Abstract
Background
The association between physical activity volume or intensity and mortality in general population with impaired renal function is unclear. We assessed these relationships among Japanese residents with impaired renal function.
Methods
We analyzed 638 individuals with estimated creatinine clearance below 60 ml/min in the Jichi Medical School cohort study. Exposures included the daily amount of physical activity converted to the physical activity index (PAI) used in the Framingham study and the activity time for each intensity. Physical activity intensity was classified into sedentary and nonsedentary. Nonsedentary activity was further divided into light-intensity and moderate-to-vigorous physical activity (MVPA). The outcome was all-cause mortality. Quartiles of the exposures were created, and hazard ratios (HRs) were calculated using the Cox proportional hazards model.
Results
The mean age of the subjects was 63.3 years, and 72.4% were female. In total, 172 deaths were registered during 11,567 person-years. No significant association was found between PAI and mortality. A significant association was found between long sedentary time and increased mortality (p = 0.042). Regarding nonsedentary activity, the HRs [95% confidence intervals (CIs)] for Q2, Q3, and Q4 versus Q1 were 0.85 (0.55–1.31), 0.67 (0.41–1.08), and 0.90 (0.54–1.45), respectively. In the subdivided analysis for light-intensity activity, the HRs (95% CIs) of Q2, Q3, and Q4 versus Q1 were 0.53 (0.33–0.84), 0.51 (0.34–0.82), and 0.57 (0.34–0.96), respectively. No significant association was found between MVPA and mortality.
Conclusions
Nonsedentary activity, especially light-intensity activity, significantly reduced mortality among residents with impaired renal function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The population with impaired renal function is increasing worldwide, as the global prevalence of chronic kidney disease (CKD) is estimated to be 9.1% [1]. Sarcopenia and frailty are frequently associated with abnormal skeletal muscle metabolism, which is considered to be a factor that increases the risk of death [2, 3].
For people with impaired renal function who have such a high risk of death, knowledge regarding the amount and intensity of physical activity that would affect their prognosis would be helpful, but few previous studies have addressed this question. Among previous studies focusing on the amount of physical activity, an analysis of 906 residents with estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2 in the USA showed that the group that was active during leisure time had a lower risk of death than the inactive group [4]. In another study of 46,375 residents with stage 1 or higher CKD in Taiwan, mortality decreased as the amount of leisure-time physical activity increased [5]. However, according to a survey of 811 residents with glomerular filtration rate (GFR) < 60 ml/min/1.73 m2 in the USA, there was no significant difference in mortality for different amounts of physical activity [6].
Fewer studies have focused on the intensity of physical activity. In one study in which the daily physical activity of 383 residents with eGFR < 60 ml/min/1.73 m2 in the USA was measured by means of an accelerometer, estimation of the exponentiation of linear contrasts of the Cox regression coefficients showed that the risk of death was significantly reduced when 2 min/h of sedentary behavior was traded off for light-intensity activity. On the other hand, the trade-off of sedentary time to moderate-to-vigorous physical activity (MVPA) did not significantly reduce mortality. However, in the analysis of the relationship between activity duration for each intensity and mortality, adjustments were not made for cardiovascular risk factors such as body mass index (BMI) or blood pressure [7].
There is no consensus on the relationship between the amount of physical activity and mortality among people with impaired renal function. Furthermore, there is only one report investigating the relationship between the intensity of physical activity and mortality, and in that study, the analysis for the relationship between activity duration of each intensity and mortality was not adjusted for confounders such as BMI, blood pressure, or time spent on physical activities of other intensities.
The aim of this study was to investigate the relationship between the amount or intensity of physical activity and the risk of death among Japanese local residents with renal dysfunction.
