Abstract
Objectives
This study was designed to examine the effect of head-up sleeping as a treatment for vasovagal syncope in otherwise healthy patients. Treatment for syncope is difficult. Pharmacological treatments have potential side effects and, although other non-pharmacological treatments such as salt and fluid loading often help, in some cases they may be ineffective or unsuitable. Head-up sleeping may provide an alternative treatment.
Methods
Twelve patients had a diagnosis of vasovagal syncope based both on the history and on early pre-syncope during a test of head-up tilting and graded lower body suction. They then underwent a period of 3–4 months of sleeping with the head-end of their bed raised by 10°, after which orthostatic tolerance (time to pre-syncope during tilt test) was reassessed.
Results
Eleven patients (92%) showed a significant improvement in orthostatic tolerance (time to pre-syncope increased by 2 minutes or more). Plasma volume was assessed in eight patients and was found to show a significant increase (P < 0.05, Wilcoxon signed-rank test). There was no significant change in either resting or tilted heart rate or blood pressure after head-up sleeping.
Interpretation
Head-up sleeping is a simple, non-pharmacological treatment which is effective in the majority of patients. However, it may not be tolerated by patients or bed-partners long term and whether the effects continue after cessation of treatment remains to be determined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vasovagal syncope is the most frequent cause of transient loss of consciousness [1, 16] and is responsible for 0.9–1.2% of hospital admissions in Europe [7]. Pharmacological interventions have usually been disappointing and often associated with unwanted effects [22]. We have found that in the majority of patients, both symptoms and measured orthostatic tolerance improve following simple advice about not standing still for long periods, increasing water and salt intake, and keeping physically active [8]. Most of the remaining patients respond well to procedures including salt loading [10, 13] and exercise training [18]. However, there remain some who either do not respond to these interventions or for whom salt is contra-indicated, for example due to pre-existing hypertension, and for whom exercise is also not appropriate. Sleeping with the head-end of the bed raised would maintain a continuous low level of orthostatic stress and may be of value to some of the syncopal patients. The principal aim of this study, therefore, was to test the effects of head-up sleeping in patients with syncopal attacks and who had an abnormally low measured orthostatic tolerance, both in terms of any symptomatic changes and by use of an objective and reproducible test of orthostatic tolerance [11].
In our previous studies of the effects of salt loading and exercise training we observed that any improvement in orthostatic tolerance, however it was produced, was associated with an increase in plasma and blood volumes [13, 20]. A further aim of this study, therefore, was to examine whether head-up sleeping increased plasma volume and further to examine the hypothesis that orthostatic tolerance is related to plasma volume.
Methods
Subjects
Patients were recruited to the study if they had failed to show improvement after simple advice and salt loading. Salt was discontinued at least 2 weeks before the baseline study. All patients had poor orthostatic tolerance as assessed by the Leeds test of combined head-up tilt and lower body negative pressure (see below). On this basis we recruited 12 patients (6 males) aged 16–60 years (mean ± SE, 42 ± 5 years). None had any significant cardiovascular or neurological disease or was taking any medication with a cardiovascular action. All subjects gave informed consent. The study was approved by the Research Ethics Committee of the Leeds Teaching Hospitals and was performed in accordance to the Declaration of Helsinki (1989) of the World Medical Association.
Orthostatic stress test
The orthostatic stress test consisted of the combination of head-up tilt and graded lower body negative pressure and has been described previously [11]. Subjects lay supine on the tilt table and a chamber was fitted to the table to cover the region of the body below the iliac crests. An appropriately shaped and sized plate completed the air-tight seal to the table. Patients were fitted with ECG leads and an auto-inflating sphygmomanometer (Hewlett Packard 78325C; Boebringen, Germany). A photoplethysmograph device (Finapres, Ohmeda, Wis) was fitted to the middle finger of the right hand for continuous blood pressure monitoring. The test protocol was as follows: patients rested supine for 20 minutes before being tilted by 60° for a further 20 minutes. Then, whilst still tilted, lower body negative pressure was applied until pre-syncope. Suction was at −20 mmHg for up to 10 minutes then, if no pre-syncope, at −40 mmHg. The test was discontinued when the subject developed signs and symptoms of impending syncope such as dizziness or nausea, and had a systolic pressure below 80 mmHg. The lower body negative pressure was stopped and the patient returned to the supine position. Orthostatic tolerance was taken as the time in minutes to pre-syncope from the start of head-up tilt. We have previously shown that the reproducibility of the test both in healthy volunteers and patients with syncope is ± 2 minutes (2 SD of differences of repeated studies [11, 13].
