Abstract
Mesenchymal stem cells derived from human teeth and bone marrow have been characterized by many research groups, but demonstrate inconsistent cellular phenotypes or functions, partly because of differences in culture methodology. Therefore, our aims were to resolve these inconsistencies and discuss the potential uses of these cells in research/clinical applications. We isolated and characterized dental stem cells (DSCs) from the dental pulp, periodontal ligament, apical papilla (APSCs) and dental follicle (DFSCs) of mature and immature teeth, along with bone marrow-derived stem cells (BMSCs) from the iliac crest. We compared the clonogenic and proliferative potentials of these cells in terms of colony-forming efficiency, proliferation potential, population doubling time and cell cycle. All DSCs, particularly APSCs and DFSCs, possessed greater proliferative potential than BMSCs. All stem cells expressed typical mesenchymal and embryonic markers, and developed alizarin red-positive mineralization nodules and Oil red O-positive lipid droplets when cultured in osteogenic and adipogenic media, respectively. Immunocytochemistry revealed that all stem cells developed neuronal markers when cultured in a control medium without neural inductive supplements. After 7 days of neurogenic culture, the differentiated cells showed a transition from fibroblast-like to neuron-like cell bodies with long processes, suggesting that the stem cells differentiated into mature neurons. Karyotyping confirmed that the stem cells maintained a normal karyotype and were chromosomally stable. Our results provide new insights into the physiological properties of stem cells with a normal karyotype and indicate that DSCs are appropriate for basic research and clinical applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stem cells are defined as clonogenic cells capable of self-renewal and multilineage differentiation, and have been identified in bone marrow, adipose tissue and dental tissue [1–3]. Mesenchymal stem cells (MSCs) can differentiate into multiple cell types including osteogenic, chondrogenic, adipogenic, myogenic and neurogenic cells, when cultured under the appropriate conditions [4–7]. MSCs were first identified in aspirates of adult bone marrow [8] and have the potential to be used in stem cell transplantation therapies of regenerative medicine.
Dental stem cells (DSCs), which are now considered a type of MSC, have a high proliferative potential and exhibit multipotency, and are thus expected to facilitate cell-based therapy [1, 9, 10]. The first human DSCs to be isolated were obtained from dental pulp tissue in the central cavity of the tooth and thus termed dental pulp stem cells (DPSCs) [11]. DPSCs have since been harvested from human exfoliated deciduous teeth [12] and the root apical papilla (APSCs) of immature teeth (originally referred to as stem cells from the apical papilla) [13]. A dental MSC-like population was also isolated from the periodontal ligament (PDLSCs) [14], which connects the surface of the tooth root to the inner wall of the alveolar bone socket. The dental follicle also harbors stem/progenitor cells for the periodontium and is expected to be a new source of DSCs, termed dental follicle precursor cells [15].
Collectively, these DSCs are capable of differentiation into multiple lineages, including osteogenic, adipogenic, neurogenic, chondrogenic and myogenic cells, when grown under defined conditions [6]. Based on these findings, extracted teeth, a waste product of many dental procedures, have been proposed as a valuable source of stem cells to aid tissue regeneration, and the DSCs obtained could be used for the research and development of cell-based therapies to replace dental/periodontal tissue and other organs [16–21].
We previously revealed the potential of expanded cultures of ex vivo heterogeneous periodontal ligament cells, which appeared to contain multipotent stem/progenitor cells, to be used for periodontal regeneration in animal experiments using dogs [22, 23]. We believe that DSCs isolated from extracted teeth could be useful for dental and periodontal regenerative therapies [24–26]. To date, no studies have included a comparative analysis of multiple stem cell types isolated and grown under identical culture conditions. Although MSCs derived from human teeth and bone marrow have been isolated and characterized by many research groups, cellular phenotypes or functions are often inconsistent. We performed the present study to (1) compare the phenotype and function of DSCs and bone marrow-derived stem cells (BMSCs) when cultured in a specific environment, and (2) resolve some of the inconsistencies in the existing descriptions of the phenotype and functions of these stem cells. We believe such research is essential to enable proper use of DSCs in research and to assess their potential clinical applications in regenerative therapy.
Materials and methods
Isolation and Culture of DSC and BMSCs
The present study was approved by the ethics committees of the Nippon Dental University and Japan Red Cross Society. Normal human third molars were collected from individuals (16–28 years old) undergoing tooth extraction. Bone marrow was collected by marrow aspiration from individuals aged 13–22 years. Informed consent was obtained from each individual after full explanation of the nature of the procedure and the intended use of the tissue obtained.
DSCs and BMSCs were isolated and cultured as previously described [8, 11]. The dental pulp and periodontal ligaments were collected from the fully grown third molar. Dental pulp tissue was obtained from the pulp chamber that was revealed by cutting around the cement–enamel junction with a sterilized dental fissure bur. The periodontal ligament was gently separated from the surface of the root with a sterile razor blade. Immature dental tissues, such as the dental follicle and apical papilla, were collected from impacted teeth. Dental follicle tissue attached to the tooth crown of the extracted immature tooth (Fig. 1a) was separated from the crown with a disposable scalpel. The apical papilla, located at the root apex of the immature tooth (Fig. 1b), was also collected with a (different) scalpel. These harvested dental tissues were physically lysed, then digested in a solution containing 3 mg/ml collagenase type I (Sigma, St Louis, MO) and 4 mg/ml dispase (Sanko Pure Chemical Ltd., Tokyo, Japan) for 1 h at 37 °C. Single-cell suspensions were obtained by passing the cells through a 70-μm cell strainer (Falcon, BD Labware, Franklin Lakes, NJ). The resulting single-cell suspensions (1 × 104 cells/dish) were seeded into 100-mm dishes (Nunc, Roskilde, Denmark) and cultured in growth medium, which consisted of Dulbecco’s modified Eagle’s medium/Ham’s nutrient mixture F12 (Gibco BRL, Carlsbad, CA) supplemented with 15 % fetal bovine serum (FBS; Lot No: 027K0361, Sigma), 2 mM glutamine (GlutaMAX I) (Invitrogen, Carlsbad, CA), 100 U/ml penicillin and 100 μg/ml streptomycin (Gibco BRL) at 37 °C/4.7 % CO2. The DSCs derived from the dental pulp, periodontal ligament, apical papilla and dental follicle were designated DPSC, PDLSC, APSC and DFSC, respectively.
