Abstract
Objective
To evaluate the impact of multiple comorbidities/complications on health-related quality of life (HRQoL) and health utilities in insulin-treated type 2 diabetes (T2DM).
Methods
In a non-interventional, epidemiological study, data were collected from medical records and via interviews for 938 subjects from various geographical areas of Greece. HRQoL and health utilities were explored with the EQ-5D-5L. Univariate associations were evaluated with the Mann–Whitney and Kruskal–Wallis tests for continuous and Chi-squared tests for nominal variables, and binary logistic regressions were employed to obtain marginal effects. Employing a split sample approach, various specifications of ordinary least squares regression models were evaluated in terms of goodness of fit, model specification, shrinkage and predictive and discriminative performance, to select the best model for mapping health utilities using the whole dataset.
Results
Overall, the most important factors of impaired HRQoL and health utilities were higher age, female gender, obesity, poor glycemic control and increased duration of insulin treatment. History and increasing concurrence of all complications assessed were associated with exacerbated HRQoL problems, decreased health utilities and diminished health state, although it was not always statistically significant. The highest disutilities were associated with stroke (− 0.082), diabetic retinopathy (− 0.066), diabetic neuropathy (− 0.051) and severe hypoglycemia (− 0.050).
Conclusions
The deleterious impact of comorbidities on insulin-dependent T2DM subjects’ HRQoL has been confirmed and clinicians should adapt the priorities of disease management accordingly. The derived health utility estimates may be valuable for conducting economic evaluations of interventions in the area of T2DM when data are not available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a chronic condition characterised by raised levels of blood glucose. DM is vested with an increasing public health interest, as its already epidemic prevalence (~ 8.3% worldwide) is projected to rise to 9.9%, i.e. 592 million afflicted people, by the year 2030 [1]. Type 2 DM (T2DM) accounts for 90–95% of all cases, with its therapy being intensified along with the disease progression [2].
T2DM is a major cause of morbidity and mortality, as its lifelong health impact is further augmented by concurrent complications that are pathophysiologically related or unrelated to DM [3,4,5]. Diabetics are correlated with increased risk of a wide range of macrovascular and microvascular conditions, such as heart failure, visual impairment, kidney failure, nerve damage (including amputation) and depression [3, 6].
Health-related quality of life (HRQoL) in T2DM is greatly impaired by the combined effect of related comorbidities in various domains of functioning and well-being [3, 7]. HRQoL in T2DM encompasses the effect of health, illness and treatment on patients’ physical, psychological and social domains of quality of life (QoL) [8]. There is a plethora of generic (e.g. the EuroQol five-dimensional questionnaire [EQ-5D]) and disease-specific (e.g. the Audit of Diabetes Dependent Quality of Life) instruments to evaluate HRQoL in diabetics. Though diabetes-specific measures are more sensitive and responsive to changes in disease severity, they fall short of providing an overall assessment of the additional negative impact of common comorbidities [9].
The relevance of HRQoL as a major endpoint is not only clinical, but patient-reported outcomes are also employed in health technology assessment and economic evaluations [10]. Preference-based tools are used to measure patient preferences for certain health states, known as utilities [11]. This approach enables the estimation of quality-adjusted life years (QALYs) that incorporate survival (or duration) and HRQoL into a single index providing a major source of guidance to decision makers in many countries [12]. In studies where utility values have not been directly elicited, empirical mapping techniques are a popular remedy. Mapping is defined as “the development and use of a model or algorithm to predict health-related utility values by using data from other measures of health outcomes” [13].
Though there have been many published studies examining HRQoL in T2DM, only a few of them have focused on insulin-dependent T2DM subjects, while also investigating a wide spectrum of comorbidities/complications, in Greece in particular. The primary objective of the present study was to evaluate the impact of comorbidities/complications on HRQoL and health utilities in insulin-treated T2DM.
Subjects, materials and methods
Study design and data collection
This was a non-interventional, epidemiological study. Insulin-treated T2DM patients were recruited from one hospital centre, as the principal investigator site, and 57 private practice centres from various geographical areas of Greece. Adult subjects (≥ 18 years) were enrolled into the study, provided they had given written informed consent. Patients who were not able to participate in the study procedures due to cognitive impairment or had participated in a similar epidemiological study within the previous year were excluded.
No treatment protocol was imposed and patients were treated according to the local summary of product characteristics and routine medical practice. The design was prospective to accomplish all objectives of the study, but HRQoL was evaluated only at the first visit. Data were collected by the physicians primarily from the medical records concerning patient demographics, clinical characteristics and comorbidities/complications and via interviews with the patients for information not documented in the archives.
Patients were required to complete the EQ-5D-5L questionnaire, which is a preference-based generic measure of HRQoL. The EQ-5D is the most commonly used instrument of measuring HRQoL, due to its simplicity and ease of administration [12]. It consists of two components: the EQ-5D-5L descriptive system and the EQ VAS [14]. The EQ-5D-5L descriptive system includes five dimensions of health (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Each dimension is measured across a five-level (5L) scale, with higher levels reflecting more problems, ultimately classifying respondents into 1 of 3.125 distinct health states [14]. The 5L version of EQ-5D-5L was developed in 2005 to improve the instrument’s sensitivity and to reduce the ceiling effects [14–16]. The new questionnaire retained the five-dimensional structure of the original three-level version (3L), however, each dimension now has 5 levels of severity, i.e. no problems, slight problems, moderate problems, severe problems and extreme problems [14, 15]. The EQ VAS measures the respondent’s self-rated health on a 20 cm visual analogue scale with endpoints labelled as “the worst imaginable health” (0) and “the best imaginable health” (100), and it records health status specifically at the time of interviewing [14].
