Abstract
Objectives
Multiple studies suggest that the EQ-5D may overestimate health-related quality of life (HRQoL) in patients with coeliac disease (CD). We aimed to develop and psychometrically test potentially relevant bolt-on dimensions to improve the measurement performance of the EQ-5D-5L in CD patients.
Methods
The development and selection of bolt-ons were informed by a literature review on HRQoL in CD, expert and patient input. A cross-sectional online survey was conducted amongst 312 adult CD patients. Respondents completed the EQ-5D-5L, two condition-specific bolt-ons newly-developed for the present study [dining (DI) and gastrointestinal problems (GI)] and three existing bolt-ons [cognition (CO), sleep (SL) and tiredness (TI)]. The following psychometric properties were tested: ceiling, informativity, convergent and known-group validity, and dimensionality (confirmatory factor analysis).
Results
Adding the TI, SL, GI, DI and CO individual bolt-ons reduced the ceiling of the EQ-5D-5L (39%) to 17%, 23%, 24%, 26% and 37%, respectively. GI excelled with strong convergent validity with the Gastrointestinal Symptom Rating Scale total score (rs=0.71) and improved the discriminatory power for all known-groups. GI was the only bolt-on loading on a different factor from the five core dimensions, whereas the other four bolt-ons loaded onto the same ‘psychosocial health’ factor as the EQ-5D-5L anxiety/depression dimension.
Conclusion
The DI, GI, SL and TI bolt-ons, especially the GI, enhance the validity of EQ-5D-5L in patients with CD, suggesting their value in capturing important HRQoL aspects potentially missed by the five core dimensions. These bolt-ons can be used in sensitivity analyses supporting health technology assessments and subsequent resource allocation decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generic preference-accompanied measures of health-related quality of life (HRQoL) are widely used in economic evaluations to assess the impact of health conditions and their treatments on HRQoL [1]. The advantages of these measures include the ability to capture the impact of conditions or treatment on the overall HRQoL rather than focusing solely on specific symptoms, and facilitating comparisons across different conditions and disease areas [1]. Among various generic preference-accompanied measures, the EQ-5D is the most commonly used instrument [2]. It has shown good validity and responsiveness in a wide array of acute and chronic health conditions [3]. Moreover, it is recommended by health technology assessment (HTA) guidelines in more than 20 countries [4, 5]. However, the EQ-5D may not perform adequately in all health conditions, given its limitations in content validity in certain HRQoL areas [6].
An area, where the EQ-5D might not fully capture all aspects of HRQoL, is gastrointestinal-related conditions. Although the ‘discomfort’ component of the pain/discomfort composite dimension is intended to assess physical discomfort, potentially incorporating various gastrointestinal symptoms, respondents often use this dimension primarily to report pain, resulting in an underreporting of physical discomfort [7]. Therefore, in any health condition where gastrointestinal problems are relevant, there is a potential to improve the instrument’s validity and sensitivity. An example is coeliac disease (CD), an immune-mediated systemic disorder activated by the ingestion of gluten in genetically susceptible individuals, with a global prevalence of 0.7–1.4% [8,9,10]. CD patients may struggle not only with gastrointestinal symptoms (e.g. abdominal pain, bloating, diarrhoea, constipation), but also with extra-intestinal symptoms (e.g. fatigue, cognitive impairment, depression) [11,12,13,14]. Currently, the only treatment option is a strict, life-long gluten-free diet (GFD) that has a complex impact on the HRQoL of patients [15]. This is due to the demanding nature of the GFD, implying increased dietary costs [16], reduced nutritional value [17], and social constraints [18,19,20]. The literature suggests that while patients’ HRQoL improves following the GFD, it does not normalize [21].
The EQ-5D has been found to potentially overestimate HRQoL among patients with CD, which is supported by three earlier EQ-5D studies from the UK, Poland and Slovenia reporting better HRQoL in CD patients after diagnosis compared to the general population [22,23,24]. One possible solution to enhance the coverage of the EQ-5D is the addition of extra dimensions, called ‘bolt-ons’, to the instrument. These additional dimensions may cover specific health problems or dysfunctions relevant to particular conditions or populations [25, 26]. So far, several bolt-on dimensions have been developed for the EQ-5D; for example, a skin irritation and self-confidence bolt-on for patients with chronic skin diseases [27,28,29], a vision bolt-on for patients with vision problems, such as cataract [30, 31], and a respiratory bolt-on for patients with asthma and chronic obstructive pulmonary disease [32]. The value added by these bolt-ons varies, and their impact on utilities may be limited in some cases [26]. For example, a sleep ‘bolt-on’ dimension to EQ-5D-3L was found to have minimal impact on utilities [33].
This study aimed to develop and assess the psychometric properties of potentially relevant bolt-ons for the EQ-5D-5L in patients with CD. We hypothesized that adding bolt-ons to the EQ-5D-5L would improve the measurement properties, compared to the original EQ-5D-5L.
Methods
Development and selection of bolt-ons
In this study, we used both newly developed condition-specific bolt-ons and relevant existing bolt-ons for the EQ-5D-5L (Online Resource S1). The development and selection of bolt-ons were informed by a literature review on HRQoL in CD as well as relevant domains from existing relevant condition-specific measures, and expert input. The panel of experts comprised a CD patient, a gastroenterologist professor and two health economists experienced in utility assessment.
