Abstract
Obesity poses important burdens not only on the individuals whose quality of life is reduced but on national welfare systems that have to face growing premature mortality rates, increase healthcare expenditures to treat obesity-related diseases, and earmark vast amounts of healthcare resources for prevention. The main goal of this paper is to analyze the relationship between excess body weight and different dimensions of health-related quality of life for people 16 years and older and to identify the health dimensions most affected by excess weight. We have drawn data from the Catalonia Health Survey (2006). Our results reveal a relationship between excess weight and health-related quality of life. Even after controlling for socio-economic status and objective health variables, excess weight is shown to have a significant negative effect on health-related quality of life. Subjects responses revealed that the negative effect of excess weight was felt the strongest in the health-related quality of life dimensions of mobility and pain/discomfort. Our results indicate there are important differences among gender and age groups. Women and older people are more likely to suffer from the negative consequences of excess weight.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity and overweight generate a considerable loss of potential life years and quality-adjusted life years lost (QALYs), in addition to direct and indirect costs. Direct costs of obesity and overweight include inpatient and outpatient care, rehabilitation and nonmedical costs. Indirect costs are huge and wide ranging: sick days, sick leave, early retirement and mortality, among others [1–7].
Against this background, there is no doubt that obesity is a challenge for public health authorities in many countries. The World Health Organization (WHO) has focused attention on the growing rate of people who are overweight or obese, and has labeled the situation as an epidemic [8]. Furthermore, prevalence among children has grown over the last 20 years to the extent that their figures mirror those of the adult population [9]. National and international health authorities are presently faced with the two-pronged task of designing effective strategies to deal with the negative consequences of obesity for today’s society and to curb its ill effects in the future.
Although figures on the prevalence of overweight and obesity vary depending on the source consulted (WHO, International Obesity Task Force, etc.), they all concur in that the rate of overweight or obesity among populations in wealthy countries is on the rise. In Europe, the prevalence has tripled in the last two decades. It was estimated that if measures were not taken, by 2010, 150 million adults (20% of the population) and 15 million children and adolescents (10% of the population), would be obese in the European region of the WHO, Spain being no exception [10–12]. The National Survey of Health carried out in Spain in 2006 indicates that 38 and 16% of the adult population, and 19 and 9% of children, are overweight and obese, respectively.
Although there are several ways of defining and measure obesity, the most usual is to present a body mass index (BMI) above 30 kg/m2. This situation would represent a strong risk factor for illnesses such as type 2 diabetes, coronary artery disease, neurological disease, gastrointestinal disease and tumors (prostate and colon cancer in men and breast, uterine, ovarian and endometrial cancer in women). Although heated controversy has arisen as to the number of deaths than can be attributed to obesity due to issues concerning methodologies assessing causality and risk factors [13–15], estimates by Banegas et al. [16] place the number of deaths in the European Union (UE-15) in 1997 attributable to excess weight between 279,000 and 401,000 (8% of total deaths). An analysis carried out by the Swedish National Institute of Public Health concluded that in the European Union, 4 and 1% of Quality-Adjusted Life Years are lost because of obesity and a lack of physical activity. In other words, a total of 5% compared to 9% attributable to smoking [17].
Several studies carried out on the general population have focused on Health-Related Quality of Life (HRQOL) in obese people [18–22] finding that people with overweight and obesity have lower HRQOL than people with a normal body weight.
In Spain, there is no strong evidence linking obesity to HRQOL. Spain is a Mediterranean country that has a high number of hours of sunlight and good weather (climatic conditions that are favorable to exercise) and a special diet (the Mediterranean diet), considered to be one of the key factors explaining the increased longevity among the Spanish population. However, over the last two decades, Spain has become one of the countries where the obesity epidemic has grown most rapidly, and the rates in children are of particular concern. In Spain, there is no strong evidence linking obesity to HRQOL. Aside from the study carried out by López–García et al. [23], for people 60 years old and older, no studies have been carried out on the relationship between quality of life and excess weight in Spain. The main goal of this article is to analyze the relationship between excess body weight and different dimensions of health-related quality of life for people 16 years and older and to identify the health dimensions most affected by excess weight.
Methods
Study subjects and data source
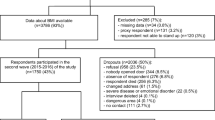
We have drawn 9,226 observations from the Health Survey of Catalonia (ESCA). The ESCA participants were residents of Catalonia who were not undergoing hospitalization at the time the survey was conducted. Subjects had spent most of the years residing in family dwellings that were their habitual or permanent residences. Data were collected and analyzed by territorial division.