A single utility score can be obtained ranging from − 0.594 to 1.0, with higher scores representing better overall health status [14]. As the Greek value sets have not yet been developed, health utilities were obtained based on time trade-off valuations from a general population study conducted at the United Kingdom [17], which have been generally found to be applicable to the Greek general population and patient groups [14, 18]. Since studies that directly elicit preference-based values from general population samples for the 5L were under development at the time of the analysis, 5L index values were calculated using the indirect method of the crosswalk function provided by the EuroQol Group [19]. Furthermore, there is currently a dispute with health technology assessment agencies concerning the use of the new English 5L value set in economic evaluation [20].
Statistical analysis
Descriptive measures (mean, standard deviation [SD], median, interquartile range [IQR], absolute and relative frequencies) were used to present the demographic, clinical and HRQoL characteristics of the sample.
The univariate associations between health utility (EQ-5D-5L index) and health status (VAS) scores and demographic/clinical factors and comorbidities/complications were assessed using non-parametric Mann–Whitney and Kruskal–Wallis tests, as scores were not normally distributed. The level of severity for each domain of the EQ-5D-5L descriptive system was dichotomized as “no problems” (i.e. level 1) and “problems” (i.e. levels 2–5) to estimate the prevalence of problems in different groups. Differences in the prevalence of problems (proportion of patients) between categories of the covariates were assessed with Chi-squared tests.
Modelling problems in HRQoL descriptive system
Binary logistic regressions were employed to obtain (average) marginal effects as well as odds ratios (ORs) and their 95% bias-corrected and accelerated bootstrap confidence intervals (95% BCA CIs; based on 1000 bootstrap samples) for comorbidities/complications, after adjustment for covariates, with the prevalence of problems in the EQ-5D-5L descriptive system for each HRQoL dimension as dependent variable. The Hosmer–Lemeshow test was used to assess goodness of fit for logistic models, which evaluates whether predicted probabilities agree with observed ones; it should be non-significant for an accurate predictive model [21].
Modelling health utilities
Preliminary analysis
The Spearman’s rank correlation coefficient was applied to covariates to identify possible highly correlated independent variables, which, for this reason, is not recommended to be included simultaneously into the model. A correlation coefficient > |0.7| was considered to signify a high correlation between predictors [22]. Independent variables included: gender, age (years), BMI (kg/m2), duration of diagnosed T2DM (years), duration of insulin treatment (years), HbA1c (%) and history of comorbidities/complications as binary outcomes, i.e. arterial hypertension, coronary artery disease/myocardial infraction, dyslipidemia/hyperlipidemia, stroke, congestive heart failure, peripheral vascular disease/diabetic foot, diabetic neuropathy, diabetic nephropathy, diabetic retinopathy and severe hypoglycemia. Severe hypoglycemic patients were considered to be all subjects with at least one hypoglycemic event requiring hospitalisation or assistance from another person during the previous year. No high correlation between covariates was found, hence, all independent variables could be inserted simultaneously into the models.
Missing data were not imputed, as this introduces an additional source of error related to the imputation method and differences in missing cells are not expected to affect the comparison of randomly split models [23, 24].
Model specification
This mapping analysis aimed to evaluate the relationship between the EQ-5D index and concurrent complications related to insulin-dependent T2DM using regression techniques, ultimately estimating the respective disutilities (i.e. utility decrements). We assumed a simple additive specification for all covariates, including comorbidities, as a previous study has demonstrated the existence of a generally additive rather than a synergistic effect of related to DM conditions on HRQoL [25].
The most common modelling technique used in the literature for mapping health utilities and comorbidities/complications in T2DM is the ordinary least squares (OLS) regression model, which assumes a linear function between EQ-5D index and its predictors [10]. It has been contended that OLS regression analysis is inappropriate for mapping HRQoL for many reasons, especially because OLS has poor predictive ability in both health state extremes (poor and full health), and it does not restrict the predicted value to be always below 1 [22]. Other methods have been proposed, including Tobit and CLAD models, which assume a latent variable that can extend beyond 1, but has been censored at 1. However, these methods inherently do not model health utility, rather the latent construct of HRQoL [26–28]. Furthermore, it has been argued that the assumptions of the Tobit model are unattainable (constant variance and normality of the error term, especially at the upper end of the uncensored measure), while the CLAD estimator models the medians instead of the means, and, in most cases, the marginal Tobit and CLAD coefficients are associated with a high degree of bias [26–28].
Continuous variables were centred to their sample mean, so that the constant coefficient could have a meaningful interpretation. However, a graphical investigation of the relationship between health utilities and covariates revealed a possibly non-linear association. Therefore, we considered examining continuous covariates also as categorical variables and we sought to generate meaningful categories with sufficient number of patients [29]. Eventually, five different specifications were investigated with OLS and were compared to select the best model:
-
1.
OLS1 = Full model (all continuous mean-centred covariates + comorbidities/complications).
-
2.
OLS2 = Significant continuous mean-centred covariates + comorbidities/complications.
-
3.
OLS3 = Full model (categorical covariates + comorbidities/complications).
-
4.
OLS4 = Significant categorical covariates + comorbidities/complications.
-
5.
OLS5 = Significant covariates (specified both as continuous mean-centred and categorical + comorbidities/complications).
For models OLS3, OLS4 and OLS5, we applied a stepwise backward elimination (p value < 0.05 for inclusion and p value > 0.1 for exclusion were the criteria) of the covariates [26, 28]. All complications/comorbidities were forced into all models, because, first, these are the investigated determinants of this paper and, second, it has been suggested that inconsistent results regarding the association between HRQoL and other variables may be attributed to the omission of this type of predictors, since they are considered to be confounder factors [3, 7, 30].
The dataset was randomly divided into two samples: an estimation sample, which was used to estimate the mapping function, and a validation sample, which examined its predictive ability.
Assessment of model performance
Overall performance was assessed via measures of goodness of fit, tests of model specification and internal model validation in the estimation sample, and predictive and discriminative ability in the validation sample. Model goodness of fit was measured using AIC and BIC, with smaller values indicating a better fitted model, and R2 and adjusted R2, where larger values are preferable. Specification was tested with the Ramsey’s RESET test, which investigates whether non-linear combinations of the covariates explain part of the variability; a significant statistic demonstrates the appropriateness of a non-linear model specification [31]. The Pregibon’s link test was also applied to check for a link error in the model; a significant result indicates a misspecification [32].