A conceptual model summarising the most important health outcomes in patients with CD has recently been published [34]. This conceptual model, based on an analysis of the item content of condition-specific measures and additional interviews with both CD clinical experts and payers, encompasses two large symptom groups (gastrointestinal and extra-intestinal) and six aspects of HRQoL. The most common gastrointestinal symptoms included in CD-specific measures are bloating, nausea, diarrhoea, abdominal pain/discomfort, loose stool and flatulence. The most common extra-intestinal symptoms in these instruments are low energy/fatigue, headaches, food cravings and slowness/difficulty thinking. The six HRQoL areas include daily activities (e.g. mobility, self-care, reduced concentration), psychological impact (e.g. anxiety, depression, stress, mental fatigue), relationships (e.g. stigmatization, family life), social or leisure (social activities, dining out at restaurants), sleep (e.g. insomnia), and treatment/dietary (e.g. bathroom usage, difficulty adhering to a GFD). While the five dimensions of the EQ-5D-5L seem to provide a good coverage of the main symptoms and HRQoL aspects of CD, there might be some important areas missed out, where the addition of bolt-ons could be particularly useful. Based on the frequency of the abovementioned symptoms and HRQoL impacts and discussions between members of the expert panel, the decision was taken to develop two new condition-specific bolt-on items to more comprehensively reflect the psychosocial and physical burden of CD on HRQoL: dining (DI), which featured examples of ‘following a diet’ and ‘eating out’, and gastrointestinal problems (GI), listing the following examples in parentheses: diarrhoea, constipation, nausea, vomiting, heartburn, bloating and gases. Furthermore, we selected three existing bolt-ons that held relevance in the context of CD: cognition (CO), sleep (SL) and tiredness (TI) [35, 36], presented in Online Resource S1. The CO bolt-on was deemed especially relevant as CD patients can experience certain neurologic and psychiatric manifestations, including cerebellar ataxia, peripheral neuropathy, brainstem dysfunction, epilepsy, dementia, headache and depression [37,38,39]. A ‘social relationships’ bolt-on dimension was not included in the study as we considered that it would potentially overlap with some aspects of HRQoL covered by the DI bolt-on (eating out) as well as the usual activities EQ-5D-5L dimension.
In developing the two new bolt-ons, we aimed to formulate the items in a way that could potentially make them suitable also for measuring HRQoL in other health conditions with similar impacts on patients’ lives. For instance, the GI bolt-on could be applied in any disease characterised by gastrointestinal problems, while the DI bolt-on could be used in other diseases requiring specific diets, such as diabetes. Both bolt-on items were framed the same manner as the EQ-5D-5L items, featuring a short dimension title accompanied by a few examples in parentheses and the same number of and severity-type response levels ranging from ‘no problems’ to ‘extreme problems’ [25]. When selecting the examples for the items, we relied on both the language used in qualitative expert interviews in an earlier study and item wordings of commonly used condition-specific instruments [34]. The language and wording of the two bolt-on items were finalized based on input gathered from a CD patient and subsequent discussions within the expert panel.
Cross-sectional survey among CD patients
An online cross-sectional survey was conducted among 312 Hungarian adult CD patients between December 2020 and January 2021 [40]. Permission for conducting the survey was obtained from the Research Ethics Committee of the Corvinus University of Budapest (reference no. KRH/390/2020). A convenience sample of CD patients was recruited through different patient organisations and social media groups. Participation in the survey was voluntary and anonymous, with no incentives offered. The survey was administered using Qualtrics (Qualtrics 2020, Provo, UT, USA). To be eligible for participation in the study, respondents needed to be aged 18 years or older, provide informed consent and confirm their diagnosis of CD.
The questionnaire consisted of four parts. The first part included questions about CD-related clinical characteristics, adherence to GFD, disease duration, and any comorbidities and symptoms experienced related to CD. The second part comprised various standardised measures to assess HRQoL and wellbeing, while the third part employed preference elicitation methods to evaluate respondents’ current own health and hypothetical health state vignettes. The final section collected sociodemographic data, such as age, sex, place of residence and employment status. All questions were mandatory, and as a result, there were no missing responses.
Outcome measures
Three main outcome measures were included in the questionnaire: EQ-5D-5L with bolt-ons, Satisfaction with Life Scale (SWLS), and the Gastrointestinal Symptom Rating Scale (GSRS).
The EQ-5D-5L comprises two parts: a five-dimensional descriptive system and a visual analogue scale (EQ VAS) [41]. The descriptive system has five dimensions, each represented by one item: mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (PD), and anxiety/depression (AD). For each item, responses are based on a 5-point severity scale, ranging from ‘no problems’ to ‘extreme problems/unable to’. A total of 55=3125 different health profiles may be described by the five dimensions. For instance, the profile of 11111 indicates that the patient has no problems in any of the five dimensions, representing the best possible health state. While the EQ-5D-5L can be scored using national value sets for the calculation of quality-adjusted life years (QALYs) [42], this approach was not used in this study. Instead, level sum scores (LSSs) were computed by taking an unweighted sum of the responses on each of the five dimensions [43]. The EQ VAS is a vertical hash marked scale with the endpoints of 0 (the worst health you can imagine) and 100 (the best health you can imagine) [41].
In our questionnaire, the five bolt-on items were completed after the EQ VAS in the following order: DI, GI, CO, TI and SL. Each bolt-on was presented on a separate screen. The total number of possible health profiles increases substantially when adding bolt-ons to the EQ-5D-5L. It becomes as high as 56=15,625 when including one, 57=78,125 when including two bolt-ons, and so forth.
CD-specific symptoms were measured with the Gastrointestinal Symptom Rating Scale (GSRS) [44], a widely used instrument in CD patients [45,46,47]. The GSRS comprises 15 items organised into five domains: reflux (2 items), abdominal pain (3 items), indigestion (4 items), diarrhoea (3 items) and constipation (3 items). Each item has seven response options ranging from ‘no discomfort at all’ (= 1) to ‘very severe discomfort’ (= 7). Adding up the item scores, the total score may range from 15 to 105, where lower scores correspond to fewer health problems.
The Satisfaction with Life Scale (SWLS) was used to assess the patients’ subjective wellbeing [48]. This measure consists of 5 statements, each rated on a 7-point Likert scale. The possible scores range from 5 to 35, where lower scores indicate dissatisfaction, and higher scores denote greater life satisfaction.
