Abstract
Purpose
Postural tachycardia syndrome (POTS) is a disorder featured by orthostatic intolerance. The purpose of this study was to investigate the severity of quality of life issues in POTS patients.
Methods
Online surveys for health related quality of life, sleep quality, fatigue, pain, and suicidal ideation were completed by 624 POTS patients and 139 controls.
Results
People with POTS have significantly more days of poor physical health (p < 0.001), fewer days with good energy (p < 0.001), and significantly more days with activity limitations (p < 0.001) than controls. Pain severity was significantly higher for those with POTS (p < 0.001) while feelings of control over life was lower than controls (p < 0.001). Sleep quality and daytime fatigue were also significantly worse for those with POTS than controls (p < 0.001). Finally, those with POTS have a significantly higher risk of suicide compared with controls (p < 0.001).
Interpretation
The myriad of symptoms from which many POTS patients suffer is associated with a decreased quality of life. Nearly half of our sample with POTS was at high risk for suicide. More work needs to be done to determine the underlying issues surrounding suicide in POTS so that an appropriate treatment regimen can be developed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postural tachycardia syndrome (POTS) is indicated by a supine-to-standing heart rate increase of ≥30 beats per minute in adults and ≥40 beats per minute in adolescents in the absence of postural hypotension [1]. POTS is a heterogeneous disorder [2] with symptoms that include neuropathic pain [1, 3], poor sleep efficiency [4], chronic fatigue [5], headaches, palpitations, tremors, gastrointestinal disturbance, facial flushing [3, 6], and orthostatic symptoms like dizziness, lightheadedness, and syncope [7]. POTS typically manifests in young, well-educated women [8] but can occur in both genders at any age.
The varying etiology and co-morbid diagnoses can make treating POTS difficult. The fact that there are no US Food and Drug Administration approved medications for treatment of POTS [9] requires physicians to prescribe off-label medications. To further complicate matters, many medications used to treat co-morbid conditions may exacerbate POTS symptoms [2]. As a result, many POTS patients get little relief from current treatment regimens for POTS.
POTS decreases quality of life [8, 10–13]. Physical functioning, bodily pain, general health, and social functioning are significantly impaired in those with POTS [8]. The severity of orthostatic intolerance symptoms (e.g., lightheadedness, brain fog, and palpitations) may lead to both depression and diminished quality of life in POTS patients [13]. Approximately 25% of POTS patients are disabled and unable to work or attend school [8, 14]. The quality of life in POTS patients is comparable to those with rheumatoid arthritis, end-stage renal disease [15], congestive heart failure, and chronic obstructive pulmonary disease [8].
The purpose of this study was to assess the health-related quality of life for people with POTS using a large, cross-sectional sample. Standardized measures were used to identify health related quality of life issues and suicide risk in this chronically ill population. We hypothesized that people with POTS would have a significantly decreased health-related quality of life and increased risk of suicide compared to non-POTS controls.
Methods
Participants
Participants were recruited online via targeted campaigns through the Standing Up to POTS Facebook page. In order to recruit non-POTS control participants, advertisements asking for healthy controls were run via the Standing Up to POTS Facebook page that targeted members and their Facebook friends. As a result, many control participants were likely family members of those with POTS. There were 624 adults reporting physician diagnosed POTS (607 females, 15 males, 2 undeclared; mean age 33.76, SD = 11.30) and 139 non-POTS controls (118 females, 21 males; mean age 40.99, SD = 14.18) who completed the Healthy Days Core Module, West Haven-Yale Multidimensional Pain Inventory-Part I, Pittsburgh Quality Sleep Inventory, Fatigue Severity Survey, and the Suicide Behavior Questionnaire-Revised. The POTS group had been symptomatic for more than a decade (mean = 10.7 years, SD = 11.88) and seen an average of 7.4 (SD = 5.29) healthcare providers in the past year.
