Abstract
This study examines the changes in marginal revenue during psychiatric inpatient stays in a large Swiss psychiatric hospital after the introduction of a mixed reimbursement system with tariff rates that vary over length of stay. A discrete time duration model with a difference-in-difference specification and time-varying coefficients is estimated to assess variations in policy effects over length of stay. Among patients whose costs are fully reimbursed by the mixed scheme, the model demonstrates a significant effect of marginal revenue on length of stay. No significant policy effects are found among patients for whom only health insurance rates are delivered as mixed tariffs and government contributions are made retrospectively. The results indicate that marginal revenue can affect length of stay in inpatient psychiatry facilities, but that the reduction in marginal revenue must be sufficiently large.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of prospective payment systems for inpatient psychiatry is increasing internationally. Prospective payment systems reimburse care by predetermined rates regardless of actual costs. In inpatient care, prospective payment systems typically include a patient classification system and per-case payments to establish incentives for the efficient provision of care. Patient classification systems aim to form homogeneous cost groups with tariff rates close to actual costs to reduce incentives for the under- or over-provision of services to patients with above or below average costs. Per-case payments are intended to reduce length of stay by decreasing marginal revenue per inpatient day. A disadvantage of per-case payments is that they deviate more from the actual cost per episode than revenues from a per diem system, which are adjusted for observed length of stay. The introduction of a per-case reimbursement system thus creates a trade-off between the accuracy of tariff rates and incentives to reduce the average length of stay. The accuracy of tariff rates is a critical issue in inpatient psychiatry, in which length of stay varies substantially within cost groups [1–6].
Many studies have investigated the effect of per-case payment on length of stay in inpatient psychiatry (for a review see Chalkley and Malcomson [7]). The early results stem from evaluations of the U.S. Medicaid and Medicare payment reforms. Frank and Lave [8] explored variations in the manner in which state Medicaid programs reimbursed psychiatric care between 1981 and 1984. They found that the average length of a stay in inpatient psychiatry was lower under per-case prospective payment systems than with cost-based reimbursement. Freiman et al. [9] documented a reduction in the length of stay for psychiatric patients treated in acute care hospitals after the 1984 Medicare prospective payment reform. The effect, which was greatest during the first months of the new system, began before it even came into effect, indicating anticipatory behavior by hospitals. An evaluation of the 1989 New Hampshire Medicaid payment reform by Ellis and McGuire [10] showed significant reductions in the average length of stay of psychiatric patients, but increased length of stay for short episodes. The authors interpreted this result as evidence of quality competition among hospitals for profitable patients, as postulated by Dranove and White [11]. A second explanation for the increase in length of stay for short episodes was provided by Norton et al. [12], who analyzed the responsiveness of length of stay to changes in marginal and average revenue per inpatient day in the cross-section. Their results suggest that providers of inpatient psychiatric care did not respond to changes in marginal revenue, but only to changes in average revenue per inpatient day, which was higher for short episodes. The absence of a marginal price effect has important policy implications: it means that a switch from per diem to per-case reimbursement reduces the accuracy of the tariff rates and leads to over- and under-treatment, but does not necessarily establish incentives to reduce average length of stay.
This study examines the decrease in marginal revenue after the switch from a per diem system to a mixed reimbursement system in a large psychiatric hospital in the Swiss canton of Zurich. The evaluated mixed system consists of a high per diem rate during the first 5 days of a stay, a per-case payment on day 6, and a low per diem rate thereafter. The objective of this study is to test whether the payment reform affected length of stay by altering the marginal or average revenue per inpatient day.
Background
During the observation period of this study (between 2008 and 2011), the cost of inpatient psychiatric care in the Swiss canton of Zurich was assumed in roughly equal amounts by private health insurance companies and the government. Prior to 2009, health insurance companies paid their share of the cost in the form of per diem rates, which differed among hospitals, resulting from negotiations between hospitals and health insurance companies. At that time, the delivery mode for government contributions depended on the patient’s canton of residence. The canton of Zurich made retrospective annual payments to hospitals; however, other cantons reimbursed the costs of their residents who were treated in the canton of Zurich in the form of per diem rates.Footnote 1 These tariff rates from other cantons were intended to cover the expected cost per inpatient day after subtracting health insurance rates. At the time of this study, no patient classification system has been implemented.