Analyses of psychometric properties
We followed the analytical framework used to test psychometric properties of bolt-ons in multiple previous studies [25, 26, 49]. First, each individual bolt-on was tested separately, and subsequently, various combinations of bolt-ons were examined. The selection of bolt-on combinations was conducted incrementally, considering the performance of each individual bolt-on. Data were analysed using Stata 14.0 (StataCorp. 2015, College Station, TX, USA) and R 4.2.0 (R Core Team, 2022, Vienna, Austria) and SPSS 27.0 (IBM Corp., 2023, Armonk, NY, USA). For all analyses, a p < 0.05 was considered statistically significant.
Distributional characteristics, ceiling and informativity
Descriptive analysis was used to summarise the demographic and clinical characteristics of the patients. The distributions of patients’ responses across different levels of the EQ-5D-5L and bolt-on items were presented as relative frequencies. We determined the frequency of different health profiles within the sample upon the addition of bolt-on(s). We calculated the ceiling both at the level of individual items and at the level of the instrument itself (i.e. proportion of patients with the best possible health profile in the EQ-5D-5L with and without bolt-on(s)). Similarly we explored the absolute (Shannon index, H’) and relative informativity (Shannon evenness index, J’) of each individual bolt-on and the EQ-5D-5L plus bolt-on(s) [50]. We hypothesized that adding bolt-on(s) would lead to a reduction in the ceiling and an improvement in both the absolute and relative informativity.
Convergent and divergent validity
Spearman’s rank-order correlations (rs) were used to test the associations between EQ-5D-5L dimensions, bolt-ons, GSRS domains and total score, and EQ VAS. Correlation coefficients were interpreted as very weak (< 0.20), weak (0.20–0.39), moderate (0.40–0.59), strong (0.60–0.79) and very strong (≥ 0.80) [51]. We assumed that the GI bolt-on would demonstrate moderate or strong correlation with GSRS domains and total score as well as with the pain/discomfort EQ-5D-5L dimension. This latter hypothesis arises from the understanding that certain gastrointestinal symptoms are associated with at least some physical discomfort [7]. Further, we anticipated a moderate correlation between (i) CO and TI with usual activities; (ii) SL and TI with pain/discomfort; (iii) CO, SL and TI with anxiety/depression [52,53,54,55,56]. Regarding the DI bolt-on, our hypothesis was that the bolt-on item would exhibit a (very) weak correlation with the five core EQ-5D-5L items due to the conceptual distinction between them.
Known-group validity
To evaluate the known-group validity of the EQ-5D-5L with bolt-on(s) as compared to the EQ-5D-5L alone, mean LSSs were computed and subsequently standardized to a 0-100 scale to ensure score comparability. Patients were categorised into known groups based on health status, as assessed on a 5-point scale (poor, fair, good, very good and excellent), tertiles of GSRS total scores and the presence of any symptoms at the time of the survey. To quantify the relative efficiency in detecting differences among these known groups, we calculated the ratio of the F-statistic from the analysis of variance. The EQ-5D-5L was taken as a reference for determining relative efficiency; thus, an F-ratio > 1 indicated that EQ-5D-5L with bolt-on(s) was more efficient at distinguishing across groups. To assess the statistical significance of an F-ratio differing from 1, we estimated 95% confidence intervals using 3000 bootstrap replications. Additional bolt-ons were added to the EQ-5D-5L until the newly included bolt-on resulted in a statistically significant improvement in relative efficiency (higher ANOVA F values), thereby indicating an improvement in the known-group validity of the instrument.
Explanatory power
We performed both univariable and multivariable linear regression analyses to compare the exploratory power of the EQ-5D-5L and bolt-on items. In all models, the EQ VAS or SWLS total scores were used as dependent variables. Furthermore, for every case, two different models were run: one unadjusted and one adjusted for age, gender and GSRS score. In the univariable models, we individually examined the five items of the EQ-5D-5L and the five bolt-on items. Multivariable models were developed incrementally by adding bolt-on items to the model, along with the five EQ-5D-5L items, that contributed the most to the adjusted R2. If the inclusion of a bolt-on item failed to increase the adjusted R², it was subsequently excluded from the model.
Dimensionality analyses
To explore the underlying factor structure of the bolt-ons, we employed principal component analysis (PCA) and confirmatory factor analysis (CFA). We included the five items EQ-5D-5L, the five bolt-ons, the five GSRS domains and the five SWLS items in these analyses. The PCA was performed using a promax rotation, and the number of factors was determined based on the Kaiser’s criterion [57]. Factor loadings were interpreted based on the following reference values: ≤0.32 (unacceptable), 0.33–0.44 (poor), 0.45–0.54 (fair), 0.55–0.62 (good), 0.63–0.70 (very good) and ≥ 0.71 (excellent) [58]. CFA was used to test whether the data fit to our hypothesized measurement model. To address the ordinal nature of items, we employed the diagonally weighted least squares (DWLS) estimator to compute factor loadings. Model fit was considered acceptable when the root mean square error of approximation (RMSEA) was less than 0.08 and the comparative fit index (CFI) exceeded 0.90 [59].
Results
Characteristics of the patient population
The mean age was 35.8 (SD 11.5), ranging from 18 to 80 years, and the majority of patients were female (70.2%) (Table 1). Most patients (89.4%) reported to have at least one comorbidity with the most common being allergies, other food intolerances and gastroesophageal reflux disease. Over two-thirds (70.8%) of the patients experienced symptoms of CD in the previous week, with fatigue being the most commonly reported. Among gastrointestinal symptoms, flatulence, heartburn, diarrhoea, upset stomach, constipation and nausea were reported by 25.3%, 22.8%, 18.3%, 12.5%, 10.3% and 5.8%, respectively.
