research on neurocognitive outcomes in these conditions, advance understanding of how to best support these individuals throughout development, and facilitate future research.
Methods
We conducted a narrative review of literature on neurocognitive outcomes in CCHS and ROHHAD, supplemented with previously unpublished data from patients with CCHS and ROHHAD at our Center for Autonomic Medicine in Pediatrics (CAMP).
Results
Individuals with CCHS and ROHHAD experience a wide range of neurocognitive functioning ranging from above average to below average, but are at particular risk for difficulties with working memory, processing speed, perceptual reasoning, and visuographic skills. An assessment framework emphasizing fluid cognition seems especially appropriate for these conditions. Owing to small cohorts and varied methods of data collection, it has been difficult to identify associations between disease factors (including CCHS PHOX2B genotypes) and cognitive outcomes. However, results suggest that early childhood is a period of particular vulnerability, perhaps due to the disruptive impact of recurrent intermittent hypoxic episodes on brain and cognitive development.
Conclusion
Neurocognitive monitoring is recommended as a component of routine clinical care in CCHS and ROHHAD as a marker of disease status and to ensure that educational support and disability accommodations are provided as early as possible. Collaborative efforts will be essential to obtain samples needed to enhance our understanding of neurocognitive outcomes in CCHS and ROHHAD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital central hypoventilation syndrome (CCHS) and rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD) are rare disorders with predominantly childhood onset and overlapping features including severe hypoventilation necessitating artificial ventilation, autonomic dysregulation, and risk for neural crest tumors [1]. These overlapping features pose risk for repeated cardiovascular dysregulation and hypoxic exposure, with potential adverse impact on neurodevelopment. Our center has extensive experience assessing neurocognition in CCHS and ROHHAD cohorts. Below we examine and compare disease manifestations in these conditions, review current knowledge of neurocognition in each, assess what the results may mean for utilization of neurocognition as a biomarker in these and other rare diseases, and offer recommendations for research and clinical management in CCHS and ROHHAD to reduce disease impact on neurodevelopment.
CCHS is an extremely rare neurocristopathy, with an estimated 3000 cases since 1970 [2]. Onset is typically in the neonatal period, although in a subset of individuals symptoms are identified after 1 month of age, described as later-onset CCHS (LO-CCHS), with the presumption that delayed symptom onset in those individuals is related to lesser disease severity. Primary clinical features of CCHS include alveolar hypoventilation resulting in hypoxemia/hypercarbia while asleep and awake, autonomic dysregulation, neural crest tumors, and Hirschsprung disease [3]. Individuals with CCHS are at risk for potentially life-threatening hypoxic and asphyxial episodes and thus require artificial ventilation while either asleep or awake and asleep, as life support. The genetic basis of CCHS has been established as a spectrum of mutations in the PHOX2B gene, a transcription factor that plays a critical role in early development of the autonomic nervous system. The most common CCHS-causing mutations in PHOX2B are expansions of a 20-alanine repeat region, known as polyalanine repeat mutations (PARMs), and there is a well-established association between increasing length of PHOX2B alanine expansions and severity of phenotypic features [4, 5]. Other CCHS-causing variations known as non-polyalanine repeat mutations (NPARMs) may also occur throughout the gene and lead to widely varying severity and presentations of the CCHS phenotype [6].
ROHHAD is a much rarer neurocristopathy, with fewer than 200 reported cases [7]. It presents unexpectedly in early childhood (ages 1.5–7 years) after seemingly typical physical and mental development. Upon disease onset, children are at risk for “stealth” onset of severe hypoventilation while asleep, necessitating artificial ventilation as life support, and, in severe cases, awake and asleep. Key disease features include the herald of rapid weight gain (20–30 pounds over 3–6 months), then disruptions of hypothalamic function, alveolar hypoventilation, and autonomic dysregulation [8, 9]. Despite attempts to identify a genetic basis for ROHHAD, its etiology has not been elucidated, though neural crest origin as well as autoimmune pathogenesis have been postulated [10], with suspected involvement of the hypothalamus and periaqueductal gray matter [11].
As presented in Table 1, CCHS and ROHHAD share the features of alveolar hypoventilation with need for artificial ventilation as life support, attention to autonomic dysregulation, and increased risk of neural crest tumors. Hypothalamic dysregulation with rapid-onset obesity are key features of ROHHAD (though a small subset of individuals with CCHS also experience growth hormone deficiency or thyroid dysfunction), while Hirschsprung disease is seen only in CCHS. The presence of a CCHS-related PHOX2B gene mutation excludes a diagnosis of ROHHAD.
Since neurocognitive difficulties are reported in many children with CCHS and ROHHAD, it is imperative to study and longitudinally follow neurocognitive functioning in these conditions and consider the extent to which neurocognitive outcomes are secondary to chronic intermittent hypoxemia, intrinsic disruption of neural development, or other factors such as altered blood pressure regulation and cerebral oxygenation/autoregulation. Furthermore, disease-extrinsic factors that can influence neurocognitive outcomes, such as socioeconomic status and parental education, must also be considered. Comparisons of individuals with CCHS, LO-CCHS, and ROHHAD may facilitate our understanding of how these factors are related to neurocognitive outcomes and how to best support this population throughout development. Below we review the published literature on neurocognition in each of these conditions.
Neurocognitive findings in CCHS
Importantly, a subset of studies below, including all studies published before 2003 when PHOX2B was established as the disease-defining gene for CCHS, do not include PHOX2B confirmation of diagnosis. Those studies established diagnoses on the basis of clinical features of CCHS, an approach that does not meet current diagnostic criteria. As such, all or some of the CCHS cases reported in those studies may not meet modern guidelines for CCHS diagnosis. To clarify this, any study lacking PHOX2B confirmation for some or all of its CCHS participants is marked with an asterisk upon first mention in the text below.