In 2009, the health administration of the canton of Zurich introduced a mixed reimbursement system to the state-run Psychiatric University Hospital of Zurich (hereafter, “intervention hospital”) while all other hospitals in the canton of Zurich (hereafter, “comparison hospitals”) remained in the traditional per diem system.Footnote 2 In the new mixed system, tariff payments made by health insurance companies consisted of a high per diem rate for the first 5 days of a stay, a per-case payment on day 6, and a low per diem rate for subsequent days (Table 1).Footnote 3 The canton of Zurich continued to make retrospective global payments based on the deficits of the prior year. However, government contributions for stays of residents from other cantons were also delivered in the form of a mixed tariff, with a per-case payment on day 6 and a low per diem rate thereafter. As a consequence, the costs of residents from the canton of Zurich were reimbursed using mixed health insurance rates and retrospective government contributions while the costs of residents from other cantons were fully reimbursed by the mixed scheme.
In the comparison hospitals, health insurance companies reimbursed the cost of care in the form of per diem rates for the entire observation period of this study. Hospitals with a reimbursement agreement received government contributions from the canton of residence of each patient. Hospitals without reimbursement agreements did not receive government contributions. The delivery mode of the government contributions made to comparison hospitals was dependent on the canton of residence of each patient. The canton of Zurich made annual payments while government contributions by other cantons were delivered as per diem rates. Tariff rates and government contributions differed among comparison hospitals due to negotiations between the hospitals, health insurance companies, and the canton of Zurich.
Hypotheses
According to Cutler [13], a switch from cost-based to prospective payment can affect length of stay by altering the marginal and average revenue per inpatient day. The decrease in marginal revenue alone creates an incentive for the provider to reduce length of stay because each inpatient day increases cost, but not revenue. Such a marginal price effect only occurs if physicians have preferences for hospital profit [14–16]. A second mechanism through which per-case payment can affect length of stay is average revenue per inpatient day or, equivalently, total revenue per episode. An average price effect occurs when physicians have preferences for medical benefit of their patients and use the available resources to maximize the quality of care under the constraint of non-negative profits. Physicians, who are imperfect agents of their patients, react to changes in marginal revenue because these changes affect the utility maximizing length of stay, and they react to changes in average revenue because these changes determine the maximum length of stay associated with non-negative hospital profit. In this model, a change in average revenue affects an imperfect agent’s choice only if the profitability constraint is binding, i.e. if the maximum affordable length of stay is shorter than the agent’s utility-maximizing choice.
The research question of this study is whether the switch from per diem to mixed reimbursement affected length of stay in the intervention hospital by altering the marginal or average revenue per inpatient day. The payment reform left the revenue during the first 5 days essentially unchanged. On day 6, the per-case payment increased the average revenue per inpatient day while the reduction in per diem rates decreased the marginal revenue. Total revenue per episode increased on day 6, but was lower than in the old per diem system after 36 or 40 days, depending on the canton of residence.Footnote 4 In a homogeneous patient population, with a constant marginal cost per inpatient day, a per diem tariff must yield non-negative profits for an infinite number of days to allow the provision of a positive amount of care without losses. This assumption suggests that the profitability constraint was not binding before the reform and its loosening did not affect length of stay. Therefore, I do not expect the increase in average revenue between days 6 and 36 (or 40) to affect length of stay in this interval, but only later, when the profitability constraint was tighter than it was previously. However, the decrease in average revenue after day 36 (or 40) did not necessarily increase the incentive to discharge patients because the profitability constraint was relaxed by retrospective government financing. Because the government of the canton of Zurich covered the deficits from the treatment of both Zurich and non-Zurich residents, the opportunity to treat a patient who yielded a negative profit did not depend on the canton of residence. However, the marginal price effect should not be affected by retrospective government financing because a decrease in marginal revenue per inpatient day reduces the utility maximizing length of stay regardless of total profit. Based on the information provided above, I hypothesize that the introduction of the mixed Zurich system produced the following effects:
-
Marginal price effect the decrease in marginal revenue on day 6 increases the probability of discharge.
-
Average price effect the decrease in average revenue after day 36 (non-Zurich residents) or day 40 (Zurich residents) increases the probability of discharge.
-
Heterogeneity in response the effects of the payment reform are larger among non-Zurich residents, for whom both the health insurance rates and government contributions were subject to the reform.
Empirical strategy
This study exploits the introduction of the mixed Zurich system in only one hospital; all other hospitals remained in the traditional per diem system. The unaffected hospitals serve as a comparison group to control for a counterfactual situation in a difference-in-difference framework. Because the marginal and average price effects of the payment reform are expected to manifest at different time points during inpatient stays, a duration model with time-varying coefficients is estimated. A change in the shape of the hazard curve over specified intervals is regarded as evidence of a marginal or average price effect.
Because the length of stay (los) of psychiatric patients is recorded in discrete intervals of days, a discrete time duration model is estimated. The discrete time hazard rate \(\lambda (t)\) is defined as the conditional probability that an event would occur during time period t, given that it had not yet occurred [17].