Distributional characteristics, ceiling and informativity
The distribution of responses to the EQ-5D-5L dimensions and bolt-ons is shown in Table 2. Among the five core dimensions, SC demonstrated the highest ceiling (98.1%), followed by MO (82.7%), UA (77.9%), AD (59.0%), and PD (58.7%) (Table 3). For all but one (CO) of the bolt-ons, the ceiling was lower than that of any of the five core EQ-5D-5L dimensions. Based on the ceiling, the order of the bolt-ons was as follows: TI (22.8%), GI (39.1%), SL (44.6%), DI (52.9%), and CO (74.0%). The ceiling of the EQ-5D-5L was 38.8% (i.e. proportion of 11111 profiles). Adding the TI, SL, GI, DI and CO individual bolt-ons reduced the ceiling to 17.0%, 23.1%, 24.0%, 26.3% and 36.5%, respectively. When adding all five bolt-ons to the EQ-5D-5L, the ceiling was reduced to 7.4%. The number of profiles significantly increased by adding bolt-ons to the EQ-5D-5L, with the largest increase observed with DI, where the number of profiles nearly doubled.
All bolt-ons but CO demonstrated both a higher absolute and relative informativity than any of the five core dimensions (Table 3). The TI and GI bolt-on items showed the highest relative informativity. Absolute informativity increased with the addition of any of the five bolt-ons to the EQ-5D-5L (from 3.71 to 4.33–4.95). Moreover, relative informativity also increased with the addition of the bolt-ons, except for CO. The highest improvement in relative informativity was achieved by adding the DI bolt-on. Absolute informativity increased with adding an increasing number of bolt-ons; however, relative informativity increased only up to four bolt-ons.
Convergent and divergent validity
The correlations between the EQ-5D-5L, EQ VAS, bolt-ons and GSRS domains and total score are shown in Table 4. In line with our hypotheses, a moderate correlation was observed between GI and PD (rs=0.508), between TI and PD (rs=0.465) and between TI and AD (rs=0.425). The GI bolt-on was strongly correlated with GSRS total score (rs=0.712) and moderately with each GSRS domain (range of rs: 0.419 to 0.584) as expected. The CO, DI and SL bolt-ons exhibited only weak or very weak correlations with any of the five core dimensions of the EQ-5D-5L.
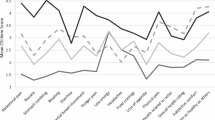
Known-group validity
The addition of the GI bolt-on significantly improved the ability of the EQ-5D-5L to discriminate between groups of patients based on self-perceived health status, GSRS tertiles and the presence of symptoms, with relative efficiencies ranging between 1.30 (95%CI 1.14–1.49) and 1.84 (95%CI 1.56–2.23) (Table 5). After the inclusion of the GI bolt-on, no additional bolt-ons were able to further improve the known-group validity of the instrument.
Exploratory power
The results of the univariable linear regression analysis revealed that UA (adjusted R2 = 0.304) and PD (adjusted R2 = 0.301) demonstrated the highest explanatory power for EQ VAS scores (Table 6). The CO (adjusted R2 = 0.196) and GI (adjusted R2 = 0.179) bolt-ons performed the best among the bolt-ons. With regard to SWLS, AD (adjusted R2 = 0.140) and PD (adjusted R2 = 0.116) exhibited the highest explanatory power, while TI (adjusted R2 = 0.103) and GI (adjusted R2 = 0.095) demonstrated the highest values among the bolt-ons. The addition of bolt-ons to the EQ-5D-5L improved the explained variance of EQ VAS and SWLS scores, as indicated by adjusted R2. Specifically, two bolt-ons (GI and CO) improved the explained variance in EQ VAS from 0.411 to 0.440, while three bolt-ons (DI, GI and SL) improved the explained variance in SWLS from 0.193 to 0.206. When adjusting the models for age, gender and GSRS score, there were only minimal differences in the best-performing bolt-ons, and the contributions of CO and GI to explaining health (EQ VAS) and DI to wellbeing (SWLS) were confirmed.
Dimensionality
The PCA identified four factors (sorted by descending eigenvalue): ‘gastrointestinal problems’, ‘satisfaction with life’, ‘psychosocial health’ and ‘pain and usual activities’ (Online Resource S2). These factors explained 61.9% of the total variance. The GSRS domains and GI bolt-on loaded onto the ‘gastrointestinal problems’ factor, while the remaining four bolt-ons along with the EQ-5D-5L AD item loaded onto the ‘psychosocial health’ factor. All five SWLS items loaded onto the ‘satisfaction with life’ factor, whereas the ‘pain and usual activities’ factor was constituted by the first four EQ-5D-5L items. The EQ-5D-5L PD item was loaded on both the ‘gastrointestinal problems’ and ‘pain and usual activities’ factors, with a higher factor loading for the latter. The CFA confirmed the results of PCA in terms of the number of factors identified and the relationships between items and factors (Table 7). The model showed an appropriate fit with an RMSEA of 0.064 and CFI of 0.927. All but two items (EQ-5D-5L SC and DI bolt-on) had a standardized factor loading of > 0.55, suggesting a good fit. Only the GI bolt-on loaded on a completely different factor than any EQ-5D-5L item; the other four bolt-ons were loaded on the same ‘psychosocial health’ factor as the EQ-5D-5L AD item.
Discussion
This study presented the psychometric testing of two newly-developed (dining and gastrointestinal problems) and three existing (cognition, sleep, tiredness) bolt-on items for the EQ-5D-5L in patients with CD. The addition of any of the five bolt-ons reduced the ceiling and increased the absolute informativity of the instrument; however, the usefulness of CO seemed marginal in this study population. While the SL and TI bolt-ons exhibited strong descriptive characteristics, the GI and DI bolt-ons appeared to perform slightly better in this specific population, which consisted of patients all following a GFD.