Procedure
Participants electronically signed the informed consent form before opening the online survey, and had the option to complete the survey in one or multiple sittings. The study protocol was approved by the Wittenberg University Institutional Review Board. All data were collected electronically via the PatientsCount.org website between April and June 2016.
Measures
Healthy Days Core Module [CDC HRQOL-14; 16]. Composed of three sections, this 14 question self-report questionnaire ascertains health-related quality of life based on number of days affected in the past month. The CDC HRQOL-4 asks questions about general, physical, and mental health, as well as number of days with poor physical or mental health. The Activity Limitations Module assesses limitations due to impairment, type of health problem, duration of limitation, and need for assistance with personal care or routine needs. The Healthy Days Symptoms Module asks how many days pain made it difficult to complete usual activities, and how many days you felt sad or blue, worried or anxious, lacking in sleep or rest, and healthy and energetic. An additional item assessing days of “brain fog” (i.e., difficulties with memory, concentration and word-finding) was added, because this is known to be a common and debilitating symptom for many POTS patients.
West Haven-Yale Multidimensional Pain Inventory, Part I [WHYMPI; 17]. This 20 question self-report measure is scored on a 7-point scale and assesses perceived pain intensity and its impact on quality of life. The Pain Severity Score uses questions like “Rate the level of your pain at the present moment,” and “How much suffering do you experience because of your pain?” The Pain Life-Control Score asks “During the past week, how much control do you feel that you have had over your life?” and “During the past week, how much do you feel that you’ve been able to deal with your problems?” The Pain Interference Score includes “In general, how much does your pain problem interfere with your day to day activities?” and “How much has your pain changed the amount of satisfaction or enjoyment you get from participating in social and recreational activities?”
Pittsburgh Sleep Quality Index [PSQI; 18]. This nine-question self-report measure assesses sleep quality and dysfunction over the past month. It separates “poor” from “good” sleep quality by measuring subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction on a 0–3 point scale. The total score ranges from 0 to 21, with scores >5 indicating poor sleep quality.
Fatigue Severity Scale [FSS; 19]. This nine question self-report measure of fatigue severity from the past week is scored on a 7-point scale. The total score ranges from 9 to 63, with higher scores indicating increased fatigue. Scores >36 indicate excessive fatigue. The FSS is an indicator of the impact of fatigue on functional ability in people with POTS [20].
Suicide Behaviors Questionnaire-Revised [SBQ-R; 21]. This four question self-report measure designates high or low suicide risk by assessing lifetime suicidal ideation and/or suicide attempts. The SBQ-R questions are: (1) “Have you ever thought about or attempted to kill yourself?” (score: 1–4a/b), (2) “How often have you thought about killing yourself in the past year?” (score: 1–5), (3) “Have you ever told someone that you were going to commit suicide, or that you might do it?” (score: 1–3a/b), and (4) “How likely is it that you will attempt suicide someday?” (score: 0–6). The SBQ-R total score was used to group participants by suicidal risk. A score ≥7 places participants into the high suicidal risk group, while scores <7 placed participants in the low suicidal risk group.
In questions one and three of the SBQ-R, two-part answers (a and b) were collapsed into a single category for Table 2. In question one, answer 3a “I have had a plan at least once to kill myself but did not try to do it” was combined with 3b “I have had a plan at least once to kill myself and really wanted to die” into “I have had a plan at least once to kill myself.” Further, answer 4a “I have attempted to kill myself, but did not want to die” was combined with 4b “I have attempted to kill myself, and really hoped to die” to be “I have attempted to kill myself.” Similarly, for question three, we combined answers 2a “Yes, at one time, but did not really want to die” with 2b “Yes, at one time, and really wanted to die” to create the answer “Yes, at one time.” We also combined answers 3a “Yes, more than once, but did not want to do it” with 3b “Yes, more than once, and really wanted to do it” into the category “Yes, more than once.”
Statistical analysis
Statistical analyses were conducted using R computer software. Differences between groups were analyzed using independent-samples t-tests and Chi square tests of independence. Statistical significance was considered at p < 0.05.