Plasma volume
Plasma volume was assessed in eight subjects using the Evans blue dye dilution method which has also been described previously [12]. Patients rested for at least 30 minutes to allow for stabilization of plasma volume and brachial venous hematocrit. The arm to be catheterized was supported at heart level, and room temperature was controlled at 20–22°C. A sterile catheter (20 G Venflon) to which a sterile plastic tap was attached was inserted into an antecubital vein. After 5 minutes, 18 ml of blood was withdrawn via the catheter to provide plasma for construction of a standard Evans blue calibration curve. Approximately 3 ml of Evans Blue dye (The New World Trading Corporation, Debarry, FL, USA) was injected through the catheter and thoroughly washed into the vein using sterile saline. Care was taken to ensure that all traces of dye were cleared from the tap. The precise amount injected was determined by weighing the syringe before and after injection. Blood samples (3 ml) were taken 10, 15, 20 and 25 minutes after injection. Care was taken to minimize the risk of hemolysis by withdrawing blood samples very slowly. Each blood sample was introduced into a sterile tube containing heparinized glass beads to prevent clotting, and then centrifuged and the plasma extracted. The tap was flushed with saline after each sample.
Standard curves were constructed for each study, using the subject’s own plasma and Evans blue dye from the same ampoule as used in the study, to make concentrations of 2.5, 5 and 10 µg/l. The absorbencies of these samples were determined and the absorbency of the subject’s plasma subtracted. These absorbencies were plotted against the known concentrations to give the standard curve. Using the standard curve, the concentration of the samples taken after dye injection were calculated and were plotted as loge concentration against time following injection to construct a decay curve. Reverse-extrapolated linear regression analysis was then used to calculate the theoretical concentration of dye at time zero (the point of injection). This concentration was used to determine the dilution of the known quantity of injected Evans blue, and hence plasma volume. Previous work has shown the repeatability of this technique to be ±45 ml (95% tolerance with 95% confidence; [12]).
Procedure
After the baseline tests, an engineer went to the patient’s home and modified their bed so that the head-end was raised at an angle of 10°. Patients were contacted after a period of 3 months to arrange restudy. The time between the two studies ranged between 3 and 4 months. Patients did not receive any other treatment during this period.
Statistical analysis
All values are reported as means ± SE. Data were tested for normality and either parametric or non-parametric testing was performed as appropriate. Values before and after treatment were assessed using a paired Student t test for parametric data, or for non-parametric data the Wilcoxon signed-rank test. Correlations between variables were examined using the Spearman rank correlation coefficient. Values were considered significantly different if P < 0.05.
Results
Symptomatic improvement
Prior to the trial all patients were experiencing frequent attacks of light headedness. They had all experienced at least one episode of syncope in the month preceding recruitment. After head-up sleeping all but one reported improvement in their symptoms. Some still experienced episodes of light headedness but none had actually fainted. The patient who did not report an improvement in symptoms also had no improvement in his measured orthostatic tolerance.
Orthostatic tolerance
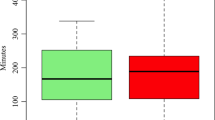
Orthostatic tolerance increased in all but one subject. Orthostatic tolerance changed by −1 to +17 minutes with a mean increase of 7.8 ± 1.6 minutes. A significant improvement was considered to be 2 minutes or more, based on the reproducibility of the test [11]. On this basis, 11 subjects were considered to have a significant improvement. All patients showing an objective improvement claimed also to have improved symptomatically. The subject who showed the decrease in orthostatic tolerance did not improve symptomatically. On the basis of previously published data [15], the mean orthostatic tolerance after head-up sleeping increased to within the normal range in five subjects compared with clearly poor tolerance in all subjects before treatment. Group data of orthostatic tolerance before and after treatment are shown in Figure 1. Prior to treatment six patients became pre-syncopal before the end of the tilt alone phase and none tolerated the test into the final phase of lower body negative pressure. After treatment only four patients became pre-syncopal during the tilt alone phase and five patients tolerated the test to the final phase of lower body negative pressure.
