Abstract
This paper provides new evidence on the degree of income-related inequality in self-assessed health in Belgium. First of all, we combine the time dimension, which has been shown to be very important in the analysis of inequality, and the use of the recently developed interval regression approach to transform a categorical health variable in a continuous one. Second, we measure how the long-run inequality differs from the short-run inequality. Finally, we decompose this health-related income mobility index as well as the long-run concentration index (CI) itself into its contributors. Using data from the panel survey of Belgian households (1994–2002), we find that health is pro-rich distributed and that its inequality is underestimated by 9.45% when neglecting the dynamics of individuals over time. Income, education, job status and age are the most important contributors in the CI and the difference between the short-run and long-run inequality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, the dynamics of health and the relation to socio-economic characteristics have caught the attention of researchers. In the literature on measurement of inequalities in health, the focus has been on the cross-sectional concentration index (CI). This is used to calculate socio-economic health inequalities at one point in time and to compare different countries (see, e.g., [7]). However, using cross-section CI in order to look at the evolution of socio-economic inequalities in health can lead to wrong conclusions, as was shown by Jones and Lopez [3]. They develop a long-term CI based on weighted short-term CIs and a term that takes into account the possibility that people may change in income rank. Then, they construct an index of health-related income mobility to measure how the longitudinal outcome differs from the cross-sectional ones. Finally, they showed how one should decompose the mobility index into its contributing factors.
The purpose of this paper is to extend the health economics literature with a first application of this methodology using Belgian data. Moreover, we compare the decomposition of the mobility index with the decomposition of the CI to see whether the same factors contribute. The structure of the paper is as follows. Methods explains the methods used to calculate the different indices and decompositions. There, relevant variables are described as well. The results are shown and explained in Results, Conclusion and Discussion conclude the paper.
Methods
Measurement of inequality
For the measurement of inequality at one point in time, we use the CI (e.g., [8, 9]). It is derived by ranking the population by a measure of socio-economic status (SES) and then comparing the cumulative proportion of health with the cumulative proportion of the population ranked by SES. We use the following formula:
where N is the sample size per wave, \({\bar{y}_{t} }\) is the mean health of the sample in the period t, y it is the health level of individual i in wave t and R t i is the relative fractional rank of the ith individual in the distribution of SES in the period t, defined as (r it − 1/2)/N with r it being the unconditional income rank of individual i in period t.
However, Jones and Lopez [3] illustrate that cross-sectional CIs can lead to wrong conclusions when trying to measure income-related health inequality in the long run as these do not take into account the possibility that people may change in income rank. As such, they derive a formula to measure inequality in the long run, which is similar to the cross-sectional CI. They find that the CI for the distribution of average health after T periods can be written as the difference between two terms: the weighted sum of the CIs for each of the subperiods (term 1) minus the difference between period specific income ranks and ranks for average income over all periods and their relationship to health (term 2) [3]:
\({\overline{\overline y} ^{T} }\) is the overall average health status in T periods, w t can be seen as the share of total health in each period.
To measure the degree by which the longitudinal perspective differs from the cross-sectional analysis, an index of health-related income mobility (MI) can be used. This is defined as one minus the long-term CI after T periods divided by the weighted sum of the cross-sectional CIs [3]:
If M T is larger than zero, the weighted average of the short-run CIs overestimates the degree of long-run inequality (whether pro-rich or pro-poor). A value smaller than zero indicates the opposite. In the case of an index value of 1, there is perfect mobility such that the long-term CI becomes 0 after T periods. If the weighted average of cross-sectional CIs and the long-run index are equal to each other, the value MI will be zero.
Decomposition of the indices
Since we have a categorical health variable, we need to transform it into a continuous one. We use the interval regression approach and predict health as a function of several covariates. These results are used for the decomposition of the index of health-related income mobility. Since our health variable is predicted in a linear way, we can build upon the decomposition method developed by Wagstaff et al. [9]. The model is then as follows:
where y it is the level of (predicted) health of individual i in period t, β k are coefficients, and x itk is the kth regressor. There is no error term in this expression as we estimated the model by interval regression. This means that the β k values can be interpreted as if we observed the predicted health value (y*) and estimated E(y*|x) = x β by ordinary least squares [10].