Materials and methods
Study population
This study is an observational study using data from the Jichi Medical School (JMS) Cohort Study. The JMS cohort study is a large-scale prospective cohort study conducted by Jichi Medical University targeting local residents in 12 districts in the countryside of Japan to examine the relationship between lifestyle and cardiovascular diseases. Details of the study have already been reported [8]. Briefly, blood tests and interview-type questionnaire surveys were conducted as the baseline survey between April 1992 and July 1995 using the mass screening examinations conducted by each local government. As a follow-up, death was confirmed by records from death certificates. Follow-up was conducted until 2013, and approximately 99% of the participants could be followed up. Informed consent for the study was obtained in writing for all participants. This study was approved by the Institutional Review Board of Jichi Medical University (Epidemiology 06-11, 2006).
Participants
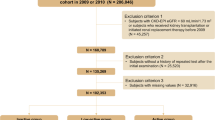
A flowchart of participants is shown in Fig. 1. In the JMS cohort study, 12,490 (4911 males and 7579 females) were eligible. Among them, the serum creatinine (sCr) levels of 5169 people (1870 males and 3299 females) from the three districts of Sakugi, Tako, and Yamato were measured by means of the Jaffe method. The estimated creatinine clearance (eCCr) was calculated from these data by means of the Cockcroft-Gault formula: eCCr (ml/min) = (140 − age) × body weight/(72 × sCr), × 0.85 for female. In total, 733 people (210 males and 523 females) had eCCr < 60.0 ml/min and were included in this study. The exclusion criteria were a history of cerebral infarction, myocardial infarction, or malignant tumor; missing medical history; or an invalid item in the physical activity questionnaire (e.g., the total time to filling out the questionnaire was not 24 h). In total, 95 people met the exclusion criteria, and 638 people (176 males and 462 females) were analyzed.
Variables and data source
The exposure was the amount of total daily physical activity and the time spent performing the physical activity at each intensity, and the outcome was all deaths. Physical activity was investigated by means of the questionnaire of the Framingham Heart Study conducted in the USA [9]. The questionnaire-based investigation was performed during an in-person interview. This survey form refers to five levels of the physical activity intensity; namely, basal, sedentary, light, moderate, and vigorous, and participants were asked to state the number of hours spent on each activity intensity in a typical day. The total amount of physical activity is represented by the physical activity index (PAI), summing up hours weighted by the factor of each intensity, with the weighting factors as follows: basal, 1.0; sedentary, 1.1; light, 1.5; moderate, 2.4; and vigorous, 5.0. The reliability and validity of the PAI have been verified in a previous study [10]. The intensity of physical activity was categorized as ‘sedentary’ and ‘nonsedentary.’ ‘Sedentary’ refers to the time entered for sedentary in the questionnaire. ‘Nonsedentary’ refers to the times entered for light, moderate, and vigorous in the questionnaire, which are combined into one variable. ‘Nonsedentary’ was further subdivided into two intensities, namely ‘light’ and ‘moderate-to-vigorous.’
Data used to confirm outcomes were collected from death certificates at the public health center with permission from the Ministry of Internal Affairs and Communications and the Ministry of Health, Labour and Welfare.
Confounding factors are age, sex, area, BMI (< 18.5, 18.5–25.0, ≥ 25.0), systolic blood pressure, total cholesterol level, drinking, smoking (never smoker, current smoker, ex-smoker), diabetes treatment, hypertension treatment, educational history (≤ 15 years old, ≥ 16 years old), marital status, job categories (primary industry, other jobs, unemployed), history of angina, and history of other heart diseases. BMI were calculated as weight (kg)/height (cm)2. Body weight was measured while wearing clothes, and the weight was recorded minus 0.5 kg in summer and 1.0 kg in other seasons. Body height was measured with the participant’s socks on. Total cholesterol levels were measured by enzymatic methods. Drinking status was categorized as current drinker or non-drinker. Smoking status was categorized as current smoker, ex-smoker, or never smoker. Patients with diabetes treatment and hypertension treatment were divided according to whether they were treated at the time of the baseline survey. Based on the ages of the participants when they went go to school, we classified them as those with a final educational background of 15 years or younger and those with a final educational background of 16 years or older. Regarding job categories, agriculture, forestry, and fisheries were classified as the primary industry, other occupations as other jobs, and retired and unemployed (including full-time homemakers) as unemployed.