Results
CDC health related quality of life-14
POTS patients had more signs of physical illness than controls. People with POTS (\(\bar{x}\) = 19.59, SD = 8.81) have significantly more days of poor physical health in the past 30 days than controls (Fig. 1; \(\bar{x}\) = 5.29, SD = 7.58; p < 0.001). POTS patients had significantly fewer days with good energy (\(\bar{x}\) = 2.26, SD = 4.07) than controls (\(\bar{x}\) = 12.34, SD = 9.57; p < 0.001), and significantly more days with activity limitations (\(\bar{x}\) = 17.48, SD = 10.06) than controls (\(\bar{x}\) = 3.88, SD = 7.03; p < 0.001). People with POTS reported more days without enough sleep or rest (\(\bar{x}\) = 22.37, SD 9.29) than controls (\(\bar{x}\) = 11.88, SD = 10.20; p < 0.001). Those with POTS reported significantly more days with pain (\(\bar{x}\) = 15.52, SD = 10.95) than controls (\(\bar{x}\) = 3.24, SD = 6.71; p < 0.001) and exhibited significantly more days with brain fog (\(\bar{x}\) = 19.34, SD = 9.97) than controls (\(\bar{x}\) = 5.19, SD = 8.99; p < 0.001).
A significantly higher proportion of people with POTS (35.4%) rated their health as poor compared with 2.2% of controls (Table 1; p < 0.001) while 97.1% reported that their activities were limited by illness, a significantly higher proportion than the 31.7% in the control group (p < 0.001). Significantly more people with POTS (76.1%) reported needing help with routine needs like shopping, chores, or conducting business compared with controls (8.6%; p < 0.001), and 30.1% reported needing help with personal care—eating, bathing, dressing, or getting around the house compared with 2.2% of controls (p < 0.001).
People with POTS also had poorer mental health than controls. The POTS group had significantly more days of poor mental health (\(\bar{x}\) = 13.86, SD = 10.14) than controls (\(\bar{x}\) = 7.48, SD = 8.47; p < 0.001). POTS patients reported more days of sadness per month (\(\bar{x}\) = 12.17, SD = 10.04) than controls (\(\bar{x}\) = 6.17, SD = 7.93; p < 0.001). Finally, people with POTS reported worrying more days per month (\(\bar{x}\) = 15.69, SD = 11.19) than controls (\(\bar{x}\) = 9.04, SD = 9.99; p < 0.001).
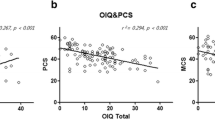
Pain
As detected by the WHYMPI, pain severity was significantly higher for those with POTS (\(\bar{x}\) = 3.35, SD = 1.47) than controls (\(\bar{x}\) = 1.35, SD = 1.47; p < 0.001). POTS patients also reported less control over their lives (\(\bar{x}\) = 2.67, SD = 1.34) than controls (\(\bar{x}\) = 3.93, SD = 1.46; p < 0.001), and that their pain (\(\bar{x}\) = 3.85, SD = 1.68) interfered with their life significantly more than controls (\(\bar{x}\) = 1.34, SD = 1.61; p < 0.001).
Sleep and fatigue
In the POTS group, 98.4% (614/624) reported poor sleep quality on the PSQI compared with 74.8% (104/139) of the controls (Table 1; p < 0.001). Sleep quality was significantly worse for those with POTS (\(\bar{x}\) = 13.34, SD = 4.08) than controls (\(\bar{x}\) = 7.54, SD = 4.02; p < 0.001). According to the FSS, people with POTS (\(\bar{x}\) = 56.21, SD = 8.66) also suffered significantly more daytime fatigue than controls (\(\bar{x}\) = 31.22, SD = 13.64; p < 0.001).