After some substitutions (for more mathematical details, the reader is referred to [3]), the result for the decomposition is:
where \({M^{T}_{{x_{k}}}}\) is the x k -related income mobility index after T periods defined in a similar way as the health-related income mobility index [see Eq. (3)].
We extend this research by decomposing the CI itself, as the MI focuses on changes in the income rank. We want to know whether the driving factors behind MI are the same as those of the total CI.
To decompose CI, we draw on the formula proposed by Wagstaff et al. [9]. CI can be written as the weighted sum of the CIs of the regressors. Again, as we worked with the interval regression, we do not have an error term here:
where CIT is the long-run CI for health, μ is mean health over all the periods, β k are coefficients, \({\overline{x} _{k}}\) is the mean of the kth regressor taken over all the periods, CI T k is the long-run CI of the kth regressor.
For the empirical application, we use nine waves (1994–2002) of the panel study of Belgian households (PSBH), a representative panel of Belgian private households. The analysis is restricted to persons of 16 years or older, who participated in all the waves and who answered the questions on relevant variables. In the final dataset we were able to follow up 2,000 individuals during nine waves (i.e. a balanced panel).
Similar to other recent studies (e.g. [6]), we use self-assessed health (SAH) as the dependent variable. It is based on the simple question “How is your health in general?”. The response categories are: “very good”, “good”, “reasonable”, “poor” and “very poor”. Despite its simplicity and its subjective nature, it is a good predictor of objective measures of health [1].
However, calculation of CIs requires a continuous health measure. Therefore, we use the interval regression approach as developed by van Doorslaer and Jones [5]. This method requires external data to scale the categorical SAH variable and assumes a stable mapping from these external data to the latent health variable in order to keep the ranking of individuals. For Belgium as a whole, no such continuous external data are available. However, a continuous health variable for Flanders (the largest region in Belgium) has been developed, based on EQ-5D questions [2]. Lecluyse and Cleemput [4] investigate the impact of the choice of external data to estimate inequalities. Therefore they compare the use of the Canadian health utility index and the Flemish EQ-5D index values as external data to calculate the thresholds for the interval regression. Their results show that the magnitude of the CIs is different when using other scaling thresholds. On the other hand, the values of the mobility index and the decomposition are more similar. This seems to be the case as long as the two health variables can be written as a (nearly) linear transformation of each other. With these results in mind, we decide to use the Flemish EQ-5D index as external data. This EQ-5D index consists of five dimensions of health in three levels of severity and can be used for the measurement of SAH [2]. The thresholds used as upper and lower boundaries in the interval regression are: 0, 0.1354, 0.5356, 0.7408, 0.9089 and 1.
Results
The results of the interval regression are shown in Table 1; for your information we present the mean of the variables as well. We see that our results confirm earlier studies. People with higher income report better health. Moreover, it seems that current income (the logarithm of equivalent household income) is not significant, while the logarithm of average equivalent household income is. The latter can be seen as a reflection of permanent income. Further, the SAH of women is significantly lower than that of men. The age and education dummies have expected signs and magnitude as well: younger respondents have significant better health than older ones, and the higher the diploma the better SAH.
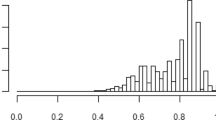
The continuous health variable is obtained as a linear prediction of this regression. The mean value is around 0.8 in each year, and there is a slight decrease in successive years. As we work with a balanced panel, this is according to our expectations, because it is known that health decreases with age (e.g. [6]).