Models were internally validated by calculating the shrinkage factor, which measures the amount of overfitting generated by the estimated model (similar to the COPAS test), as well as its out- and in-sample predictive bias, as defined by Bilger and Manning [33]. Briefly, out-of-sample shrinkage is caused by both model misspecification and overfitting, in-sample shrinkage arises by model misspecification in the estimation sample, and final shrinkage statistic emerges from overfitting alone. All shrinkage statistics were estimated using repeated tenfold cross-validation, and their means (as percentages) are presented together with their standard errors (SE). A higher shrinkage value indicates greater overfitting of the data.
Predictive ability in the validation sample was assessed with summary statistics (mean, median, SD, 25th and 75th percentiles and range), the mean absolute error (MAE) and the root mean squared error (RMSE) for the whole dataset and across subsets of the range of EQ-5D-5L index values (EQ-5D < 0, 0 ≤ EQ-5D < 0.25, 0.25 ≤ EQ-5D < 0.5, 0.5 ≤ EQ-5D < 0.75, 0.75 ≤ EQ-5D ≤ 1) to determine whether errors were affected by disease severity [13]. Both MAE and RMSE indicate the error between estimated and observed health utility values, and smaller values represent better performance, however, RMSE is more sensitive to extreme deviations. We also computed the proportions of predictions deviating from observed values by less than 0.05, 0.10 and 0.25, since these estimates can show the distribution of errors and how often models fail to produce useful predictions [34, 35].
To assess the discriminative performance of the predictive health utilities in the validation sample, the continuous VAS variable was ranked and categorised into its quartiles. Discriminative ability across groups of health states was assessed using the ANOVA F test, while the means, MAEs and RMSEs were compared between models for each group separately.
Model selection
Across the mapping and model-fitting literature, there is no consensus concerning a single criterion for selecting the best-fitting model [22]. In this analysis, we have opted to assign equal weighting to all model performance statistics used to rank models, with the model exhibiting the best mean ranking being ultimately selected. The best performing model was then re-estimated using the full dataset to increase the precision of the coefficients [13].
The best OLS model specification was also used to assess the determinants of the health state of the sample, as it was measured with the VAS of the EQ-5D-5L.
While OLS coefficients are (asymptotically) unbiased regardless of distributional assumptions, this does not apply also for the statistics derived from the standard errors, such as p values and confidence intervals [27]. OLS estimates coupled with standard errors based on non-parametric bootstrapping are advocated as a valid approach to overcome this issue [28]. Herein, the normal distribution-assumed p values and the 95% BCA CIs (for comparison) based on 1000 bootstrap samples are reported.
Statistical significance level was set at α = 0.05 for all tests, but other levels are reported as well. Analyses were conducted using SPSS v.23 and STATA v.13 [36, 37].
Results
Patients’ characteristics
A total of 938 eligible subjects ultimately joined the study. The mean age of the sample was 67.02 years (± 10.69), with 55.2% being females (Table 1). At baseline, participants had been diagnosed with T2DM for 15.1 years (± 8.19) and had been under insulin treatment for 4.94 years (± 5.35), on average. The vast majority of the sample (88.7%) was afflicted with at least one comorbidity/complication, with arterial hypertension being the most frequently encountered (72.3%). Higher prevalence of difficulties in the EQ-5D descriptive system was observed in the anxiety/depression domain (70.3%), followed by the pain/discomfort (52.2%) and mobility (49.1%) dimensions. The mean EQ-5D index for the sample was 0.713 (± 0.239) and the mean VAS was 67.71 (± 18.39). There appears to be no significant differences in patient characteristics between the randomly splitted datasets.
Univariate associations of HRQoL and utilities
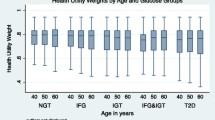
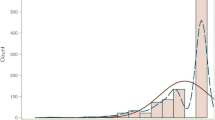
The distribution of the EQ-5D index appears to be roughly trimodal, with one peak at full health, one at around upper-moderate and one at more severe, but well over zero, states being observed (Fig. 1).
Interested readers can find detailed cross-tabulations of the prevalence of problems in the EQ-5D-5L descriptive system and the mean EQ-5D-5L index and VAS scores by demographic and disease-related factors in the Online Resource file (Supplementary Tables 1 and 2). Overall, the female gender, obesity, longer duration of diagnosed T2DM and insulin treatment, poor glycemic control and the presence, multiple in particular, of comorbidities/complications were all associated with more problems (p < 0.05) in all of the EQ-5D-5L descriptive system domains, except for anxiety/depression, where only female gender and comorbidities/complications appear to exhibit a significant negative HRQoL impact. Arterial hypertension, congestive heart failure and severe hypoglycemia were the comorbidities/complications most consistently correlated with higher prevalence of HRQoL problems across the EQ-5D-5L dimensions. Comorbidities/complications primarily impaired the mobility domain, though, notably, the presence of peripheral vascular disease/diabetic foot did not achieve statistical significance. Although more HRQoL problems were reported for this complication, the test was probably not powered enough (n = 26). Again, health utilities and health state were lower with female gender, higher BMI, more time with T2DM and lengthier insulin treatment, poorer glycemic control and the co-existence of other medical conditions (p value < 0.05). All of the comorbidities/complications were associated with a significant reduction in the mean EQ-5D index and VAS scores. However, the decrease did not establish statistical significance in the case of peripheral vascular disease/diabetic foot for both measures.
