Abstract
Background
There is limited evidence of medication adherence related to progression of chronic kidney disease (CKD) worldwide. The aim of this study was to determine associations between medication adherence and the progression of CKD in outpatients with CKD.
Methods
This cohort study recruited 339 Thai patients with stages 3–5 CKD. Patients with a glomerular disease or receiving renal replacement therapy before recruitment were excluded. 295 were followed up regarding their serum creatinine, blood pressure, glycated hemoglobin, and low-density lipoprotein cholesterol over 12 months. Medication adherence was measured at baseline using the Thai version of the 8-Item Morisky Medication Adherence Scale®. The primary outcome was the progression of CKD. The progression of CKD was defined as either a decline in estimated glomerular filtration rate of at least 3 ml/min/1.73 m2/year or initiation of renal replacement therapy. Univariate and multivariate analyses were performed using Chi-squared tests and multiple logistic regressions.
Results
Twenty-one percent had poor adherence. Younger patients were more likely to have poor adherence (adjusted OR 2.81, 95 % CI 1.45–5.43). Anti-hypertensive agents were the most frequently reported as not being taken (52 %). Patients with poor adherence were associated with the progression of CKD (adjusted OR 1.96, 95 % CI 1.02–3.76). Those with poor adherence were less likely to control their blood pressure, than moderate-to-high adherence group (p < 0.01).
Conclusion
The findings suggest that CKD patients with poor medication adherence are more likely to have progression of CKD. Health care providers should acknowledge these findings and provide effective strategies to deal with this issue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medication adherence is an important contributor to achieving the goals of treatment. Patients with diabetes or hypertension who have a high level of medication adherence are more likely to control their blood sugar or blood pressure, or to decrease mortality [1–3]. Patients with chronic kidney disease (CKD) are likely to have poor medication adherence due to the high number of medications used and the complexity of their medicine regime [4, 5]. Typically patients with CKD use 6–12 different medicines to treat all their medical conditions [6].
The prevalence of non-adherence to medication in non-dialysis patients with CKD ranged from 8 to 33 % assessed using various measures of medication adherence, such as the proportion of days covered, medication possession ratio, and the 4-Item Morisky Medication Adherence Scale [7–11]. A systematic review of medication adherence in dialysis patients has reported that a self-report questionnaire is frequently used to evaluate medication adherence [12]. This is a common tool for measuring medication adherence in clinical practice due to being convenient and inexpensive, despite having the disadvantages of recall and social desirability bias, and the likelihood of overestimating medication adherence [13].
Characteristics of CKD patients with poor adherence are not consistent across studies. Magacho et al. reported that poor adherence was associated with both a high number of medications and medicines administrated by a caregiver [7]. Meanwhile, Muntner et al. found no association of poor adherence with the number of medications, but younger age was related to poor adherence [11]. Both studies also reported that gender and a level of education were not related to poor medication adherence [7, 11]. Schmitt’s study in 2010 revealed that the more kidney function worsened, the more the level of medication adherence decreased [9]. Depressive symptoms were associated with a low level of medication adherence in patients with CKD [11].
There is a lack of evidence regarding associations between medication adherence and the progression of CKD in non-dialysis patients. One large retrospective study in patients with CKD has shown that poor adherence was associated with uncontrolled blood pressure [9]. Therefore, our study aimed to determine any associations between medication adherence and the progression of CKD. The secondary objective was to determine characteristics associated with poor medication adherence in patients with CKD.
Methods
This cohort study recruited 357 patients who were diagnosed with CKD and had an estimated glomerular filtration rate (eGFR) of less than 60 ml/min/1.73 m2 from two kidney clinics in public teaching hospitals in Thailand during January–June 2012. The first hospital represented an urban population, while the second hospital represented a rural population. Thailand’s Universal Coverage Scheme supported the costs of medications for Thai patients with CKD in these hospitals. An eGFR was calculated using the Thai Modification of Diet in Renal Disease equation [14]. Patients either having a glomerular disease diagnosed by a doctor, or receiving renal replacement therapy at baseline were excluded. Two hundred and ninety-five patients were followed up over the 12 months and recorded their serum creatinine, blood pressure, HbA1c, and LDL. Serum creatinine was measured using an enzymatic method, which has provided more accurate calculation of eGFR. This study was approved by the Institutional Review Board for Research in Human Subjects at Faculty of Medicine, Chulalongkorn University (IRB. No 297/54) and Srinakharinwirot University (SWUEC/Ex 43/2555), Thailand.