Suicide risk
Suicide risk was increased in the POTS group. Those with POTS (\(\bar{x}\) = 7.06, SD = 3.69) had a significantly higher risk of suicide compared with controls (Table 1; \(\bar{x}\) = 4.91, SD = 2.28; p < 0.001) using their raw scores on the SBQ-R. Among POTS patients, 47.6% (297/624) were at high risk of suicide—significantly higher than the 17.9% (25/139) of controls (p < 0.001). POTS patients had a mean total score of 7.0, just at the cut-off for being considered at high risk (≥7), and also significantly higher than controls’ mean total score of 4.9 (p < 0.001). Among the POTS group, 23.7% had formed at least one suicide plan which was significantly higher than the 13.8% of controls (p = 0.01). In addition, significantly more POTS patients (37.2%) had threatened to make a suicide attempt (Item 3, responses 2–3) compared to controls (18.7%; p < 0.001). Significantly more POTS patients (15.7%) had attempted to kill themselves in the past compared with controls (2.9%; p < 0.001). When asked about the likelihood of attempting suicide in the future, significantly more POTS patients (7.2%) reported that they were likely to do so, compared to controls (1.4%; p = 0.01; Table 2; Item 4, responses 4–6).
Discussion
We found significant decreases in quality of life for POTS patients including more days of poor health and activity limitations that compromise both routine and personal care. Poor sleep quality was reported, with more days without enough rest and excessive daytime fatigue. Further, those with POTS had more severe pain for a larger proportion of the month. Finally, those in the POTS group had an increased risk for suicidal ideation and behavior compared with controls.
As expected, we found decreased physical health in this large sample of POTS patients. In fact, 97% reported activity limitations based on their health problems. Thirty percent required assistance to eat, bathe, dress, or move around the house. This is concerning because our sample consisted of predominately young women (\(\bar{x}\) = 33.76 years). It was interesting that only 35% of these participants rated themselves as having poor health, but this was 16 times higher than the control group. Perhaps young women are unlikely to rate themselves in the lowest category on a five point scale when people with cancer or other illnesses appear more obviously ill. Benrud-Larson et al. showed that general health, physical functioning, role functioning, vitality, and social functioning were all impaired in people with POTS. Bagai et al. demonstrated a decrease in both physical and mental health in POTS patients, with physical health having a greater impact on quality of life [15]. The quality of life in people with POTS is similar to those with congestive heart failure and chronic obstructive pulmonary disorder [8]. This inability to participate in their own lives increase the likelihood of perceived burdensomeness [22, 23].
Pain is a well-known symptom of POTS [3, 20, 28]. More than half of POTS patients report significant neuropathic pain [1, 6]. People with POTS often experience headaches and abdominal pain as well [2, 6, 29]. Central visceral pain sensitization can increase pain perception and contribute to decreased quality of life [30]. As expected, our POTS group displayed significantly more pain, both in severity and number of days in pain, than did controls. We found that pain interfered with daily tasks and POTS patients felt decreased control over their own lives. The impact of chronic pain on sleep and other aspects of the quality of life of the POTS patient should not be underestimated.
Sleep disturbances, including non-restorative sleep and insomnia, are typical for many with POTS who tend to have poor sleep, high rates of fatigue, and decreased quality of life [3, 24]. In fact, sleep problems can account for half of their diminished quality of life score [15]. Sleep disturbances were also found in this study, with 98.4% of POTS patients reporting poor sleep quality and more days without enough sleep or rest. Poor sleep efficiency is common in POTS patients [4, 24, 25].
Fatigue is another pervasive issue for POTS patients. There is a known overlap between POTS and chronic fatigue syndrome [26, 27]. Fatigue levels are up to threefold greater in POTS than controls [15, 20] and energy levels are significantly lower in POTS patients [8]. Our data confirms increased daytime fatigue in POTS.