Questionnaire-based surveys
Questionnaire-based surveys were the focus of two investigations attempting to gauge the neurocognitive impact of CCHS. In 2004, Vanderlaan et al.* surveyed families of patients who were registered with the CCHS Family Network [12]. In total, 196 families (75% response rate) returned the surveys, primarily from countries that are socioeconomically advantaged, with patients’ ages ranging from infancy to middle adulthood. Of the 153 school-age participants, 63% reported having difficulty learning (25% involving reading/comprehension and 21% involving math/spatial concepts), 34% were receiving special education assistance, and 31% had repeated a grade in school. A 2009 survey by Montirosso et al. of 26 children with PHOX2B-confirmed CCHS described parental concerns related to attention, oral expression, and psychomotor skills in more than 30% of the sample, with particular concerns noted (65%) about attention problems [13].
Psychometric comparisons with peers
Table 2 presents an overview of investigations of neurocognition in CCHS that are discussed below, seven of which were descriptive and did not report formal statistical analyses. Those studies are identified in Table 2 by notations indicating a lack of significance testing. Unless explicitly indicated, the studies below did not report formal statistical comparisons of subjects with CCHS against general population means or a control group.
Concerns were first raised about the neurocognitive impact of CCHS in 1987 by Oren et al.*, who published a case report of six children and adolescents [14]. All were described as having mild to moderate learning disabilities and developmental delays requiring individualized educational programs, with delays particularly affecting fine motor and cognitive skills along with speech development.
Several years later, Marcus et al.* described medical and psychosocial outcomes of a cohort of 13 children with CCHS [15]. Results of neurocognitive testing were available for nine of the children, based upon the Kaufman Assessment Battery for Children (K-ABC) [16], the Peabody Picture Vocabulary Test (PPVT) [17], and the Beery Developmental Test of Visual Motor Integration (Beery) [18]. Eight of the nine had a delay of more than one standard deviation (SD) below the population mean on the K-ABC Mental Processing Composite, which estimates overall cognitive functioning. As a whole, the children were described as functioning in the “slow learner” range. Two children scored > 2 SD below the population mean, indicating significant delay. Delays were also noted on the PPVT, which measures receptive vocabulary, and the Beery, which measures visuographic skills. A retrospective study by Silvestri et al.* the same year described neurocognitive outcomes of 17 children and adolescents with CCHS based on a series of clinical evaluations, with measures that varied by age [19]. Indices of development and intelligence varied widely in their sample, from below the 5th percentile to the 85th percentile, with academic difficulties reported in 78% of their school-age participants. Also, 82% of the children who were evaluated using the Beery visuographic task scored below the 50th percentile. Ruof et al.* described K-ABC testing results of nine children with CCHS, with median scores for the Mental Processing Composite in the low average range, for the Sequential Processing Index (which emphasizes working memory) in the borderline deficient range, and for the Simultaneous Processing Index (which emphasizes gestalt-like integration of stimuli) in the mid-average range [20].
The first report of neurocognitive functioning in PHOX2B mutation-confirmed CCHS was published by Zelko et al. [21] with a sample of 20 patients ranging from school age to early adulthood, based upon Wechsler intelligence scales [22, 23]. The mean Full Scale IQ (FSIQ) of the sample was depressed significantly, falling one SD below the general population mean (p < 0.01). Scores on Wechsler subtests measuring perceptual reasoning (block design, p < 0.002) and processing speed (coding, p < 0.017) were significantly below population means, indicating particular vulnerabilities in those cognitive subdomains.
Early childhood neurocognitive outcomes in CCHS were addressed in a study by Charnay et al. based on administrations of the Bayley Scales of Infant Development [24] to a cohort of 31 children below 40 months of age [25]. Results indicated mean mental (p = 0.001) and motor development (p < 0.001) scores significantly below the general population mean, falling respectively in the low average and borderline deficient ranges.
Lagercrantz et al. administered the Wechsler intelligence scales and the Beery to a sample of 11 children and adults with CCHS [26]. They described median FSIQ and perceptual reasoning indexes in the borderline deficient range, verbal comprehension and working memory indexes in the mid average range, and processing speed and Beery scores in the very low average range. Macdonald et al. described results of Wechsler intelligence testing of a cohort of seven children and young adults with CCHS, with mean values for FSIQ, verbal comprehension, fluid reasoning, working memory, and processing speed in the borderline-deficient range [27].
A survey of physicians was used by Ogata et al.* to retrieve information from medical records of 123 patients with CCHS [28]. Results of neurocognitive testing with various scales of intelligence and development were obtained for 35 of the 88 patients aged 6 years and older whose records were surveyed for the study. Of the 35, 53% were found to be receiving special education or to have IQ scores < 75, indicating intellectual disability. Only a subset of this cohort had PHOX2B-confirmation of CCHS. Trang et al. followed 34 consecutive patients with CCHS who were administered Wechsler intelligence scales [29]. Their sample had a mean FSIQ in the low average range, and they found Wechsler working memory and processing speed scores to be significantly lower than verbal comprehension, visuospatial ability, and fluid reasoning scores.
Welbel et al. recently presented results of neurocognitive testing in 51 patients with CCHS with a novel computerized measure, the NIH Toolbox Cognitive Battery (NTCB) [30, 31]. Using this alternate test of mental ability, which breaks down cognition into crystallized (based upon past learning) and fluid cognition (based upon new learning and speed of information processing) components, they found the NTCB Fluid Cognition index (p < 0.001) and summary Cognition Composite (p = 0.01) to be significantly below population norms, while the NTCB Crystallized Cognition index did not significantly differ. They also studied Wechsler intelligence indices in a subsample of 24 of their patients with CCHS and found that, while all indices were below the population mean of 100, none of them was significantly depressed.
Heretofore unpublished data from our Center for Autonomic Medicine in Pediatrics (CAMP) are presented in Table 3, which provides the most recent Wechsler intelligence and Beery scores from clinical follow-up testing in a sample of 47 patients with CCHS ranging from 6 to 21 years of age. To our knowledge, this is the largest sample to date of individuals with CCHS who have received prospective Wechsler intellectual assessments. These data indicate significantly lower Wechsler indices of FSIQ, perceptual reasoning, working memory, and processing speed, and significantly lower Beery scores, than general population means.