The ESCA used the EQ–5D, which consists of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. HRQOL is measured on three levels in regard to functional state (no health problems, some health problems and extreme health problems), resulting in 243 aggregate combinations. Participants were surveyed on the five dimensions of EQ–5D and each observation was translated to a single health score using the Spanish time trade-off (TTO) value set [24, 25]. The Spanish value set have scores ranging from –0.653 to 1, where 1 corresponds to a perfect state of health and 0 corresponds to death.
Explanatory variables are provided on socio-economic characteristics (gender, age, Spanish nationality, marital status, level of education, employment status and income level), risk factors arterial hypertension, diabetes mellitus, high cholesterol), BMI and diagnosed diseases (vascular illness, rheumatic disease, digestive illness, mental illness, osteomuscular disease) and undergoing hospitalization. The weight/height classification was determined using a commonly accepted method, whereby individuals with a BMI lower than 18.5 were considered underweight, individuals with a BMI between 18.5 and 24.9 kg/m2 were considered normal weight, between 25 kg/m2 and 29.9 kg/m2 were overweight and a BMI equal to or exceeding 30 kg/m2, were classified as obese. Persons in this latter group were further classified as having obesity that was either class I (30 kg/m2 ≤ BMI < 35 kg/m2) or class II or III (BMI ≥ 35 kg/m2) [24]. Underweight subjects were excluded due to their low number and distinct behavior pattern.
Given both the recent literature demonstrating gender and age differences in HRQOL [19, 26–28] and recent debate on whether estimations should include comorbidity variables as explanatory factors [5], we carry out additional analyses by gender and by gender and age (Age1: 15–44 years old; Age2: 45–64 years old; Age3: 65 years old or older). As obesity is a risk factor for a large number of diseases, excluding these variables would mean that the estimated effect of obesity on HRQOL might include the influence of omitted illnesses, so the parameter of obesity might be overestimated. On the other hand, including them could in fact result in an underestimation of the impact of obesity on HRQOL because to some degree it would have already been included in the diagnosed disease. In our main analysis, we have opted to provide estimations twice, with and without diagnosed diseases. The importance of this empirical strategy is twofold. Firstly, we will obtain a range of the impact of overweight and obesity on HRQOL. Secondly, we will observe how robust the results are.
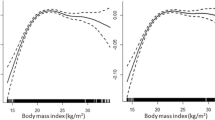
The empirical framework was selected based on the nature of the endogenous variables. We use the ordinary least square technique (OLSQ) for analyzing the relationship between HRQOL (values from the Spanish TTO based on the EQ–5D value set) and BMI. Additionally, we define each EQ–5D dimension (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) as dichotomous variables that takes the value 1 if the individual has suffered from any problem related to each dimensions, and 0 otherwise. We carry out five independent probit estimations, one for each dimension.
The estimation design of HRQOL (i indexes individuals) is summarized as follows:
HRQOL i indicates individual self-perception of health, SocioDemo i is a vector of socio-demographic characteristics (gender, age, Spanish nationality, marital status, level of education, employment status and income level), BodyWeight i control for body weight with four dummy variables (Normal weight, Overweight, Obesity1 (30 ≤ BMI < 35) and Obesity2 (BMI ≥ 35), Normal weight being the reference variable), Diseases i is a vector of diagnosed problems (vascular illness, rheumatic disease, digestive illness, mental illness, osteomuscular disease and undergoing hospitalization) and ν i is a zero-mean disturbance term. The key parameter of interest is φ because in absence of technical problems, such as endogeneity or unobserved heterogeneity, it provides information on the causal effect of body weight on an individual’s self-perception of health. The fundamental challenge in using observational data to estimate φ is the possibility that even after controlling for observed characteristics, the unobserved determinants (ν i ) may vary with the health factor BodyWeight i . Our initial response to this challenge is simple: we repeat estimations including and excluding a very rich set of observed characteristics of diagnosed health problems (Diseases i ). Within the conceptual economic framework, and in light of the insights of other social science research, it is natural to expect that diagnosed health problems are important determinants of both HRQOL i and BodyWeight i . For example, people with osteomuscular problems may be more likely to report excess weight and to perceive their state of health as worse. Controlling for a range of diagnoses health problems reduces unobserved heterogeneity and improves our estimates of φ. However, we are also aware that including these variables in the estimations introduces a severe problem of endogeneity. We do not analyze the estimated parameters of these variables because they may reflect bias. The importance of this strategy lies on the fact that if the estimation of φ is robust, its value will not vary significantly for the variables we consider in the model. At the same time, we will be also able to define intervals with minimum and maximum values of the estimated parameters, depending we include or exclude Diseases i.