The results in Fig. 1 clearly show that there is pro-rich health inequality in each wave, as all CIs are positive. A closer look at these short-run CIs teaches us that there is an overall increase in inequality, with the exception of 1995. These results confirm what was found earlier: in his dataset (PSBH 1994–1998), Van Ourti [8] also found an increase in the pro-rich health inequality and there was also a decline in inequality in 1995.
The “CI total” curve shows the long-term CI. Again inequality is increasing. The curves “term 1” and “term 2” correspond to the respective terms in Eq. (2).
Term 1 is the weighted average of the cross-sectional CIs up to the corresponding wave. The same evolution can be seen: an increase in inequality, again with the sole exception of the second year of the dataset. Thus, the CI within a period contributes to the long-term trend. However, term 1 is smaller than the total long-term CI, meaning that the short-term indices underestimate long-term inequality. Consequently, term 2 is negative in each year, implying that downwardly income mobile individuals tend to report below-average health levels compared to upwardly income mobile individuals. The mobility index (the lower graph in Fig. 1) is increasing over the years (in absolute values), meaning that the error of taking a cross-section CI instead of a longitudinal index becomes larger. After nine years we find that the income-related long-term health inequality increases by 9.45% due to the effect of individuals moving on the income distribution.
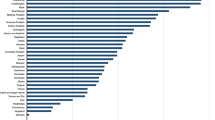
In Table 2, the contribution of each of the regressors to the health-related income mobility index after nine periods is presented.
“CIT” shows the CI of the regressor on income after nine periods. If this CI is positive, the variable has a pro-rich distribution and vice versa. For example, being divorced has a total CI of −0.12. As a result, it is more concentrated among the poor.
The second column presents the x k -related income-related mobility index. A negative mobility index means that the weighted average of short-run CIs underestimates the degree of long-run inequality (whether pro-rich or pro-poor). If this number has a positive value, it indicates the reverse. For example, the short-run CI overestimates the pro-rich inequality of the logarithm of the (current) equivalent income, while the negative mobility index of the logarithm of average equivalent income indicates that the long-run inequality is higher.
The next column, “Elasticity(x)” contains the inequality-weighted elasticity of health with respect to the regressor. Here, the sign does not indicate whether the dynamics of the regressor influences pro-rich income-related health inequality in the long-run. Consider for example the logarithm of equivalent income and the logarithm of average income: both have a positive elasticity, but the impact on the distribution of health is different. Despite a similar sign for both CIs (positive) and both coefficients (positive, see Table 1), the mobility indices have a different sign. It is positive for the logarithm of equivalent income, indicating that the inequality in income is less pro-rich distributed in the long-run. As a consequence, the positive elasticity indicates that the dynamics of equivalent income lead to a less pro-rich income-related health inequality in the long run. The contrary holds for the logarithm of the average equivalent income, i.e. the distribution of the logarithm of average income is more pro-rich in the long run. In this case, the positive elasticity means that the dynamics of the average of equivalent income leads to a more pro-rich income-related health inequality in the long run. One should reason along the same lines for the other covariates.
Multiplying the mobility index and the elasticity gives their contribution. A negative sign means that the regressor stimulates a more pro-rich income-related inequality of health and vice versa.
The last two columns show the contribution of each of the regressors and per vector respectively, expressed as percentages of the total index. Education has the largest contribution, followed by income, job status and age.
Now we compare those results with the decomposition of the long-run CI of health, presented in Fig. 2. The upper part of the graph repeats the decomposition of the MI visually, and the lower part represents the decomposition of the long-run CI. The latter is calculated according to Eq. (6). In general, we see that the same variables have the largest impact. However, there are some important differences. First of all, income now makes the largest contribution, followed by education, then job status and age. We also find a much smaller impact of marital status, moreover it is now positive. Looking in further detail (not reported here), we see that the equivalent income also has a reversed impact on the mobility index compared to the CI. In the case of the mobility index, the dynamics of equivalent income leads to a less pro-rich distribution of health, while it stimulates the CI itself. On the contrary, average income leads to a more pro-rich distribution of both the mobility and CI, with a larger impact on the former.