Tissue collection, cell culture and self-renewal capability of DSCs and BMSCs. An extracted impacted third molar from a human showing a a dental follicle attached to the tooth crown (arrow) and b the apical papilla of the root apex (arrowheads). c BMSCs grown in primary culture after 3 weeks. d A cell cluster derived from PDLSCs formed a single colony and was stained with 0.1 % toluidine blue after 14 days of culture. The cell morphology of all DSCs is typical of fibroblast-like cells. e Clonogenic efficiency was determined in the four types of DSCs. Approximately 1 × 104 DSCs were seeded in a 100-mm dish and cell clusters that formed a solitary colony were counted at 14 days of culture. Aggregates of more than 50 cells were scored as colonies. CFU-F values were significantly higher for DFSCs and APSCs compared with PDLSCs and DPSCs (*p < 0.05). f Growth curves for DPSCs, PDLSCs, APSCs, DFSCs and BMSCs over 12 days of culture. Initially, 3 × 103 cells were seeded into 24-well plates and cultured. Cells were harvested and counted in triplicate with a hemocytometer every 2 days over a 12-day culture period. All four DSCs exhibited significantly greater growth than BMSCs (**p < 0.01), while there were statistically significant differences between each type of DSC, as follows: DFSC > APSC > PDLSC > DPSC (*p < 0.05). g Flow cytometric data to analyze cells in the G0/G1 phase indicated that the BMSC population contained a higher percentage of cells compared with the DPSC, PDLSC, DFSC and APSC populations and two cancer cell lines, SKN and HSC-2, in the G0/G1 phase (*p < 0.05). h Flow cytometric data indicated that the BMSC population contained a lower proportion of cells compared with the DPSC, PDLSC, DFSC and APSC populations and the two cancer cell lines, SKN and HSC-2, in the G2/M phase (*p < 0.05)
To isolate BMSCs, the aspirated bone marrow was seeded and cultured in growth media. Non-adherent cells were removed by rinsing with fresh growth media 48 h after initial plating, while adherent cells attached to the culture dish were processed for primary culture (Fig. 1c). Throughout the expansion of the above primary stem cells, growth media were refreshed every 2 days, and the cells were passaged at a density of 5 × 104 cells/cm2 in 60-mm culture dishes. Once confluent, cells were detached using 0.25 % trypsin/0.02 % ethylenediaminetetraacetic acid (EDTA). All primary stem cells used in this study were examined at passage 3, except in colony-forming unit fibroblast (CFU-Fs) assays (which were used at passage 0).
To further compare the cellular proliferative potential, two cancer cell lines were prepared for cell cycle analysis using flow cytometry: a human uterine cervical leiomyosarcoma cell line, named SKN [27], and a line derived from human oral squamous cell carcinoma, named HSC-2 [28].
Determination of CFU-Fs
Primary dental cells (passage 0) were used for colony-forming assays. Approximately 1 × 104 cells were seeded in a 100-mm culture dish and cultured for 14 days. Cells were then fixed with 4 % paraformaldehyde (PFA) and stained with 0.1 % toluidine blue. Colonies (designated as an aggregate of 50 or more cells) were counted under a microscope (Fig. 1d), and the number of colonies was calculated and compared among the four types of DSCs. CFU-F was not determined for BMSCs because of the differences in cell isolation and primary culture methods used.
Cell proliferation assay
Cell growth potential was determined by plating 3 × 103 cells/well in 24-well culture plates and culturing in growth media. The cultured cells were collected by trypsin/EDTA treatment and counted in triplicate with a hemocytometer every 48 h for 12 days. We calculated the population doubling time (PDT) of all stem cells examined, as previously described [29] using the formula: PDT = (t − t 0)log2/log(N − N 0), where t is time (hours), N the number of harvested cells and N 0 is the number of cells in the inoculum.
Flow cytometry for determining cell cycle status
Cell cycle status was analyzed using flow cytometry. Cells were plated at 9 × 104 cells/100-mm dish plates and cultured at 37 °C/4.7 % CO2. After 8 days, cells were collected by trypsin/EDTA treatment, washed with phosphate-buffered saline (PBS), and centrifuged. The cell pellet was resuspended in 1.5 ml of cold ethanol, vortexed to provide a homogenous cell suspension and fixed for 2 h at −20 °C. Fixed cells were washed with PBS and stained with propidium iodide (Guava Technologies, Hayward, CA) for 30 min at 4 °C. Cell cycle analysis was carried out using a Guava™ flow cytometer and Guava™ cell cycle software version 5.3 (Guava Technologies, Hayward, CA).
Flow cytometry for specific cell markers
To examine the specific cell markers of the stem cells, a flow cytometry analysis was performed. Fluorescein isothiocyanate-conjugated mouse monoclonal antibodies against CD14, CD90 and CD105 (Abcam, Cambridge, MA) and CD34 and CD44 (Becton, Dickinson, San Jose, CA) were used. Phycoerythrin-conjugated mouse immunoglobulin G1 (Becton, Dickinson) was used as a negative control. Data acquisition and analyses were performed with Guava™ Express Plus (version 5.3) software (Guava Technologies).