The hazard rate h(t) can be estimated as the probability of discharge \(P(\mathrm{discharge}_{t}=1)\) at time t by a discrete choice model in a dataset containing one observation per inpatient day. The dependent binary variable (\(\mathrm{discharge}_{t}\)) indicates whether a patient is discharged on day t. A link function specifies the dependence of the hazard on predictors and time. Commonly used link functions for discrete time duration models are probit, logit, and complementary log–log. This study uses the complementary log–log specification, as shown in Eq. (2), which is the discrete time counterpart of continuous time proportional hazards models [18]. Complementary log–log models are a popular choice for grouped continuous time variables because the coefficients are the same as the coefficients from the corresponding continuous time proportional hazards model [19, 47], and the coefficients are invariant to the length of the discrete time intervals [20]. Complementary log–log models invoke the proportional hazards assumption, whereas logit models depend on the proportional odds assumption, which is less well integrated into the survival time theory. Although logit and complementary log–log functions yield similar results when hazards are low, a logit link is also tested in sensitivity analyses.
To test the formulated hypotheses, each inpatient episode is characterized by predictors of the hazard rate during time period t. Let \(D_{i}\) be a binary variable indicating whether an episode was recorded at the intervention hospital, and let \(T_{i}\) be an indicator of admission during the post-intervention period (after January 1, 2009). The interaction term \(D_{i}T_{i}\) captures the exposure to the payment reform.
Because this study focuses on the effect of the mixed Zurich system on the shape of the hazard function, the treatment effect is allowed to vary over length of stay using an interaction term between the \(D_{i}T_{i}\) term and interval dummies \(I_{6+}\), \(I_{36+}\), \(I_{40+}\) and \(I_{60+}\); in accordance with the proposed hypotheses, the interval dummies indicate whether an inpatient day is observed later than day 6, day 36, day 40, or day 60, respectively. With such a backward difference coding, the treatment effect in an interval is compared with the effect in the prior interval. This model describes the effect of the payment reform on within-spell variation in the hazard rate, not only a proportional shift.
Indicator variables for hospitals in the comparison group \(H_{i}\) and indicators of the quarter of admission \(Q_{i}\) counted from January 1, 2008, are used to control for hospital and quarterly fixed effects. The time dependence of the probability of discharge is controlled for by piecewise constant baseline hazards \(B_{t}\). The piecewise baseline hazards are estimated in daily intervals for the first 2 weeks, in 2-day intervals during days 15–28, in weekly intervals between days 29 and 63, in monthly intervals from day 64 to day 183, and in quarters thereafter.
In this non-linear difference-in-difference model the marginal price effect of the payment reform on the hazard rate is not identified by the coefficient \(\mu _{t}\), but by its incremental effect \(h_{i}^{1}(t)-h_{i}^{0}(t)\) at a given day [21]. Because the incremental effect of \(\mu _{t}\) on the hazard rate is only positive if \(\mu _{t}\) is positive one can still interpret the sign of the coefficient \(\mu _{t}\) [22].
The empirical model identifies the marginal and average price effects of the payment reform by examining changes in the shape of the hazard curve under the following assumptions. The first assumption is that the shape of the hazard curves in the intervention and comparison hospitals would have similarly changed in the absence of the payment reform. Differing shapes of the hazard curves before the policy reform and deviating trends in overall length of stay do not affect the estimates as long as the shape of the hazard curves follows a common trend. Under the common trend assumption, an endogenous treatment assignment that is based on pre-intervention outcomes also does not affect the parameter estimates. Unfortunately, the assumption of a common trend in the shape of the hazard curves cannot be tested using only one pre-intervention year. However, it seems plausible that the hazard curves would follow the same general trend because all of the analyzed hospitals operate in the same geographically small jurisdiction and adhere to the same regulations.
The second critical assumption of the difference-in-difference strategy is the absence of anticipatory responses to the policy reform. The health administration of the canton of Zurich announced the policy reform only four months before it came into effect, making anticipatory effects unlikely.
The third assumption is that the marginal costs per inpatient day were unaffected by the payment reform and remained constant throughout the length of stay. If the physicians had responded to the payment reform by reducing the intensity of care, a decrease in marginal and average revenue per inpatient day would not transform into the same decrease in marginal and average profit per inpatient day. The decrease in average revenue could create incentives for physicians with preferences for patient benefit to reduce marginal costs and maintain the length of stay for patients who primarily need time in a protected environment. However, the decrease in marginal revenue is not expected to increase the incentive to reduce marginal costs because physicians with preferences for hospital profit could have increased the hospital profit by reducing marginal costs even before the payment reform. Unfortunately, the policy effects on marginal costs per inpatient day cannot be examined because no data regarding these costs of care are available.