To our knowledge, there are no studies currently published on suicide risk in POTS patients. In this study, 47.6% of people diagnosed with POTS fell into the high risk group for suicide. Nearly 40% of those with POTS surveyed either had made a plan to kill themselves or had made an attempt. Further, 37% of the POTS group had threatened suicide at least once and 7.2% reported being likely to kill themselves in the future. While this has not been previously studied in POTS patients, suicide risk is known to be elevated in patients who suffer from chronic pain [31, 32] and insomnia [33, 34] in disorders like chronic fatigue syndrome and fibromyalgia. Many POTS patients suffer from chronic pain [3, 20, 28] and/or sleep disturbances [4, 24, 25] which may therefore be linked to suicidal thoughts and behavior. In addition, the need for assistance to complete daily chores or personal care can lead to feelings of perceived burdensomeness, another risk factor for suicide [22, 23] in this population.
Our study has limitations. Data was taken from online self-report measures, rather than objective physical assessment. Participants reported having physician diagnosed POTS, but some may also have had co-morbid diagnoses that could worsen their symptomology. Regrettably, surveys measuring depression were not used, especially when so many people with POTS qualified for the high risk of suicide group. Unfortunately, we do not know whether this high risk is related to depression, pain, sleep, disturbance, or another cause. We did not control for the wide range of pharmaceutical and non-pharmaceutical treatments that were likely used by participants. Finally, our sample may not be representative of all POTS patients, as many in online support groups have more debilitating symptoms than the general POTS population.
Many people with POTS suffer from sleep disturbance, pain, fatigue, and brain fog which can severely diminish quality of life and lead to suicidal ideation. Assessment of quality of life issues should become a standard tool in evaluating the effectiveness of POTS symptom management [13]. The fact that nearly half of our POTS population is at high risk for suicide should be taken seriously. More work needs to be done on suicide risk in POTS patients to determine the underlying causes of suicidal ideation in this population so that proper treatment regimens can be developed.
References
Thieben MJ, Sandroni P, Sletten DM et al (2007) Postural orthostatic tachycardia syndrome: the Mayo Clinic experience. Mayo Clin Proc 82(3):308–313
Benarroch EE (2012) Postural tachycardia syndrome: a heterogeneous and multifactorial disorder. Mayo Clin Proc 87(12):1214–1225
Ojha A, Chelimsky TC, Chelimsky G (2011) Comorbidities in pediatric patients with postural orthostatic tachycardia syndrome. J Pediatr 158:119–122
Bagai K, Wakwe CI, Malow B et al (2013) Estimation of sleep disturbances using wrist actigraphy in patients with postural tachycardia syndrome. Auton Neurosci Basic Clin 177:260–265
Rowe PC, Barron DF, Calkins H, Maumenee IH, Tong PY, Geraghty MT (1999) Orthostatic intolerance and chronic fatigue syndrome associated with Ehlers–Danlos syndrome. J Pediatr 135(4):494–499
Deb A, Morgenshtern K, Culbertson CJ, Wang LB, Hohler–DePold A (2015) A survey-based analysis of symptoms in patients with postural orthostatic tachycardia syndrome. Baylor Univ Med Cent Proc 28(2):157–159
Freitas J, Azevedo E, Santos R, Rocha-Goncalves F (2015) Autonomic activity and biomarker behavior in supine position and after passive postural stress in different orthostatic intolerance syndromes. Portuguese J Cardiol 34(9):543–549
Benrud-Larson LM, Dewar MS, Sandroni P, Rummans TA, Haythornthwaite JA, Low PA (2002) Quality of life in patients with postural tachycardia syndrome. Mayo Clin Proc 77:531–537
Conner R, Sheikh M, Grubb B (2012) Postural orthostatic tachycardia syndrome (POTS): evaluation and management. Br J Med Pract 5(4):540