Following this structure and taking into account the dichotomous nature of the EQ–5D dimensions, the estimation of EQ–5D dimensions (i indexes individuals and j indexes each one of the five domains) is defined as it follows:
EQ–5D* ij indicates the unobserved propensities to suffer from any problem included in the health-related quality of life survey (EQ–5D). As mentioned above, the key parameters of interest are δj because they provide information on the causal effect of body weight on the dimension j of the EQ–5D. Based on the same line of reasoning, we employ the same empirical strategy with and without the vector Diseases i .
Results
The sample contains an equal number of men and women. Distribution by age is as follows: 47% between 15 and 44 years old, 29% between 45 and 64 years old, and 24% older than 64 years old. A descriptive analysis of means by age and gender reveal that women and older people give themselves a lower score for health and report more health problems than men and younger people. For example, 9 and 16% of men and women aged between 15 and 44 years old suffer from anxiety or depression compared to 16 and 40% of men and women older than 64 years old. Moreover, the data also reveals that gender differences are markedly greater for older population groups. Regarding BMI, women and younger people control their weight better than men and older people. For example, 37 and 19% of men and women aged between 15 and 44 years old are overweight versus 51 and 41% of men and women older than 64 years old (see Table 1).
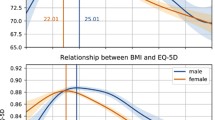
Table 2 shows the OLSQ estimated coefficients of BodyWeight for HRQOL, where Normal weight is the reference category. Results from Table 2 reveal statistically significant differences in health-related quality of life for women with normal weight in relation to their overweight and obese counterparts. Excess weight is negatively correlated with self-perception of health, and more importantly, the greater the excess weight, the worse is the self-perception of health. For men, there is only empirical evidence that obese men perceive their health worse than men with normal weight. Gender differences reveal that excess weight is a stronger predictor of self-perceived health for women than for men. In addition, excess weight has an increasing negative effect on women’s health according to age group. After adjusting for Diseases, the magnitudes of estimated coefficients lose intensity and significance, as would be expected. Intensity ranges drop by between one-third and one half of the previous estimated parameters. Results show strong differences to women with normal weight to obese women, and men with normal weight to men with chronic problems of obesity. When estimations by age and gender subpopulation group are repeated, results remain statistically significant for women, whereas for men only two (out of nine) coefficients are statistically significant. Estimations for females by age group confirm that the negative influence of excess weight on self-perception of health increases with the age of the woman. This empirical evidence loses strength when we control for Diseases. (See Table 2).
Table 3 completes earlier results. The dimension most strongly association with excess weight was mobility, followed by pain/discomfort. For example, overweight women and men are 8 and 2% more likely than their normal weight counterparts to suffer from mobility problems. The percentages increase to 29 and 19% when we compare obese men and women with their normal weight counterparts. Empirical evidence also points to a positive correlation between excess weight and other problems of EQ–5D for women (in order of importance: anxiety/depression, problems related to daily life activities and self-care problems), whereas for men there is near no additional empirical significance. Estimations with the vector Diseases and by age population group change results in the same manner as for HRQOL. (See Table 4).
Conclusions and discussion
The study of the Spanish case is relevant because not even the occurrence of positive environmental factors, such as Mediterranean diet and weather, have stopped the international tendency of adopting lifestyles that promote obesity. In fact, Spain has become one of the countries where the obesity rates have grown most rapidly, especially among children.
The results of this study support a significant inverse relationship between BMI and HRQL. Our empirical results are not only statistically significant, but given the magnitudes of the negative effect of overweight and obesity on the quality of life, they are also clinically important. Our results confirm that the loss of health-related quality of life is clearly correlated with obesity, and this correlation is magnified in the case of women and the elderly. The observed changes in HRQOL are much higher than the values often cited in international literature as the minimal clinically important difference where responder definitions for the EQ–5D TTO ranged from 0.074 to 0.08 [29, 30]. Results that are statistically and clinically significant might be robust enough to serves as the basis for health policies that benefit general population groups. In addition, obesity is associated with significant worsening in the EQ–5D dimensions relating to mobility and pain/discomfort, and may be associated with problems with performing usual activities and mental problems (anxiety/depression), especially among women.
