Abstract
Background
Cathepsin D (CTSD) is an aspartyl proteinase that plays an important role in protein degradation, antigen processing and apoptosis. It has been associated with several pathologies such as cancer, Alzheimer’s disease and inflammatory disorders. Its function in lung diseases remains, however, controversial. In the current study, we determined CTSD activity in serum of patients with chronic obstructive pulmonary disease (COPD) and evaluated the correlations between this proteinase and inflammatory and oxidative parameters. We also investigated the impact of a CTSD C224T polymorphism on enzyme activity and clinicopathological parameters.
Methods
Our population included 211 healthy controls and 138 patients with COPD. CTSD activity, MMPs (-1/-7/-12), cytokines (IL-6, TNF-α), malondialdehyde (MDA), nitric oxide and peroxynitrite levels were measured in patients and controls using standard methods. Genotyping of CTSD C224T polymorphism was determined using PCR–RFLP.
Results
Our results showed an increased CTSD activity in COPD patients compared to healthy controls (4.87 [3.99–6.07] vs. 3.94 [2.91–5.84], respectively, p < 0.001). COPD smokers presented also a higher CTSD activity when compared to nonsmokers (4.91[3.98–6.18] vs. 4.65[4.16–5.82], respectively, p = 0.01), while no differences were found when subjects were compared according to their GOLD stages. The activity of this proteinase was not dependent on the C224T polymorphism because we did not found any influence of this SNP on proteinase activity among patients and controls. Furthermore, our data provide the first evidence of the interrelationships between CTSD activity and both MMPs and TNF-α levels (MMP-1[r = − 0.4; p = 0.02], MMP-7[r = 0.37; p = 0.04], MMP-12[r = 0.43; p = 0.02], TNF-α [r = 0.89, p = 0.001]) in COPD smokers. There were no correlations, however, between CTSD activity and oxidative stress parameters in controls and patients.
Conclusion
Our findings suggest that CTSD could be a relevant marker for COPD disease. Alteration of CTSD activity may be related to increased MMPs and TNF-α levels, particularly in COPD smokers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common cause of morbidity and mortality, and its incidence is still increasing. It is predicted by the World Health Organization to become the third leading cause of death worldwide by 2030 [1]. COPD is characterized by a progressive reversible airflow limitation that is associated with an abnormal inflammatory response of the lungs to noxious particles and gases [2]. Besides inflammation, the pathogenesis of COPD involves other processes such as oxidative stress and imbalance in the activity of proteases and antiproteases in the lung parenchyma. Growing evidence suggests the contribution of proteases in pulmonary diseases and especially in COPD. As an example, neutrophil elastase has been shown to aggravate airflow obstruction in COPD by enhancing inflammation and apoptosis [3, 4]. Matrix metalloproteinases-9 and -12 are also implicated in tissue damage and remodeling and were associated with the severity of COPD [5, 6]. Among cysteine proteases, cathepsin S and caspase-8 were found to be highly expressed in COPD patients [7, 8]. In contrast, little is known about the role of aspartic proteases, particularly cathepsin D (CTSD) in the pathogenesis of COPD.
CTSD is a lysosomal acid proteinase synthesized as a preprocathepsin D in the rough endoplasmic reticulum. It breaks down denatured and abnormal proteins and modulates proteolysis by activating precursor forms of many proteases and inactivating their inhibitors [9]. It is also involved in antigen processing and apoptosis [10]. CTSD has been associated with numerous human pathologies such as cancer, Alzheimer’s disease and inflammatory disorders [11,12,13]. The gene encoding of this proteinase is located on chromosome 11 (11q12). A C to T substitution in exon 2 at position 224 (rs17571) of the CTSD gene has been suggested to affect protein secretion and maturation in breast cancer cells [14].
The goals of the current report were therefore to explore the CTSD activity in patients with COPD and to evaluate relationships with tobacco smoking, inflammatory and oxidative stress markers. We also investigated whether the CTSD C224T polymorphism affects CTSD activity and risk of COPD.