Statistical method
Quartiles [Q1 (low)–Q4 (high)] of PAI of the analysis subjects were created. Using Q1 as a reference, HRs for the all-cause mortality of each quartile for PAI were calculated using the Cox proportional hazards model. Similarly, for sedentary duration and nonsedentary activity duration, quartiles were created for each, and HRs for the all-cause mortality of each quartile were calculated using the Cox proportional hazards model. Furthermore, to analyze the effect of each activity intensity contained in nonsedentary activity individually, nonsedentary activity was subdivided into light-intensity activity and MVPA. Then, quartiles of light-intensity activity duration and MVPA duration were created in the same manner, and all-cause mortality in each quartile was calculated using the Cox proportional hazards model.
Model 1 was crude. Model 2 adjusted for age, sex, area, drinking, smoking, job, marital status, and educational history. In model 3, potential intermediate factors such as BMI, systolic blood pressure, total cholesterol levels, diabetes treatment, hypertension treatment, and a history of other heart diseases were included in addition to the covariates in model 2. In the analysis of the physical activity duration of ‘light’ and ‘moderate-to-vigorous’ in models 2 and 3, the other intensity durations for physical activity were adjusted in addition to the above covariates. For example, in the analysis of light-intensity activity duration, the moderate-to-vigorous intensity activity duration was added to the covariates, and in the moderate-to-vigorous analysis, the light-intensity activity duration was added to the covariates. Covariate data were missing for drinking (n = 5), smoking (n = 12), job (n = 4), marital status (n = 18), and educational history (n = 9). After participants with missing covariate data were excluded, 594 participants were included in the multivariable analysis. Missing data were removed and analyzed. The statistical significance level was set to 5%. All analyses were performed using IBM SPSS statistics 25.
Results
Descriptive data
The characteristics of the analysis subjects by quartiles of PAI are shown in Table 1. The mean age of the subjects was 63.3 years, and 72.4% were females. The mean systolic blood pressure was 129.9 mmHg, the mean total cholesterol level was 197.9 mg/dl, and 47 (7.4%) people had a BMI ≧ 25.0. A total of 187 (29.3%) people had a drinking habit, and 91 (14.3%) had a smoking habit. Regarding occupation, the highest unemployed/homemaker constituted the largest category at 269 (42.2%) participants, followed by primary industry workers, comprising 241 (37.8%) participants.
The mean eCCr value was 52.5 ml/min. The distribution of eCCr was as follows: The number of participants with eCCr 45–59 ml/min was 567 (88.9%); that with eCCr 30–44 ml/min was 70 (11.0%); and that with eCCr 15–29 ml/min was 1 person (0.2%). No one had an eCCr of less than 15 ml/min.
The mean PAI was 33.2. The mean times of physical activity at each intensity were as follows: sedentary, 8.8 h/day; nonsedentary, 8.6 h/day; light, 4.8 h/day; and moderate-to-vigorous, 3.9 h/day.
HRs on physical activity volume and intensity for mortality
Of the 11,567 person-years, 172 deaths were registered, including 57 cardiovascular (CVD) deaths, 43 cancer deaths, and 72 other-cause deaths. First, regarding the quartile of physical activity volume expressed by PAI, no significant association was found between PAI and all-cause mortality. Specifically, HRs [95% confidence intervals (CIs)] for all-cause mortality based on Q1 (PAI < 29.2) of Q2 (29.2–32.3), Q3 (32.3–36.3), and Q4 (≥ 36.3) were 0.94 (0.58–1.51), 0.76 (0.46–1.24), and 1.01 (0.62–1.66) in model 2, respectively.