The negative association between excess weight and HRQOL is stronger and more significant for women than for men. For women, there is also empirical evidence that excess weight influences the self-perception of health more in older women than in their younger counterparts. Many problems derived from overweight and obesity might not be perceived as painful at early stages of life as at later stages, and the decline may be especially true for women. Among women, obesity contributes to a more rapid and serious deterioration in the EQ–5D dimensions related to mobility and pain/discomfort. It may also be associated with mental problems (anxiety/depression) and/or problems in performing usual activities. Consequently, elderly women represent a vulnerable population group [31–33]. One plausible explanation for this result may be that at postmenopausal ages, certain health diagnosed problems, but also undiagnosed, (such as bone decalcification, muscle loss or inflammatory problems) get worse with overweight. For instance, in the elderly, decreased muscle mass (sarcopenia) and increased fat mass (obesity) may contribute to get worse physical functions [34]. Compared with women with a healthy body composition, obese women were more likely to experience difficulties with most of the physical functions assessed [35]. Moreover, the skeletal muscle mass adjusted for both height and body weight was a significant predictor of mobility limitation in a large sample of elderly men and women, where limitations were shown to be more intense for women [36]. A similar case can be made for the concurrence of obesity and the storage of excess fat in tissues other than adipose tissue, including liver and skeletal muscle tissues, which can lead to local insulin resistance or stimulate inflammation. Obesity-induced inflammatory changes in adipose tissue and liver support the growing recognition that obesity is characterized by a state of chronic low-level inflammation [37]. In spite of these explanations, the reasons for gender differences in the self-reported assessment of functional limitations are very complex. Studies may need to consider men and women separately, because how BMI relates to function is tied to gender [38]. Further research is needed to evaluate how changes in weight and body composition during middle and old age affect functional status.
It is worth bearing in mind that the effects of obesity are to a great extent manifest in the illnesses for which it is a risk factor, and when the effects of these illnesses are controlled for statistically, it is assumed that the effect of obesity on HRQOL for the given illness may be “watered down” or underestimated. Nevertheless, it is noteworthy that even after controlling for the mentioned illnesses, in the case of women, obesity exhibits a clear negative and significant association with perceived health. Our results are consistent with HRQOL studies on populations in different countries [22, 23, 39], where the association between obesity and quality of life is always significant and negative for women. In men, the significance is lower. Nevertheless, when we remove the statistical control on the effect of diagnosed diseases, there obesity still has a significant and negative effect on HRQOL, even in men.
Although the negative effects on quality of life are greatest among the elderly, children and adolescents are the usual targets of policy makers. Health prevention policies aim to reduce the prevalence of obesity among children for two reasons: on one hand, obese children tend to be obese adults [40, 41], and on the other hand, obesity during adolescence is positively correlated with health problems in adulthood. In addition, the growing rate of childhood obesity is not a trend limited to Spain, but is also seen in other European countries and even worldwide [42], which is why the conclusions of this study may be of international interest. Lessons might be drawn from the experiences of other countries that started to address the problem of high obesity rates before Spain. For example, health information and communication strategies can enhance population awareness about the benefits of healthy eating and physical activity; fiscal measures can promote the adoption of healthy diet recommendations by increasing the price of unhealthy foods and reducing the cost of healthy foods rich in fiber; and regulatory measures, such restricting children’s access to unhealthy foods at schools, might have a positive influence on their state of health when they become adults [43]. With this in mind, public health messages should promote a healthy weight at all ages [44]. In France, a Mediterranean country which, like Spain, has traditionally had low rates of obesity, it has also been necessary to promote messages on nutrition, such as the importance of eating fresh fruit and vegetables often. In terms of equality, food stamp policy has reduced health inequalities, whereas reductions in the VAT have increased them. In terms of efficiency, VAT reductions have had more health benefits than food stamps policies. Taking into account invested resources and obtained results, information campaigns have been the most cost-effective policies. Lastly, market forces, such as marketing strategies, might limit the impact of public health policies designed to promote the consumption of fresh fruits and vegetables [45]. There are also programs that have proven effective for specific groups, such as incorporating exercise in children’s play [46–51] or adopting a healthy diet plan for senior citizens [52]. However, the key question of how to create a balance between the intake and burning of calories through exercise remains unanswered. In general, long-term multicomponent weight management programs have been shown to lead to weight loss in overweight or obese adults. However, little weight is lost and weight regain is common [53]. As a consequence, although cost-effectiveness studies offer some evidence that weight management programs are likely to be cost-effective, caution is required due to a number of limitations in the studies. The steps taken to combat obesity across the globe and its multidimensional nature, makes a single gold standard impossible. Nevertheless, the success of policies depends on a combination of measures that take into account cultural, economical and social aspects. Because the increase in obesity rates are the result of cultural, social, economical and technological influences (sedentary jobs, the cheap prices of food rich in sugar and fat, the high opportunity cost of cooking at home, the use of private cars, and so on), it is difficult to identify cost-effective strategies [54].