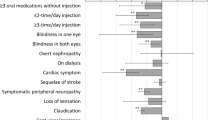
Multivariable adjustment of determinants of HRQoL
The results of the multivariable logistic regression models for each of the five domains of the EQ-5D-5L are displayed in Tables 2 and 3, where the marginal effects and their 95% BCA CIs are reported. The respective estimates of the adjusted ORs can be found in the Online Resource file (Supplementary Table 3). Females were associated with higher probability of reporting at least some problems in all HRQoL domains compared with males. Older patients were more likely to report limitations compared with younger participants in all dimensions except for anxiety/depression, where the increase in the likelihood did not achieve statistical significance. Obesity was correlated with impaired HRQoL in the self-care, usual activities and pain/discomfort domains, in cases with BMI > 35 in particular. The duration of the condition and the length of the insulin treatment did not exert a consistent and significant effect on the prevalence of HRQoL problems. Poorer glycemic control increased the likelihood of reporting problems in all dimensions. Regarding comorbidities/complications, most of them were correlated with more difficulties in all domains, though this negative impact did not establish statistical significance in most cases. Nevertheless, history of severe hypoglycemia was significantly associated with more limitations in all domains apart from mobility and self-care, arterial hypertension was significantly correlated with higher burden in mobility, pain/discomfort and anxiety/depression dimensions, coronary artery disease/myocardial infraction significantly limited mobility and generated pain/discomfort, and, finally, history of stroke significantly impaired the mobility and self-care domains.
Mapping health utilities and health state
Table 4 presents the performance of the OLS models mapping the EQ-5D-5L index and their mean rankings. The estimates of the OLS2 model were omitted, as the results were identical with the OLS1 model. The best-performing model was the OLS3 model, which used the comorbidities/complications along with the categorised continuous covariates. Its R2 (0.256) and adjusted R2 (0.209) is second only to OLS5 and the model was well specified, as suggested by both the RESET and link tests. Its predicted mean (0.725) was higher than in the other estimates, compared with the observed mean (0.713), however, the predicted 25th, 50th and 75th percentiles were the closest or among the closest to the observed values. All models failed to predict full health and negative values, though OLS5 produced the largest range of predictions (0.327–0.993). Furthermore, OLS5 was associated with the lowest MAE (0.172) and the second best RMSE (0.230), also displaying more consistent estimates across the ranges of utility subsets and health states, on average. Still, in general, predictive accuracy was better for higher utilities and health states for all models. Finally, all models were able to discriminate between health states, with the OLS5 producing the second highest F statistic value.
The OLS5 model, which was identified as the best-performing model in the previous analysis, was re-estimated using the full dataset and its specification was also used to evaluate the determinants of the VAS score (Table 5). Females, older participants (> 70 years in particular) and poor glycemic control (HbA1c > 7) were independently associated with lower health utilities. Higher BMI and duration of insulin treatment decreased the EQ-5D-5L index, but not all categories reached statistical significance. After adjustment for other covariates, only arterial hypertension, coronary artery disease/myocardial infraction and severe hypoglycemia established a statistically significant reduction in health utilities. For male subjects, between 18 and 49 years, under-to-normal weight (BMI < 25), with 0–5 years of diagnosed T2DM and 0–5 years of insulin treatment, having controlled condition (HbA1c ≤ 7) and with none of the examined comorbidities/complications, the mean health utility was 0.957. The highest disutility imposed by a comorbidity/complication was predicted for stroke (− 0.082), followed by diabetic retinopathy (− 0.066), diabetic neuropathy (− 0.051), severe hypoglycemia (− 0.050), arterial hypertension (− 0.041), coronary artery disease/myocardial infraction (− 0.038), congestive heart failure (− 0.037), peripheral vascular disease/diabetic foot (− 0.020), diabetic nephropathy (− 0.018) and dyslipidemia/hyperlipidemia (− 0.011).
Finally, regarding the VAS scores, female gender, increased age, BMI and duration of insulin treatment (6–10 years group particularly), lack of control of diabetes and the presence of coronary artery disease/myocardial infraction and diabetic retinopathy compromised significantly the health state of participants.
Discussion
This was a non-interventional, epidemiological study, which aimed to investigate the impact of comorbidities/complications on HRQoL and on health utilities in insulin-treated T2DM in Greece using univariate methods and regression-based adjustments and mapping.
Both the descriptive system and the index of the EQ-5D-5L instrument were able to capture HRQoL decrements associated with typical DM-related concurrent complications. All of the comorbidities/complications assessed were correlated with exacerbated HRQoL problems, decreased health utilities and diminished health state, although the deterioration was not found always to be statistically significant, broadly in accordance with previous findings [7, 38, 39]. Furthermore, not only the type, but also the increasing number of comorbidities/complications was negatively correlated with worsen HRQoL, confirming previous research in both general and diabetic populations [5, 7, 40].
The mean difference in health utilities between diabetics with and without a comorbidity/complication (0.669 vs. 0.821) was comparable to most other published studies, though these surveys did not focus on insulin-treated T2DM subjects, but instead their sample comprised patients under all types of treatment [10, 30, 41–43]. The subgroup of participants without complications were related to a somewhat higher than expected mean health utility, an outcome encountered in most other studies as well, which may be attributed to a healthy survivor effect [44]. This may also indicate that the EQ-5D-5L instrument may not have the capacity to capture important non-health aspects of QoL, as it is not diabetes-specific, and lowered scores may reflect the impact of unrelated comorbidities [30].
History of arterial hypertension, congestive heart failure, stroke, diabetic retinopathy and severe hypoglycemia were univariately associated with the highest increase in the prevalence of problems in the HRQoL domains. After adjustment, comorbidities/complications were found to be significantly associated with poorer HRQoL in different dimensions of the EQ-5D-5L descriptive system: history of arterial hypertension, coronary artery disease/myocardial infraction and stroke in mobility, stroke and severe hypoglycemia in self-care, severe hypoglycemia in usual activities, arterial hypertension, coronary artery disease/myocardial infraction and severe hypoglycemia in pain/discomfort, and arterial hypertension and severe hypoglycemia in anxiety/depression.