Reverse-transcription polymerase chain reaction (RT-PCR)
Total RNA was isolated from cultured cells using an RNeasy Mini kit (Qiagen, Hilden, Germany). Using 1 μg of mRNA, cDNA was synthesized with a High-Capacity cDNA Reverse Transcription kit (Applied Biosystems, Carlsbad, CA) and amplification was performed using a PCR Supermix Platinum kit (Invitrogen). The PCR conditions were as follows: denaturation for 2 min at 94 °C, 30 s annealing at 55 °C, 30 s of extension at 72 °C, and 35 cycles of amplification in a Veriti™ 96-well Thermal Cycler (Applied Biosystems). The PCR products were separated by electrophoresis on a 1.8 % (w/v) agarose gel and stained with ethidium bromide. The specific primer sequences for each gene are shown in Table 1. Glyceraldehyde-3-phosphate dehydrogenase was used as the internal control.
Multilineage cell differentiation
Stem cells were subjected to differentiation using osteogenic, adipogenic and neurogenic induction conditions. To induce osteogenic or adipogenic differentiation, cells were seeded at 1 × 105 cells/well in six-well plates and maintained in growth media until confluent. For osteogenic induction, cells were cultured in α-modified minimal essential medium (α-MEM; Wako Pure Chemical, Osaka, Japan) containing 10 % FBS, 10 nM dexamethasone (Sigma), 10 mM β-glycerophosphate (Wako Pure Chemical) and 100 μM l-ascorbate-2-phosphate (Wako Pure Chemical) for 3 weeks. To visualize the mineralized deposits, the cultures were fixed in 4 % PFA for 10 min and stained with 1 % alizarin red S (Merck, Darmstadt, Germany) for 30 min at room temperature followed by microscopic examination. For adipogenic differentiation, the cells were cultured in α-MEM containing 10 % FBS, 0.5 mM isobutylmethylxanthine (Wako Pure Chemical), 0.5 μM hydrocortisone (Sigma) and 60 μM indomethacin (Sigma) for 3 weeks. Lipid-laden fat cells were then fixed with 4 % PFA and stained with Oil red-O (Sigma) for 30 min at room temperature followed by microscopic examination. Control cultures were maintained in α-MEM supplemented with 10 % FBS lacking the osteogenic or adipogenic supplements.
To induce neurogenic differentiation, cells were seeded at 3 × 103 cells/well in a Lab-Tek 4-well chamber slide (Nunc) and cultured in Neurobasal A medium (Invitrogen) containing B27 supplement (1× concentration), 20 ng/ml epidermal growth factor (EGF) (Pepro Tech, Rocky Hill, NJ, USA), 40 ng/ml basic fibroblast growth factor (b-FGF) (Wako Pure Chemical), 0.5 μM retinoic acid (Sigma, St Louis, MO) and 1× insulin–transferrin–sodium-selenite (ITS) supplement (Roche Diagnostics, Mannheim, Germany) for 7 days. Control samples were cultured in FBS-free α-MEM. Differentiation and control media were each changed after 2–3 days.
Immunocytochemistry
Cells were fixed with 100 % methanol (Wako Pure Chemical) at −30 °C for 10 min, washed with PBS three times and then incubated in 1 % bovine serum albumin for 30 min at room temperature. The cultures were incubated with the following primary antibodies overnight at 4 °C: monoclonal mouse anti-vimentin (1:1000; Sigma), polyclonal rabbit anti-nestin (1:1000; Sigma), polyclonal rabbit anti-neurofilament (NF)-200 (1:1000; Sigma), and polyclonal chicken anti-βIII-tubulin (1:500) (Millipore, Bedford, MA). After washing with PBS, the samples were incubated with the following secondary antibodies for 30 min at room temperature in the dark: Alexa Fluor 488 goat anti-mouse immunoglobulin G (IgG), Alexa Fluor 488 donkey anti-rabbit IgG; Alexa Fluor 488 goat anti-chicken immunoglobulin Y (all diluted 1:1000) (Molecular Probes, Eugene, OR). The chamber slides were washed with PBS three times and mounted with Vectashield mounting medium containing 4′,6-diamidino-2-phenylindole (DAPI) (Vector Laboratories, Burlingame, CA). For negative controls, the primary antibody was omitted during immunostaining.
Efficiency of neurogenic induction
The majority of immunostained DSCs and BMSCs cultured in FBS-free α-MEM and exposed to conditions likely to induce neurogenesis were positive for neurogenic markers, and the morphology of differentiated cells changed from a fibroblastic to a neuronal-like appearance. To quantify morphological changes, the cells were cultured in induction or control media for 7 days, followed by immunostaining for nestin, βIII-tubulin and NF-200. The number of neurogenic marker-positive DSCs and BMSCs, defined as cells with a multipolar morphology and extending a thin process three times longer than the cell body, was counted in five randomly selected fields of view at 20× magnification in four-well chamber slides at 7 days post-culture. The total number of neurogenic marker-positive cells was also determined in the same fields of view. The number of neuron-like cells was divided by the total number of immunostained cells. The evaluation was repeated in three independent experiments, with six chamber slides per cell type per experiment. The morphological evaluation and calculation for the efficiency of neurogenic induction in this study was carried out as previously described [30], except that we defined cells as those having ‘a multipolar morphology and extending a thin process three times longer than the cell body’, instead of cells having ‘a circular, three-dimensional appearance and extending a thin process at least three times longer than their cell body’.