If the marginal costs per inpatient day decreased over the length of stay, the effects of the changes in marginal and average revenue on marginal and average profit per inpatient day would depend on the length of stay. When the patterns of marginal costs over the length of stay differ between patients, the payment reform could show heterogeneous policy effects. However, the variation in the marginal costs over the length of stay is not an obstacle to the identification strategy of this study because a change in marginal and average revenue transforms into an identical change in marginal and average profit per inpatient day as long as the patterns did not change after the payment reform.
The effects of the payment reform on the hazard rate can be affected by three types of endogeneity. First, the intervention hospital could have diverted more high-cost patients to outpatient care or day care facilities. Such a response would create a sample selection bias that cannot be corrected because no information about these outpatient or day care cases is available. Second, the intervention hospital could have diverted high-cost patients to other psychiatric hospitals. Altered patient selection leading to shifts between hospitals is controlled for by using an extensive set of patient characteristics as covariates in the sensitivity analysis. Early discharges to other hospitals are not excluded because patients cannot be identified across hospitals and the focus of this study is on the incentives created by the payment reform in the intervention hospital regardless of each patient’s destination after discharge. Third, the results may be affected by dynamic selection because only those patients who remain hospitalized can experience changes in marginal and average revenue. The use of patients’ individual characteristics as covariates in the sensitivity analysis should also control for the heterogeneity in the baseline hazard.
Data
The primary data source analyzed in this study is the PSYREC registry, a database of all inpatient episodes in 13 psychiatric hospitals in the canton of Zurich between 2008 and 2012. The PSYREC registry contains information about patient characteristics, diagnoses, therapies, and clinical assessments of functioning and symptom severity.
The variable of interest in this study is the length of psychiatric inpatient stays in days. Non-reimbursable therapeutic leaves during a stay are not counted as days spent in the hospital. The patient identification numbers in the PSYREC registry allow the identification of readmissions to the same hospital, but not to other hospitals. Inpatient episodes in different hospitals, therefore, cannot be attributed to specific patients.
Together with the mixed Zurich system, the health administration of the canton of Zurich introduced a new definition for treatment episodes in the intervention hospital. Beginning on January 1, 2009, readmissions within 30 days after the last discharge from the intervention hospital were reimbursed as a treatment continuation after a non-reimbursable therapeutic leave. To allow a comparison between the intervention hospital and the comparison hospitals and to obtain a consistent picture over time, I apply this definition to all the episodes in the dataset and connect readmissions to the same hospital within 30 days to the previous episode. This strategy leads to a reduction in the number of spells and an increase in the average length of stay compared with other publications using the PSYREC registry data.
For this study, only data from patients 18 to 65 years of age at admission were available. The sample includes only completed spells of 365 days or less with an admission date between February 1, 2008, and December 31, 2011. I do not consider the period between January 1 and January 31, 2008, in this analysis to ensure that after recoding readmissions within 30 days as continuations of previous stays, all studied episodes begin during the observation period. The year 2012 is excluded because hospital financing was reformed in the entire country that year.
Results
Descriptive statistics
Between 2008 and 2011, there were 10,644 inpatient episodes that fulfill the inclusion criteria described in Sect. 5 in the intervention hospital and 24,794 inpatient episodes in the comparison hospitals (Table 2). The intervention hospital is a large provider of psychiatric inpatient care in the canton of Zurich and provides care to approximately 30 % of all psychiatric patients. The vast majority of the patients treated in the included hospitals lived in the canton of Zurich. In 2008, residents of the canton of Zurich constituted 95.30 % of the patients in the intervention hospital and 89.50 % in the comparison hospitals.
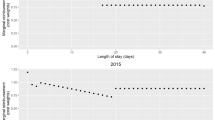
The average length of stay was shorter in the intervention hospital than in the comparison hospitals during the entire observation period, although it followed a similar trend (Fig. 1). Both groups exhibited an increase from 2008 to 2009, followed by a steady decline until 2011. Compared with the year 2008, the average post-intervention length of stay was 0.83 days shorter in the intervention hospital and 0.90 days shorter in the comparison hospitals (Table 2).
The observed density of length of stay exhibited a different pattern in the intervention hospital than in the comparison hospitals (Fig. 2). A much greater proportion of patients were discharged from the intervention hospital during the first 5 days of hospitalization. The peak on day 5 shown in Fig. 2 can be explained by the standard “crisis intervention” package, which lasts for exactly 5 days, provided in the intervention hospital. The higher proportion of episodes lasting 2, 3, or 4 days could be a consequence of early discharges from crisis intervention. Unfortunately, the data does not allow to identify cases treated using crisis intervention. However, in the regression analysis, the initial difference in the shape of the hazard curves between the intervention and comparison hospitals is controlled for using piecewise constants and should not pose a threat to the empirical approach of this study. In addition, the use of individual characteristics as covariates in the sensitivity analysis controls for the differing patient populations in the intervention and comparison hospitals.