Whenever a study has limitations, results should be interpreted with caution. The most patent limitation in this study is that estimations are based on cross-sectional data. This means that while in the majority of cases it would be reasonable to assume that obesity leads to lower HRQOL scores, the opposite may also be true. For example, a person with normal weight who indicates a low HRQOL score due to decreased mobility may gain weight, thereby increasing her/his BMI, and become overweight or obese. In addition, a person with severe anxiety or depression (low HRQOL) may gain weight. Therefore, the estimated associations cannot be interpreted as causal relationships without incurring a certain amount of bias. Another limitation of the study is that the height and weight measurements were self-reported by the participants. A subject’s estimated BMI may in fact differ from the BMI that would have been obtained using objective measurements [13, 55–59]. Self-report bias in BMI is related to gender, older age, and the presence of overweight or obesity. Gorber et al. [60] carried out a systematic review to determine what empirical evidence exists regarding the agreement between objective (measured) and subjective (reported) measures in assessing height, weight and BMI. Their results showed trends of under-reporting for weight and BMI and over-reporting for height, although the degree of the trend varied according to the gender and other characteristics of the population being examined. In another study, Elgar & Stewart [61] showed that self-reports correlated highly with body measurements but on average, self-reported height was greater (0.88 cm) than measured height and self-reported weight was 2.33 kg less than measured weight. As a consequence of these biases, the BMI derived from self-reports was 1.16 lower than BMI derived from measurements. A third study, performed by Gil and Mora [62], found that the more satisfied an individual is with his own body image, the less likely he is to under-report his weight. The authors found no evidence of a similar impact caused by social norms related to height. As a result, they discuss that the prevalence of obesity was significantly underestimated. As a consequence, more studies are needed that compares self-reported height and weight with BMI obtained using objective measurements.
In addition, the lack of longitudinal data means that there is no information regarding the relationship between reduced life expectancy and overweight or obesity among different age groups [63]. Obesity is considered a risk factor for vascular disease and is associated with certain types of cancer. Even wounds and injuries from accidents can be greater and more serious in obese people [64]. Circulatory diseases, tumors and unintentional injuries are, together with neuropsychiatric conditions, the main causes of premature mortality and years of potential life lost (YPLL) among Spanish and European populations. Therefore, a study on how obesity affects quality-adjusted life years (QALY) in Spain is unfeasible at this time due to the lack of sufficient available data.
Physical impairments and mental health problems associated with obesity can lead to disabilities that severely affect individuals with excess weight. With this in mind, steps must be taken that go beyond short to mid-term innovative health care solutions designed to reduce the number of deaths for which obesity is a risk factor as they fail to take into account factors leading to a reduced quality of life among individuals with excess weight. Public health systems and authorities should increase their efforts at prevention and develop institutional schemes in social, labor and educational settings that call for greater measures for controlling weight and reducing the incidence and prevalence of obesity.
Obesity is finally being considered a problem and poses a challenge for the decades that lie ahead. Spain has just recently begun developing policies to reduce its effects [65, 66]. Antoñanzas and Rodríguez [9] point out that this area offers important opportunities for economic research. Important studies have already been conducted on the effects of food prices, economic explanations for the rise in obesity, and the cost-effectiveness of medical and public health interventions, among others. Nevertheless, further analysis is necessary. Designing and implementing measures in a setting that promotes nutrition, physical activity and the prevention of obesity is only possible where clear, up-to-date information is available on the eating patterns and physical activity of the population as well as other policies which may not have been adopted with this phenomenon in mind but nevertheless could have a direct or indirect effect on these public health policy instruments.
It is imperative that health policy decision makers have access to key sources of data on the burdens associated with obesity, such as reduced life expectancy and lower health-related quality of life. Instruments on the cost-effectiveness of interventions and criteria of equity are prerequisites for building sound public policy to reduce the negative effects of overweight and obesity on today’s society.