Karyotype analysis
Karyotype analysis was carried out as previously described [31]. Sub-confluent cells were incubated with 100 nM colcemid (Sigma) for 4 h at 37 °C, then harvested and centrifuged. The cells were resuspended in 70 mM KCl at a concentration of 1 × 104 cells/ml for 20 min at 37 °C, then centrifuged and fixed with freshly prepared methanol:acetic acid (3:1) solution for 5 min at room temperature. Cells were centrifuged again and the supernatant discarded; the pellet was incubated overnight at 4 °C and then resuspended in the methanol:acetic acid solution. The cell suspension in the fixative was dropped onto a wet and cold micro-glass slide and stained with Giemsa solution. Fifty mitotic figures were chosen randomly, chromosomal distribution was counted and the karyotype analyzed.
Statistical analysis
CFU-F determination, cell growth/proliferation assays and cell cycle analysis were repeated three times. Results are expressed as mean ± standard deviation. Statistical analysis was performed using one-way analysis of variance with Bonferroni post hoc testing. Values of p < 0.05 were considered statistically significant, although we have additionally indicated where p < 0.01. Data were analyzed using SPSS 13.0J for Windows (SPSS Japan, Tokyo, Japan).
Results
Colony-forming efficiency of DSCs
The number of CFU-Fs was determined 14 days after plating 1 × 104 cells into a 100-mm dish. The numbers of emerging DPSC, PDLSC, APSC and DFSC colonies were 84 ± 12, 102 ± 24, 140 ± 21, and 151 ± 26, respectively (Fig. 1e). CFU-F values were significantly higher for DFSCs and APSCs compared with PDLSCs and DPSCs (p < 0.05), but there were no statistically significant differences between the DFSC and APSC colonies or between the PDLSC and DPSC colonies.
Cell growth and PDT of DSCs and BMSCs
To evaluate their proliferative capacity, DPSCs, PDLSCs, DFSCs, APSCs and BMSCs were plated at a density of 3 × 103 cells/well in 24-well culture plates and cultured for 12 days in growth media. All four DSCs exhibited significantly greater growth than BMSCs (p < 0.01; Fig. 1f). We detected statistically significant differences between each type of DSC, as follows: DFSC > APSC > PDLSC > DPSC (p < 0.05). The PDT for DPSCs, PDLSCs, APSCs, DFSCs and BMSCs were 28.8, 28.1, 28.0, 27.7 and 32.7 h, respectively.
Cell cycle status of DSCs, BMSCs and cancer cell lines
Flow cytometric analysis revealed that the BMSC population contained a higher percentage of cells in the G0/G1 phase (60.5 ± 2.21 %; Fig. 1g) and a lower percentage of cells in the G2/M phase (24.0 ± 2.58 %; Fig. 1h) compared with the DPSC (51.7 ± 3.98 % and 31.8 ± 6.38 %), PDLSC (46.1 ± 4.56 % and 37.9 ± 0.29 %), DFSC (45.1 ± 5.00 % and 42.7 ± 3.30 %) and APSC (46.2 ± 3.24 % and 42.0 ± 0.55 %) populations. Significant differences between BMSCs and the four DSCs were observed in the proportion of cells in the G0/G1 and G2/M phases following flow cytometric analysis (p < 0.05). The percentages of SKN cells (60.7 ± 9.0 %) and HSC-2 cells (51.9 ± 2.0 %) in the G2/M phase were significantly higher than those of all DSCs and BMSCs (Fig. 1h). In contrast, the percentages of SKN cells (27.7 ± 4.5 %) and HSC-2 cells (36.2 ± 5.6 %) in the G0/G1 phase were significantly lower than those of the other cell types tested (Fig. 1g).
Specific cell surface markers of DSCs and BMSCs
The specific cell markers of DSCs and BMSCs were characterized by flow cytometric analysis (Fig. 2). DSCs and BMSCs showed similar characteristics. All of the five stem cell types were strongly positive for CD44, CD90 and CD105 (cell surface markers associated with mesenchymal stromal cells), but negative for CD14 and CD34 (cell surface markers of hematopoietic cells).
Gene expression profile of DSCs and BMSCs
We used RT-PCR to evaluate gene expression in DSCs and BMSCs before induction. All of the stem cells expressed typical markers for mesenchymal (vimentin), osteogenic (type I collagen and Runx2), neurogenic (nestin) and embryonic (Nanog, Oct3/4 and Sox2) cells (data not shown).
Multilineage differentiation capabilities of DSCs and BMSCs
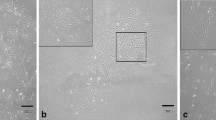
To determine their ability to differentiate, the four types of DSCs and the BMSCs were subjected to osteogenic, adipogenic and neurogenic differentiation procedures. After osteogenic induction for 3 weeks, alizarin red-positive mineralized nodules were observed in all DSCs and in BMSCs (Fig. 3a–e), whereas no alizarin red staining was observed in the control cultures (Fig. 3f–j). After 3 weeks of adipogenic induction, clusters of Oil red O-positive cells were detected among the induced DSCs and BMSCs (Fig. 3k–o), but not in the control cells (Fig. 3p–t).