Previously unpublished Bayley data from 15 of the youngest members of our current CCHS CAMP cohort (i.e., those below 6 years of age) indicate functioning in the low average range. Single-sample t-tests comparing means with the general population reveal that the Bayley Motor Development Index is significantly depressed (80.67 ± 26.52; t = −2.823, p = 0.014). The Bayley Cognitive Development Index is a standard deviation below the population mean but falls short of statistical significance (84.73 ± 33.25; t = −1.778, p = 0.097), as does the Bayley Language Development Index (89.07 ± 24.76; t = −1.710, p = 0.109) [24]. Though these data are limited by a modest sample size, they are consistent with the previous report of significantly depressed Bayley indices [25]. It is noteworthy that motor development scores were lower than cognitive development scores in both samples, though the differences between the two indices were not statistically significant in either sample.
Associations with CCHS phenotype, disease-intrinsic, and treatment factors
Several studies have attempted to identify associations between neurocognitive outcomes and clinical factors related to the severity and treatment of CCHS. A starting point for such analyses is the CCHS-related PHOX2B genotype. Among known patients with CCHS, 90–92% have PARM genotypes of 20/24 to 20/33 (heterozygous; in this nomenclature, the normal allele has 20 alanine repeats and affected allele has 24–33 alanine repeats; normal genotype is 20/20) [3]. PARM length correlates with CCHS phenotype severity, with longer expansions presenting greater need for respiratory support and increased risk of Hirschsprung disease, tumors, cardiovascular dysfunction, and autonomic dysregulation [3–5]. Consequently, associations between PHOX2B genotypes and neurocognitive outcomes have been a focus of interest.
In our studies of school-aged and older individuals, including our unpublished sample described above, we have been unable to identify statistically significant differences between groups with different PARM expansion lengths [21, 32]. However, Trang et al. reported significantly higher Wechsler working memory scores in school-aged children with a 20/25 genotype than in 20/26 and 20/27 genotype groups [29]. They also reported negative correlations between Wechsler intellectual indices and the number of polyalanine repeats, reaching statistical significance for Wechsler fluid reasoning and working memory scores. In a smaller CCHS sample (n = 7) preventing statistical analyses, Macdonald et al. noted that their subjects with a 20/27 genotype had, on average, lower IQ scores (58.33 ± 18.15) than those with a 20/25 genotype (86.33 ± 18.23) [27]. In their sample of preschool children, Charnay et al. found Bayley scores of mental and motor ability to be indistinguishable from the general population mean among those with a 20/25 genotype, and significantly higher in their 20/25 group than in their 20/26 and 20/27 genotype groups [25].
Another comparison of interest in CCHS involves individuals whose symptoms manifest after 1 month of age, a subset referred to as LO-CCHS. Our unpublished CAMP CCHS dataset presented above includes 12 individuals with LO-CCHS along with 35 individuals with typical neonatal onset CCHS, indicating that 25% of our CCHS clinical population falls into this later-onset group. Means from Wechsler intelligence testing in these two subgroups are presented in Table 4, along with t-tests comparing each group with population means. In our neonatal-onset CCHS group, mean Wechsler FSIQ, perceptual reasoning, working memory, and processing speed indices, and Beery visuographic scores, are significantly lower than the general population. However, in the LO-CCHS group, significant differences are only found for Wechsler perceptual reasoning and the Beery. We found no significant differences in direct comparisons between our neonatal-onset and LO-CCHS groups on any neurocognitive indices. While these findings suggest greater neurocognitive impact in neonatal-onset CCHS than LO-CCHS, given the small size of the LO-CCHS group, and the fact that indices such as Wechsler FSIQ were slightly (but not significantly) lower in the LO-CCHS group than in the neonatal onset CCHS group, it is important to be cautious in interpreting these results.
Shimokaze et al. described a cohort of 92 children with PHOX2B mutation-confirmed CCHS [33]. Of those, a subset of 19 with a 20/25 PHOX2B genotype received testing with various measures of intellectual ability, either the Enjoji Test of Analytical Development [34], the Kyoto Scale of Psychological Development [35], or the Wechsler intelligence scale [23]. The mean standard score for this subsample was in the borderline-deficient range, with 42% having scores below 80 and described as meeting criteria for intellectual disability. This sample is noteworthy because 12 out of the 19 were not diagnosed until after the neonatal period (i.e., > 1 month of age), although 8 of those 12 had experienced hypoventilation as neonates (i.e., ≤ 1 month of age). Delayed diagnoses in those 20/25 participants may have resulted in delay of ventilator support initiation, with adverse impact upon their neurocognitive outcomes. The median age of diagnosis in these 12 cases was 21.5 months (range 1–180 months), compared with a median age of diagnosis of 57.25 months (range 1.8–168 months) in the later-onset cohort of our above-described previously unpublished CAMP dataset.
Other clinical factors have also been studied in relation to neurocognitive outcomes in several CCHS cohorts, including hours/days of ventilatory support, duration of initial hospitalization, growth parameters (weight/height), pulmonary hypertension, seizures, brain atrophy, central and peripheral hearing deficits, ophthalmologic abnormalities [19], seizure history and use of a cardiac pacemaker [21], and age of disease onset and presence of Hirschsprung disease, without finding significant associations [29]. However, in their early-childhood cohort, Charnay et al. found significantly lower Bayley mental and motor scores in individuals with CCHS with a history of severe breath-holding spells, with prolonged sinus pauses, and requiring 24 h per day artificial ventilation, as well as significantly lower Bayley motor scores in individuals with a history of seizures [25]. As presented in Table 5, in our unpublished cohort of 15 patients with CCHS referenced above who were administered the Bayley, we found significantly lower cognitive (t = 3.387, p = 0.005), language (t = 3.342, p = 0.005), and motor (t = 3.624, p = 0.003) development scores in individuals with Hirschsprung disease than those without it. We also found significantly lower cognitive (t = 3.479, p = 0.004) and language (t = 2.454, p = 0.029) development scores in preschoolers with CCHS who have a a history of cyanotic breath-holding spells than those without them, but motor development scores were not significantly different (t = 2.039, p = 0.062).
