Abstract
Objectives
We tested that slow heart rate recovery (HRR) after exercise testing, indicative of decreased parasympathetic nervous system activity, is associated with the development of type 2 diabetes in 1,813 healthy men.
Methods
Heart rate recovery was calculated as the difference between maximum heart rate during the exercise test and heart rate 1 min after cessation of the exercise test.
Results
During an average of 6.4 years of follow-up, 64 (3.5%) subjects developed type 2 diabetes. The unadjusted relative risk (RR) of developing incident diabetes in the slowest versus the fastest HRR quartile was 3.13 (95% CI, 1.28–7.65). However, the association was no longer significant after adjustment for diabetes risk factors and baseline glucose (RR = 2.28, 95% CI, 0.87–5.95).
Conclusion
Slow HRR is associated with the development of type 2 diabetes, but these relationships were largely explained by baseline fasting glucose in healthy men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impaired autonomic nervous system function may be an underlying factor in the development of type 2 diabetes [1–3]. This temporal association is plausible since the pancreas is heavily innervated by parasympathetic fibers, which stimulate the β-cells to release insulin in response to circulating glucose levels [7]. In the presence of autonomic impairment, glucose levels may continue to rise unchecked, contributing to the development of type 2 diabetes. Whether autonomic impairment contributes to the development of diabetes across ethnic groups is unknown. Insulin secretion capacity is genetically lower in Korean and Japanese individuals than in Caucasians [10]. Slow heart rate recovery (HRR) after exercise testing is an estimate of parasympathetic nervous system dysfunction [5] that has previously been shown to worsen with increasing fasting glucose, insulin levels, fitness and inflammatory markers in healthy populations [6, 8, 9]. Therefore, we tested the hypothesis that slow HRR after exercise testing is associated with development of type 2 diabetes in Korean adults.
Methods
Subjects
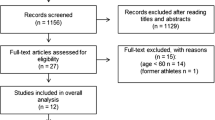
Subjects were recruited from a patient population seen at the Samsung Medical Center in Seoul, Korea for routine health examinations and screening in 1996. We identified 1,813 healthy non-smoking men (aged 46.7 ± 6.9) without previous diagnosis of diabetes, or measured fasting glucose ≥126 mg/dl. Incident diabetes was identified at any follow-up health examination as fasting glucose ≥126 mg/dl or the use of diabetes medication. Participants were followed for a maximum of 9 years. Written informed consent was obtained from all subjects before health screening, and the study was approved by the medical center institutional review board.
Exercise testing and heart rate recovery
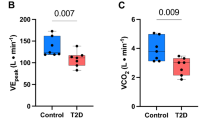
Blood pressure was measured during seated rest using an automated blood pressure monitor (Dinamap PRO 100, Milwaukee, WI, USA). Blood samples were collected in the morning following a 12-h overnight fast and analyzed in the hospital clinical laboratory. Total cholesterol (TC), triglycerides (TG) and high density lipoprotein cholesterol (HDL-C) were analyzed enzymatically using a Hitachi 747 (Tokyo, Japan) analyzer. Low-density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald formula. Fasting glucose levels were determined using the glucose oxidase method (Hitachi-747, Tokyo, Japan). The white blood cell count was determined using a quantitative automated hematology analyzer (Sysmex, Japan). Resting heart rate was measured in the supine position using an electrocardiogram (Hewlett-Packard ECG M 1700A, WI, USA) following at least 5 min of quiet rest. Subjects performed maximal treadmill exercise testing using the Bruce protocol. VO2peak (ml/kg/min) was defined as the highest value recorded during the test. The maximal heart rate using 12-lead ECGs (Quinton Q-4500, Bothell, WA, USA) was defined as the highest value achieved during the test. HRR was calculated as the difference between maximum HR during the test and HR 1 min after cessation of exercise. The recovery protocol consisted of 1 min of light walking (1.2 mph of speed and 0% of grade) immediately after peak exercise testing.