Differentiation of DSCs and BMSCs along the osteogenic and adipogenic lineages. Alizarin red staining indicated the deposition of mineralization in a DPSCs, b PDLSCs, c DFSCs, d APSCs and e BMSCs cultured in the osteogenic induction medium for 3 weeks. No mineralized nodule formation was observed in f DPSCs, g PDLSCs, h DFSCs, i APSCs and j BMSCs cultured in control medium. Oil red O-staining indicated lipid clusters in k DPSCs, l PDLSCs, m DFSCs, n APSCs and o BMSCs cultured in the adipogenic induction medium for 3 weeks. No lipid clusters were observed in p DPSCs, q PDLSCs, r DFSCs, s APSCs and t BMSCs cultured in the control medium. Scale bars 100 μm
Morphological changes of DSCs and BMSCs following neural induction
To examine the neurogenic potential of the stem cells, all samples were seeded into four-well chamber slides for immunocytochemistry and cultured in neurogenic differentiation or control medium. The control cells displayed positive staining when incubated with antibodies against neurogenic markers such as nestin, βIII-tubulin and NF-200 (Fig. 4a). Subsequently, cells were induced into a neurogenic differentiation pathway by culturing them in neural induction medium for 7 days. The efficiency of neural differentiation was examined by immunocytochemistry, with neurogenic markers detected after induction, similar to the results observed in cultured cells that were not subjected to induction. However, we found that the differentiated cells showed changes in cell morphology from a fibroblast-like appearance to a neuron-like appearance with multipolarity and long processes (Fig. 4a). Therefore, we compared the morphology of the different cell types based on the length of their processes (e.g. neurites) when cells were cultured in neurogenic induction or control medium (Fig. 4b). The results indicated that the number of neuronal-like cells that were positively stained for each neural antibody was significantly increased after neurogenic induction in all stem cell cultures (Fig. 4c; p < 0.01).
Differentiation potential of DSCs and BMSCs along the neurogenic lineage. a Representative image showing morphological changes in PDLSCs by neural induction. Immunocytochemical staining for nestin, βIII-tubulin, and NF-200 was carried out in all stem cells cultured in the presence (+) and absence (−) of neurogenic inductive supplements. Cultures in which the primary antibody was omitted during immunostaining are also given as a negative control. The majority of cells stained positive under both culture conditions. Cell nuclei are depicted with DAPI staining. b, c Evaluation of neurogenic marker-positive cells for neural differentiation efficiency before and after neurogenic induction. b Morphological criteria of a ‘neuron-like’ cell, as exhibited by PDLSCs immunostained with antibody against NF-200. The number of neurogenic marker-positive cells, defined as cells having multipolar morphology that extend a thin process at least three times longer (3L<) than their cell body (L) were counted in five randomly selected fields of view at ×20 magnification for each well in four-well chamber slides, 0 or 7 days after induction. c Percentage of neuronal-like cells among the total number of immunostained cells when cultured in neurogenic induction medium (+) or control medium (−) (*p < 0.01)
Karyotype analysis of DSCs and BMSCs
To examine the karyotype and chromosomal stability of the cultured cells (passage 3), we performed G-banded karyotype analysis. This analysis showed that all samples had a normal karyotype with a diploid chromosome number (2n = 46; Fig. 5).
Karyotype analysis of DSCs and BMSCs. All stem cells were examined at passage 3 and had normal karyotype and diploid sets of chromosomes (2n = 46, XX). a Representative results of PDLSCs. b Distribution of the chromosome number of PDLSCs. Over 95 % of the cells examined had normal chromosomal numbers in all stem cell cultures (2n = 46)
Discussion
In the present study, we isolated four MSC populations from mature teeth (DPSC and PDLSC), impacted immature teeth (APSC) and from the surrounding tissue (DFSC) using well-established cell isolation methods, incorporating collagenase/dispase-catalyzed enzymatic digestion [11]. We also isolated stem cells from human bone marrow by conventional adherent culture techniques [8]. The isolated cells contained a diploid set of chromosomes and had a normal karyotype. To the best of our knowledge, there are no other comparative analyses of this many multiple stem cell types cultured under identical conditions. Our data provide valuable insight into the properties of these stem cells to facilitate their use in research and potential clinical applications.
All of the primary cells obtained from dental tissues exhibited high replicative potential and formed many colonies that appeared to be derived from a single cell when the primary cells were seeded at a low density in a culture dish. DFSCs and APSCs formed a greater number of colonies than either DPSCs or PDLSCs (Fig. 1e). It is possible that DFSCs and APSCs have greater proliferative capabilities because they originate from developing tissues, namely the dental follicle and the apical papilla, respectively. The CFU-F data in this study suggest that the efficiency of colony-forming was comparable to that reported previously [32]. All of the DSCs had better growth characteristics than the BMSCs (Fig. 1f), which are expected to be an important source of autologous cells for stem cell therapy. These findings were reflected by the PDT, with values ranging from 27.7 to 28.8 h for DSCs, compared with 32.7 h for BMSCs. As shown in Fig. 1g, h, cell cycle analysis indicated that over 30 % of cells in the DPSC, PDLSC, DFSC and APSC populations were in the G2/M phase compared with approximately 20 % for BMSCs (Fig. 1h; p < 0.05). By contrast, approximately 60 % of BMSCs were in the G0/G1 phase compared with <50 % of DPSCs, PDLSCs, DFSCs and APSCs (Fig. 1g; p < 0.05). These findings suggest that a greater proportion of DSCs were undergoing mitosis (G2/M phase) whereas the majority of BMSCs were in a state of cell cycle arrest (G0/G1 phase). Interestingly, two cancer cell lines were found to have lower percentages of cells in the G0/G1 phase (Fig. 1g; p < 0.05), and higher percentages in the G2/M phase (Fig. 1h; p < 0.05), than any of the stem cell lines. Taken together, these findings indicate that stem cells obtained from dental tissues have greater clonogenic and proliferative potentials than BMSCs, consistent with previous findings [11, 32, 33], while the active proliferative potential of DSCs is less than that of cancer cells.