Effect of head-up sleeping on orthostatic tolerance. Time 0–20 minutes was head-up tilt alone, 20–30 minutes tilt and lower body suction at −20 mmHg, and time 30–40 minutes tilt and lower body suction at −40 mmHg. Orthostatic tolerance expressed as time to pre-syncope (minutes) was significantly increased after head-up sleeping. Before head-up sleeping all subjects became pre-syncopal by the end of the first level of lower body suction (30 minutes) whereas after head-up sleep five were able to tolerate this; i.e., had normal results
Heart rate and blood pressure
Figure 2 shows the resting supine values of heart rate and systolic and diastolic blood pressures before and after head-up sleeping. There were no significant changes. Resting supine heart rates before and after head-up sleeping were 66.6 ± 1.7 and 66.1 ± 2.1 beats/minute (P > 0.05). Resting mean arterial pressures before and after head-up-sleeping were 85.3 ± 3.2 and 85.9 ± 2.4 mmHg (P > 0.05).
The values of heart rate and blood pressure during the tilt test, before and after the period of head-up sleep, are shown in Figure 3. Head-up tilt resulted in increases in heart rate, systolic and diastolic pressures in both conditions. Head-up sleep had no significant effect on heart rate. Systolic and mean arterial pressures were higher after head-up sleep, but only significantly at minute 22 (P < 0.05). Diastolic pressure was significantly higher after head-up sleep at minute 2 only.
Values of heart rate, systolic, diastolic and mean pressure during orthostatic stress testing at baseline and after head-up sleep (HUS). HUS had no effect on resting variables. Diastolic pressure was higher a minute 2 post tilt only and systolic and mean pressures were only different at minute 22 post tilt (*P > 0.05)
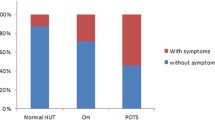
Plasma volume
Individual and mean changes in plasma volume are shown in Figure 4. Of the eight patients tested, plasma volume increased after head-up sleeping in six. The average values before and after were 3.18 l/kg (range 2.21–4.39), and 3.40 l/kg (2.44–4.66). Overall the change was statistically significant (P < 0.05, Wilcoxon signed-rank test). All patients who showed improvement in their orthostatic tolerance by more than 2 minutes also showed increases in plasma volume (+0.34 ± 0.14 l).
Effect of head-up sleeping on plasma volume. Overall there was a significant increase in plasma volume (*P < 0.05, Wilcoxon signed-rank test). The six patients in whom plasma volume increased had increases in time to pre-syncope of more than 2 minutes; the two in whom plasma volume failed to increase had changes in time to pre-syncope of +2 and −1 minute
Discussion
In this study we examined the effects of sleeping with the head-end of the bed raised by 10°. In all but one of our patients, orthostatic tolerance, determined by repeat tilt testing, was improved. If the limit of normal orthostatic tolerance was taken as 30 minutes, that is 20 minutes of head-up tilt alone and 10 minutes of combined head-up tilt and lower body negative pressure at −20 mmHg, then prior to treatment all 12 patients had low-orthostatic tolerance. However, after treatment only seven of them would be considered to have low-orthostatic tolerance. Of the patients who improved there was a significant negative correlation between baseline orthostatic tolerance and improvement. That is, those with the worst orthostatic tolerance to begin with improved the most. We assessed whether there was a symptomatic improvement following head-up sleep and most patients claimed to be better. We have to interpret this with some caution, however, as incidence of syncope tends to be very irregular and, in some patients, infrequent. For this reason, therefore, we place more reliance on our objective assessment.
Plasma volume was measured in eight of the patients and, in all the patients in whom orthostatic tolerance increased by more than 2 minutes (the level of reproducibility of the test [11, 13]), plasma volume always increased.