Next, regarding the association between sedentary duration and mortality, compared with that of Q1 (< 7.5 h/day), the HRs (95% CIs) of Q3 (8.0–9.5 h/day) and Q4 (≥ 9.5 h/day) were significantly higher, at 1.61 (1.01–2.56) and 1.95 (1.23–2.97), respectively, in model 1. In addition, the trend tests that treated the data of each participant as a continuous variable showed significance at p < 0.001. In model 2, adjusted for confounding factors, no significant association was found between any quartile and mortality, but the trend test showed significance at p = 0.042. In model 3 with cardiovascular risk factors, none of the quartiles were significantly associated with mortality.
Regarding the association between nonsedentary duration and mortality, the longer the activity time was, the lower the mortality would be (p for trend = 0.032). However, when adjustments were made for confounding factors in model 2, compared with that of Q1 (< 6.5 h/day), the HRs (95% CIs) of Q2 (6.5–9.0 h/day), Q3 (9.0–11.0 h/day), and Q4 (≥ 11.0 h/day) for all-cause mortality were not significant, but that of Q3 was the lowest (HR 0.67, 95% CI 0.41–1.08). Adjusting for cardiovascular risk factors in model 3 resulted in a significantly lower mortality for Q3 (HR 0.58, 95% CI 0.35–0.97).
In the subdivided analysis of nonsedentary activity, compared with that of Q1 (< 2.0 h/day) for light-intensity activity duration, the HRs (95% CIs) of Q2 (2.0–4.0 h/day), Q3 (4.0–7.0 h/day), and Q4 (≥ 7.0 h/day) for all-cause mortality were 0.53 (0.33–0.84), 0.53 (0.34–0.82), and 0.57 (0.34–0.96), respectively. The trend tests were also significant at p = 0.018. Similar results were obtained when adjustments were made for cardiovascular risk factors in model 3. MVPA duration also tended to reduce mortality as follows: Compared with that of Q1 (0.0 h/day), HRs (95% CIs) of Q2 (0.0–3.0 h/day), Q3 (3.0–7.0 h/day), and Q4 (≥ 7.0 h/day) were 1.02 (0.61–1.70), 0.66 (0.40–1.11), and 0.80 (0.45–1.43), respectively, which were not significant (Table 2).
Discussion
Light-intensity physical activity significantly reduced all-cause mortality among local residents with renal dysfunction, while there was no significant association between the amount of physical activity and mortality in this study.
High total physical activity volume tended to decrease mortality, but there was no significant association in this study. Wen et al. reported a significant association between physical activity volume and mortality risk among 46,375 local residents with CKD stage 1 to 5, while Chen et al. reported no significant association among 811 local residents with GFR < 60 ml/min/1.73 m2 [5, 6]. The number of subjects in our study was 638, which was on the same scale as that reported by Chen et al., and the fact that no significant association was found may be due to insufficient power. Among other previous studies, Beddhu et al. investigated the relationship between physical activity and mortality among 906 subjects with eGFR < 60 ml/min/1.73 m2, a sample size that was almost the same as that in this study, and found a significant relationship. However, it is possible that their analysis was likely to reveal a difference because the reference was ‘no activity’ [4].
Regarding the impact of sedentary duration on mortality, the trend tests were significant in the adjusted model. This was a similar result to that previous study [7]. However, no significant association was found between any quartile and mortality. The reason why no significant association was found with any quartile may be that the power was insufficient and that the sedentary duration of this cohort was shorter than that of the previous study. For example, the mean sedentary duration of the cohort investigated by Beddhu et al. was 9.5 h/day because the mean wearing time of the accelerometer was reported to be 14.0 h/day and the mean sedentary duration was 40.8 min/h [7]. In our cohort, only 179 subjects (28.1%) had a sedentary duration of 9.5 h/day or more. Therefore, it may have been difficult to find an association with mortality because few participants had long sedentary durations.