The GI bolt-on demonstrated excellent measurement performance, including strong convergent validity with the GSRS domains and total score, enhanced explanatory power for EQ VAS and significantly improved known-group validity. Notably, this was the only bolt-on that loaded on a different factor from any of the five core dimensions, supporting its value in capturing an aspect of HRQoL not addressed by the core dimensions. However, earlier qualitative and quantitative findings indicate that the impact of gastrointestinal problems can, to some extent, be picked up by the pain/discomfort item [7, 60,61,62]. This aligns with our convergent validity results, showing a moderate correlation (rs=0.51) between the GI bolt-on and the pain/discomfort item. Previous research suggests that several respondents use this item mainly to report ‘pain’, but not other forms of physical discomfort [7, 63, 64]. Targeted bolt-ons addressing specific aspects of physical discomfort, such as skin irritation, breathing problems or gastrointestinal problems, therefore can enhance the instrument’s content validity and sensitivity [27,28,29, 65]. While our study confirms the value of the GI bolt-on, further investigations are recommended to better understand the potential conceptual overlap between the GI bolt-on with pain/discomfort and to identify specific areas where a GI bolt-on could add the greatest value to the instrument.
The inclusion of the DI bolt-on resulted in a substantial improvement in explanatory power for subjective wellbeing, suggesting its capacity to capture additional information. In factor analyses, the DI bolt-on loaded onto the ‘psychosocial health’ factor alongside the CO, SL and TI bolt-ons, as well as the EQ-5D-5L anxiety/depression item, indicating potential partial overlap in constructs. However, the inclusion of more closely dining-related items might have revealed a separate ‘diet’ factor, as proposed by conceptual models for HRQoL in coeliac disease [34]. The DI bolt-on did not further enhance known-group validity after the addition of the GI bolt-on (that performed best). This may be attributed to our definition of known groups, which focused on physical health categories rather than psychosocial health or wellbeing groups. Further investigations are recommended to assess the DI bolt-on’s measurement properties in different populations, incorporating more diet-related items and questions.
This research has a few limitations. The data collection was conducted through a self-administered online survey, relying on self-reported clinical data that were not verified by physicians. The sample was not representative of the whole population of CD patients in Hungary, as all patients followed GFD at the time of the survey, and a voluntary online survey may be affected by self-selection bias. Due to the cross-sectional nature of the study, we did not evaluate test-retest reliability or responsiveness of the bolt-ons. Furthermore, the data collection took place during the second wave of Covid-19 pandemic in Hungary. This timing might have impacted the HRQoL and wellbeing of patients, potentially affecting the measurement properties of the instrument and bolt-ons. As the current study focused on assessing the added value of the bolt-ons, the determination of a final item wording was not within the scope. Future studies are recommended to better understand patients’ perspectives and experiences to finalize the item wording for the new bolt-ons. Further research is needed to investigate the psychometric properties of these bolt-ons in diverse patient groups, such as a sample consisting of both patients following and not following a GFD. Testing the bolt-ons in other relevant patient populations (e.g. gluten intolerance, irritable bowel syndrome and inflammatory bowel disease) is also recommended. Lastly, while our findings suggest the added value of bolt-ons, the impact of these bolt-ons on utilities and, consequently, their potential to enhance the sensitivity of QALY estimations in cost-utility analyses are an additional important direction for future research.
Conclusion
Our findings suggest that the DI, GI, SL and TI bolt-ons improve the measurement performance of the EQ-5D-5L in patients with CD. Among the bolt-on items, GI demonstrated strong psychometric performance in multiple tests, suggesting its value in capturing important aspects of HRQoL, that are potentially missed by the core five dimensions of EQ-5D-5L in patients with CD.
Data availability
All data of this study are available from the corresponding author upon reasonable request.
Code availability
N/A.
References
Brazier, J., Ara, R., Rowen, D., Chevrou-Severac, H.: A review of generic preference-based measures for use in cost-effectiveness models. Pharmacoeconomics. 35(Suppl 1), 21–31 (2017). https://doi.org/10.1007/s40273-017-0545-x
Richardson, J., Khan, M.A., Iezzi, A., Maxwell, A.: Comparing and explaining differences in the magnitude, content, and sensitivity of utilities predicted by the EQ-5D, SF-6D, HUI 3, 15D, QWB, and AQoL-8D multiattribute utility instruments. Med. Decis. Mak. 35(3), 276–291 (2015). https://doi.org/10.1177/0272989x14543107