Statistical analysis
Data are expressed as mean ± SD. To test for associations between HRR after exercise and incidence of type 2 diabetes, subjects were divided into quartiles according to HRR based on the data. Comparisons were performed using analysis of variance to determine relationship between HRR quartiles and risk factors. Cox proportional hazards’ regression with adjustment for confounding factors was used to determine the effect of baseline HRR quartiles on the incidence of diabetes. After conducting unadjusted regression, our multivariable modeling strategy was to adjust for age (model 1) and additional potential-confounding factors (BMI, SBP, TC/HDL-C ratio, WBC and VO2peak, model 2). Because we expected a strong association between baseline fasting glucose and the risk of developing diabetes, we additionally adjusted for models 1, 2 plus baseline glucose in model 3. Statistical significance was set at P < 0.05. All tests for statistical significance were two sided. Analyses were conducted using the SPSS 12.0 (SPSS, Chicago, IL, USA).
Results
During an average of 6.4 years of follow-up (range 2–9 years), 64 (3.5%) subjects developed type 2 diabetes. Participants with the fastest baseline HRR (quartile 4) were on average younger, and had lower DBP, TC, TG, TC/HDL-C ratio, glucose, WBC and higher HDL levels than participants in the slowest quartile of HRR (P < 0.05, all of them) (Table 1).
Table 2 demonstrates that the relative risks (RRs) of developing type 2 diabetes were inversely associated with quartile of HRR. The unadjusted and adjusted (model 2) RR of developing incident diabetes in the slowest as compared with the fastest HRR quartile were 3.13 (95% CI, 1.28–7.65) and 2.56 (95% CI, 1.04–6.30), respectively (Table 2).
While a trend toward elevated risk was present in the final model, the association attenuated to non-significance after complete adjustment for baseline glucose levels [RR = 2.28 (95% CI, 0.87–5.95)].
Discussion
We observed that slow HRR is associated with the development of type 2 diabetes in healthy Korean men. However, the association was explained by known risk factors for type 2 diabetes, and in particular, by fasting glucose levels measured concurrently with HRR.
Generally, insulin deficiency rather than insulin resistance has been suggested as the major pathogenic mechanism for the development of type 2 diabetes in most Koreans [10]. Previous research suggests that autonomic dysfunction is more strongly associated with plasma insulin levels than with fasting glucose levels [8]. Parasympathetic fibers stimulate the β-cells to release insulin in response to circulating glucose levels, whereas sympathetic activation inhibits insulin secretion from the β-cells, resulting in impaired transport of blood glucose to the muscle cells. In response to declining insulin secretion and decreased liver and muscle metabolism, blood glucose may gradually increase to result in the development of frank diabetes. Therefore, we hypothesized that autonomic impairment would be an underlying causal factor in the development of type 2 diabetes in Korean adults without diabetes. To our knowledge, only a few prospective studies have been conducted on the relationship between autonomic nervous system dysfunction and the incidence of type 2 diabetes [1–3]. Carnethon et al. [1] reported that among participants with poor fitness, the risk of developing diabetes was 3.4-fold greater when 2 min HRR was <42 versus >42 bpm. In both the Atherosclerosis Risk in Communities cohort [2] and the Diabetes Prevention Program trial [3], autonomic nervous system dysfunction, estimated by high resting heart rate and low heart rate variability, was modestly associated with the development of diabetes in healthy adults.
Although slow HRR has previously been shown to worsen with increasing fasting glucose and insulin levels, in the present study slow HRR was not an independent predictor of incidence of type 2 diabetes in healthy Korean men once concurrently measured glucose was taken into account. Prior prospective studies did not take baseline fasting glucose into account. Additional differences between our study and prior research include different methods of estimating autonomic nervous system function, our sample of Korean men, and the small number of incident cases of type 2 diabetes. While previous studies have defined autonomic dysfunction using slow HRR at 2 min post recovery combined with poor fitness and higher resting heart rate, we defined autonomic dysfunction as slow HRR at 1 min post exercise. It has been suggested that HRR at 1 min post exercise is more reflective of parasympathetic autonomic nervous system function, while HRR at 2 min reflects activity of both branches of the autonomic nervous system [4].