References
Borg, S., Persson, U., Odegaard, K., Berglund, G., Nilsson, J.A., Nilsson, P.M.: Obesity, survival, and hospital costs-findings from a screening project in Sweden. Value Health. 8(5), 562–571 (2005)
Finkelstein, E.A., Fiebelkorn, I.C., Wang, G.: National medical spending attributable to overweight and obesity: how much, and who’s paying? Health Aff. (Millwood) Suppl Web Exclusives, W3-219–W3-226 (2003)
Katzmarzyk, P.T., Janssen, I.: The economic costs associated with physical inactivity and obesity in Canada: an update. Can. J. Appl. Physiol. 29(1), 90–115 (2004)
Kortt, M.A., Langley, P.C., Cox, E.R.: A review of cost-of-illness studies on obesity. Clin. Ther. 20(4), 772–779 (1998)
Konnopka, A., Bödemann, M., König, H.H.: Health burden and costs of obesity and overweight in Germany. Eur. J. Health Econ. Pending of publication (2010)
Schmid, A., Schneider, H., Golay, A., Keller, U.: Economic burden of obesity and its comorbidities in Switzerland. Soz. Praventivmed. 50(2), 87–94 (2005)
Wolf, A.M., Colditz, G.A.: Current estimates of the economic cost of obesity in the United States. Obes. Res. 6(2), 97–106 (1998)
World Health Organization. Global strategy on diet, physical activity and health. Resolution WHA57.17, Geneva. (2004)
Antoñanzas, F., Rodríguez, R.: Feeding the economics of obesity in the EU in a healthy way. Eur. J. Health Econ. 11, 351–353 (2010)
Aranceta, J., Pérez-Rodrigo, C., Serra-Majem, L., Ribas-Barba, L., Quiles-Izquierdo, J., Vioque, J., et al.: Prevalencia de la obesidad en España: resultados del estudio SEEDO 2000. Med. Clin. (Barc). 120, 608–612 (2003)
Gutiérrez-Fisac, J.L., Regidor, E., Banegas, J.R., Rodríguez, F.: The size of obesity differences associated with educational level in Spain, 1987 and 1995–97. J. Epidemiol. Community Health 56, 457–460 (2002)
Spanish National Health Survey: National Institute of Statistics- Instituto Nacional de Estadística, 2007. Available in \\http:www.ine.es
Flegal, K.M., Graubard, B.I., Williamson, D.F., Gail, M.H.: Excess deaths associated with underweight, overweight, and obesity. JAMA 293(15), 1861–1867 (2005)
Mark, D.H.: Deaths attributable to obesity. JAMA 293(15), 1918–1919 (2005)
Mokdad, A.H., Marks, J.S., Stroup, D.F., Gerberding, J.L.: Actual causes of death in the United States, 2000. JAMA 291(10), 1238–1245 (2004)
Banegas, J.R., Lopez-Garcia, E., Gutierrez-Fisac, J.L., Guallar-Castillon, P., Rodriguez-Artalejo, F.: A simple estimate of mortality attributable to excess weight in the European union. Eur. J. Clin. Nutr. 57(2), 201–208 (2003)
Swedish National Institute of Public Health: determinants of the burden of disease in the European Union. Stockholm (1997)
Yancy Jr, W.S., Olsen, M.K., Westman, E.C., Bosworth, H.B., Edelman, D.: Relationship between obesity and health-related quality of life in men. Obes. Res. 10(10), 1057–1064 (2002)
Katz, D.A., McHorney, C.A., Atkinson, R.L.: Impact of obesity on health-related quality of life in patients with chronic illness. J. Gen. Intern. Med. 15(11), 789–796 (2000)
Jia, H., Lubetkin, E.I.: The impact of obesity on health-related quality-of-life in the general adult US population. J. Public Health (Oxf) 27(2), 156–164 (2005)
Kortt, M.A., Clarke, P.M.: Estimating utility values for health states of overweight and obese individuals using the SF-36. Qual. Life Res. 14(10), 2177–2185 (2005)
Huang, I.C., Frangakis, C., Wu, A.W.: The relationship of excess body weight and health-related quality of life: evidence from a population study in Taiwan. Int. J. Obes. (Lond) 30(8), 1250–1259 (2006)
López-García, E., Banegas, J.R., Gutiérrez-Fisac, J.L., Pérez-Regadera, A.G., Gañán, L.D., Rodríguez-Artalejo, F.: Relation between body weight and health-related quality of life among the elderly in Spain. Int. J. Obes. Relat. Metab. Disord. 27(6), 701–709 (2003)
Badia, X., Schiaffino, A., Alonso, J., Herdman, M.: Using the EuroQol 5 D in the Catalan general population: feasibility and construct validity. Qual. Life Res. 7, 311–322 (1998)