Self-reported medication adherence was measured using the Thai version of the 8-Item Morisky Medication Adherence Scale® (MMAS-8) due to it being relatively short and validated in Thai patients with diabetes [15, 16]. Patients were interviewed face to face about their medication adherence at baseline. This questionnaire was validated, and tested for internal consistency (Cronbach’s alpha 0.67) and test–retest reliability (intraclass correlation coefficient 0.73) in Thai patients with CKD in our pilot study [17]. From the pilot study, patients with a low level of medication adherence were more likely to have poorer kidney function measured using eGFR, compared with those with higher levels of adherence. However, the total number of participants was not sufficient to estimate the relationship with statistical significance at the p < 0.05 level. This finding suggested that the degree of medication adherence could be classified into two groups, poor (MMAS < 6) and moderate-to-high adherence (6 ≤ MMAS ≤ 8). In this study, the questionnaire assessed adherence to all types of prescribed medications.
Regarding the definition of the primary outcome, progression of CKD was defined as either a decline in eGFR of at least 3 ml/min/1.73 m2/year or the initiation of renal replacement therapy [18]. The rate of a decline in eGFR over 12 months, for an individual, was estimated using the slope of the best fit linear regression line [19]. At least three measures of eGFR over a year, for each participant, were used to minimize any lack of precision in the rate of decline in eGFR [19, 20]. The secondary outcomes were uncontrolled blood pressure, HbA1c, and LDL. Uncontrolled blood pressure was defined as a mean blood pressure of more than 130/80 mm Hg [21]. Uncontrolled HbA1c was defined as a mean HbA1c of more than 7 % [21]. Finally, uncontrolled LDL was defined as a mean LDL of at least 100 mg/dl [21]. Such information was extracted from participants’ medical notes. The mean of these outcomes over 1 year was calculated using at least three measures of these levels from clinic readings.
The rate of a decline in eGFR at baseline was calculated using at least three measures of serum creatinine in the previous year. A baseline period of a mean blood pressure, HbA1c, and LDL was extracted data from participants’ medical notes in the 3–6 months prior to recruitment.
Existing proteinuria was a potential confounding factor of the progression of CKD, and was defined as 24-h urinary protein excretion rate over 300 mg/24 h in the 3–6 months prior to recruitment, a protein and creatinine ratio (PCR) more than 500 mg/g creatinine in the 3–6 months prior to the recruitment, an albumin and creatinine ratio (ACR) more than 300 mg/g, or at least 2+ urine dipstick protein measurements for diabetic patients in the 3–6 months prior to the recruitment or at least 1+ of urine dipstick protein measurement for non-diabetic patients in the 3–6 months prior to the interview date [21, 22].
Demographic characteristics are presented as frequencies with percentages. Univariate analyses were performed to determine any associations between the level of medication adherence and the progression of CKD. Multiple logistic regression analysis included all statistically significant factors from the univariate analyses to control confounding factors, such as age and sex. In addition, univariate and multiple logistic regression analyses were performed to determine any relationships between poor adherence and demographics. This model included all possible factors related to poor adherence from the questionnaire or medical notes, such as age, gender, education levels, the number of prescribed medications, and severity of CKD. Tests were two-tailed, and a p value <0.05 was considered statistically significant.
Results
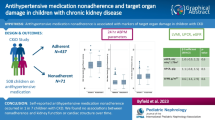
Of 339 patients recruited, 28 patients (8 %) died and 16 (5 %) were lost to follow up. Two hundred and ninety-five patients were followed up over the 12 months, and 18 patients received dialysis during the follow-up period (6 %). A flow chart of study population is shown in Fig 1. The mean age of these patients at baseline was 68 years (SD 12) and 52 % were female. Mean eGFR was 39 ml/min/1.73 m2 (SD 12). Figure 2 shows the distribution of change in eGFR over 12 months. The median follow-up period was 12 months (range 9–16). Ninety-five percent (n = 279) and 65 % (n = 193) had hypertension and diabetes, respectively. Twenty-two percent (n = 64) and 34 % (n = 99) received angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor antagonists, respectively. Patients received other medicines for CKD complications, such as erythropoietin (n = 57, 19 %), iron supplements (n = 94, 32 %), folic acid (n = 127, 43 %), vitamin B1-6-12 (n = 57, 19 %), loop diuretics (n = 82, 28 %), sodium or calcium polystyrene sulfonate (n = 57, 19 %), phosphate binders (n = 88, 30 %), sodium bicarbonate (n = 68, 23 %), and allopurinol (n = 98, 33 %).