Materials and methods
Study population
The subjects included in this study were 138 patients with COPD, recruited from the services of Physiology and Pneumology, Farhat Hached Hospital, Sousse, Tunisia. The control group consisted of 211 healthy subjects having normal spirometry results and no history of any disease. A questionnaire was filled out containing demographic characteristics, severity of disease based on the criteria of Global Initiative for Chronic Obstructive Pulmonary Disease [2] and history of cigarette smoking. Written informed consent was obtained from all subjects. All patients had a diagnosis confirmed by plethysmography (ZAN 500 Body II; ZAN Meβgrerate GmbH, Germany) according to American Thoracic Society standardizations [15]. COPD was diagnosed based on a clinical history of dyspnea and not fully reversible airflow obstruction which is defined as the ratio of forced expiratory volume in one second (FEV1)/ forced vital capacity (FVC) < 70% after the inhalation of 400 µg salbutamol. COPD patients were classified using GOLD criteria [2] as mild (GOLD I) with FEV1 ≥ 80% predicted, moderate (GOLD II) FEV1 < 80% and ≥ 50% predicted, severe (GOLD III) with FEV1 < 50% and ≥ 30% predicted and very severe (GOLD IV) with FEV1 < 30% predicted. None of the COPD patients reported exacerbation for the previous two months.
Genotyping of C224T CTSD variant
Genotyping of CTSD was performed using by PCR–RFLP. The PCR mixture was composed of DNA (100 ng), 5 μl of 5 × PCR buffer, 1.5 mM of MgCl2, 100 μmol/l of desoxynucleotide triphosphates, 0.5 units of Taq®DNA polymerase (Promega Corp., Madison, WI, USA) and 60 pmol of each primer 5′-GTGACAGGCAGGAGTTTGGT-3′(forward)and5′-GGGCTAAGACCTCATACTCACG-3′(reverse). Reaction conditions used were as follows: 94 °C for 5 min, 35 cycles of 94 °C for 1 min, 60 °C for 1 min and an elongation step at 72 °C for 1 min, final elongation at 72 °C for 7 min. The PCR products were digested with the restriction enzyme MwoI and separated by electrophoresis on a 2% agarose gel (Supplementary file1).
Determination of CTSD activity
Blood samples were collected within the same period from healthy controls and patients with COPD. Serum and plasma were immediately frozen at − 80 °C for further analysis.
Preparation of hemoglobin solution: The supernatant containing plasma and leukocytes was removed after centrifugation at 8000 rpm for 10 min. Packed erythrocytes were then washed four times with isotonic saline (NaCl, 9 g/l), hemolyzed and frozen at − 20 °C. Then, the supernatant was denaturated with citrate buffer (400 mM, pH 2.8). After precipitation with ammonium sulfate (0.1 M) for 30 min at 4 °C, 10 ml of water was added. Then, the supernatant was frozen at − 20 °C for dialysis. To 1 ml of hemoglobin solution (2.5%), 1.5 ml water was added and was applied on a NAP-10 column.
Enzymatic assay: serum CTSD activity was assayed using hemoglobin as a substrate as previously described [16]. Serum was incubated with dialyzed hemoglobin in citrate buffer (400 mM, pH 2.8) for 20 h at 37 °C, and the reaction was stopped with addition of trichloroacetic acid (5%). After centrifugation, the supernatant was rescued and the absorbance of the liberated peptides was measured according to Lowry procedure [17]. The amount of 0.5 ml of supernatant was supplemented with 1.5 ml of copper reagent. Then, 0.25 ml of Folin and Ciocalteu's reagent diluted with distilled water (2:1 v/v ratio) was added. The absorbance was measured at 750 nm after 30 min, and the activity of CTSD was expressed as nM of tyrosine/mg protein/min. Reactions were made in the presence or absence of the CTSD inhibitor pepstatin (1.43 mM).