The reason that some individuals show early syncope during orthostatic stress is still unclear and can probably be attributed to various causes. Ultimately, the reason for loss of consciousness is inadequate cerebral perfusion and the reasons for this are likely to differ in different patients. In most asymptomatic subjects, the loss of effective plasma volume due to venous pooling and transudation through dependent capillaries does not even result in a decrease in arterial blood pressure due to effective reflex compensation [14, 21]. Even if blood pressure does fall the cerebral circulation is protected by efficient autoregulation [17]. In fainting subjects the stress may be greater or the compensation less effective than in non-fainters. For example the reflex vasoconstriction has been shown to be less in subjects with poor tolerance to orthostatic stress [2]. Some asymptomatic subjects also have small reflex responses but they, unlike the fainters, compensate by increased postural movements and this would minimize venous pooling [5, 6]. Another factor which may predispose to syncope is that the autoregulation of the cerebral blood flow has been shown not to be as effective in fainters [20].
Since the main stress of orthostasis is the reduction in effective circulatory volume, it might be expected that individuals with relatively large plasma volumes would have good orthostatic tolerances. Also if we are able to increase plasma volume this should also increase orthostatic tolerance. Work from our laboratory in recent years has largely upheld this hypothesis. There was found to be a good correlation between orthostatic tolerance and normalized plasma volume [20]. Procedures which were effective in increasing plasma volume usually also increased orthostatic tolerance. These included salt loading [10, 13, 19] and exercise training [20]. We speculated that spending the night in a head-up position might also increase plasma volume. The mechanisms for this are unknown but might include a reduction of central blood volume during the night leading to compensatory mechanisms which increase actual plasma volume. In the event we found that plasma volume did increase in six of the eight patients in whom it was measured and that orthostatic tolerance also increased in those six patients. In the two patients who failed to increase plasma volume, orthostatic tolerance changed by only +2 and −1 minute.
One limitation of this study is that it was not possible to be certain that all our patients did actually sleep head-up all the time, so failure to respond may have been due to failure to comply. This would imply that the true effect of head-up sleeping could be even greater than we actually observed. Another major limitation is that it was not possible to have a “blinded” control group and so a “placebo” effect cannot be excluded. This criticism cannot entirely be refuted as all subjects were clearly aware that a procedure designed to be of help was being undertaken. We do not, however, believe that it was simply a random change. This belief is based on our earlier study of the repeatability of the test in normal subjects [11] and the study of the effects of salt, where those on placebo who did not change plasma volume did not change orthostatic tolerance [13]. Another limitation is the small number of subjects in which plasma volume was assessed. This was in part due to the limited availability of Evan’s Blue Dye. However, even with this small number of subjects a statistically significant difference was found.
One particularly interesting observation was that, although numbers are small, there was an association between the change in orthostatic tolerance and the change in plasma volume. Figure 5 shows the relation between change in orthostatic tolerance and change in plasma volume induced by three different methods: salt loading, exercise training and head-up sleeping. All interventions usually resulted in increases in both and it seems reasonable to speculate that the increased plasma volume is implicated in causing the improved tolerance. However, the effectiveness of the increase in plasma volume in increasing orthostatic tolerance may not be identical for all interventions. Salt loading, in patients in whom it was effective, seems to result in larger changes in orthostatic tolerance for a given change in plasma volume and this may be explained by it also causing an enhancement of the reflex vascular responses [4, 9]. Assessment of salt excretion may therefore be useful to help dissect the contribution of any change in salt intake from any other intervention on change in plasma volume.
When episodes of syncope occur frequently it can be a severely debilitating condition impacting employment and social opportunities. Medical therapy for syncope is generally unsatisfactory with many medications having the potential side effect of raising supine blood pressure [22]. Therefore a non-pharmacological approach would be advantageous. Simple advice of increasing salt and water intake as well as physical counter maneuvres is often effective [8]. However, there are still a few patients for whom this is inappropriate or unsuccessful. We would suggest that head-up sleeping is a relatively simple and safe intervention to use in such patients. Most of our patients soon became accustomed to sleeping head-up, although we only used an angle of 10° after a preliminary study indicated that greater angles were not acceptable and we felt that compliance might be a problem. Furthermore, we only recruited patients who we considered to be well motivated. We also do not know yet whether the effects of head-up sleeping persist beyond the 3- to 4-month period studied or whether it is necessary to continue indefinitely with head-up sleeping.