Feng, Y.S., Kohlmann, T., Janssen, M.F., Buchholz, I.: Psychometric properties of the EQ-5D-5L: A systematic review of the literature. Qual. Life Res. 30(3), 647–673 (2021). https://doi.org/10.1007/s11136-020-02688-y
Kennedy-Martin, M., Slaap, B., Herdman, M., et al.: Which multi-attribute utility instruments are recommended for use in cost-utility analysis? A review of national health technology assessment (HTA) guidelines. Eur. J. Health Econ. 21(8), 1245–1257 (2020). https://doi.org/10.1007/s10198-020-01195-8
Rencz, F., Gulácsi, L., Drummond, M., et al.: EQ-5D in Central and Eastern Europe: 2000–2015. Qual. Life Res. 25(11), 2693–2710 (2016). https://doi.org/10.1007/s11136-016-1375-6
Brazier, J.: Is the EQ-5D fit for purpose in mental health? Br. J. Psychiatry. 197(5), 348–349 (2010). https://doi.org/10.1192/bjp.bp.110.082453
Rencz, F., Janssen, M.F.: Analyzing the Pain/Discomfort and Anxiety/Depression composite domains and the meaning of discomfort in the EQ-5D: A mixed-methods study. Value Health. (2022). https://doi.org/10.1016/j.jval.2022.06.012
Singh, P., Arora, A., Strand, T.A., et al.: Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 16(6):823–836 e2. (2018). https://doi.org/10.1016/j.cgh.2017.06.037
Roberts, S.E., Morrison-Rees, S., Thapar, N., et al.: Systematic review and meta-analysis: The incidence and prevalence of paediatric coeliac disease across Europe. Aliment. Pharmacol. Ther. 54(2), 109–128 (2021). https://doi.org/10.1111/apt.16337
Leffler, D.A., Dennis, M., Edwards George, J., et al.: A validated disease-specific symptom index for adults with celiac disease. Clin. Gastroenterol. Hepatol. 7(12), 1328–1334 (2009). 1334.e1-3 https://doi.org/10.1016/j.cgh.2009.07.031
Jelsness-Jørgensen, L.P., Bernklev, T., Lundin, K.E.A.: Fatigue as an extra-intestinal manifestation of Celiac Disease. Syst. Rev. Nutrients. 10(11) (2018). https://doi.org/10.3390/nu10111652
Clappison, E., Hadjivassiliou, M., Zis, P.: Psychiatric manifestations of Coeliac Disease, a systematic review and Meta-analysis. Nutrients. 12(1) (2020). https://doi.org/10.3390/nu12010142
Leffler, D.A., Green, P.H., Fasano, A.: Extraintestinal manifestations of coeliac disease. Nat. Rev. Gastroenterol. Hepatol. 12(10), 561–571 (2015). https://doi.org/10.1038/nrgastro.2015.131
Caio, G., Volta, U., Sapone, A., et al.: Celiac disease: A comprehensive current review. BMC Med. 17(1), 142 (2019). https://doi.org/10.1186/s12916-019-1380-z
Kivela, L., Caminero, A., Leffler, D.A., Pinto-Sanchez, M.I., Tye-Din, J.A., Lindfors, K.: Current and emerging therapies for coeliac disease. Nat. Rev. Gastroenterol. Hepatol. 18(3), 181–195 (2021). https://doi.org/10.1038/s41575-020-00378-1
Lee, A.R., Ng, D.L., Zivin, J., Green, P.H.: Economic burden of a gluten-free diet. J. Hum. Nutr. Diet. 20(5), 423–430 (2007). https://doi.org/10.1111/j.1365-277X.2007.00763.x
Thompson, T., Dennis, M., Higgins, L.A., Lee, A.R., Sharrett, M.K.: Gluten-free diet survey: Are americans with coeliac disease consuming recommended amounts of fibre, iron, calcium and grain foods? J. Hum. Nutr. Diet. 18(3), 163–169 (2005). https://doi.org/10.1111/j.1365-277X.2005.00607.x
Addolorato, G., De Lorenzi, G., Abenavoli, L., Leggio, L., Capristo, E., Gasbarrini, G.: Psychological support counselling improves gluten-free diet compliance in coeliac patients with affective disorders. Aliment. Pharmacol. Ther. 20(7), 777–782 (2004). https://doi.org/10.1111/j.1365-2036.2004.02193.x
Sverker, A., Hensing, G., Hallert, C.: Controlled by food’- lived experiences of coeliac disease. J. Hum. Nutr. Diet. 18(3), 171–180 (2005). https://doi.org/10.1111/j.1365-277X.2005.00591.x
Leffler, D.A., Edwards-George, J., Dennis, M., et al.: Factors that influence adherence to a gluten-free diet in adults with celiac disease. Dig. Dis. Sci. 53(6), 1573–1581 (2008). https://doi.org/10.1007/s10620-007-0055-3
Burger, J.P.W., de Brouwer, B., IntHout, J., Wahab, P.J., Tummers, M., Drenth, J.P.H.: Systematic review with meta-analysis: Dietary adherence influences normalization of health-related quality of life in coeliac disease. Clin. Nutr. 36(2), 399–406 (2017). https://doi.org/10.1016/j.clnu.2016.04.021
Violato, M., Gray, A.: The impact of diagnosis on health-related quality of life in people with coeliac disease: A UK population-based longitudinal perspective. BMC Gastroenterol. 19(1), 68 (2019). https://doi.org/10.1186/s12876-019-0980-6
Norstrom, F., Lindholm, L., Sandstrom, O., Nordyke, K., Ivarsson, A.: Delay to celiac disease diagnosis and its implications for health-related quality of life. BMC Gastroenterol. 11, 118 (2011). https://doi.org/10.1186/1471-230X-11-118
Turk, E., Micetic-Turk, D., Sikic-Pogacar, M., Tapajner, A., Vlaisavljevic, V., Prevolnik Rupel, V.: Health related QoL in celiac disease patients in Slovenia. Health Qual. Life Outcomes. 18(1), 356 (2020). https://doi.org/10.1186/s12955-020-01612-9
Mulhern, B.J., Sampson, C., Haywood, P., et al.: Criteria for developing, assessing and selecting candidate EQ-5D bolt-ons. Qual. Life Res. 31(10), 3041–3048 (2022). https://doi.org/10.1007/s11136-022-03138-7
Geraerds, A., Bonsel, G.J., Janssen, M.F., Finch, A.P., Polinder, S., Haagsma, J.A.: Methods used to identify, test, and assess impact on preferences of Bolt-Ons: A systematic review. Value Health. 24(6), 901–916 (2021). https://doi.org/10.1016/j.jval.2020.12.011