Anderson JW, Lambert EA, Sari CI et al (2014) Cognitive function, health-related quality of life, and symptoms of depression and anxiety sensitivity are impaired in patients with the postural orthostatic tachycardia syndrome (POTS). Front Physiol 5:1–9
Bhatia R, Kizibash SJ, Ahrens S et al (2016) Outcomes of adolescent-onset postural orthostatic tachycardia syndrome. J Pediatr 173:149–153
Benrud-Larson LM, Sandroni P, Haythornthwaite JA, Rummans TA, Low PA (2003) Correlates of functional disability in patients with postural tachycardia syndrome: preliminary cross-sectional findings. Health Psychol 22(6):643–648
Moon J, Kim DY, Byun JI et al (2016) Orthostatic intolerance symptoms are associated with depression and diminished quality of life in patients with postural tachycardia syndrome. Health Qual Life Outcomes 14(1):144
Kavi L, Nuttall M, Low DA et al (2016) A profile of patients with postural tachycardia syndrome and their experience of healthcare in the UK. Br J Cardiol 23:33
Bagai K, Song Y, Ling JF et al (2011) Sleep disturbance and diminished quality of life in postural tachycardia syndrome. J Clin Sleep Med 7(2):204–210
Center for Disease Control (2000) Measuring healthy days. Atlanta, CDC
Kerns RD, Turk DC, Rudy TE (1985) The west haven-yale multidimensional pain inventory (WHYMPI). Pain 23(4):345–356
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD (1989) The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 46(10):1121–1123
Miglis MG, Muppidi S, Feakins C, Fong L, Prieto T, Jaradeh S (2016) Sleep disorders in patients with postural tachycardia syndrome. Clin Auton Res 26(1):67–73
Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX (2001) The suicidal behaviors questionnaire-revised (SBQ-R): validation with clinical and nonclinical samples. Assessment 8(4):443–454
Kowal J, Wilson KG, McWilliams LA, Peloquin K, Duong D (2012) Self-perceived burden in chronic pain: relevance, prevalence, and predictors. Pain 153(8):1735–1741
Kanzler KE, Bryan CJ, McGeary DD, Morrow CE (2012) Suicidal ideation and perceived burdensomeness in patients with chronic pain. Pain Pract 12(8):602–609
Xu X, Huang H, Sethi S, Zuzuarregui JRP, Weinberg J, Hohler AD (2016) A survey based study on sleep disturbance in postural tachycardia syndrome. J Neurol Sci 365:199–202
Mallien J, Isenmann S, Mrazek A, Haensch C-A (2014) Sleep disturbances and autonomic dysfunction in patients with postural orthostatic tachycardia syndrome. Front Neurol 5:118–124
Cauwenbergh D, Nijs J, Kos D, Weijnen L, Struyf F, Meeus M (2014) Malfunctioning of the autonomic nervous system in patients with chronic fatigue syndrome: a systematic literature review. Eur J Clin Invest 44(5):516–526
Hoad A, Spickett G, Elliott J, Newton J (2008) Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome. Int J Med 101(12):961–965
Jarjour IT (2013) Postural tachycardia syndrome in children and adolescents. Semin Pediatr Neurol 20(1):18–26
Johnson JN, Mack KJ, Kuntz NL, Brands CK, Porter CJ, Fischer PR (2010) Postural orthostatic tachycardia syndrome: a clinical review. Pediatr Neurol 42(2):77–85
Khurana RK (2014) Visceral sensitization in postural tachycardia syndrome. Clin Auton Res 24(2):71–76
Breivik H, Reme SE, Linton SJ (2014) High risk of depression and suicide attempt among chronic pain patients: always explore catastrophizing and suicide thoughts when evaluating chronic pain patients. Scand J Pain 5(1):1–3
Calata R, Laglaoui Bakhiyi C, Artero S, Ilgen M, Courtet P (2015) The impact of physical pain on suicidal thoughts and behaviors: meta-analyses. J Psychiatr Res 71:16–32
Bernert R, Kim JS, Iwata NG, Perlis ML (2015) Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep 17(3):15–24
Ribeiro JD, Pease JL, Gutierrez PM et al (2012) Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord 136(3):743–750
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Rights and permissions
About this article
Cite this article
Pederson, C.L., Brook, J.B. Health-related quality of life and suicide risk in postural tachycardia syndrome. Clin Auton Res 27, 75–81 (2017). https://doi.org/10.1007/s10286-017-0399-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-017-0399-5