For tyrosine estimation, 0.5 to 2 μg of tyrosine was made up to 1 ml with 0.5 ml TCA 5% and 0.5 ml citrate buffer (400 mM, pH 2.8). Then, 1.5 ml of copper reagent was added to the solution followed by 0.25 ml of 2:1 diluted Folin–Ciocalteu reagent. The absorbance was taken at 750 nm. The amount of total protein was measured at 595 nm using the Bradford protein assay [18].
Enzyme-linked immunosorbent assays of serum MMPs (-1, -7 and 12)
MMPs (-1/-7/-12) levels were determined by enzyme-linked immunosorbent assays using commercially available kits according to the manufacturer’s instructions [MMP-1 (OK-0272); Assay Biotechnology Company, Inc., Sunnyvale, CA, USA; MMP-7 (DMP700); R&D Systems, Abingdon, UK, and MMP-12 (EK0950); Boster Biological Technology, Pleasanton, CA, USA)].
2.5 Enzyme-linked immunosorbent assays of cytokines (IL-6 and TNF- α).
IL-6 and TNF-α levels were evaluated by ELISA using commercially available kits according to the manufacturer’s instructions [IL-6 (D6050); TNF-α (DTA00C) R&D Systems].
Determination of nitric oxide (NO), peroxynitrite and thiobarbituric acid-reactive substances (MDA-TBARS)
Nitric oxide was determined using the Griess reaction as previously described [19] and was expressed as pmol/mg of protein. The concentration of peroxynitrite was determined according to VanUffelen and colleagues [20] and was expressed in µmol/ml of plasma. The concentration of MDA was assayed as previously described [21] and was expressed in μmol/l of plasma.
Statistical Analysis
Statistical analyses were performed using SPSS, version 17.0 (SPSS Inc., Chicago, IL, USA). Student's t test and Mann–Whitney U test were applied to compare groups, and data were expressed as the mean ± SD or median (interquartile range). Correlations between the different parameters were analyzed using the Spearman rank correlation coefficient. The genotype frequencies of CTSD polymorphism were compared between patients and controls using the Chi-square (χ2) test. The odds ratios (OR) and 95% confidence intervals (CI) were calculated using an unconditional logistic regression model and were adjusted for age and sex. A p value < 0.05 was considered statistically significant.
Results
Clinical characteristics of the control subjects and patients with chronic obstructive pulmonary disease
Clinical characteristics of patients and controls are summarized in Table1. The study included 211 controls and 138 patients with COPD. As shown in Table1, the mean age was 61.61 ± 13.2 in cases and 57.2 ± 9.6 in healthy subjects. As expected, FEV1% and FVC% were significantly lower in patients compared to controls (55.7 ± 18.6 vs. 93.8 ± 0.8 and 77.9 ± 19.6 vs. 96.2 ± 10.2, respectively) (Table1). As indicated in Table1, CTSD activity was significantly increased in COPD patients compared to healthy controls (4.87 [3.99–6.07] vs. 3.94 [2.91–5.84] nM tyr/mg prot/min, respectively, p < 0.001). Similarly, the levels of MMP-12, MDA and IL-6 were markedly higher in cases than in controls (p < 0.05) (Table1). Conversely, increased level of NO was found in healthy controls in comparison with patients with COPD (213.3 [142.7–309.68] vs. 178.6 [128.07–269.18] pmol/mg, respectively, p = 0.01). There were no significant differences in MMP-7/-1, peroxynitrite and TNF-α levels between COPD patients and healthy subjects (p > 0.05) (Table1). In COPD group, there were 10.2%, 44.9%, 39.1% and 5.8% patients with stages I, II, III and IV disease, respectively. No significant differences in MMPs, oxidative and inflammatory parameters were found in patients with mild–moderate disease (GOLD I/II) when compared to patients with advanced disease stages (GOLD III/IV) (Table1).
Impact of smoking on clinicopathological parameters in COPD patients and controls
We also determined the impact of smoking on the different clinicopathological parameters (Table2).