In 2008, the patient populations of the intervention and comparison hospitals exhibited different characteristics. The intervention hospital accommodated more patients of foreign nationalities, fewer patients with supplementary private insurance plans and fewer patients undergoing compulsory hospitalization. The proportions of cases of psychotic disorders (ICD-10 F2) and disorders in childhood and adolescence (ICD-10 F9) were higher, and the proportion of cases of affective disorders (ICD-10 F3) was lower than in the comparison hospitals. The intervention hospital has a long tradition in the treatment of schizophrenia and still specializes in this field.
The descriptive statistics presented in Table 2 also reveal some changes in the patient population of the intervention hospital between the pre- and post-intervention periods. The proportion of patients with mandatory schooling decreased from 22.25 to 11.07 %, and the proportion of patients with an apprenticeship declined from 26.21 to 20.53 %. These reductions in the number of patients with low educational status accompany an increase in the number of records with unknown educational status from 26.90 to 44.34 %. The proportion of patients with a paid job decreased from 40.79 to 29.44 % in the intervention hospital, but increased slightly from 36.49 to 37.99 % in the comparison hospitals. After the payment reform the combined proportion of patients with a main diagnosis of a psychotic (ICD-10 code F2) or affective disorder (ICD-10 code F3) increased from 42.93 to 50.61 %, while the proportion of patients with a disorder occurring in childhood and adolescence (ICD-10 F9) decreased from 7.97 to 0.81 %. The intervention hospital appears to have become even more specialized in the treatment of schizophrenia than before the payment reform. The frequency of patients undergoing compulsory hospitalization increased markedly from 1.39 to 5.93 % in the intervention hospital but decreased from 6.45 to 4.04 % in the comparison hospitals. The illness severity at admission, which was measured using the Clinical Global Impression Scale (CGI), shifted toward lower severity in the intervention hospital.
Some of the observed changes in patient characteristics may be the consequence of revised coding practices. The lower severity ratings, the higher proportion of jobless patients, and the altered distribution of main diagnoses, however, may indicate altered patient selection after the switch from per diem to mixed reimbursement. A model with covariates from Table 2 is, therefore, estimated to examine the effects of compositional changes in the patient population. The increase in the number of compulsory hospitalizations is unlikely to be a consequence of altered patient selection because these admissions are primarily initiated by an adult protection authority representative who also has input into the decisions regarding the patient’s discharge.
Regression results
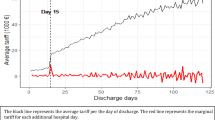
A regression analysis is used to test whether the payment reform changed the shape of the hazard curve over the length of stay in the intervention hospital. The coefficient of the interaction term \(\mathrm{treat}\times \mathrm{post}\) gives a difference-in-difference estimate of the policy effect on the probability of discharge during the first 5 days of inpatient episodes. This coefficient alone cannot be interpreted in a non-linear model because the marginal effect of the payment reform in this interval depends on the expected outcome of each patient and is not constant across the treated group [21, 22]. The coefficient of the multiple interaction \(\mathrm{treat}\times \mathrm{post}\times I_{6+}\) indicates the increase in the treatment effect after day 6 compared with the first 5 days. This coefficient demonstrates how the payment reform changed the shape of the hazard curve on day 6. The positive coefficient of 0.6322 (\(p\ <\ 0.005\)) in the group of non-Zurich residents is interpreted as evidence of a marginal price effect of the payment reform on length of stay. In the group of Zurich residents, however, this coefficient is close to zero and shows no marginal price effect. The coefficients of the interaction terms \(\mathrm{treat}\times \mathrm{post}\times I_{40+}\) (Zurich residents) and \(\mathrm{treat}\times \mathrm{post}\times I_{36+}\) (non-Zurich residents) indicate whether the probability of discharge increased after day 40 or day 36 compared with the earlier days of inpatient episodes, which could be interpreted as an average price effect. The analysis does not reveal a significant change in the treatment effect in this time interval, thus providing no evidence of an average price effect. The decrease in the probability of discharge after day 60 does not necessarily represent an effect of the mixed tariff system because the per diem rates in the comparison hospitals and the pre-intervention rates in the intervention hospital also decreased after day 60 (Table 1).
A prediction of the hazard functions of the post-intervention episodes in the intervention hospital and the counterfactual functions of the same episodes, without the treatment effect, allow a graphical representation of the regression results (Fig. 3). For this exercise, I simulate the treatment effect for the second quarter of 2009, which had the smallest quarterly fixed effect. The hazard curves of Zurich residents are predicted to be essentially unaffected by the policy reform. The hazard curves of non-Zurich residents, however, exhibit a pronounced change in shape.