Our results showed that a large amount of light-intensity physical activity reduced the risk of death. Similar results have been confirmed in previous studies. Beddhu et al. investigated the effect of each physical activity intensity on the risk of death for their analysis of total daily physical activity among participants with eGFR < 60 ml/min/1.73 m2. They reported that a 2-min/h trade-off of sedentary duration for light-intensity activity reduced the HR for all-cause mortality. However, replacing sedentary duration with MVPA did not significantly reduce mortality [7]. Our results were similar, showing no significant association between MVPA duration and mortality. This might be due to insufficient power. From these results, it is considered that even light physical activity has a positive effect on reducing mortality among people with impaired renal function. In addition, Beddhu et al. analyzed the relationship between the duration of each physical activity intensity and mortality, but the analysis did not adjust for cardiovascular risk factors such as BMI or cholesterol level or the durations of activities with other intensities. It seems novel that we have shown the effect of the physical activity duration for each intensity on mortality adjusted for cardiovascular risk factors, socioeconomic factors, and duration of activities of other intensities.
To reveal what types of deaths were associated with light-intensity physical activity, we performed sensitivity analysis for each cause of death. HRs for CVD mortality and cancer mortality were calculated in the same way as all-cause mortality. Regarding CVD mortality, light-intensity activity duration tended to be lower HRs as follows: compared with that of Q1 (< 2.0 h/day), the HRs (95% CIs) of Q2 (2.0–4.0 h/day), Q3 (4.0–7.0 h/day), and Q4 (≥ 7.0 h/day) were 0.42 (0.19–0.94), 0.41 (0.18–0.91), and 0.56 (0.22–1.41) in model 2, respectively (Online Resource 1). Similarly for cancer mortality, compared with that of Q1 (< 2.0 h/day) for light-intensity activity, the HRs (95% CIs) of Q2 (2.0–4.0 h/day), Q3 (4.0–7.0 h/day), and Q4 (≥ 7.0 h/day) were 0.26 (0.07–0.92), 0.55 (0.23–1.33), and 0.71 (0.26–1.93) in model 2, respectively (Online Resource 2). These results suggest that light-intensity activity also decrease CVD mortality and cancer mortality in general population with mild to moderate renal impairment.
Additionally, to examine differences in effects of light-intensity activity duration for all-cause mortality by subgroup of age at baseline, the HRs on high light-intensity activity level (Q2–Q4: ≥ 2.0 h/day) compared to that of low light-intensity activity level (Q1: < 2.0 h/day) for all-cause mortality were calculated separately for non-elderly participants (age < 65 years at baseline) and elderly participants (age ≥ 65 years at baseline) using the Cox proportional hazards model. Furthermore, the interaction between age at baseline and light-intensity activity duration for all-cause mortality was analyzed by adding the interaction term of ‘age (< 65 years or ≥ 65 years) × light-intensity activity duration (< 2.0 h/day or ≥ 2.0 h/day)’ in model. The results showed that, compared with that of Q1 (< 2.0 h/day), the HRs (95% CIs) of Q2–Q4 (≥ 2.0 h/day) were 0.39 (0.118–0.84) in non-elderly participants and 0.54 (0.34–0.86) in elderly participants, respectively. The interaction between age at baseline (< 65 years or ≥ 65 years) and light-intensity activity duration (< 2.0 h/day or ≥ 2.0 h/day) for all-cause mortality was not significant (Online Resource 3). These results showed that light-intensity activity reduces all-cause mortality regardless of age at baseline.
One of the strengths of this study is its investigation of the impacts of both the volume and intensity of physical activity on mortality, with adjustments for cardiovascular and socioeconomic factors in the general population with renal dysfunction. In addition, our results can be applied to more people because data on participants with renal dysfunction were extracted from a medical examination study targeting the entire community rather than from a group of recruited CKD patients who had already been treated at the hospital. Moreover, the JMS cohort study had a very high follow-up rate of 99%, and losses to follow-up were slight. The long follow-up period and the high validity of the outcome due to confirmation of the death certificate are also considered to be the advantages of this study.