A significant increase in CTSD activity was found among COPD smokers as compared with nonsmokers (4.91 [3.98–6.18] vs. 4.65 [4.16–5.82] nM tyr/mg prot/min, respectively, p = 0.01) (Table2). CTSD activity was also significantly higher in COPD smokers than in healthy controls (4.91 [3.98–6.18] vs. 3.94 [2.91–5.84] nM tyr/mg prot/min, respectively, p < 0.001). Likewise, the levels of MMP-7/-12, NO, MDA and IL-6 were significantly higher in the COPD smokers group when compared with the controls group (p < 0.05). NO and MDA levels were also increased in COPD nonsmokers compared to healthy controls (p < 0.05) (Table2). However, no difference in the mean values of the other parameters was found between the two COPD subgroups.
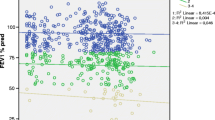
Relationships between CTSD activity and the different studied parameters in COPD patients and controls
There were correlations between CTSD activity and both MMPs [MMP-12 (r = 0.4, p = 0.02), MMP-7 (r = 0.27, p = 0.04), MMP-1 (r = − 0.32, p = 0.02)] and TNF-α (r = 0.85, p < 0.001) levels in COPD patients (Table3). CTSD activity was also correlated with MMPs and TNF-α levels in COPD smokers (Table3). Conversely, no correlations were found for the different parameters in controls and COPD patients.
Impact of the C224T CTSD polymorphism on COPD risk
The distribution of CTSD C224T genotypes in patients and controls did not differ from that expected from Hardy–Weinberg equilibrium (Table4). The frequencies of CC, CT, and TT genotypes in the control and COPD groups were 78.7%, 18.5% and 0.9% and 81.2%, 18.1% and 0.7%, respectively. There were no significant differences in genotype distribution of the CTSD C224T polymorphism between the two groups before and after adjustment for age and sex (Table4). As shown in Table4, the distribution of the C224T CTSD genotypes was not different between smokers without COPD and COPD smokers.
Impact of a C224T polymorphism on cathepsin D activity and clinicopathological parameters
We further analyzed the correlations between CTSD C224T variants and clinicopathological parameters in COPD patients and healthy controls (Table5). Table5 shows lower FEV1/FVC in patients carrying CT and TT genotypes when compared to those having the CC genotype (51.8 ± 2.4 vs. 57.57 ± 1.06, respectively, p = 0.02). Likewise, decreased FEV1% was also observed in patients with CT and TT genotypes but the difference was not significant (Table5). No significant impact of the.
CTSD C224T polymorphism on lung function was found among controls. As shown in Table5, MMP-7 and MMP-12 levels were significantly higher among patients carrying the T allele in comparison with those with the C allele (p < 0.05). Similarly, levels of MMP-7 and MMP-12 still significantly higher in COPD smokers with the T allele compared to those with the C allele. No significant impact of CTSD C224T polymorphism on MMP-7 and MMP-12 levels was found, however, among healthy subjects (Table5). CTSD activity, MMP-1, NO, peroxynitrite, MDA and cytokines levels did not differ also according to CTSD C224T genotypes in cases and controls (Table5).
Discussion
The purpose of the current study was to explore CTSD activity in COPD patients and to determine the impact of smoking as well as relationships with inflammatory and oxidative markers. We also evaluated the role of a C224T CTSD variant on enzyme activity and susceptibility to COPD.