Similarly, on the one hand, congestive heart failure, diabetic retinopathy and diabetic neuropathy, and, on the other, congestive heart failure, diabetic retinopathy and severe hypoglycemia exhibited the highest univariate reductions in the mean EQ-5D-5L index and VAS scores, respectively. The final regression models revealed that only arterial hypertension, coronary artery disease/myocardial infraction and severe hypoglycemia for health utilities, and coronary artery disease/myocardial infraction and diabetic retinopathy for health state were significant independent predictors, corroborating the findings of other studies [30, 38, 41, 43, 45, 46]. Despite the EQ-5D-5L index being a function of the score in the dimensions, a significant difference in the mean values does not necessarily imply a significant difference in one or more dimensions [30]. Results concerning hypertension are notable, considering it is mainly an asymptomatic condition that does not exert a negative influence on HRQoL to the same degree as other symptomatic diseases [5, 47]. Nevertheless, hypertension and DM are two intertwined disorders with a significant overlap in underlying risk factors and comorbidities [48].
As expected, all comorbidities/complications exhibited lower utility scores with varying magnitude related to their type. Disutility outcomes considering comorbidities/complications may be interpreted as the mean relative decrement associated with the presence of each comorbidity/complication, in reference to the specific baseline employed in the final regression model. The highest disutilities were associated with the presence of stroke, diabetic retinopathy, diabetic neuropathy and severe hypoglycemia, in decreasing order. The range of the utility reductions varied from 0.011 to 0.082. Values were generally lower than in other studies, as presented in a relatively recent systematic review [10]. This may be due to the simultaneous control of many covariates, as the marginal effect of independent variables is usually dampened when good predictors are added into the regression models [49]. Also, it could be the result of focusing solely on insulin-dependent subjects or it may be explained by other dissimilarities in the main characteristics of the participants, the clinical setting, the range of complications considered and the statistical methods used [43].
Our results suggest a negative HRQoL impact of female gender and increasing age, particularly pronounced among individuals over 70 years, which is a common finding among researchers [7, 50, 51]. It is well established that age is a risk factor for the development of the condition. Also, it has a deleterious effect on several aspects of HRQoL, especially those related to physical functioning, a reduced tolerance to the constraints associated with the condition, and an increased probability of comorbidities [3, 52]. Furthermore, it is generally accepted that men and women with DM face different challenges in the management of the disease and they respond differently to factors related to their health [43, 53].
Also, we confirmed the health and HRQoL benefits associated with good glycemic control, which may reduce the development of major microvascular events, primarily nephropathy, though it is accompanied by an increased risk of severe hypoglycemia [54]. The health and HRQoL benefits of good glycemic control are well established and it has been demonstrated to be crucial in controlling the clinical and economic burden in DM and its related complications [54–58]. Tighter glycemic control may not present tangible immediate improvement in HRQoL and it involves an additional burden, which is the root of non-adherence to treatment. Nevertheless, the literature has suggested an association between diabetic microvascular and macrovascular complications as well as with poor glycemic control, which may also in part explain the positive association of insulin use and HRQoL in several studies [3, 59, 60].
An approximately inversed U-shaped association was found between BMI and health utilities, with the highest mean values located in the group with a BMI score between 25.00 and 29.99. BMI has both a direct effect on HRQoL in subjects with T2DM, through impairment of physical functioning and reduction of energy levels, and an indirect effect, as it is a risk factor for developing T2DM-related complications [43, 60]. The shape of the curve flattened and slightly increased with BMI values over 40, suggesting the existence of a threshold in the detrimental HRQoL impact of obesity or a healthy participant bias [61].
After adjustment for covariates, duration of T2DM did not predict health utilities or health state, suggesting that the commencement of insulin treatment, as an indication of the progression of the condition, is the underlying mark of HRQoL deterioration in insulin-treated patients. In most other studies sampling from the whole T2DM population, duration of the disease retains its independent significance even after adjustment for other covariates, though subjects under insulin treatment usually exhibit considerably lower scores [62]. This implies that, whereas duration of the condition may capture the severity of the disease in the general T2DM population, duration of insulin treatment is a better surrogate for disease development in the insulin-dependent sub-population, which may explain some contradicting findings in the literature [3].
Finally, marginal effects revealed that the highest HRQoL burden was associated with age over 70 years, the female gender, obesity and poor glycemic control, which implies that these were predictors of compromised HRQoL per se, and not only through their links with greater comorbidity.
There were some limitations embedded in the present study that should be noted. First, the design was cross-sectional, which warrants caution for any causal inferences. Furthermore, this non-randomized sample may not be representative of the total Greek insulin-treated T2DM population in certain aspects, such as socioeconomic and clinical characteristics, and type of treatment. Also, the sample size for some concurrent complications was relatively small, which entails low statistical power, and may explain the non-significant results [30].
Though we did incorporate many important covariates as suggested in the relevant literature, the non-inclusion of some unrecorded and potentially useful clinical or sociodemographic characteristics of participants that influence HRQoL in our analysis, such as socioeconomic status, could have possibly biased our results. Furthermore, the current study was performed at only one point in time and fluctuations are likely to be observed if HRQoL is measured at multiple points in time [39, 49]. Also, the HRQoL impact of clinical events may change over time or in relation to the number of the events and the severity of the condition, and our study did not collect data for these parameters [27, 43, 44]. In any case, it is broadly recommended that if the intention of the mapping study is to have a wider use of the results, then it should incorporate only explanatory covariates that are most commonly collected in relevant studies [13]. The relatively low goodness of fit results may be indicative of the possible omission of other important covariates and confounders, though our R2 results are analogous to most published studies on HRQoL in T2DM.