Ventilatory method (mask versus tracheostomy) has been studied in relation to neurocognitive outcomes, with seemingly contradictory results. Trang et al. [29] reported higher Wechsler intelligence indices in patients with CCHS receiving mask ventilation than those receiving tracheostomy ventilation. This report contrasts with the findings of Ogata et al. [28], who reported that individuals treated with tracheostomy in the first 3 months of life had a better developmental prognosis than individuals managed via tracheostomy after 3 months of age or treated with mask ventilation. However a confound in the Trang et al. study is that their patients who received tracheostomy ventilation likely had more severe CCHS to start with, so the neurocognitive differences reported may reflect differences in baseline severity that resulted in mask versus tracheostomy treatment.
Associations with CCHS disease-extrinsic factors
While several studies of neurocognitive outcomes in CCHS have compared their functioning with general population norms, doing so risks biased results if factors potentially related to cognitive outcomes but extrinsic to the disease, such as socioeconomic status and parent education, differ in a CCHS sample from the general population. For example, in our own research we have noted a disproportionate share of participants from households with parents educated at or above the college level [32, 36]. This raises a potential confound because some areas of cognitive functioning are known to be associated with variables such as parent education [37], with cognitive test scores higher in children from households with higher parent education levels, which are in turn also related to socioeconomic status. As a result, cognitive impacts due to CCHS may be underestimated in a sample with higher-than-average parent education levels if it is compared with general population means, because those means do not reflect the anticipated cognitive benefit that parents’ higher educational status and/or socioeconomic privilege has on an individual with CCHS. Parents or other first-degree relatives in the same household represent a particularly interesting alternative comparison group. Differences between patients with CCHS and unaffected first-degree relatives living within the same household are more likely to be attributable to disease-intrinsic factors than differences between patients with CCHS and general population means, because patients and their parents are more closely matched on factors that are extrinsic to CCHS.
Following this reasoning, our group took an alternate approach to assessing the neurocognitive impact of CCHS by comparing the intellectual functioning of individuals with CCHS with their parents as well as with general population norms [32]. We did this using a brief IQ measure called the Shipley Institute of Living Scale, 2nd edition (Shipley-2), which provides indices of overall reasoning [38]. We expected parents to be slightly above the general population norm on these measures, and we also expected to find differences between patients with CCHS and their parents that we would not find between patients with CCHS and population norms. As predicted, parent means were slightly above the general population value of 100 for overall intelligence (103.9 ± 10.8), vocabulary (106.6 ± 8.6), and abstraction (101.0 ± 12.1), though the differences were not statistically significant. We found significant CCHS patient–parent differences for overall intelligence, vocabulary, and abstract reasoning, but not for perceptual reasoning. In contrast, differences between individuals with CCHS and general population norms were significant only for abstraction and perceptual reasoning. The impact of the comparison group (parent versus general population norms) for vocabulary scores was of particular interest, because vocabulary is strongly associated with socioeconomic status [39].
Neurocognitive findings in ROHHAD
Owing to its extreme rarity, current knowledge of neurocognitive outcomes in rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD) is based primarily on individual case and small multiple-case reports. Neuropsychiatric dysfunction has been noted, and it has been described as a key feature, though primarily in children with suboptimal artificial ventilation [8]. Disturbances of attention, personality, mood, and social behavior, including autistic spectrum symptomatology, have been reported in several very early case studies [40–44].
Neurocognitive difficulties have been noted in several of the same reports, though not as a consistent finding. Descriptions of neurocognitive functioning in ROHHAD have been mostly qualitative, though quantitative results of serial neuropsychological testing were provided for two children in a dual-case cyclophosphamide trial [10]. Core verbal and nonverbal ability estimates ranged from borderline deficient to mid-average for one child but were higher (low average to mid average) for the second. In a systematic review of ROHHAD surveying 28 single-case and 8 multiple-case reports, Lee et al. identified behavioral impairments in 60% of the sample, poor school performance in 6%, developmental delay in 6%, and intellectual disability in 4% [45]. Khaytin et al. recently published a 10-year retrospective report of a patient with ROHHAD with conservative ventilatory management [7]. The patient’s neurocognitive performances were largely stable over time, indicating verbal comprehension and processing speed in the high average to superior range, notably higher than low average to average performances on perceptual reasoning tasks, and contrasting even more with performances ranging from borderline deficient to average on visuographic and perceptual motor tasks. To our knowledge, a study presenting aggregated neurocognitive test results in ROHHAD has not been published.
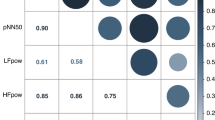
The Center for Autonomic Medicine in Pediatrics has been involved in the care of nearly 150 individuals with ROHHAD, and in the course of routine clinical follow-up we have collected neurocognitive test results from a sample of 19 individuals ranging in age from 7.4 to 18.5 years, with a mean of 12.3 years (SD 3.6). Portions of these data were previously presented in abstract form by Warner et al. [46]. Heretofore unpublished Wechsler intelligence and Beery visuographic test results from these evaluations are presented in Table 6, along with results of single-sample t-tests comparing them with general population means. The comparisons indicate significantly lower perceptual reasoning (p = 0.047), working memory (p = 0.023), and processing speed (p = 0.003) scores in patients with ROHHAD than in the general population. Additionally, patients scored significantly below population means on the Beery measure of visuographic skills, (87.00 ± 13.68, p < 0.001).
Three additional children in our ROHHAD cohort exhibited severe developmental delay and/or behavioral disturbance that prevented the administration of the Wechsler intelligence scales. Parent-reported ratings of adaptive functioning for those children indicated significant disability, based on General Adaptive Composite standard scores of 52, 53, and 55 on the Adaptive Behavior Assessment System, 2nd edition (ABAS-II) [47]. These outliers are particularly noteworthy because they resemble early ROHHAD case descriptions of neuropsychiatric disturbance. Although our 19 patients represent approximately 10% of the estimated worldwide prevalence of 200 individuals with ROHHAD, our sample is admittedly modest from a statistical standpoint, so it is not possible to perform formal tests of association between indices of neurocognitive functioning and ROHHAD disease factors.