CTSD is a lysosomal aspartic proteinase involved in proteolytic degradation, apoptosis and inflammation. It is synthesized as an inactive preprocathepsin D form, which undergoes several proteolytic cleavages to produce the active enzyme [22]. Up to now, only a few studies explored the role of this proteinase in pulmonary diseases. Among these, Faiz et al. [23] reported no significant differences in the activity and expression of CTSD in the bronchoalveolar lavage fluid from asthmatics. Pulmonary emphysema was associated, however, with the activation of cathepsins D and E [24, 25]. In pulmonary fibrosis, CTSD was involved in airway remodeling with excessive apoptosis and prolonged inflammation leading to tissue degradation [26, 27]. In the current report, we found an increase in CTSD activity among COPD patients in comparison with healthy controls, which suggests a potential role of this enzyme in COPD. This confirms earlier findings showing higher levels of CTSD in blood and bronchoalveolar lavage fluid from COPD patients [28,29,30]. The higher activity of CTSD in COPD patients was not dependent, however on the C224T variant since no influence of this SNP on proteinase activity was found among patients and controls. These findings contrast with two previous reports showing that a C to T transition corresponding to the substitution of alanine by valine might alter procathepsin D secretion and maturation [14, 31]. Besides, the C224T genotype frequencies were not different between COPD patients and healthy controls, which may suggest that this variant is not associated with the risk of COPD among Tunisians. From our results, there was also a significant increase in CTSD activity in patients with mild to moderate disease, as well as, those with advanced COPD in comparison with healthy individuals. We did not find, however, significant differences in activity between different GOLD stages which may suggest a role of this proteinase in COPD development rather than to disease progression. These results contrast with data from Ohlmeier et al. [30] showing higher levels of this enzyme in mild to moderate individuals in comparison with patients with advanced disease.
Considering smoking status, an increased CTSD activity was observed in COPD smokers compared with both healthy controls and COPD nonsmokers. These results are consistent with data from Bracke et al. [32], showing a higher CTSD expression after exposure of pulmonary macrophages to cigarette smoke. Similarly, Nagaraj et al. [33] suggested that treatment for human oral squamous cell carcinomas with cigarette smoke condensate activates cathepsins B, D and L in a dose-dependent manner and further increases MMPs expression and/or activity. In the current report, as for CTSD, the levels of MMP-7, MMP-12 and IL-6 were increased in COPD smokers compared to healthy subjects, which may suggest that CTSD could play a role in COPD development through enhanced tissue destruction and inflammation. In line with this, CTSD has been reported to contribute to tissue degradation and remodeling in the alveolar epithelium during early and late stages of pulmonary fibrosis [26]. It also plays an important role in the activation of nuclear factor-kappa B required for the transcription of most pro-inflammatory factors [34].
We further determined the relationships between CTSD activity and both MMPs and inflammatory markers. Interestingly, CTSD activity was positively correlated with TNF-α levels in both COPD and smoking patients, which suggest the contribution of this proteinase in inflammatory processes [35]. In this regard, Liu and colleagues [36] found that elevated levels of TNF-α and FasL induced the expression and activity of CTSD. From our results, significant relationships were also found between CTSD activity and MMP-1/-7/-12 levels in COPD smokers which may support the role of these enzymes in extracellular matrix breakdown and abnormal tissue remodeling in COPD leading to airway limitation [37]. These results agree with data from Wang and colleagues [24] demonstrating that an emphysematous response in mice associates with the activation of both MMP-12 and cathepsin D.
Conclusion
Our results highlight an increase in CTSD activity in COPD patients and particularly in smokers. This proteinase was also correlated with both MMPs (-1/-7/-12) and TNF-α levels in COPD patients. Our observations do not support, however, the impact of a CTSD C224T polymorphism on CTSD activity and susceptibility to COPD. Further studies in a larger population are needed to validate our findings and to clarify the mechanism of action of CTSD in COPD.
References
World Health Organization Chronic obstructive pulmonary disease (COPD) 2020 [Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Available from: https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019.
Qiu Y, Zhu J, Bandi V, et al. Biopsy neutrophilia, neutrophil chemokine and receptor gene expression in severe exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2003;168:968–75.
Lee KH, Lee CH, Jeong J, et al. Neutrophil elastase differentially regulates IL-8 and VEGF production by cigarette smoke extract. J Biol Chem. 2015;290:28438–45.