Twenty-one percent of the patients (62 patients) had poor medication adherence at baseline, and 79 % (233 patients) had moderate-to-high adherence. Median number of prescribed medication at baseline was 8 items (range 2–20). The median number of pills per day at baseline was 11 pills (range 2–57). There was no difference in the number of pills per day between patients with poor (13, SD 7) and moderate-to-high medication adherence (13, SD 7).
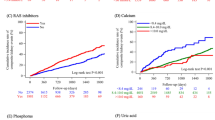
Among the low medication adherence group (n = 62), anti-hypertensive agents were the most frequently reported as not being taken (52 %), followed by hypoglycemic agents (39 %), and lipid-lowering agents (21 %), compared with other prescribed medicines. These patients could report more than one type of medicines that they forgot to take. Regarding medications for CKD complications, such as hyperphosphatemia and anemia, phosphate binders and iron supplements (19, 18 %) were commonly reported as poor adherence, followed by sodium bicarbonate (13 %) and folic acid (10 %).
Regarding reasons why patients with CKD did not adhere to their prescribed medications, forgetting to take their medications was the most frequently reported (n = 130, 44 %), followed by feeling of inconvenience in taking their medications every day (n = 88, 30 %), and missing taking their medications due to other reasons rather than forgetting (n = 81, 28 %). A small number of patients stopped using their medications when either they felt worse after taking medications (n = 29, 10 %), or their disease was under control (n = 12, 4 %).
Univariate analyses of potential factors related to the clinical outcomes between the groups of poor and moderate-to-high adherence are shown in Table 1. Younger age (<60 years) was more likely to have poor medication adherence (p < 0.01). No other statistically significant factors associated with poor adherence were found. In addition, there was no difference in eGFR at baseline between the poor and moderate-to-high adherence groups (38 ± 12 and 39 ± 12 ml/min/1.73 m2, p = 0.37).
Regarding multiple logistic regression analysis of associations between poor medication adherence and demographic characteristics, Younger patients were more likely to have poor medication adherence (adjusted odds ratio 2.81, 95 % CI 1.45–5.43). No other demographics were found to be associated with poor adherence (Table 2).
Table 3 shows the univariate analyses between potential risk factors at baseline and the primary outcome—the fast progression of CKD. Patients with poorer medication adherence and existing proteinuria were more likely to have faster progression of CKD (p < 0.01). Table 4 shows the multiple logistic regression analysis of the association between poor adherence and the progression of CKD over 1 year. Patients with poor medication adherence and existing proteinuria were associated with the progression of CKD (adjusted OR 1.96, 95 % CI 1.02–3.76 and adjusted OR 3.28, 95 % CI 1.90–5.69, respectively). Univariate and multiple logistic regression analyses of other outcomes, which were uncontrolled blood pressure, HbA1c and LDL, found no associations between poor adherence and these outcomes (uncontrolled BP adjusted ORage,sex 1.08, 95 % CI 0.58–2.01; uncontrolled HbAc adjusted ORage,sex 1.26, 95 % CI 0.63–2.53; and uncontrolled LDL adjusted ORage,sex 1.54, 95 % CI 0.81–2.93). However, there was a significant difference of five clinical cutoff points of BP between the poor and moderate-to-high adherence over 1 year (p < 0.01). The poor adherence group is less likely to control their blood pressure. The five clinical cutoff points of BP were (1) BP < 120/80 mm Hg, (2) BP = 120/80–130/80 mm Hg, (3) BP = 131/81–140/90 mm Hg, (4) BP > 140/90–150/90 mm Hg, and (5) BP > 150/90 mm Hg. The group of moderate-to-high adherence is more likely to control their blood pressure than the poor adherence (at BP < 120/80, 14 % of the adherence group vs. 9 % of the poor adherence group; at BP = 120/80–130/80, 23 % of the adherence group vs. 27 % of the poor adherence group; and at BP = 131/81–140/90, 35 % of the adherence group vs. 18 % of the poor adherence). Meanwhile, the proportion of the poor adherence at BP > 150/90 (26 %) was higher than another group (9 %).