Discussion
Collectively, research to date indicates that individuals with CCHS experience a wide range of neurocognitive functioning. Many are successful, and in fact thrive, with appropriate academic and therapeutic supports. As a group, however, they are at risk for reduced cognitive functioning relative to the general population. It has been difficult to quantify the degree of cognitive divergence associated with CCHS disease factors. Mean estimates of overall cognition (e.g., Wechsler Full Scale IQ) in different CCHS samples have varied from the borderline range (standard scores in the 70s) to the mid-average range (standard scores in the 90s), and it is unclear what factors account for this variability.
An obvious candidate is PHOX2B genotype. While Trang et al. found significant associations between Wechsler intelligence indices and PHOX2B genotypes in their CCHS sample [29], a similar finding has been reported only in a sample of very young children using the Bayley Scales of Infant Development [25]. Difficulties in identifying associations between genotypes and cognitive phenotypes may stem from the fact that most reports of neurocognitive outcome in CCHS have been based on samples of fewer than 30 individuals. The Trang et al. study, one of the largest, tested 34 children with Wechsler intelligence scales, including 8 patients with a 20/25 genotype, 11 with a 20/26 genotype, and 7 with a 20/27 genotype [29]. Similarly, the Charnay et al. study of 31 young children with CCHS included 7 patients with a 20/25 genotype, 9 with a 20/26 genotype, and 8 with a 20/27 genotype [25]. Given the modest size of genotype subsamples in most studies, conclusions regarding associations between cognitive outcomes and genotypes should be considered tentative. The question of a significant association between CCHS PHOX2B genotypes and neurocognitive outcomes is a critical one that clearly deserves further investigation in larger samples.
Studies of associations between neurocognitive outcomes and other CCHS disease factors have provided modest evidence of significant effects in the CCHS population as a whole. However, Charnay et al. found significant associations between history of severe breath-holding spells, prolonged sinus pauses, need for 24 h per day artificial ventilation, and seizures and performance on the Bayley Scales of Infant Development [25]. Similarly, our latest Bayley data, described above, also indicate significant associations between Bayley indices of development and the disease factors of Hirschsprung disease and cyanotic breath-holding episodes.
Findings of associations in early childhood between neurocognitive outcomes and CCHS genotypes and other disease factors raise the possibility that the relative contribution of these factors to cognitive outcomes (as compared with other factors such as ventilatory/medical management and socioeconomic factors) may vary with age. For example, the variance contributed by PHOX2B genotype and CCHS disease severity to cognitive outcomes may be greater in early childhood, a critical period of brain development, especially if CCHS diagnosis is delayed and a child experiences hypoxic events as a result. In later childhood and adulthood, with effective ventilation and stable disease management, the relative impact of other factors such as socioeconomic status, parent education, and educational interventions may increase. Factors extrinsic to both CCHS and ROHHAD such as socioeconomic status must be considered in future investigations, either by comparing affected individuals with a group that is more closely matched to them than the general population, or by covarying for extrinsic factors such as parent education levels to the extent possible. In this review we have not addressed the stability or evolution of neurocognitive phenotypes in CCHS and ROHHAD over time. No published studies to date have studied neurocognitive functioning longitudinally in CCHS or ROHHAD cohorts. This is an extremely important question that will require collaborative efforts with carefully designed neurocognitive assessment protocols.
An important challenge to address in studying CCHS is the potential for conflation between indicators of age of onset and indicators of disease severity. While a positive PHOX2B gene test conclusively establishes a diagnosis of CCHS and indicates the expected phenotype severity based on the effect on the PHOX2B protein, it is the emergence of clinical symptomatology that brings an individual to the attention of a physician who is then able to recognize its significance and obtain a confirmatory PHOX2B test. Individuals with more severe genetic mutations who are the most neurodevelopmentally vulnerable generally exhibit visible clinical symptomatology earlier and are diagnosed earlier. But, for some individuals with milder PHOX2B gene variants, recognition of features such as hypoventilation and autonomic dysregulation may be delayed, along with appropriate treatment. The concern is that, even in individuals with the mildest PHOX2B genotype, delayed identification and treatment may result in repeated early hypoxic episodes along with cardiovascular and other ANS dysregulation events that may disrupt typical neurocognitive development. These findings emphasize the importance of the earliest years of childhood as a period of neurocognitive vulnerability in CCHS deserving particular research attention. Unraveling the impact of factors such as CCHS severity and ventilatory method upon neurocognitive outcome will be difficult. Given the ATS CCHS Policy Statement [3] and the consensus within the field that tracheostomy ventilation is the only appropriate method in individuals with severe CCHS, a true clinical trial is not feasible. Methodologies such as random assignment to mask versus tracheostomy treatment groups, regardless of disease severity, cannot be carried out owing to the extreme risk of hypoxic events affecting brain functioning and neurocognitive development.
Compared with general population norms, areas of cognition related to fluid abilities such as working memory and processing speed appear particularly likely to be underdeveloped in CCHS. In contrast, areas of cognition related to crystallized ability such as vocabulary and verbal comprehensions appear to be less severely affected. Similar findings are seen in other clinical populations such as traumatic brain injury and dementia, and the neuroanatomical circuitry underlying fluid cognition is generally thought to be more vulnerable to insult than the circuitry of crystallized cognition in a variety of neurologic and systemic medical disorders. However, verbal difficulties may be underestimated by comparisons of individuals with CCHS with general population norms, because CCHS samples have often been drawn from households that confer socioeconomic and educational advantages to a child’s verbal abilities. When those advantages are controlled for by comparing children with CCHS against their parents, differences of verbal ability may also become apparent. Repeated findings of visuographic and Bayley Motor Development performances significantly below the population mean also indicate that perceptual-motor and fine motor skills are areas of special vulnerability in CCHS. Interestingly, visuographic and perceptual reasoning performances are also significantly depressed in ROHHAD. These findings suggest that measures of visuographic and perceptual-motor skills are likely to be especially useful for monitoring outcomes in both CCHS and ROHHAD.