Chaudhuri R, McSharry C, Brady J, et al. Sputum matrix metalloproteinase-12 in patients with chronic obstructive pulmonary disease and asthma: relationship to disease severity. Allergy Clin Immunol. 2012;129(655):e8-663.e8.
Linder R, Rönmark E, Pourazar J, et al. Serum metalloproteinase-9 is related to COPD severity and symptoms - cross-sectional data from a population based cohort-study. Respir Res. 2015;16:28.
Geraghty P, Greene CM, O’Mahony M, et al. Secretory leucocyte protease inhibitor inhibits interferon-gamma-induced cathepsin S expression. Biol Chem. 2007;282(46):33389–95.
Gogebakan B, Bayraktar R, Ulaslı M, et al. The role of bronchial epithelial cell apoptosis in the pathogenesis of COPD. Mol Biol Rep. 2014;41(8):5321–7.
Minarowska A, Gacko M, Karwowska A, et al. Human cathepsin D. Folia Histochem Cytobiol. 2008;46(1):23–38.
Pereira H, Oliveira CSF, Castro L, et al. Côrte-Real M. Yeast as a tool to explore cathepsin D function. Microb Cell. 2015; 2(7): 225–234.
Pruitt FL, He Y, Franco OE, et al. Cathepsin d acts as an essential mediator to promote malignancy of benign prostatic epithelium. Prostate. 2013;73:476–88.
Chai YL, Chong JR, Weng J, et al. Lysosomal cathepsin D is upregulated in Alzheimer’s disease neocortex and may be a marker for neurofibrillary degeneration. Brain Pathol. 2019;29(1):63–74.
Hausmann M, Obermeier F, Schreiter K, et al. Cathepsin D is up-regulated in inflammatory bowel disease macrophages. Clin Exp Immunol. 2004;136(1):157–67.
Touitou I, Capony F, Brouillet JP, et al. Missense polymorphism (C/T224) in the human cathepsin D pro-fragment determined by polymerase chain reaction-single strand conformational polymorphism analysis and possible consequences in cancer cells. Eur J Cancer. 1994;30A(3):390–4.
American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995; 152:S77–S121
Anson ML. The estimation of pepsin, trypsin, papain, and cathepsin with hemoglobin. J Gen Physiol. 1938;22(1):79–89.
Lowry OH, Rosebrough NJ, Farr AL, et al. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193(1):265–75.
Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–54.
Arif E, Ahsan A, Vibhuti A, et al. Endothelial nitric oxide synthase gene variants contribute to oxidative stress in COPD. Biochem Biophys Res Commun. 2007;361(1):182–8.
Vanuffelen BE, Van Der Zee J, De Koster BM, et al. Intracellular but not extracellular conversion of nitroxyl anion into nitric oxide leads to stimulation of human neutrophil migration. Biochem J. 1998;330(Pt 2):719–22.
Draper HH, Hadley M. Malondialdehyde determination as index of lipid peroxidation. Methods Enzymol. 1990;186:421–31.
Pranjol MZ, Gutowski N, Hannemann M, et al. The potential role of the proteases Cathepsin D and Cathepsin L in the progression and metastasis of epithelial ovarian cancer. Biomolecules. 2015;5(4):3260–79.
Faiz A, Tjin G, Harkness L, et al. The expression and activity of Cathepsins D, H and K in asthmatic airways. PLoS ONE. 2013;8(3):e57245.
Wang Z, Zheng T, Zhu Z, et al. Interferon gamma induction of pulmonary emphysema in the adult murine lung. J Exp Med. 2000;192(11):1587–600.
Zhang X, Shan P, Homer R, et al. Cathepsin E promotes pulmonary emphysema via mitochondrial fission. Am J Pathol. 2014;184(10):2730–41.
Kasper M, Lackie P, Haase M, et al. Immunolocalization of cathepsin D in pneumocytes of normal human lung and in pulmonary fibrosis. Virchows Arch. 1996;428(4–5):207–15.