Also, the EQ-5D instrument may not be adequate to discriminate between all comparisons or treatment modalities in T2DM, which may partly explain the non-significant results of certain comorbidities/complications [7, 43]. Therefore, the use of EQ-5D-5L in conjunction with a DM-specific instrument could have provided a better understanding and be more responsive to changes in HRQoL scores between the groups compared [63]. Finally, lacking a Greek EQ-5D-5L tariff, we used the UK tariff based on TTO to calculate the health utilities, which is the most commonly used globally [30]. Nevertheless, our estimates may not be as accurate as they would have been if a Greek tariff had been applied. Therefore, we emphasize the need for a national algorithm and the development of a Greek value set, especially considering that recently a Health Technology Assessment process has been introduced for the first time in Greece [64]. Once the Greek value set is available, future studies should revisit our estimates.
In conclusion, we have corroborated the detrimental impact of comorbidities/complications on insulin-dependent T2DM subjects’ HRQoL. Better management of the disease may prevent or delay the progression of comorbidities/complications, alleviating the HRQoL impairment related to DM, and clinicians should adapt the priorities of DM interventions accordingly. Overall, the most important determinants of impaired HRQoL were found to be higher age, female gender, obesity, poor glycemic control and history of stroke, diabetic retinopathy, diabetic neuropathy and severe hypoglycemia. Furthermore, to our knowledge, this is the first Greek study that derives a set of health utility estimates associated with multiple insulin-treated T2DM-related comorbidities/complications. It has been suggested that it is important to select as many utility values as possible from a single study for internal consistency reasons [10], hence these estimates may be valuable for conducting economic evaluations of interventions in the area of T2DM. Other statistical techniques, such as two-part models, splining, limited dependent variable mixture models and response mapping could provide an efficient alternative approach to estimation of disutilities, and future research should explore the relative merits.
References
Whiting, D.R., Guariguata, L., Weil, C., Shaw, J.: IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res. Clin. Pract. 94(3), 311–321 (2011)
Fonseca, V.: Defining and characterising progression of type 2 diabetes. Br J Diab Vasc Dis 8, S3 (2008)
Rubin, R.R., Peyrot, M.: Quality of life and diabetes. Diabetes Metab. Res. Rev. 15(3), 205–218 (1999). https://doi.org/10.1002/(sici)1520-7560(199905/06)15:3%3c205:aid-dmrr29%3e3.0.co;2-o
International Diabetes Federation.: IDF Diabetes Atlas. International Diabetes Federation. http://www.idf.org/diabetesatlas (2013). Accessed 17 Jan 2018
O’Shea, M.P., Teeling, M., Bennett, K.: Comorbidity, health-related quality of life and self-care in type 2 diabetes: a cross-sectional study in an outpatient population. Ir. J. Med. Sci. (2014). https://doi.org/10.1007/s11845-014-1190-4
National Institute for Health and Clinical Excellence.: Clinical Guideline 87: Type 2 diabetes: the management of type 2 diabetes. http://www.nice.org.uk/guidance/ta203/resources/nice-recommends-liraglutide-for-type-2-diabetes-mellitus4. (2009). Accessed 17 Jan 2018
Kontodimopoulos, N., Pappa, E., Chadjiapostolou, Z., Arvanitaki, E., Papadopoulos, A.A., Niakas, D.: Comparing the sensitivity of EQ-5D, SF-6D and 15D utilities to the specific effect of diabetic complications. Eur. J. Health Econ. 13(1), 111–120 (2012). https://doi.org/10.1007/s10198-010-0290-y
Ali, S., Stone, M., Skinner, T.C., Robertson, N., Davies, M., Khunti, K.: The association between depression and health-related quality of life in people with type 2 diabetes: a systematic literature review. Diabetes/Metab. Res. Rev. 26(2), 75–89 (2010)
Anderson, R.M., Fitzgerald, J.T., Wisdom, K., Davis, W.K., Hiss, R.G.: A comparison of global versus disease-specific quality-of-life measures in patients with NIDDM. Diabetes Care 20(3), 299–305 (1997)
Beaudet, A., Clegg, J., Thuresson, P.-O., Lloyd, A., McEwan, P.: Review of utility values for economic modeling in type 2 diabetes. Value Health 17(4), 462–470 (2014)
Torrance, G.W., Furlong, W., Feeny, D.: Health utility estimation. (2002).
Glasziou, P., Alexander, J., Beller, E., Clarke, P.: Which health-related quality of life score? A comparison of alternative utility measures in patients with Type 2 diabetes in the ADVANCE trial. Health Qual. Life Outcomes 5(5), 21 (2007)
Longworth, L., Rowen, D.: Mapping to obtain EQ-5D utility values for use in NICE health technology assessments. Value Health 16(1), 202–210 (2013)
Yfantopoulos, J.N., Chantzaras, A.E.: Validation and comparison of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in Greece. Eur. J. Health Econ. 18(4), 519–531 (2017)
Rabin, R., Oemar, M., Oppe, M., Janssen, B., Herdman, M.: EQ-5D-5L User Guide: Basic information on how to use the EQ-5D-5L instrument. Version 1.0. EuroQol Group, Rotterdam (2011)
Herdman, M., Gudex, C., Lloyd, A., Janssen, M.F., Kind, P., Parkin, D., Bonsel, G., Badia, X.: Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 20(10), 1727–1736 (2011). https://doi.org/10.1007/s11136-011-9903-x
Dolan, P., Gudex, C., Kind, P., Williams, A.: A social tariff for EuroQol: results from a UK general population survey. CHE Discussion Paper. Centre for Health Economics, York (1995)