To confirm whether the four types of DSCs and BMSCs could differentiate into osteogenic and adipogenic lineages, these cells were cultured in the presence of dexamethasone, β-glycerophosphate and l-ascorbate-2-phosphate for osteogenic induction, and with indomethacin, hydrocortisone and isobutylmethylxanthine for adipogenic induction. After 3 weeks of induction, alizarin red-positive mineralized nodules and Oil red-O-positive lipid droplets were observed in all cultures (Fig. 3), demonstrating the multipotent characteristics of these MSCs. These MSC characteristics of DSCs and BMSCs were confirmed by our flow cytometric analysis of the phenotype of cell surface markers expressed on these cells (Fig. 2). All stem cells were positive for the typical MSC markers (CD44, CD90 and CD105), in agreement with previous studies [19, 34], whereas CD14 and CD34 (markers of blood cell types) were negative, suggesting that our initial cell isolation and primary culture procedures were performed rigorously and established primary cell populations of MSCs that were not contaminated with blood cells. The characterization of our cells as MSC was supported by RT-PCR assays, which showed that gene expression levels of vimentin, type I collagen, Runx2 and nestin (markers for mesenchymal, osteogenic and neurogenic potential, respectively) were similar in all cell types (data not shown). These gene expression patterns seem to be reasonable because the harvested teeth and bone marrow are thought to be reservoirs of MSCs [35]. All of the stem cells expressed Nanog, Oct3/4 and Sox2, which are well-known transcription factors involved in the maintenance of pluripotency in embryonic stem (ES) cells or induced pluripotent stem (iPS) cells [36, 37]. These findings suggest that a small population of pluripotent stem cells, comparable with ES/iPS cells, may exist in our stem cell cultures that are composed of multiple colony-derived stem cell populations. To confirm this hypothesis, we hope to establish a clonal stem cell line originating from a single cell. Future studies should also compare the gene expression profiles of DSCs with those of BMSCs to determine the pluripotency and plasticity of these cell lines, and evaluate their ability to produce functional tissues that could be used in regenerative medicine.
To investigate the neurogenic potential of our stem cells, we first confirmed the endogenous production of neurogenic markers by immunocytochemistry when cultured in non-inductive medium. We found that almost all cultured cells were positively stained by antibodies against nestin, βIII-tubulin and NF-200 (Fig. 4a). Next, neurogenic differentiation was induced in these cultures by supplementing the medium with b-FGF, EGF, ITS and B27. After 7 days of neurogenic induction, the cell morphology changed from a spindle-like fibroblastic appearance to a neuron-like multipolar appearance (Fig. 4a), suggesting cellular maturation in stem cells cultured with neurogenic medium. Therefore, we quantitatively assessed the morphological changes based on the cell body processes formed under neural inductive and non-inductive conditions. The results showed a greater proportion of cells with a neuron-like morphology and neurite outgrowth following differentiation (Fig. 4c; p < 0.01), suggesting that the cultured stem cells differentiated into mature neurons under these conditions. Other reports have described that some DSCs or BMSCs express neural markers, such as nestin and βIII-tubulin, under non-inductive culture conditions [38–40]. Recent studies from our laboratories and other researchers suggest that neurogenic potential is an innate characteristic of MSCs, particularly those of a dental origin that are derived from the cranial neural crest cells [41, 42]. We believe that our established stem cells have high neurogenic potential and would contribute to stem cell research and stem cell therapy for neural disease. However, it is unclear whether the differentiated dental and bone marrow cells were terminally differentiated and had acquired the cellular functions of neurons. This issue will need to be clarified in future studies.
Of particular interest is that the stem cells obtained in this study maintained chromosomal stability and had a normal karyotype at passage 3 (Fig. 5). Previous studies did not describe whether the isolated stem cells had a normal karyotype or chromosomal stability. It is possible that transformation of ex vivo expanded stem cells can result in an abnormal karyotype and chromosomal instability, similar to cancer or sarcoma cell lines [31, 43, 44]. Based on these findings and our hypothesis, we suggest that the stem cells used here retain their physiological cellular phenotype and characteristics during the experiments. Our culture methods and the stem cell lines could be valuable for the development of a practical approach to stem cell transplantation that is both safe and reliable.
Although bone marrow is widely accepted as a reliable source for of MSCs [45, 46], an alternative pool of adult stem cells that can be obtained using less invasive methods is also required [47]. Thus, we focused on extracted teeth and their surrounding tissue as accessible stem cell sources because they can be obtained without additional injury and are usually discarded following dental procedures. Our and other research groups have reported that expanded cultures of ex vivo stem cells derived from dental sources can be recovered after cryopreservation without losing their proliferation and multipotent potential [22, 48–50]. These findings suggest that it may be possible to preserve DSCs in a cell bank system for future clinical use without adverse effects on their properties.
We have described the isolation and characterization of MSCs derived from dental tissue and bone marrow using a standardized cell culture protocol. The stem cells tested showed almost identical properties in terms of gene expression profiles and multipotency traits such as differentiation into osteogenic, adipogenic and neurogenic lineages, but differed in their clonogenic and proliferative potentials. However, these findings suggest that our stem cells consist of heterogeneous cell populations ranging from immature (ES/iPS-like) stem cells to cell lineage-committed progenitor cells, which have some clonogenicity in primary cultures when seeded at a low density. In this culture condition, it appears that committed and differentiated cells cannot proliferate or produce a colony. The properties of the DSCs documented here, and our ability to obtain these from what is essentially medical waste after routine dental extraction procedures, represent significant advantages of these cells in comparison with BMSCs, the collection of which requires invasive bone marrow aspiration. Functional studies are now being planned to confirm whether these DSCs can form tissues in vivo, particularly the use of DPSCs and APSCs to generate dentin/pulp-like tissue, and PDLSCs and DFSCs to generate cementum/PDL-like tissue. The results of such studies will be particularly important to confirm the viability of DSCs being applied clinically. The concept of DSC-based medicine could allow new regenerative therapies to treat not only dental and periodontal diseases but also systemic diseases such as nerve injury and neurodegenerative diseases.