Chwieralski CE, Welte T, Bühling F. Cathepsin-regulated apoptosis. Apoptosis. 2006;11(2):143–9.
Almansa R, Socias L, Sanchez-Garcia M, et al. Critical COPD respiratory illness is linked to increased transcriptomic activity of neutrophil proteases genes. BMC Res Notes. 2012;5:401.
Tu C, Mammen MJ, Li J, et al. Large-scale, ion-current-based proteomics investigation of bronchoalveolar lavage fluid in chronic obstructive pulmonary disease patients. J Proteome Res. 2014;13(2):627–39.
Ohlmeier S, Nieminen P, Gao J, et al. Lung tissue proteomics identifies elevated transglutaminase 2 levels in stable chronic obstructive pulmonary disease. Am J Physiol Lung Cell Mol Physiol. 2016;310(11):L1155–65.
Mása M, Maresová L, Vondrásek J, et al. cathepsin D propeptide: mechanism and regulation of its interaction with the catalytic core. Biochemistry. 2006;45(51):15474–82.
Bracke K, Cataldo D, Maes T, et al. Matrix metalloproteinase-12 and cathepsin D expression in pulmonary macrophages and dendritic cells of cigarette smoke-exposed mice. Int Arch Allergy Immunol. 2005;138(2):169–79.
Nagaraj NS, Zacharias W. Cigarette smoke condensate increases cathepsin-mediated invasiveness of oral carcinoma cells. Toxicol Lett. 2007 Apr 25;170(2):134–45.
Gan P, Xia Q, Hang G, et al. Knockdown of cathepsin D protects dopaminergic neurons against neuroinflammation-mediated neurotoxicity through inhibition of NF-κB signalling pathway in Parkinson’s disease model. Clin Exp Pharmacol Physiol. 2019;46:337–49.
Conus S, Perozzo R, Reinhecke T, et al. Caspase-8 is activated by cathepsin D initiating neutrophil apoptosis during the resolution of inflammation. J Exp Med. 2008;205(3):685–98.
Liu J, Yang L, Tian H, et al. Cathepsin D is involved in the oxygen and glucose deprivation/reperfusion-induced apoptosis of astrocytes. Int J Mol Med. 2016;38(4):1257–63.
Navratilova Z, Kolek V, Petrek M. Matrix metalloproteinases and their inhibitors in chronic obstructive pulmonary disease. Arch Immunol Ther Exp (Warsz). 2016;64(3):177–93.
Acknowledgements
This work was supported by the Ministry of Higher Education and by the Ministry of Public Health of the Tunisian Government. The authors wish to thank all the patients and controls who participated in this study.
Funding
The authors S. Bchir, S. Boumiza, H. ben Nasr, A. Garrouch, I. Kallel, Z. Tabka and K. Chahed declare that this study was funded by the Tunisian Ministry of Higher Education and Research (LR19ES09).
Author information
Authors and Affiliations
Contributions
S. Bchir collected clinical samples, analyzed and interpreted data and drafted the manuscript. S. Boumiza and H. ben Nasr collected clinical samples and revised the manuscript. A. Garrouch and Z. Tabka recorded clinical characteristics of participants and revised the manuscript. I. Kallel provided critical technical support in data analysis. K. Chahed contributed to experimental design, analyzed and interpreted data and drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors S. Bchir, S. Boumiza, H. ben Nasr, A. Garrouch, I. Kallel, Z. Tabka and K. Chahed have no conflicts of interest that are directly relevant to the content of this article.
Ethical approval and informed consent
The study was approved by the local ethical committee of Farhat Hached Hospital (Sousse, Tunisia, approval number: 08–2011).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bchir, S., Boumiza, S., ben Nasr, H. et al. Impact of cathepsin D activity and C224T polymorphism (rs17571) on chronic obstructive pulmonary disease: correlations with oxidative and inflammatory markers. Clin Exp Med 21, 457–465 (2021). https://doi.org/10.1007/s10238-021-00692-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-021-00692-1