Yfantopoulos, J., Chantzaras, A., Kontodimas, S.: Assessment of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in psoriasis. Arch. Dermatol. Res. (2017). https://doi.org/10.1007/s00403-017-1743-2
Van Hout, B., Janssen, M.F., Feng, Y.S., Kohlmann, T., Busschbach, J., Golicki, D., Lloyd, A., Scalone, L., Kind, P., Pickard, A.S.: Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 15(5), 708–715 (2012). https://doi.org/10.1016/j.jval.2012.02.008
Yang, F., Devlin, N., Luo, N.: Cost-utility analysis using EQ-5D-5L data: does how the utilities are derived matter? Value Health 22(1), 45–49 (2019). https://doi.org/10.1016/j.jval.2018.05.008
Hosmer Jr, D.W., Lemeshow, S., Sturdivant, R.X.: Applied logistic regression, 3rd ed. Wiley, Hoboken, NJ (2013)
Longworth, L., Yang, Y., Young, T., Mulhern, B., Hernandez Alava, M., Mukuria, C., Rowen, D., Tosh, J., Tsuchiya, A., Evans, P., Devianee Keetharuth, A., Brazier, J.: Use of generic and condition-specific measures of health-related quality of life in NICE decision-making: a systematic review, statistical modelling and survey. Health Technol. Assess. (Winchester, England) 18(9), 1–224 (2014). https://doi.org/10.3310/hta18090
Kent, S., Gray, A., Schlackow, I., Jenkinson, C., McIntosh, E.: Mapping from the Parkinson’s disease questionnaire PDQ-39 to the Generic EuroQol EQ-5D-3L: the value of mixture models. Med. Decis. Making 35(7), 902–911 (2015). https://doi.org/10.1177/0272989X15584921
Chuang, L.H., Kind, P.: Converting the SF-12 into the EQ-5D: an empirical comparison of methodologies. PharmacoEconomics 27(6), 491–505 (2009). https://doi.org/10.2165/00019053-200927060-00005
Wee, H.-L., Cheung, Y.-B., Li, S.-C., Fong, K.-Y., Thumboo, J.: The impact of diabetes mellitus and other chronic medical conditions on health-related Quality of Life: is the whole greater than the sum of its parts? Health Qual. Life Outcomes 3(1), 2 (2005)
Pullenayegum, E.M., Tarride, J.-E., Xie, F., O’Reilly, D.: Calculating utility decrements associated with an adverse event marginal Tobit and CLAD coefficients should be used with caution. Med. Decis. Mak. 31(6), 790–799 (2011)
O’Reilly, D.J., Xie, F., Pullenayegum, E., Gerstein, H.C., Greb, J., Blackhouse, G.K., Tarride, J.-E., Bowen, J., Goeree, R.A.: Estimation of the impact of diabetes-related complications on health utilities for patients with type 2 diabetes in Ontario, Canada. Qual. Life Res. 20(6), 939–943 (2011)
Pullenayegum, E.M., Tarride, J.E., Xie, F., Goeree, R., Gerstein, H.C., O’Reilly, D.: Analysis of health utility data when some subjects attain the upper bound of 1: are Tobit and CLAD models appropriate? Value Health 13(4), 487–494 (2010)
Quah, J.H., Luo, N., Ng, W.Y., How, C.H., Tay, E.G.: Health-related quality of life is associated with diabetic complications, but not with short-term diabetic control in primary care. Ann. Acad. Med. Singap. 40(6), 276 (2011)
Solli, O., Stavem, K., Kristiansen, I.: Health-related quality of life in diabetes: the associations of complications with EQ-5D scores. Health Qual. Life Outcomes 8(1), 18 (2010)
Ramsey, J.B.: Tests for specification errors in classical linear least-squares regression analysis. J. R. Stat. Soc. Ser. B (Methodological) 31(2), 350–371 (1969)
Pregibon, D.: Data analytic methods for generalized linear models. Ph.D. Dissertation, University of Toronto (1979)
Bilger, M., Manning, W.G.: Measuring overfitting in nonlinear models: a new method and an application to health expenditures. Health Econ. 24(1), 75–85 (2015)
Dakin, H., Petrou, S., Haggard, M., Benge, S., Williamson, I.: Mapping analyses to estimate health utilities based on responses to the OM8-30 Otitis Media Questionnaire. Qual. Life Res. 19(1), 65–80 (2010). https://doi.org/10.1007/s11136-009-9558-z
Khan, K.A., Madan, J., Petrou, S., Lamb, S.E.: Mapping between the Roland Morris Questionnaire and generic preference-based measures. Value Health 17(6), 686–695 (2014)
IBM Corp.: IBM SPSS Statistics for Windows. IBM Corp., Armonk (2015)
StataCorp: Stata Statistical Software. StataCorp LP, College Station (2013)
Venkataraman, K., Wee, H.L., Leow, M.K., Tai, E.S., Lee, J., Lim, S.C., Tavintharan, S., Wong, T.Y., Ma, S., Heng, D., Thumboo, J.: Associations between complications and health-related quality of life in individuals with diabetes. Clin. Endocrinol. (Oxf) 78(6), 865–873 (2013). https://doi.org/10.1111/j.1365-2265.2012.04480.x
Javanbakht, M., Abolhasani, F., Mashayekhi, A., Baradaran, H.R., Jahangiri noudeh, Y.: Health related quality of life in patients with type 2 diabetes mellitus in Iran: a national survey. PloS one 7(8), e44526 (2012). https://doi.org/10.1371/journal.pone.0044526
Sepúlveda, E., Poínhos, R., Constante, M., Pais-Ribeiro, J., Freitas, P., Carvalho, D.: Relationship between chronic complications, hypertension, and health-related quality of life in Portuguese patients with type 2 diabetes. Diabetes, Metab. Syndr. Obes. Targets Ther. 8, 535 (2015)
U.K. Prospective Diabetes Study Group: Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). Diabetes Care 22(7), 1125–1136 (1999)
Matza, L.S., Boye, K.S., Yurgin, N., Brewster-Jordan, J., Mannix, S., Shorr, J.M., Barber, B.L.: Utilities and disutilities for type 2 diabetes treatment-related attributes. Qual. Life Res. 16(7), 1251–1265 (2007). https://doi.org/10.1007/s11136-007-9226-0