This study has some limitations. The first is that the index of renal function was eCCr calculated by the Cockcroft–Gault formula (C–G formula) based on the serum creatinine level. eCCr is known to overestimate the glomerular filtration rate (GFR) and may miss people with mild renal impairment [11]. The standard eGFR formula for Japanese individuals (eGFR (ml/min/1.73 m2) = 194 × sCr−1.094 × age−0.287, × 0.739 for female) as a renal function index assumes that the enzyme method Cr value is used; therefore, it was not used in this study. Second, participants had relatively mild renal dysfunction, mostly eCCr 30–59 ml/min. The percentage of Japanese subjects who had a medical examination and an eGFR less than 30 ml/min/1.73 m2 was 0.2–1.0% [11, 12]. The proportion of people with eCCr less than 30 ml/min in our cohort was small compared to that in previous studies, which may be because eCCr overestimated GFR.
The recommended amount of physical activity suggested to people with renal dysfunction is currently left to the discretion of each physician due to a lack of sufficient evidence. The results of this study show that light-intensity activity reduces the risk of death, and these findings may be helpful when giving advice to patients with renal dysfunction.
Data availability statement
The data underlying this article were provided by Secretariat of the JMS Cohort Study by permission. The data will be shared on request to the corresponding author with permission of Secretariat of he JMS Cohort Study.
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33.
Sharma D. Association of sarcopenia with eGFR and misclassification of obesity in adults with CKD in the United States. Clin J Am Soc Nephrol. 2014;9:2079–88.
Carrero JJ. Etiology of the protein-energy wasting syndrome in chronic kidney disease: a consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J Renal Nutr. 2013;23:77–90.
Beddhu S. Physical activity and mortality in chronic kidney disease (NHANES III). Clin J Am Soc Nephrol. 2009;4:1901–6.
Wen CP. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378:1244–53.
Chen JL. Association of physical activity with mortality in chronic kidney disease. J Nephrol. 2008;21:243–52.
Beddhu S. Light-Intensity physical activities and mortality in the United States general population and CKD subpopulation. Clin J Am Soc Nephrol. 2015;10:1145–53.
Ishikawa S. The Jichi Medical School (JMS) cohort study: design, baseline data and standardized mortality ratios. J Epidemiol. 2002;12:408–17.
Tan ZS. Physical activity, brain volume, and dementia risk: the Framingham study. J Gerontol A Biol Sci Med Sci. 2017;72:789–95.
Sasai H. Simultaneous validation of seven physical activity questionnaires used in Japanese cohorts for estimating energy expenditure: a doubly labeled water study. J Epidemiol. 2018;28:437–42.
Nagata M. Trends in the prevalence of chronic kidney disease and its risk factors in a general Japanese population: the Hisayama Study. Nephrol Dial Transplant. 2010;25:2557–64.
Imai E. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol. 2009;13:621–30.
Acknowledgements
We would like to thank all the residents who participated in the JMS cohort study and the staff who conducted the medical examination.
Funding
This work was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan; grants from the Foundation for Community Development, Tochigi, Japan; a Grant-in-Aid from the Ministry of Health, Labour and Welfare of Japan; and Health and Labour Sciences Research Grants for Research on Health Services [Grant numbers H26-Junkankitou (Seisaku)-Ippan-001, H29-Junkankitou-Ippan-003, and 20FA1002].
Author information
Authors and Affiliations
Contributions
SI, TG, YN, KK, and TO developed the research design and conducted the data acquisition and data analysis of the JMS cohort study. NK, YS, and TO participated in the design of the study, performed statistical analysis, and drafted the manuscript. YS, TO, HY, SI, TG, YN, KK, and TO made significant contributions to the analysis and interpretation of the data in this study. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors have declared no competing interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (IRB approval number Epidemiology 06-11, 2006) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kinoshita-Katahashi, N., Shibata, Y., Yasuda, H. et al. Association between physical activity and mortality in the Japanese general population with mild to moderate impaired renal function: the Jichi Medical School (JMS) cohort study. Clin Exp Nephrol 27, 243–250 (2023). https://doi.org/10.1007/s10157-022-02301-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-022-02301-1