Badia, X., Roset, M., Herdman, M., Kind, P.: A comparison of United Kingdom and Spanish general population time trade-off values for EQ-5 D health states. Med. Decis. Mak. 21(1), 7–16 (2001)
Coakley, E.H., Kawachi, I., Manson, J.E., Speizer, F.E., Willet, W.C., Colditz, G.A.: Lower levels of physical functioning are associated with higher body weight among middle-aged and older women. Int. J. Obes. Relat. Metab. Disord. 22, 958–965 (1998)
Fine, J.T., Colditz, G.A., Coakley, E.H., Moseley, G., Manson, J.E., Willett, W.C., et al.: A prospective study of weight change and health-related quality of life in women. JAMA 282, 2136–2142 (1999)
Kolotkin, R.L., Head, S., Hamilton, M., Tse, C.K.: Assessing impact of weight on quality of life. Obes. Res. 3, 49–65 (2005)
Walters, S.J., Brazier, J.E.: Comparison of the minimally important difference for two health state utility measures: EQ-5 D and SF-6D. Qual. Life Res. 14, 1523–1532 (2005)
Pickard, A.S., Neary, M.P., Cella, D.: Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual. Life. Outcomes 5, 70 (2007)
Søltoft, F., et al.: The association of body mass index and health-related quality of life in the general population: data from the 2003 health survey of England. Qual. Life Res. 18, 1293–1299 (2009)
Larsson, U., Karlsson, J., Sullivan, M.: Impact of overweight and obesity on health-related quality of life—a Swedish population study. Int. J. Obes. Relat. Metab. Disord. 26(3), 417–424 (2002)
Zabelina, D.L., Erickson, A.L., Kolotkin, R.L., Crosby, R.D.: The effect of age on weight-related quality of life in overweight and obese individuals. Obes. (Silver Spring) 17, 1410–1413 (2009)
Rolland, Y., et al.: Difficulties with physical function associated with obesity, sarcopenia, and sarcopenic-obesity in community-dwelling elderly women: the EPIDOS (EPIDemiologie de l’OSteoporose) study. Am. J. Clin. Nutr. 89, 1895–1900 (2009)
Rolland, Y.M., Perry III, H.M., Patrick, P., Banks, W.A., Morley, J.E.: Loss of appendicular muscle mass and loss of muscle strength in young postmenopausal women. J. Gerontol. A Biol. Sci. Med. Sci. 62, 330–335 (2007)
Newman, A.B., Kupelian, V., Visser, M., et al.: Sarcopenia: alternative definitions and associations with lower extremity function. J. Am. Geriatr. Soc. 5, 1602–1609 (2003)
Stienstra, R., et al.: PPARs, obesity, and inflammation. PPAR Res. Volume, Article ID 95974, 10. (2007). doi:10.1155/2007/95974)
Friedmann, J.M., Elasy, T., Jensen, G.L.: The relationship between body mass index and self-reported functional limitation among older adults: a gender difference. J. Am. Geriatr. Soc. 49, 398–403 (2001)
Aronne, L.J.: Classification of obesity and assessment of obesity-related health risks. Obes. Res. 2, 105S–115S (2002)
Franco, M., Sanz, B., Otero, L., Domínguez-Vila, A., Caballero, B.: Prevention of childhood obesity in Spain: a focus on policies outside the health sector. SESPAS report 2010. Gac. Sanit. 24(suppl 1), 49–55 (2010)
Rajmil, L., Díez, E., Peiró, R.: Social inequalities in child health. SESPAS report 2010. Gac. Sanit. 24(suppl 1), 42–48 (2010)
Malecka-Tendera, E., Mazur, A.: Childhood obesity: a pandemic of the twenty-first century. Int. J. Obes. 30(suppl 2), S1–S3 (2006)
Cecchini, M., Sassi, F., Lauer, J.A., Lee, Y.Y., Guajardo-Barron, V., Chisholm, D.: Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet 376, 1775–1784 (2010)
Sabia, S., et al.: Body mass index over the adult life course and cognition in late midlife: the Whitehall II cohort study. Am. J. Clin. Nutr. 89, 601–607 (2009)
Dallongeville, J., Dauchet, L., Mouzon, O., Réquillart, V., Soler, L.G.: Increasing fruit and vegetable consumption: a cost-effectiveness analysis of public policies. Eur. J. Public Health 21(1), 69–73 (2011)
Martínez-Vizcaíno, V., Salcedo Aguilar, F., Franquelo Gutiérrez, R., et al.: Assessment of an after-school physical activity program to prevent obesity among 9- to 10- year-old children: a cluster randomized trial. Int. J. Obes. (Lond) 32, 12–22 (2008)
Wang, L.Y., Gutin, B., Barbeau, P., et al.: Cost-effectiveness of a school-based obesity prevention program. J. Sch. Health 78, 619–624 (2008)