Kiadaliri, A.A., Gerdtham, U.-G., Eliasson, B., Gudbjörnsdottir, S., Svensson, A.-M., Carlsson, K.S.: Health utilities of type 2 diabetes-related complications: a cross-sectional study in Sweden. Int. J. Environ. Res. Public Health 11(5), 4939–4952 (2014)
Clarke, P., Gray, A., Holman, R.: Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med. Decis. Mak. 22(4), 340–349 (2002)
de Visser, C.L., Bilo, H.J., Groenier, K.H., de Visser, W., Jong Meyboom-de, B.: The influence of cardiovascular disease on quality of life in type 2 diabetics. Qual. Life Res. 11(3), 249–261 (2002)
Coffey, J.T., Brandle, M., Zhou, H., Marriott, D., Burke, R., Tabaei, B.P., Engelgau, M.M., Kaplan, R.M., Herman, W.H.: Valuing health-related quality of life in diabetes. Diabetes Care 25(12), 2238–2243 (2002)
Miksch, A., Hermann, K., Rolz, A., Joos, S., Szecsenyi, J., Ose, D., Rosemann, T.: Additional impact of concomitant hypertension and osteoarthritis on quality of life among patients with type 2 diabetes in primary care in Germany—a cross-sectional survey. Health Qual Life Outcomes 7, 19 (2009). https://doi.org/10.1186/1477-7525-7-19
Long, A.N., Dagogo-Jack, S.: The comorbidities of diabetes and hypertension: mechanisms and approach to target organ protection. J. Clin. Hypertens. (Greenwich, Conn.) 13(4), 244–251 (2011). https://doi.org/10.1111/j.1751-7176.2011.00434.x
Alva, M., Gray, A., Mihaylova, B., Clarke, P.: The effect of diabetes complications on health-related quality of life: the importance of longitudinal data to address patient heterogeneity. Health Econ. 23(4), 487–500 (2014)
Kontodimopoulos, N., Pappa, E., Niakas, D., Yfantopoulos, J., Dimitrakaki, C., Tountas, Y.: Validity of the EuroQoL (EQ-5D) instrument in a Greek general population. Value Health 11(7), 1162–1169 (2008)
Papadopoulos, A.A., Kontodimopoulos, N., Frydas, A., Ikonomakis, E., Niakas, D.: Predictors of health-related quality of life in type II diabetic patients in Greece. BMC Public Health 7(1), 186 (2007). https://doi.org/10.1186/1471-2458-7-186
Tan, M.C., Ng, O.C., Wong, T.W., Hejar, A.R., Anthony, J., Sintonen, H.: The association of cardiovascular disease with impaired health-related quality of life among patients with type 2 diabetes mellitus. Singap. Med. J. 55(4), 209 (2014)
Grant, J.F., Hicks, N., Taylor, A.W., Chittleborough, C.R., Phillips, P.J.: Gender-specific epidemiology of diabetes: a representative cross-sectional study. Int. J. Equity Health 8(1), 6 (2009)
Patel, A., MacMahon, S., Chalmers, J., Neal, B., Billot, L., Woodward, M., Marre, M., Cooper, M., Glasziou, P., Grobbee, D., Hamet, P., Harrap, S., Heller, S., Liu, L., Mancia, G., Mogensen, C.E., Pan, C., Poulter, N., Rodgers, A., Williams, B., Bompoint, S., de Galan, B.E., Joshi, R., Travert, F.: Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N. England J. Med. 358(24), 2560–2572 (2008). https://doi.org/10.1056/NEJMoa0802987
Stratton, I.M., Adler, A.I., Neil, H.A., Matthews, D.R., Manley, S.E., Cull, C.A., Hadden, D., Turner, R.C., Holman, R.R.: Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321(7258), 405–412 (2000)
Brown, A., Reynolds, L.R., Bruemmer, D.: Intensive glycemic control and cardiovascular disease: an update. Nat. Rev. Cardiol. 7(7), 369–375 (2010)
The Diabetes Control and Complications Trial Research Group: The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 329, 977–986 (1995)
Testa, M.A., Simonson, D.C.: Health economic benefits and quality of life during improved glycemic control in patients with type 2 diabetes mellitus: a randomized, controlled, double-blind trial. J. Am. Med. Assoc. 280(17), 1490–1496 (1998). https://doi.org/10.1001/jama.280.17.1490
UK Prospective Diabetes Study Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). The Lancet 352(9131), 837–853 (1998)
Zhang, P., Brown, M.B., Bilik, D., Ackermann, R.T., Li, R., Herman, W.H.: Health utility scores for people with type 2 diabetes in US managed care health plans results from Translating Research Into Action for Diabetes (TRIAD). Diabetes Care 35(11), 2250–2256 (2012)
Whitehurst, D.G.T., Bryan, S., Lewis, M.: Systematic review and empirical comparison of contemporaneous EQ-5D and SF-6D group mean scores. Med. Decis. Mak. 31(6), E34–E44 (2011). https://doi.org/10.1177/0272989X11421529
Bourdel-Marchasson, I., Druet, C., Helmer, C., Eschwege, E., Lecomte, P., Le-Goff, M., Sinclair, A.J., Fagot-Campagna, A.: Correlates of health-related quality of life in French people with type 2 diabetes. Diabetes Res. Clin. Pract. 101(2), 226–235 (2013). https://doi.org/10.1016/j.diabres.2013.05.011
Wong, C., Lo, Y., Wong, W., Fung, C.: The associations of body mass index with physical and mental aspects of health-related quality of life in Chinese patients with type 2 diabetes mellitus: results from a cross-sectional survey. Health Qual Life Outcomes 11(1), 142 (2013)
Yfantopoulos, J.N., Chantzaras, A.: Drug policy in Greece. Value Health Reg. Issues 16, 66–73 (2018). https://doi.org/10.1016/j.vhri.2018.06.006
Acknowledgements
The authors would like to thank two anonymous reviewers for their helpful comments that contributed to improving the final version of the paper.
Funding
No funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yfantopoulos, J., Chantzaras, A. Health-related quality of life and health utilities in insulin-treated type 2 diabetes: the impact of related comorbidities/complications. Eur J Health Econ 21, 729–743 (2020). https://doi.org/10.1007/s10198-020-01167-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-020-01167-y