Robustness tests
The robustness tests that are performed include a specification with covariates, a comparison between the complementary log–log function and the logit link function, and two subgroup analyses. The short pre-intervention period does not allow a test of the vital common trend assumption. A finer temporal resolution would provide too few observations per period, particularly in the group of non-Zurich residents.
Model with covariates
A model with covariates is estimated to determine whether the results are influenced by compositional changes in the patient populations or by dynamic selection over length of stay. When the patient characteristics listed in Table 2 are controlled for, the standard errors in the non-Zurich sample become smaller, and the sizes of the coefficients increase slightly (Table 3). The coefficient of the interaction term \(\mathrm{treat}\times \mathrm{post}\times I_{6+}\), however, does not change considerably, indicating that the base case results are not biased by patient selection or by “spurious” duration dependence because of unobserved heterogeneity [23, p. 64]. Unfortunately, the effect of unobserved heterogeneity cannot be tested using a complementary log–log model with gamma frailty because the likelihood function cannot be maximized in specification (2).
Alternative link function
The complementary log–log link function seems particularly appropriate for the problem at hand because the dependent variable is a grouped continuous time variable [19]. An alternative specification with a logit link function is estimated to examine whether the results are sensitive to the choice of the link function. As shown in Table 3, this is not the case; the results are similar in both estimations.
Subgroup analyses
The results of this study are in contrast to the findings of Norton et al. [12], who did not find a marginal price effect among patients with schizophrenia and affective disorder. A subgroup analysis by main diagnosis at discharge could reveal whether this selection of patients could explain some of the differences between my results and those of Norton et al. [12]. Indeed, the estimation among non-Zurich residents with psychotic and affective disorders (ICD-10 codes F2 and F3) produces smaller coefficients for the shift after day 6, indicating that the marginal price effect is weaker in this patient group (Table 4).
A second subgroup analysis by the severity of illness, measured using the global clinical impression (CGI) at admission as a proxy for cost per day, is performed.Footnote 5 Patients with scores between 1 and 4 are classified as moderate cases, and those with scores above 5 are considered to be severe cases. According to the model estimates in Table 5 and the graphs in Fig. 4, the marginal price effect among non-Zurich residents is stronger in moderately ill patients. This result indicates that the payment reform does not disproportionately affect patients with greater needs.
Predicted hazard functions of post-intervention spells in the intervention hospital vs. counterfactual hazard functions by severity of illness. a Full sample: severe cases. b Full sample: moderate cases. c Zurich residents: severe cases. d Zurich residents: moderate cases. e Non-Zurich residents: severe cases. f Non-Zurich residents: moderate cases
Discussion
At a time when many countries are implementing prospective payment systems for inpatient psychiatry, this study produced some interesting policy-related findings. The results indicate that the marginal revenue per inpatient day can affect length of stay and that a switch from per diem to per-case or mixed reimbursement can reduce length of stay even if the average revenue remains similar.
A significant change in the shape of the hazard curve is found only for the subgroup of non-Zurich residents, for whom the payments by both the health insurance companies and the government were delivered as mixed tariff rates. No effect is found in the subgroup of Zurich residents for whom only health insurance rates were subject to the payment reform, and government contributions were delivered as retrospective annual payments based on accumulated losses. The difference between the Zurich and non-Zurich residents suggests that the decrease in marginal revenue must be sufficiently large to establish incentives to reduce length of stay. A small change in marginal revenue may not be a strong incentive, for example, when the management and optimization of patients’ length of stay is costly. Another possible explanation for the heterogeneity in response is that simultaneous retrospective government financing could function as a disincentive for improving operational efficiency. The retrospective government financing mechanism may also be responsible for the lack of evidence of an average price effect because this mechanism allows hospitals to make negative profits if they have medical motives for treating patients longer than the tariffs allow.
The subgroup analysis produces larger estimates of the marginal price effect among moderately ill non-Zurich residents and smaller estimates among the severely ill. A stronger marginal price effect among the less severe cases suggests that the motive to make a financial profit is stronger in the treatment of moderately ill patients, whereas the motive to create medical benefit is relatively stronger in the treatment of severely ill patients. This interpretation could allay concerns that a switch to a prospective payment system particularly harms patients with greater needs.
This study also reveals differences between diagnostic subgroups. The estimated effect of the decrease in marginal revenue is smaller among the patients with psychotic (ICD-10 F2) and affective (ICD-10 F3) disorders. If this observation is generally valid, it might explain the difference between the results of this study and those of Norton et al. [12], who did not find evidence of a marginal price effect. One possible interpretation of the effect heterogeneity across diagnostic subgroups is quality competition for profitable patients. Because the intervention hospital specializes in the treatment of psychotic disorders, it may be more efficient in the treatment of these cases and could respond less markedly to the payment reform compared with cases of other diagnostic groups.