Owing to its exceptional rarity, our knowledge about neurocognitive outcomes in ROHHAD is severely limited, and largely based on single-case and multiple-case reports that have anecdotally noted neuropsychiatric impairments in a subset of individuals with ROHHAD. Given the lack of published group studies of individuals with ROHHAD, it is difficult to know the extent to which cases with neuropsychiatric impairment represent a distinct subgroup. However, our own sample, as presented in Table 5, suggests that individuals with ROHHAD experience a range of neurocognitive outcomes, some having difficulties with working memory, processing speed, perceptual reasoning, and visuographic skills that are similar to those seen in CCHS. The longitudinal case study by Khaytin et al. [7] illustrates the point that, with conservative management, neurocognitive outcomes in ROHHAD can be excellent. The subgroup of children with ROHHAD that we found “untestable” is small (in our experience, 3 out of 22) but of particular interest, because it connects with past case reports, and because a similar level of behavioral disturbance is rarely seen in CCHS. The presence of this small and apparently distinct subgroup with severe neuropsychiatric disturbance raises the possibility of a “bifurcation” of neurocognitive outcomes in ROHHAD, with most individuals experiencing relatively mild challenges but with a small group of individuals experiencing severe behavioral and cognitive disability for reasons that are unclear.
Inconsistency of findings regarding associations between disease factors and neurocognitive outcomes in CCHS is undoubtedly in part a consequence of the small sizes of samples in published studies of this rare condition. As noted above, even fewer data are available on ROHHAD. However, inconsistency may also result from protocols for the collection of clinical and neurocognitive data that vary over time (e.g., different intellectual measures used at different ages) and from one research setting to another. Inconsistent findings may also reflect the possibility that, even when they are significant, associations (effect sizes) between disease factors and neurocognitive outcomes are modest, or that they vary over a patient’s lifetime, for example, being greater in critical years of neurocognitive development in early childhood but decreasing as an individual with CCHS gets older. A clear and differentiated picture of neurocognitive outcomes in CCHS and ROHHAD will be possible only with the development of large datasets via collaborations among clinical research centers.
Figure 1 shows a conceptual model depicting the myriad factors that may affect neurocognitive outcomes in CCHS and ROHHAD. The model emphasizes the complexity of intrinsic (i.e., disease-related), treatment-related, and extrinsic (e.g., environmental, social) factors that may influence neurocognitive outcomes in CCHS and ROHHAD. This complexity poses a challenge to researchers aiming to explicate neurocognitive outcomes in these conditions, because their rarity limits data gathering and statistical analyses.
Recommendations
-
1)
Standardized neurocognitive testing of those with CCHS and ROHHAD should occur every 6 months under the age of 3 years and then annually after age 3 as a routine component of clinical care. Interval testing is essential for timely recognition of educational and disability accommodation needs, to ensure that individuals with CCHS and ROHHAD are optimally supported in working toward their full potential. Longitudinal neurocognitive testing may also serve as a marker of general physiologic wellness and stability.
-
2)
Neurocognitive monitoring in CCHS and ROHHAD should target areas such as working memory, processing speed, perceptual reasoning, and visuographic skills, which appear to be particularly vulnerable in both conditions. The crystallized/fluid ability model of cognition noted above seems especially promising as a framework for monitoring, with a primary focus on fluid cognition.
-
3)
While it is not a substitute for comprehensive clinical neuropsychological assessment, the NIH Toolbox Cognitive Battery (NTCB) is recommended as a novel, economical, time-effective, and highly transferable measure of neurocognitive functioning that can facilitate longitudinal neurocognitive monitoring and collaboration across centers caring for individuals with CCHS and ROHHAD. However, aside from English, the NTCB has been formally validated only in Spanish, Swahili, and Dholuo [48, 49], so universal application is not currently possible and will require its adaptation to other languages and cultures.
-
4)
To deepen our understanding of CCHS and ROHHAD, collaborative efforts across centers caring for individuals with these conditions will be essential, with aggregated samples large enough to provide statistical power necessary for analyses of intrinsic and extrinsic factors, as well as longitudinal neurocognitive outcomes. It will be necessary for future collaborative research to collect consistent data across centers that clearly define variables such as age at symptom onset as well as age at formal diagnosis, along with details of ventilatory and other interventions and management compliance, as well as extrinsic variables such as parent education and socioeconomic status. The NIH Toolbox Cognitive Battery (NTCB) is an excellent example of an easily transferable measure that could facilitate collaborative study of neurocognitive outcomes in these conditions, though ongoing use of traditional neurocognitive measures will also play a critical role in longitudinal neurocognitive research and clinical follow-up.