Conclusion
Head-up sleeping appeared to be an effective treatment in over 80% of the patients treated and fully normalized orthostatic tolerance in over 40%. It is a simple, non-pharmacological treatment. However, it may not be tolerated by all patients and whether the effects persist in the long term or continue after cessation of treatment remains to be determined.
References
Brignole M, Alboni P, Benditt D et al (2001) Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 22:1256–1306
Brown CM, Hainsworth R (2000) Forearm vascular responses during orthostatic stress in control subjects and patients with posturally related syncope. Clin Auton Res 10(2):57–61
Claydon VE, Hainsworth R (2003) Cerebral autoregulation during orthostatic stress in healthy controls and in patients with posturally related syncope. Clin Auton Res 13(5):321–329
Claydon VE, Hainsworth R (2004) Salt supplementation improves orthostatic cerebral and peripheral vascular control in patients with syncope. Hypertension 43(4):809–813
Claydon VE, Hainsworth R (2005) Increased postural sway in control subjects with poor orthostatic tolerance. J Am Coll Cardiol 46(7):1309–1313
Claydon VE, Hainsworth R (2006) Postural sway in patients with syncope and poor orthostatic tolerance. Heart 92(11):1688–1689
Colman N, Nahm K, Ganzeboom KS et al (2004) Epidemiology of reflex syncope. Clin Auton Res 14:I9–I17
Cooper VL, Fuentealba P, Hainsworth R, McIntosh SJ (2006) Is simple advice all that is needed to manage patients with syncope? Clin Auton Res 16:341 (abstr)
Cooper VL, Hainsworth R (2002) Effects of head-up tilting on baroreceptor control in subjects with different tolerances to orthostatic stress. Clin Sci (Lond) 103(3):221–226
Cooper VL, Hainsworth R (2002) Effects of dietary salt on orthostatic tolerance, blood pressure and baroreceptor sensitivity in patients with syncope. Clin Auton Res 12(4):236–241
El-Bedawi KM, Hainsworth R (1994) Combined head-up tilt and lower body suction: a test of orthostatic tolerance. Clin Auton Res 4(1–2):41–47
El-Sayed H, Goodall SR, Hainsworth R (1995) Re-evaluation of Evans blue dye dilution method of plasma volume measurement. Clin Lab Haematol 17(2):189–194
El-Sayed H, Hainsworth R (1996) Salt supplement increases plasma volume and orthostatic tolerance in patients with unexplained syncope. Heart 75(2):134–140
Gilbert CA, Stevens PM (1996) Forearm vascular responses to lower body negative pressure and orthostasis. J App Physiol 21:1265–1272
Hainsworth R, El-Bedawi KM (2004) Orthostatic tolerance in patients with unexplained syncope. Clin Auton Res 4(5):239–244
Kapoor WN (2000) Syncope. N Engl J Med 343:1826–1856
Lassen NA (1959) Cerebral blood flow and oxygen consumption in man. Physiol Rev 39:183–238
Mtinangi BL, Hainsworth R (1998) Increased orthostatic tolerance following moderate exercise training in patients with unexplained syncope. Heart 80(6):596–600
Mtinangi BL, Hainsworth R (1998) Early effects of oral salt on plasma volume, orthostatic tolerance, and baroreceptor sensitivity in patients with syncope. Clin Auton Res (4):231–235
Mtinangi BL, Hainsworth R (1999) Effects of moderate exercise training on plasma volume, baroreceptor sensitivity and orthostatic tolerance in healthy subjects. Exp Physiol 84(1):121–130
Olsen H, Lanne T (1998) Reduced venous compliance in lower limbs of ageing humans and its importance for capacitance function. Am J Physiol 275:H878–H886
Pathak A, Raoul V, Montastruc JL, Senard JM (2005) Adverse drug reactions related to drugs used in orthostatic hypotension: a prospective and systematic pharmacovigilance study in France. Eur J Clin Pharmacol 61(5–6):471–474
Conflict of interest statement
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooper, V.L., Hainsworth, R. Head-up sleeping improves orthostatic tolerance in patients with syncope. Clin Auton Res 18, 318–324 (2008). https://doi.org/10.1007/s10286-008-0494-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-008-0494-8