The heterogeneity of the effects underlines the need for an accurate patient classification in prospective payment systems. Considering that per-case payments come at the price of a higher deviation of tariff rates from actual costs, the per-case component of a mixed tariff could be higher in more homogeneous cost groups, in which the per-case payments are closer to actual costs, and in moderately ill patients, in which incentives for a reduction in length of stay are more effective.
The empirical model uses variations in marginal and average revenue over length of stay to test for the presence of marginal and average price effects. In the special case of the mixed Zurich system, which has a per-case payment on day 6 and a lower per diem rate thereafter, the marginal price effect is measured by testing for changes in the shape of the hazard curve over specified intervals. The difference-in-difference approach controls for the initial difference in the shape of the hazard curve between the intervention and comparison hospitals and identifies the policy effects according to different changes in the shape of the hazard curves. The use of an extensive set of patient characteristics as control variables in the sensitivity analysis showed that the results are not affected by altered patient selection as a reaction to the payment reform.
Note that this analysis has some limitations. The first and major limitation is that, with only one pre-intervention year, I cannot examine the pre-intervention trends to support the vital common trend assumption. Second, the identification of the average price effect is based on the assumption that the marginal costs per inpatient day were unaffected by the payment reform. If physicians reduced the intensity of care to maintain length of stay, the decrease in average revenue might not lead to a decrease in length of stay. However, the marginal price effect should not be affected by such a quality-quantity substitution as the increase in total profit resulting from a decrease in marginal costs is the same under both reimbursement systems. Third, I do not analyze the effects of the payment reform on readmission rates or on the total number of inpatient days. However, the simultaneous policy regulation stipulating that readmissions to the intervention hospital within 30 days should be reimbursed as a continuation of the previous stay may have partially offset the incentives to increase the number of cases. Future research should shed more light on the effects of the payment reform on readmissions and the total number of inpatient days. Fourth, the analysis does not inform the reader about the effects of the payment reform on the overall length of stay or destination after discharge. The non-linear model does not identify the marginal price effect on overall length of stay and the length of stay in the intervention hospital may underestimate the duration of inpatient care per disease episode if patients are discharged to other hospitals. Unfortunately, the data do not allow identifying patients across hospitals and analyzing discharges made to other hospitals. However, the focus of this study is on the incentives created by changes in marginal and average revenue per inpatient day in the intervention hospital; both of these factors are independent of the destination after discharge. Fifth, this study cannot estimate the exact elasticities of the length of stay with respect to marginal revenue in the cross-section because the comparison hospitals cannot be identified for legal reasons and no tariff rates can be attached to the inpatient episodes. A comparison between the presented duration approach and the elasticities estimated in the cross-section might produce some interesting methodological insights.
Notes
Between 2008 and 2011, the following cantons had reimbursement agreements with the canton of Zurich that allowed their residents to be treated in Zurich hospitals: Appenzell-Innerhoden, Appenzell-Auserrhoden, Glarus, Graubünden, St. Gallen, Schaffhausen, Thurgau, and Zug. Patients from other cantons or from abroad had to pay the government share themselves.
According to staff of the health administration of the canton of Zurich the intervention hospital was selected because it was a state run hospital and because it treated a typical patient population. The comparison group also included state-run hospitals.
As an example, a stay of 20 days in the intervention hospital was reimbursed by health insurance with \(20 \times 309=6180\) in 2008, and \(3062 + 5 \times 356 + 15 \times 217 = 8097\) in 2009.
An episode of a non-Zurich resident of 36 days was reimbursed by health insurance and the government with \(36\times 803=28{,}908\) in 2008, and with \(7720 + 5\times 897 + 31 \times 546 = 29{,}131\) in 2009. The revenue from health insurance for a stay of a Zurich resident of 40 days was \(40 \times 309 = 12{,}360\) in 2008, and \(3062 + 5 \times 356 + 35 \times 217 = 12{,}437\) in 2009.
The CGI rating is an overall assessment of symptom severity by the treating physician; its scores range from 1 (normal, not at all ill) to 7 (extremely ill).