Swinburn, P., Lloyd, A., Boye, K.S., Edson-Heredia, E., Bowman, L., Janssen, B.: Development of a disease-specific version of the EQ-5D-5L for use in patients suffering from psoriasis: Lessons learned from a feasibility study in the UK. Value Health. 16(8), 1156–1162 (2013). https://doi.org/10.1016/j.jval.2013.10.003
Rencz, F., Mukuria, C., Bató, A., Poór, A.K., Finch, A.P.: A qualitative investigation of the relevance of skin irritation and self-confidence bolt-ons and their conceptual overlap with the EQ-5D in patients with psoriasis. Qual. Life Res. 31(10), 3049–3060 (2022). https://doi.org/10.1007/s11136-022-03141-y
Szlávicz, E., Szabó, Á., Kinyó, Á., et al.: Content validity of the EQ-5D-5L with skin irritation and self-confidence bolt-ons in patients with atopic dermatitis: A qualitative think-aloud study. Qual. Life Res. 33(1), 101–111 (2024). https://doi.org/10.1007/s11136-023-03519-6
Longworth, L., Yang, Y., Young, T., et al.: Use of generic and condition-specific measures of health-related quality of life in NICE decision-making: A systematic review, statistical modelling and survey. Health Technol. Assess. 18(9), 1–224 (2014). https://doi.org/10.3310/hta18090
Luo, N., Wang, X., Ang, M., et al.: A Vision Bolt-On Item could increase the discriminatory power of the EQ-5D index score. Value Health. 18(8), 1037–1042 (2015). https://doi.org/10.1016/j.jval.2015.08.002
Hoogendoorn, M., Oppe, M., Boland, M.R.S., Goossens, L.M.A., Stolk, E.A., Rutten-van Mölken, M.: Exploring the impact of adding a respiratory dimension to the EQ-5D-5L. Med. Decis. Mak. 39(4), 393–404 (2019). https://doi.org/10.1177/0272989x19847983
Yang, Y., Brazier, J., Tsuchiya, A.: Effect of adding a sleep dimension to the EQ-5D descriptive system: A bolt-on experiment. Med. Decis. Mak. 34(1), 42–53 (2014). https://doi.org/10.1177/0272989x13480428
Clifford, S., Taylor, A.J., Gerber, M., et al.: Concepts and instruments for patient-reported Outcome Assessment in Celiac Disease: Literature Review and experts’ perspectives. Value Health. 23(1), 104–113 (2020). https://doi.org/10.1016/j.jval.2019.07.018
Janssen, B., Krabbe, P., Lamers, L., et al.: The Cognition dimension revisited: A detailed study on its added value and interactions with EQ-5D core dimensions. Presented at: The 30th scientific Plenary Meeting of the EuroQol Group Montréal, September 12–13, 2013;
Haagsma, J.: al. e.: POPCORN: longitudinal effects of the COVID-19 pandemic on individual’s health-related quality of life. (EQ project 238-RA)
Bushara, K.O.: Neurologic presentation of celiac disease. Gastroenterology. 128(4 Suppl 1), S92–S97 (2005). https://doi.org/10.1053/j.gastro.2005.02.018
Casella, G., Bordo, B.M., Schalling, R., et al.: Neurological disorders and celiac disease. Minerva Gastroenterol. Dietol. 62(2), 197–206 (2016)
Giuffrè, M., Gazzin, S., Zoratti, C., et al.: Celiac Disease and neurological manifestations: From gluten to Neuroinflammation. Int. J. Mol. Sci. 23(24) (2022). https://doi.org/10.3390/ijms232415564
Angyal, M.M., Lakatos, P.L., Jenei, B., Brodszky, V., Rencz, F.: Health utilities and willingness to pay in adult patients with coeliac disease in Hungary. Qual. Life Res. 32(9), 2503–2516 (2023). https://doi.org/10.1007/s11136-023-03418-w
Herdman, M., Gudex, C., Lloyd, A., et al.: Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 20(10), 1727–1736 (2011). https://doi.org/10.1007/s11136-011-9903-x
Rencz, F., Brodszky, V., Gulácsi, L., et al.: Parallel valuation of the EQ-5D-3L and EQ-5D-5L by Time Trade-Off in Hungary. Value Health. 23(9), 1235–1245 (2020). https://doi.org/10.1016/j.jval.2020.03.019
Feng, Y.S., Jiang, R., Pickard, A.S., Kohlmann, T.: Combining EQ-5D-5L items into a level summary score: Demonstrating feasibility using non-parametric item response theory using an international dataset. Qual. Life Res. 31(1), 11–23 (2022). https://doi.org/10.1007/s11136-021-02922-1
Svedlund, J., Sjodin, I., Dotevall, G.: GSRS–a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig. Dis. Sci. 33(2), 129–134 (1988). https://doi.org/10.1007/BF01535722
Hindryckx, P., Levesque, B.G., Holvoet, T., et al.: Disease activity indices in coeliac disease: Systematic review and recommendations for clinical trials. Gut. 67(1), 61–69 (2018). https://doi.org/10.1136/gutjnl-2016-312762
Kulich, K.R., Madisch, A., Pacini, F., et al.: Reliability and validity of the gastrointestinal Symptom Rating Scale (GSRS) and quality of life in reflux and dyspepsia (QOLRAD) questionnaire in dyspepsia: A six-country study. Health Qual. Life Outcomes. 6, 12 (2008). https://doi.org/10.1186/1477-7525-6-12
Canestaro, W.J., Edwards, T.C., Patrick, D.L.: Systematic review: Patient-reported outcome measures in coeliac disease for regulatory submissions. Aliment. Pharmacol. Ther. 44(4), 313–331 (2016). https://doi.org/10.1111/apt.13703
Diener, E., Emmons, R.A., Larsen, R.J., Griffin, S.: The satisfaction with Life Scale. J. Pers. Assess. 49(1), 71–75 (1985). https://doi.org/10.1207/s15327752jpa4901_13
Rencz, F., Janssen, M.F.: Testing the Psychometric Properties of 9 bolt-ons for the EQ-5D-5L in a General Population Sample. Value in Health. 27(7), 943–954 (2024). https://doi.org/10.1016/j.jval.2024.03.2195