McAuley, K.A., Taylor, R.W., Farmer, V.L., et al.: Economic evaluation of a community based obesity prevention program in children: the APPLE project. Obesity 18, 131–136 (2009)
Haby, M.M., Vos, T., Carter, R., et al.: A new approach to assessing the health benefit from obesity interventions in children and adolescents: the assessing cost effectiveness in obesity project. Int. J. Obes. 30, 1463–1475 (2006)
Brown 3rd, H.S., Pérez, A., Li, Y.P., et al.: The cost-effectiveness of a school-based overweight program. Int. J. Behav. Nutr. Phys. Act. 4, 47 (2007)
Wang, L.Y., Yang, Q., Lowry, R., et al.: Economic analysis of a school-based obesity prevention program. Obes. Res. 11, 1313–1324 (2003)
Knoops, K.T.B., et al.: Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women. The HALE Project JAMA 292, 1433–1439 (2004)
Loveman, E., Frampton, G., Shepherd, J., Picot, J., Cooper, K., et al.: The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health Technol. Assess. 15(2), 1–182 (2011)
Lakdawalla, D., Philipson, T.: The growth of obesity and technological change. Econ. Hum. Biol. 7(3), 283–293 (2009)
Gunnell, D., Berney, L., Holland, P., Maynard, M., Blane, D., Frankel, S., Davey, G.: How accurately are height, weight and leg length reported by the elderly, and how closely are they related to measurements recorded in childhood? Int. J. Epidemiol. 29(3), 456–464 (2000)
Burström, G., Diderichsen, F.: Socioeconomic differentials in misclassification of height, weight and body mass index based on questionnaires data. Int. J. Epidemiol. 26(4), 860–866 (1997)
Kuczmarski, M.F., Kuczmarski, R.J., Najjar, M.: Effects of age on validity of self-reported height, weight and body mass index: findings from the Third NHANES 1988–1994. J. Am. Diet. Assoc. 101(1), 28–34 (2001)
Niedhammer, I., Bugel, I., Bonenfant, S., Goldberg, M., Leclerc, A.: Validity of self-reported weight and height in the French GAZEL cohort. Int. J. Obes. 24(9), 1111–1118 (2000)
Spencer, E.A., Appleby, P.N., Davey, G.K., Key, T.J.: Validity of self-reported height, weight in 4808 EPIC-Oxford participants. Public Health Nutr. 5(4), 561–565 (2002)
Gorber, S.C., Tremblay, M., Moher, D., Gorber, B.: A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes. Rev. 8(4), 307–326 (2007)
Elgar, F.J., Stewart, J.M.: Validity of self-report screening for overweight and obesity evidence from the Canadian community health survey. Can. J. Public Health 99(5), 423–427 (2008)
Gil, J., Mora, T.: The determinants of misreporting weight and height: the role of social norms. Econ. Hum. Biol. 9(1), 78–91 (2011)
Peeters, A., et al.: Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann. Intern. Med. 138, 24–32 (2003)
Matter, K.C., Sinclair, S.A., Hostetler, S.G., Xiang, H.: A comparison of the characteristics of injuries between obese and non-obese inpatients. Obesity (Silver Spring) 15(10), 2384–2390 (2007)
Oliva, J., González, L., Labeaga, J.M., Alvarez Dardet, C.: Public health, obesity and economics: the good, the bad and the ugly. Gac. Sanit. 22(6), 507–510 (2008)
Spanish Ministry for Health and Consumer Affairs/Ministerio de Sanidad y Consumo. Estrategia para la nutrición, actividad física y prevención de la obesidad (Strategy for Nutrition, Physical Activity and the Prevention of Obesity) Estrategia NAOS: Invertir la tendencia de la obesidad. Madrid: Ministerio de Sanidad y Consumo (2004)
Acknowledgments
The Departament de Salut-Servèi Catalá de la Salut-Generalitat de Catalunya provided data obtained through the ESCA for this study. Support for this research was provided by the ECO2008-06395-C05-03/ECON, funded by the Spanish Ministry of Science and Technology. We thank the comments of two anonymous reviewers and the support of Francisco José García and Manuel García Goñi.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oliva-Moreno, J., Gil-Lacruz, A. Body weight and health-related quality of life in Catalonia, Spain. Eur J Health Econ 14, 95–105 (2013). https://doi.org/10.1007/s10198-011-0343-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-011-0343-x