References
Huang GT, Gronthos S, Shi S. Mesenchymal stem cells derived from dental tissues vs. those from other sources: their biology and role in regenerative medicine. J Dent Res. 2009;88:792–806.
Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, Benhaim P, Lorenz HP, Hedrick MH. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7:211–28.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–7.
Baksh D, Yao R, Tuan RS. Comparison of proliferative and multilineage differentiation potential of human mesenchymal stem cells derived from umbilical cord and bone marrow. Stem Cells. 2007;25:1384–92.
Kern S, Eichler H, Stoeve J, Kluter H, Bieback K. Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue. Stem Cells. 2006;24:1294–301.
Shi S, Bartold PM, Miura M, Seo BM, Robey PG, Gronthos S. The efficacy of mesenchymal stem cells to regenerate and repair dental structures. Orthod Craniofac Res. 2005;8:191–9.
Hung SC, Chen NJ, Hsieh SL, Li H, Ma HL, Lo WH. Isolation and characterization of size-sieved stem cells from human bone marrow. Stem Cells. 2002;20:249–58.
Friedenstein AJ, Gorskaja JF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol. 1976;4:267–74.
Casagrande L, Cordeiro MM, Nor SA, Nor JE. Dental pulp stem cells in regenerative dentistry. Odontology. 2011;99:1–7.
Mao JJ, Giannobile WV, Helms JA, Hollister SJ, Krebsbach PH, Longaker MT, Shi S. Craniofacial tissue engineering by stem cells. J Dent Res. 2006;85:966–79.
Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci USA. 2000;97:13625–30.
Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, Shi S. SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci USA. 2003;100:5807–12.
Sonoyama W, Liu Y, Fang D, Yamaza T, Seo BM, Zhang C, Liu H, Gronthos S, Wang CY, Wang S, Shi S. Mesenchymal stem cell-mediated functional tooth regeneration in swine. PLoS One. 2006;1:e79.
Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J, Young M, Robey PG, Wang CY, Shi S. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet. 2004;364:149–55.
Morsczeck C, Gotz W, Schierholz J, Zeilhofer F, Kuhn U, Mohl C, Sippel C, Hoffmann KH. Isolation of precursor cells (PCs) from human dental follicle of wisdom teeth. Matrix Biol. 2005;24:155–65.
Ishkitiev N, Yaegaki K, Calenic B, Nakahara T, Ishikawa H, Mitiev V, Haapasalo M. Deciduous and permanent dental pulp mesenchymal cells acquire hepatic morphologic and functional features in vitro. J Endod. 2010;36:469–74.
Ding G, Liu Y, Wang W, Wei F, Liu D, Fan Z, An Y, Zhang C, Wang S. Allogeneic periodontal ligament stem cell therapy for periodontitis in swine. Stem Cells. 2010;28:1829–38.
Iohara K, Zheng L, Wake H, Ito M, Nabekura J, Wakita H, Nakamura H, Into T, Matsushita K, Nakashima M. A novel stem cell source for vasculogenesis in ischemia: subfraction of side population cells from dental pulp. Stem Cells. 2008;26:2408–18.
Ikeda E, Yagi K, Kojima M, Yagyuu T, Ohshima A, Sobajima S, Tadokoro M, Katsube Y, Isoda K, Kondoh M, Kawase M, Go MJ, Adachi H, Yokota Y, Kirita T, Ohgushi H. Multipotent cells from the human third molar: feasibility of cell-based therapy for liver disease. Differentiation. 2008;76:495–505.
Huang AH, Snyder BR, Cheng PH, Chan AW. Putative dental pulp-derived stem/stromal cells promote proliferation and differentiation of endogenous neural cells in the hippocampus of mice. Stem Cells. 2008;26:2654–63.
Gandia C, Arminan A, Garcia-Verdugo JM, Lledo E, Ruiz A, Minana MD, Sanchez-Torrijos J, Paya R, Mirabet V, Carbonell-Uberos F, Llop M, Montero JA, Sepulveda P. Human dental pulp stem cells improve left ventricular function, induce angiogenesis, and reduce infarct size in rats with acute myocardial infarction. Stem Cells. 2008;26:638–45.
Nakahara T, Nakamura T, Kobayashi E, Kuremoto K, Matsuno T, Tabata Y, Eto K, Shimizu Y. In situ tissue engineering of periodontal tissues by seeding with periodontal ligament-derived cells. Tissue Eng. 2004;10:537–44.
Nakahara T, Nakamura T, Kobayashi E, Inoue M, Shigeno K, Tabata Y, Eto K, Shimizu Y. Novel approach to regeneration of periodontal tissues based on in situ tissue engineering: effects of controlled release of basic fibroblast growth factor from a sandwich membrane. Tissue Eng. 2003;9:153–62.
Nakahara T. Tooth/periodontal organ engineering: the ultimate goal of tooth regeneration. In: GN. G, editor. Tissue Eng Res Trends. New York: Nova Science Publishers; 2008. p. 7-13.
Nakahara T, Ide Y. Tooth regeneration: implications for the use of bioengineered organs in first-wave organ replacement. Hum Cell. 2007;20:63–70.
Nakahara T. A review of new developments in tissue engineering therapy for periodontitis. Dent Clin North Am. 2006;50:265–76. ix-x.
Ishiwata I, Nozawa S, Nagai S, Kurhihara S, Mikata A. Establishment of a human leiomyosarcoma cell line. Cancer Res. 1977;37:658–64.
Momose F, Araida T, Negishi A, Ichijo H, Shioda S, Sasaki S. Variant sublines with different metastatic potentials selected in nude mice from human oral squamous cell carcinomas. J Oral Pathol Med. 1989;18:391–5.