Conclusion
In this paper, we try to explain the evolution of income-related inequality in health. Therefore, we used a balanced panel consisting of nine waves of the PSBH. We transformed our categorical SAH variable into a continuous one using the interval regression approach. As external data for scoring the intervals we used the EQ-5D index values developed for Flanders.
The results show a pro-rich distribution of SAH in each year. Moreover, cross-section as well as long-run inequality increases towards later periods. However, using the former underestimates inequality due to the fact that downwards mobile people in the income rank tend to report a below-average level of health. The difference caused by this mobility is captured by the health-related income mobility index, which is 9.45% in absolute values after nine years. Decomposing the mobility index into its contributors reveals that the dynamics of income, education, job status and age have the largest influence. These are the same for the decomposition of the long-run income-related health inequality. We also find that equivalent (current) income has a reverse effect on the mobility index compared to the CI.
Discussion
In our analysis we used a dynamic approach to measure inequality in health rather than a static one. Where the latter approach is often used to compare inequality at two different points in time, the dynamic approach is especially useful when interest lies in long-run rather than short-run inequality (which can be the case for, e.g., policy makers). As Jones and Lopez [3] prove theoretically and as is also shown in this study with Belgian data, looking at different points in time using short-run CI does not give a complete picture. We find an increase in the absolute value of the CI of 9.45% when taking dynamics into consideration.
We performed our analysis using a balanced panel subsample of the PSBH. The advantage is that the same individuals can be followed during a certain period. Here we look at how change in income distribution has an impact on the inequality in SAH. Because we are able to follow each individual in every year we have a complete picture of their relative evolution. However, we have to be aware that in other studies evidence exists for the fact that poorer people or people in worse health are more likely to drop out of the sample. Therefore we must be careful in drawing conclusions for Belgium as a whole.
References
Benjamins, M.R., Hummer, R.A., Eberstein, I.W., Nam, C.B.: Self-reported health and adult mortality risk: an analysis of cause-specific mortality. Soc. Sci. Med. 59, 1297–1306 (2004)
Cleemput, I.: Economic evaluation in renal transplantation. Ph.D. Thesis, Leuven (2003)
Jones, A.M., Lopez, A.: Measurement and explanation of socioeconomic inequality in health with longitudinal data. Health Econ. 13, 1015–1030 (2004)
Lecluyse, A., Cleemput, I.: Making health continuous: implications of different methods on the measurement of inequality. Health Econ. Lett. 15, 99–104 (2006)
van Doorslaer, E., Jones, A.M.: Inequalities in self-reported health: validation of a new approach to measurement. J. Health Econ. 22, 61–78 (2003)
van Doorslaer, E., Koolman, X.: Explaining the differences in income-related health inequalities across European countries. Health Econ. 13, 609–628 (2004)
van Doorslaer, E., Wagstaff, A., Bleichrodt, H., Calonge, S., Gerdtham, U.G., Gerfin, M., et al: Income-related inequalities in health: some international comparisons. J. Health Econ. 16, 93–112 (1997)
Van Ourti, T.: Socio-economic inequality in ill-health amongst the elderly. Should one use current or permanent income? J. Health Econ. 22, 219–241 (2003)
Wagstaff, A., van Doorslaer, E., Watanabe, N.: On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J. Econom. 112, 207–233 (2003)
Wooldridge, J.M.: Econometric Analysis of Cross Section and Panel Data. Mass. MIT Press, Cambridge (2002)
Acknowledgments
I am grateful to D. De Graeve and T. Van Ourti for their helpful suggestions. I also wish to thank Irina Cleemput for supplying scores of the EQ-5D, which I needed as external data for the interval regression approach.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lecluyse, A. Income-related health inequality in Belgium: a longitudinal perspective. Eur J Health Econ 8, 237–243 (2007). https://doi.org/10.1007/s10198-006-0024-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-006-0024-3