References
Ashcraft, M.L.F., Fries, B.E., Nerenz, D.R., Falcon, S., Srivastava, S.V., Lee, C.Z., Berki, S.E., Errera, P.: A psychiatric patient classification system: an alternative to diagnosis-related groups. Med. Care 27(5), 543–557 (1989)
Siegel, C., Alexander, M.J., Lin, S., Laska, E.: An alternative to drugs: a clinically meaningful and cost-reducing approach. Med. Care 24(5), 407–417 (1986)
Warnke, I., Rössler, W., Herwig, U.: Does psychopathology at admission predict the length of inpatient stay in psychiatry? Implications for financing psychiatric services. BMC Psychiatry 11(1), 120 (2011)
Hunter, C.E., McFarlane, A.C.: DRGs and Australian psychiatry. Aust. N. Z. J. Psychiatry 28(1), 114–120 (1994)
Taube, C., Lee, E.S., Forthofer, R.N.: Drgs in psychiatry: an empirical evaluation. Med. Care 22(7), 597–610 (1984)
Drozd, E., Cromwell, J., Gage, B., Maier, J., Greenwald, L., Goldman, H.: Patient casemix classification for medicare psychiatric prospective payment. Am. J. Psychiatry 163(4), 724–732 (2006)
Chalkley, M., Malcomson, J.M.: Government purchasing of health services. In: Culyer AJ, Newhouse JP (eds) Handbook of Health Economics, vol. 1, chap. 15, pp. 847–890. Elsevier, Amsterdam (2000)
Frank, R.G., Lave, J.R.: A comparison of hospital responses to reimbursement policies for medicaid psychiatric patients. Rand J. Econ. 20(4), 588–600 (1989)
Freiman, M.P., Ellis, R.P., McGuire, T.G.: Provider response to medicare’s PPS: reductions in length of stay for psychiatric patients treated in scatter beds. Inquiry 26, 192–201 (1989)
Ellis, R.P., McGuire, T.G.: Hospital response to prospective payment: moral hazard, selection, and practice-style effects. J. Health Econ. 15(3), 257–277 (1996)
Dranove, D., White, W.D.: Recent theory and evidence on competition in hospital markets. J. Econ. Manag. Strategy 3(1), 169–209 (1994)
Norton, E.C., Van Houtven, C.H., Lindrooth, R.C., Normand, S.L.T., Dickey, B.: Does prospective payment reduce inpatient length of stay? Health Econ. 11(5), 377–387 (2002)
Cutler, D.M.: The incidence of adverse medical outcomes under prospective payment. Econom. J. Econom. Soc. 63(1), 29–50 (1995)
Ellis, R.P., McGuire, T.G.: Provider behavior under prospective reimbursement: Cost sharing and supply. J. Health Econ. 5(2), 129–151 (1986)
Ellis, R.P., McGuire, T.G.: Optimal payment systems for health services. J. Health Econ. 9(4), 375–396 (1990)
McGuire, T.G.: Physician agency and payment for primary medical care. In: Glied, S., Smith, P.C. (eds.) The Oxford Handbook of Health Economics, chap. 25, pp. 602–623. Oxford University Press Inc., New York
Singer, J.D., Willett, J.B.: It’s about time: using discrete-time survival analysis to study duration and the timing of events. J. Educ. Stat. 18(2), 155–195. ISSN 03629791 (1993)
Beck, N., Katz, J.N., Tucker, R.: Taking time seriously: time-series-cross-section analysis with a binary dependent variable. Am. J. Polit. Sci. 42(4), 1260–1288 (1998)
Kalbfleisch, J., Prentice, R.: The statistical analysis of failure time data. In: Applied Probability and Statistics. Wiley Series in Probability and Mathematical Statistics. Wiley, New York (2002). ISBN: 9780471055198
Allison, P.D.: Discrete-time methods for the analysis of event histories. Sociolog. Methodol. 13, 61–98 (1982). ISSN: 00811750
Ai, C., Norton, E.C.: Interaction terms in logit and probit models. Econ. Lett. 80(1), 123–129 (2003)
Puhani, P.A.: The treatment effect, the cross difference, and the interaction term in nonlinear difference-in-differences models. Econ. Lett. 115(1), 85–87 (2012)
Lancaster, T.: The econometric analysis of transition data. In: Econometric Society Monographs. Cambridge University Press, Cambridge (1992). ISBN: 9780521437899
Acknowledgments
I am very grateful to Claude Jeanrenaud, Per Johansson, and Simon Wieser for their support and guidance. Carsten Colombier, Peter Zweifel, Maarten Lindeboom, Jürgen Maurer, Alberto Holly, Mark Dusheiko, and other participants of the Swiss Health Economics Workshop and the SSPH+ PhD seminar provided useful comments. I also thank the two anonymous reviewers whose comments helped improve and clarify this manuscript. All errors are my own.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There are no current external funding sources for this study.
Conflict of interest
The author declares that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Pletscher, M. Marginal revenue and length of stay in inpatient psychiatry. Eur J Health Econ 17, 897–910 (2016). https://doi.org/10.1007/s10198-015-0735-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-015-0735-4