Deasy BM, Gharaibeh BM, Pollett JB, Jones MM, Lucas MA, Kanda Y, Huard J. Long-term self-renewal of postnatal muscle-derived stem cells. Mol Biol Cell. 2005;16:3323–33.
Vierbuchen T, Ostermeier A, Pang ZP, Kokubu Y, Sudhof TC, Wernig M. Direct conversion of fibroblasts to functional neurons by defined factors. Nature. 2010;463:1035–41.
Nakahara T, Tamaki Y, Tominaga N, Ide Y, Nasu M, Ohyama A, Sato S, Ishiwata I, Ishikawa H. Novel amelanotic and melanotic cell lines NM78-AM and NM78-MM derived from a human oral malignant melanoma. Hum Cell. 2010;23:15–25.
Jo YY, Lee HJ, Kook SY, Choung HW, Park JY, Chung JH, Choung YH, Kim ES, Yang HC, Choung PH. Isolation and characterization of postnatal stem cells from human dental tissues. Tissue Eng. 2007;13:767–73.
Alge DL, Zhou D, Adams LL, Wyss BK, Shadday MD, Woods EJ, Gabriel Chu TM, Goebel WS. Donor-matched comparison of dental pulp stem cells and bone marrow-derived mesenchymal stem cells in a rat model. J Tissue Eng Regen Med. 2010;4:73–81.
Wada N, Menicanin D, Shi S, Bartold PM, Gronthos S. Immunomodulatory properties of human periodontal ligament stem cells. J Cell Physiol. 2009;219:667–76.
Barry FP, Murphy JM. Mesenchymal stem cells: clinical applications and biological characterization. Int J Biochem Cell Biol. 2004;36:568–84.
Taura D, Noguchi M, Sone M, Hosoda K, Mori E, Okada Y, Takahashi K, Homma K, Oyamada N, Inuzuka M, Sonoyama T, Ebihara K, Tamura N, Itoh H, Suemori H, Nakatsuji N, Okano H, Yamanaka S, Nakao K. Adipogenic differentiation of human induced pluripotent stem cells: comparison with that of human embryonic stem cells. FEBS Lett. 2009;583:1029–33.
Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–72.
Vollner F, Ernst W, Driemel O, Morsczeck C. A two-step strategy for neuronal differentiation in vitro of human dental follicle cells. Differentiation. 2009;77:433–41.
Arthur A, Rychkov G, Shi S, Koblar SA, Gronthos S. Adult human dental pulp stem cells differentiate toward functionally active neurons under appropriate environmental cues. Stem Cells. 2008;26:1787–95.
Hermann A, Liebau S, Gastl R, Fickert S, Habisch HJ, Fiedler J, Schwarz J, Brenner R, Storch A. Comparative analysis of neuroectodermal differentiation capacity of human bone marrow stromal cells using various conversion protocols. J Neurosci Res. 2006;83:1502–14.
Chai Y, Jiang X, Ito Y, Bringas P Jr, Han J, Rowitch DH, Soriano P, McMahon AP, Sucov HM. Fate of the mammalian cranial neural crest during tooth and mandibular morphogenesis. Development. 2000;127:1671–9.
Thesleff I, Sharpe P. Signalling networks regulating dental development. Mech Dev. 1997;67:111–23.
Suzuki M, Tominaga N, Ide Y, Ohyama A, Nakahara T, Ishikawa H, Tanaka A, Mataga I. Establishment and characterization of the rhabdomyosarcoma cell line designated NUTOS derived from the human tongue sarcoma: special reference to the susceptibility of anti-cancer drugs. Hum Cell. 2010;23:65–73.
Ide Y, Nakahara T, Nasu M, Tominaga N, Ohyama A, Tachibana T, Yasuda M. Establishment and characterization of the NEYS cell line derived from carcinosarcoma of human ovary with special reference to the susceptibility test of anticancer drugs. Hum Cell. 2009;22:72–80.
Rahaman MN, Mao JJ. Stem cell-based composite tissue constructs for regenerative medicine. Biotechnol Bioeng. 2005;91:261–84.
Holden C, Vogel G. Stem cells. Plasticity: time for a reappraisal? Science. 2002;296:2126–9.
Nakahara T. Potential feasibility of dental stem cells for regenerative therapies: stem cell transplantation and whole-tooth engineering. Odontology. 2011;99:105–11.
Ding G, Wang W, Liu Y, An Y, Zhang C, Shi S, Wang S. Effect of cryopreservation on biological and immunological properties of stem cells from apical papilla. J Cell Physiol. 2010;223:415–22.
Papaccio G, Graziano A, d’Aquino R, Graziano MF, Pirozzi G, Menditti D, De Rosa A, Carinci F, Laino G. Long-term cryopreservation of dental pulp stem cells (SBP-DPSCs) and their differentiated osteoblasts: a cell source for tissue repair. J Cell Physiol. 2006;208:319–25.
Seo BM, Miura M, Sonoyama W, Coppe C, Stanyon R, Shi S. Recovery of stem cells from cryopreserved periodontal ligament. J Dent Res. 2005;84:907–12.
Acknowledgments
This work was supported by a Grant-in-Aid for Scientific Research (No. 20390501 to H. I., S. S., T. N. and 19791467 to T. N.) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Science Research Promotion Fund (2008–2010 to T. N., H. I., S. S.) from the Promotion and Mutual Aid Corporation for Private Schools of Japan; and a Research Grant (2009–2010 to T. N., H. I., S. S.) from the Nippon Dental University.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tamaki, Y., Nakahara, T., Ishikawa, H. et al. In vitro analysis of mesenchymal stem cells derived from human teeth and bone marrow. Odontology 101, 121–132 (2013). https://doi.org/10.1007/s10266-012-0075-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-012-0075-0