Janssen, B.M.F., Birnie, E., Bonsel, G.J.: Evaluating the discriminatory power of EQ-5D, HUI2 and HUI3 in a US general population survey using Shannon’s indices. Qual Life Res. 16(5), 895–904 (2007). https://doi.org/10.1007/s11136-006-9160-6
Straightforward statistics for the behavioral sciences: Thomson Brooks/Cole Publishing Co. xxii, 600–xxii, 600 (1996)
de Graaf, J.A., Kuijpers, M., Visser-Meily, J., Kappelle, L.J., Post, M.: Validity of an enhanced EQ-5D-5L measure with an added cognitive dimension in patients with stroke. Clin. Rehabil. 34(4), 545–550 (2020). https://doi.org/10.1177/0269215520907990
Ophuis, R.H., Janssen, M.F., Bonsel, G.J., Panneman, M.J., Polinder, S., Haagsma, J.A.: Health-related quality of life in injury patients: The added value of extending the EQ-5D-3L with a cognitive dimension. Qual. Life Res. 28(7), 1941–1949 (2019). https://doi.org/10.1007/s11136-019-02156-2
Geraerds, A., Polinder, S., Spronk, I., et al.: Sensitivity of the EQ-5D-5L for fatigue and cognitive problems and their added value in Q-fever patients. Qual. Life Res. 31(7), 2083–2092 (2022). https://doi.org/10.1007/s11136-021-03069-9
Rencz, F., Brodszky, V., Janssen, M.F.: A direct comparison of the Measurement properties of EQ-5D-5L, PROMIS-29 + 2 and PROMIS Global Health Instruments and EQ-5D-5L and PROPr utilities in a General Population Sample. Value Health. 26(7), 1045–1056 (2023). https://doi.org/10.1016/j.jval.2023.02.002
Chen, G., Olsen, J.A.: Filling the psycho-social gap in the EQ-5D: The empirical support for four bolt-on dimensions. Qual. Life Res. 29(11), 3119–3129 (2020). https://doi.org/10.1007/s11136-020-02576-5
Horn, J.L.: A rationale and test for the number of factors in factor analysis. Psychometrika. 30(2), 179–185 (1965). https://doi.org/10.1007/BF02289447
Comrey, A.L., Lee, H.B.: A First Course in Factor Analysis, 2nd edn. Lawrence Erlbaum Associates, Hillsdale, NJ, US (1992)
Hu, L., Bentler, P.M.: Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol. Methods. 3(4), 424–453 (1998). https://doi.org/10.1037/1082-989X.3.4.424
Bulamu, N.B., Vissapragada, R., Chen, G., et al.: Responsiveness and convergent validity of QLU-C10D and EQ-5D-3L in assessing short-term quality of life following esophagectomy. Health Qual. Life Outcomes. 19(1), 233 (2021). https://doi.org/10.1186/s12955-021-01867-w
Rencz, F., Lakatos, P.L., Gulácsi, L., et al.: Validity of the EQ-5D-5L and EQ-5D-3L in patients with Crohn’s disease. Qual. Life Res. 28(1), 141–152 (2019). https://doi.org/10.1007/s11136-018-2003-4
Ito, K., Mitobe, Y., Inoue, R., Momoeda, M.: Impact of nausea/vomiting on EQ-5D-5L utility scores in patients taking iron preparations for heavy menstrual bleeding or anemia. BMC Womens Health. 23(1), 505 (2023). https://doi.org/10.1186/s12905-023-02652-1
McDonald, R., Mullett, T.L., Tsuchiya, A.: Understanding the composite dimensions of the EQ-5D: An experimental approach. Soc. Sci. Med. 265, 113323 (2020). https://doi.org/10.1016/j.socscimed.2020.113323
Engel, L., Whitehurst, D.G.T., Haagsma, J., Janssen, M.F., Mulhern, B.: What is measured by the composite, single-item pain/discomfort dimension of the EQ-5D-5L? An exploratory analysis. Qual. Life Res. 32(4), 1175–1186 (2023). https://doi.org/10.1007/s11136-022-03312-x
Hoogendoorn, M., Jowett, S., Dickens, A.P., et al.: Performance of the EQ-5D-5L Plus Respiratory Bolt-On in the Birmingham Chronic Obstructive Pulmonary Disease Cohort Study. Value Health. 24(11), 1667–1675 (2021). https://doi.org/10.1016/j.jval.2021.05.006
Acknowledgements
The authors acknowledge Gabor Rabatin for his support in programming the questionnaire, and Alex Bató for his support in conducting the data analyses.
Funding
F.R.’s work was supported by the János Bolyai Research Scholarship of the Hungarian Academy of Sciences (BO/00304/21) and the New National Excellence Program of the Ministry for Innovation and Technology from the source of the National Research, Development and Innovation Fund (ÚNKP-23-5-CORVINUS-5). Project no. 2023 − 2.1.2-KDP-2023-00016 has been implemented with the support provided by the Ministry of Culture and Innovation of Hungary from the National Research, Development and Innovation Fund, financed under the KDP-2023 funding scheme for M.M.A.’s work.
Open access funding provided by Corvinus University of Budapest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained from the Research Ethics Committee of the Corvinus University of Budapest (no. KRH/390/2020).
Informed consent
Informed consent was obtained from all patients included in the study.
JEL classification
I10.
Conflict of interest
M.F.J. and F.R. are members of the EuroQol Group. The views expressed in this article are those of the authors and do not necessarily reflect those of the EuroQol Research Foundation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Angyal, M.M., Janssen, M.F., Lakatos, P.L. et al. The added value of the cognition, dining, gastrointestinal problems, sleep and tiredness bolt-on dimensions to the EQ-5D-5L in patients with coeliac disease. Eur J Health Econ (2024). https://doi.org/10.1007/s10198-024-01719-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10198-024-01719-6