References
Saiyed R, Rand C, Carroll MS, Weese-Mayer DE (2014) Hypoventilation syndromes of infancy, childhood, and adulthood: congenital central hypoventilation syndrome (CCHS), later-onset CCHS, and rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation. Sleep Med Clin 9:P425-439
Weese-Mayer DE, Rand CM, Khaytin I, Slattery SM, Yap KL, Marazita ML, Berry-Kravis EM (2021) Congenital Central Hypoventilation Syndrome. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Mirzaa GM, Amemiya A (eds). GeneReviews((R)). Seattle (WA)
Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Keens TG, Loghmanee DA, Trang H, Subcommittee ATSCCHS (2010) An official ATS clinical policy statement: congenital central hypoventilation syndrome: genetic basis, diagnosis, and management. Am J Respir Crit Care Med 181:626–644
Weese-Mayer DE, Berry-Kravis EM, Zhou L, Maher BS, Silvestri JM, Curran ME, Marazita ML (2003) Idiopathic congenital central hypoventilation syndrome: analysis of genes pertinent to early autonomic nervous system embryologic development and identification of mutations in PHOX2b. Am J Med Genet A 123A:267–278
Matera I, Bachetti T, Puppo F, Di Duca M, Morandi F, Casiraghi GM, Cilio MR, Hennekam R, Hofstra R, Schober JG, Ravazzolo R, Ottonello G, Ceccherini I (2004) PHOX2B mutations and polyalanine expansions correlate with the severity of the respiratory phenotype and associated symptoms in both congenital and late onset central hypoventilation syndrome. J Med Genet 41:373–380
Zhou A, Rand CM, Hockney SM, Niewijk G, Reineke P, Speare V, Berry-Kravis EM, Zhou L, Jennings LJ, Yu M, Ceccherini I, Bachetti T, Pennock M, Yap KL, Weese-Mayer DE (2021) Paired-like homeobox gene (PHOX2B) nonpolyalanine repeat expansion mutations (NPARMs): genotype–phenotype correlation in congenital central hypoventilation syndrome (CCHS). Genet Med 23:1656–1663
Khaytin I, Stewart TM, Zelko FA, Kee MAL, Osipoff JN, Slattery SM, Weese-Mayer DE (2022) Evolution of physiologic and autonomic phenotype in rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation over a decade from age at diagnosis. J Clin Sleep Med 18:937–944
Ize-Ludlow D, Gray JA, Sperling MA, Berry-Kravis EM, Milunsky JM, Farooqi IS, Rand CM, Weese-Mayer DE (2007) Rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation presenting in childhood. Pediatrics 120:e179–188
Carroll MS, Patwari PP, Kenny AS, Brogadir CD, Stewart TM, Weese-Mayer DE (2015) Rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD): response to ventilatory challenges. Pediatr Pulmonol 50:1336–1345
Jacobson LA, Rane S, McReynolds LJ, Steppan DA, Chen AR, Paz-Priel I (2016) Improved behavior and neuropsychological function in children with ROHHAD after high-dose cyclophosphamide. Pediatrics 138(1): e20151080
Chow C, Fortier MV, Das L, Menon AP, Vasanwala R, Lam JC, Ng ZM, Ling SR, Chan DW, Choong CT, Liew WK, Thomas T (2015) Rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD) syndrome may have a hypothalamus-periaqueductal gray localization. Pediatr Neurol 52:521–525
Vanderlaan M, Holbrook CR, Wang M, Tuell A, Gozal D (2004) Epidemiologic survey of 196 patients with congenital central hypoventilation syndrome. Pediatr Pulmonol 37:217–229
Montirosso R, Morandi F, D’Aloisio C, Berna A, Provenzi L, Borgatti R (2009) International classification of functioning, disability and health in children with congenital central hypoventilation syndrome. Disabil Rehabil 31(Suppl 1):S144–152
Oren J, Kelly DH, Shannon DC (1987) Long-term follow-up of children with congenital central hypoventilation syndrome. Pediatrics 80:375–380
Marcus CL, Jansen MT, Poulsen MK, Keens SE, Nield TA, Lipsker LE, Keens TG (1991) Medical and psychosocial outcome of children with congenital central hypoventilation syndrome. J Pediatr 119:888–895
Kaufman AS, Kaufman NL (1983) Kaufman Assessment Battery for Children (K-ABC). American Guidance Service, Circle Pines, MN
Dunn LM (1997) Peabody Picture Vocabulary Test—third edition (PPVT-III). American Guidance Service, Circle Pine, MN
Beery KE, Buktenica NA, Beery MA (2010) The Beery-Buktenica Developmental Test of Visual-Motor Integration: administaration, scoring, and teaching manual, 6th edn. Pearson, Minneapolis, MN
Silvestri JM, Weese-Mayer DE, Nelson MN (1992) Neuropsychologic abnormalities in children with congenital central hypoventilation syndrome. J Pediatr 120:388–393
Ruof H, Hammer J, Tillmann B, Ghelfi D, Weber P (2008) Neuropsychological, behavioral, and adaptive functioning of Swiss children with congenital central hypoventilation syndrome. J Child Neurol 23:1254–1259
Zelko FA, Nelson MN, Leurgans SE, Berry-Kravis EM, Weese-Mayer DE (2010) Congenital central hypoventilation syndrome: neurocognitive functioning in school age children. Pediatr Pulmonol 45:92–98
Wechsler D (2008) Wechsler Adult Intelligence Scale, 4th edn. Pearson, San Antonio, TX
Wechsler D (2014) Wechsler Intelligence Scale for Children, 5th edn. Pearson, San Antonio, TX
Bayley N (2006) Bayley scales of infant and toddler development® 3rd edition (Bayley-III®). The Psychological Corporation, San Antonio, TX
Charnay AJ, Antisdel-Lomaglio JE, Zelko FA, Rand CM, Le M, Gordon SC, Vitez SF, Tse JW, Brogadir CD, Nelson MN, Berry-Kravis EM, Weese-Mayer DE (2016) Congenital central hypoventilation syndrome: neurocognition already reduced in preschool-aged children. Chest 149:809–815
Lagercrantz R, Bergman K, Lagercrantz H, Markström A, Böhm B (2020) Neurocognitive function and quality of life with congenital central hypoventilation syndrome. J Sleep Med Disord 6:1097–1101
Macdonald KT, Mosquera RA, Yadav A, Caldas-Vasquez MC, Emanuel H, Rennie K (2020) Neurocognitive functioning in individuals with congenital central hypoventilation syndrome. BMC Pediatr 20:194
Ogata T, Muramatsu K, Miyana K, Ozawa H, Iwasaki M, Arakawa H (2020) Neurodevelopmental outcome and respiratory management of congenital central hypoventilation syndrome: a retrospective study. BMC Pediatr 20:342
Trang H, Bourgeois P, Cheliout-Heraut F (2020) Neurocognition in congenital central hypoventilation syndrome: influence of genotype and ventilation method. Orphanet J Rare Dis 15:322
Akshoomoff N, Newman E, Thompson WK, McCabe C, Bloss CS, Chang L, Amaral DG, Casey BJ, Ernst TM, Frazier JA, Gruen JR, Kaufmann WE, Kenet T, Kennedy DN, Libiger O, Mostofsky S, Murray SS, Sowell ER, Schork N, Dale AM, Jernigan TL (2014) The NIH toolbox cognition battery: results from a large normative developmental sample (PING). Neuropsychology 28:1–10
Welbel RZ, Rand CM, Zhou A, Fadl-Alla A, Chen ML, Weese-Mayer DE, Zelko FA (2022) Neurocognitive monitoring in congenital central hypoventilation syndrome with the NIH Toolbox(R). Pediatr Pulmonol 57:2040–2047
Zelko FA, Stewart TM, Brogadir CD, Rand CM, Weese-Mayer DE (2018) Congenital central hypoventilation syndrome: broader cognitive deficits revealed by parent controls. Pediatr Pulmonol 53:492–497
Shimokaze T, Sasaki A, Meguro T, Hasegawa H, Hiraku Y, Yoshikawa T, Kishikawa Y, Hayasaka K (2015) Genotype-phenotype relationship in Japanese patients with congenital central hypoventilation syndrome. J Hum Genet 60:473–477
Enjoji M, Yanai N (1961) Analytic test for development in infancy and childhood. Pediatr Int 4:2–6
Ikuzawa M, Matsushita Y, Nakase A (2002) The Kyoto Scale of Psychological Development test. Kyoto International Social Welfare Exchange Centre, Kyoto, Japan
Welbel RZ, Rand CM, Zhou A, Fadl-Alla A, Chen ML, Weese-Mayer DE, Zelko FA (2022) Neurocognitive monitoring in congenital central hypoventilation syndrome with the NIH Toolbox®. Pediatr Pulmonol 57:2040–2047.