Previous studies have observed this association between autonomic impairment and incident diabetes in western populations. Therefore, whether autonomic impairment contributes to the development of diabetes in different ethnic groups is still unknown. In our sample of healthy Korean men, a trend remained for an inverse association between HRR and incidence of type 2 diabetes. Thus, our data do not completely rule out the possibility of an association between HRR and incidence of type 2 diabetes. The lack of statistical power in our data is attributed to a relatively small number of men who developed diabetes (n = 64). Longer follow-up with greater accrual of events may have yielded a significant finding. Further studies are needed to clarify the association between these relationships.
This study has several limitations. We did not control for diet status, which may potentially confound the relationship between HRR and incidence of type 2 diabetes. We defined incidence of type 2 diabetes as fasting glucose ≥126 mg/dl or the use of diabetes medication. We did not administer an oral glucose tolerance test and so may not have captured all cases of incident diabetes. Finally, we did not assess reproducibility of HRR in this population.
In summary, these results suggest that slow HRR, an estimate of autonomic nervous system dysfunction, is associated with development of type 2 diabetes, but these relationships were attributable to confounding factors. Although a relationship between autonomic function and development of type 2 diabetes may exist in non-Asian populations, further studies are needed to clarify this association in racially diverse populations.
References
Carnethon MR, Golden SH, Folsom AR, Haskell W, Liao D (2003) Prospective investigation of autonomic nervous system function and the development of type 2 diabetes: the Atherosclerosis risk in communities study, 1987–1998. Circulation 107:2190–2195
Carnethon MR, Prineas RJ, Temprosa M, Zhang ZM, Uwaifo G, Molitch ME, Diabetes Prevention Program Research Group (2006) The association among autonomic nervous system function, incident diabetes, and intervention arm in the Diabetes Preventions Program. Diabetes Care 29:914–919
Carnethon MR, Sidney S, Jacobs DR Jr, Liu K (2003) Influence of autonomic nervous system dysfunction on the development of type 2 diabetes: The CARDIA study. Diabetes Care 26:3035–3041
Freeman JV, Dewey FE, Hadley DM, Myers J, Froelicher VF (2006) Autonomic nervous system interaction with the cardiovascular system during exercise. Prog Cardiovasc Dis 48:342–362
Imai K, Sato H, Hori M, Kusuoka H, Ozaki H, Yokoyama H, Takeda H, Inoue M, Kamada T (1994) Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J Am Coll Cardiol 24:1529–1535
Jae SY, Ahn ES, Heffernan KS, Woods JA, Lee MK, Park WH, Fernhall B (2007) Relation of heart rate recovery after exercise to C-reactive protein and white blood cell count. Am J Cardiol 99:707–710
Kiba T (2004) Relationships between the autonomic nervous system and the pancreas including regulation of regeneration and apoptosis: recent developments. Pancreas 29:e51–e58
Lind L, Andren B (2002) Heart rate recovery after exercise is related to the insulin resistance syndrome and heart rate variability in elderly men. Am Heart J 144:666–672
Panzer C, Laure MS, Brieke A, Blackstone E, Hoogwerf B (2002) Association of fasting plasma glucose with heart rate recovery in healthy adults: a population-based study. Diabetes 51:803–807
Shin CS, Lee HK, Koh CS, Kim YI, Shin YS, Yoo KY, Paik HY, Park YS, Yang BG (1997) Risk factors for the development of NIDDM in Yonchon country, Korea. Diabetes Care 20:1842–1846
Conflict of interest statement
None of the authors had any conflicting interests in connection with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jae, S.Y., Carnethon, M.R., Heffernan, K.S. et al. Heart rate recovery after exercise and incidence of type 2 diabetes in men. Clin Auton Res 19, 189–192 (2009). https://doi.org/10.1007/s10286-009-0007-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-009-0007-4