Cave SN, Wright M, von Stumm S (2022) Change and stability in the association of parents’ education with children’s intelligence. Intelligence 90:1–8
Shipley W, Gruber C, Martin T, Klein A (2009) Shipley-2 Manual. Western Psychological Services, Los Angeles, CA
Maguire MJ, Schneider JM, Middleton AE, Ralph Y, Lopez M, Ackerman RA, Abel AD (2018) Vocabulary knowledge mediates the link between socioeconomic status and word learning in grade school. J Exp Child Psychol 166:679–695
Grudnikoff E, Foley C, Poole C, Theodosiadis E (2013) Nocturnal anxiety in a youth with rapid-onset obesity, hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD). J Can Acad Child Adolesc Psychiatry 22:235–237
Kocaay P, Siklar Z, Camtosun E, Kendirli T, Berberoglu M (2014) ROHHAD syndrome: reasons for diagnostic difficulties in obesity. J Clin Res Pediatr Endocrinol 6:254–257
Erensoy H, Ceylan ME, Evrensel A (2016) Psychiatric symptoms in rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation syndrome and its treatment: a case report. Chin Med J (Engl) 129:242–243
Kot K, Moszczynska E, Lecka-Ambroziak A, Migdal M, Szalecki M (2016) ROHHAD in a 9 year-old boy—clinical case. Endokrynol Pol 67:226–231
Al-Harbi AS, Al-Shamrani A, Al-Shawwa BA (2016) Rapid-onset obesity, hypothalamic dysfunction, hypoventilation, and autonomic dysregulation in Saudi Arabia. Saudi Med J 37:1258–1260
Lee JM, Shin J, Kim S, Gee HY, Lee JS, Cha DH, Rim JH, Park SJ, Kim JH, Ucar A, Kronbichler A, Lee KH, Shin JI (2018) Rapid-onset obesity with hypoventilation, hypothalamic, autonomic dysregulation, and neuroendocrine tumors (ROHHADNET) syndrome: a systematic review. Biomed Res Int 2018:1250721
Warner JJ, Zelko FA, Weese-Mayer DE (2018) Rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation (ROHHAD): dichotomy of Neurocognitive Performance. In: American Thoracic Society. San Diego, CA
Harrison P, Oakland T (2003) Adaptive Behavior Assessment System, 2nd edn. Pearson, San Antonio, IX
Gershon RC, Fox RS, Manly JJ, Mungas DM, Nowinski CJ, Roney EM, Slotkin J (2020) The NIH Toolbox: overview of development for use with Hispanic populations. J Int Neuropsychol Soc 26:567–575
Duffey MM, Ayuku D, Ayodo G, Abuonji E, Nyalumbe M, Giella AK, Hook JN, Tran TM, McHenry MS (2022) Translation and cultural adaptation of NIH Toolbox cognitive tests into Swahili and Dholuo languages for use in children in western Kenya. J Int Neuropsychol Soc 28:414–423
Funding
This project was supported by the PHOX2B Patent Fund Chicago Community Trust Foundation and the National Institutes of Health National Center for Advancing Translational Sciences (NUCATS) Pilot and Voucher Grant. The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Contributions
Conceptualization: F.A.Z., R.Z.W., C.M.R., D.W.-M.; literature search: F.A.Z., R.Z.W., C.M.R., D.W.-M.; data collection/curation: F.A.Z., C.M.R., T.S., A.F.A., I.K., S.M.S., D.W.-M.; writing, original draft: F.A.Z., R.Z.W., C.M.R.; writing, review and editing: F.A.Z., R.Z.W., C.M.R., T.S., A.F.A., I.K., S.M.S., D.W.-M.; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Data presented from the Center for Autonomic Medicine in Pediatrics were collected under research approved by the Internal Review Board of the Ann & Robert H. Lurie Children’s Hospital of Chicago (protocols 2013–15230, 2016–137, 2017–1399). Consent for participation was obtained from subjects age 18 years and older, and from parents of individuals under 18 years of age. Assent for participation was also obtained from individuals between 12 and 17 years of age.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zelko, F.A., Welbel, R.Z., Rand, C.M. et al. Neurocognition as a biomarker in the rare autonomic disorders of CCHS and ROHHAD. Clin Auton Res 33, 217–230 (2023). https://doi.org/10.1007/s10286-022-00901-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-022-00901-1