Comparing the means of the four outcomes between the adherence groups showed that the low adherence group showed significantly poorer outcomes over the 12 months for eGFR −4.4 ± 6.7 ml/min/1.73 m2/year, and SBP 138 ± 15 mmHg and DBP 75 ± 9 for poor adherence, compared with −0.9 ± 7.4 ml/min/1.73 m2/year, and SBP 134 ± 12 mmHg and DBP 72 ± 8 mmHg for high adherence (t = 3.13, p < 0.01, t = −2.32, p < 0.05 and t = −2.31, p < 0.05, respectively), see Table 5.
Discussion
The mean age of participants in this study (68 years, SD 12) is consistent with the Thai population of CKD stages 2–4 (65 years, SD 13) [23]. Our study found similar levels of eGFR to the published literature (39 ml/min/1.73 m2, SD 12 vs. 42 ml/min/1.73 m2, SD 16), and the percentages of patients with hypertension (95 vs. 91 %) were also similar to published rates [23]. However, the proportion of women in our study (52 %) and those with diabetes (65 %) were higher than previous studies of CKD (44, 56 %, respectively) [23]. There was no difference in the mean number of medicines between the present study (8 items) and the literature among patients with CKD (6–12 items) [6, 7].
The rate of poor medication adherence in the present study (21 %) fell within the range of non-adherence seen in other studies of non-dialysis patients with CKD (8–33 %) [7–11]. Most participants did not take their medications due to forgetfulness. This finding is similar to Muntner’s study [11]. Feelings of inconvenience in taking medicines every day were the second frequently reported reason for non-adherence in our participants.
Our study showed that younger patients with CKD were more likely to have poor adherence to prescribed medications. However, associations between poor adherence and the number of pills, gender or educational level were not found. These findings are consistent with Muntner’s study [11]. The present study found no relationship between the severity of CKD and poor adherence. This finding is not consistent with a previous study which suggested that lower eGFR was associated with non-adherence [9]. However, that study measured adherence only to hypertensive agents, while our study evaluated adherence to all types of prescribed medications. This may account the difference in results, and in addition, the studies used different tools for measuring adherence.
The present cohort study is the first to report associations between poor medication adherence and the progression of CKD in non-dialysis patients with CKD. The findings suggest that a low level of medication adherence is associated with the progression of CKD, although the existing proteinuria had a stronger association with the progression of CKD, compared with poor adherence. Patients with moderate-to-high medication adherence are likely to have a slower progression of CKD. This may be because patients who adhere to medication are more likely to comply with diet control, such as restriction of protein intake and a high sugar diet. If patients comply with ACEIs, ARBs, their hypoglycemic agents, and the restriction of such diets, their kidney function is less likely to worsen. Our findings seem to confirm that statement. Patients with moderate-to-high medication adherence are more likely to control their sugar level and blood pressure than those with poor adherence. There were no purposive changes of patient care between the two groups during the baseline and study periods. Physicians took care of their patient as usual, and did not know which patients were classified into the poor group or moderate-to-high adherence groups.
Pharmacists, therefore, should provide strategies for patients with CKD to improve their medication adherence. Further studies should examine what intervention is suitable for solving this problem. Medication adherence is a factor related to these outcomes. Other factors which may have influenced these outcomes were not measured, such as consumption of a high-salt diet. In addition, the higher level of DBP in the poor adherence group may have been influenced by the higher proportion of younger patients and was more likely to have higher DBP [24]. Further studies of a high number of sample sizes are needed to examine these associations in patients with CKD to confirm the findings.
Limitations of this study are that this study did not examine several factors related to poor adherence, such as socioeconomic status, depressive symptoms and medications administered by a caregiver. Medication adherence was assessed by a self-report questionnaire in the present study, so this may have resulted in overestimates of adherence due to recall and social desirability bias. We measured medication adherence once at baseline, so some patients in the moderate-to-high adherence group may not have adhered to this level over the period of the study [8] and so the findings should be interpreted with caution. Finally, our study did not investigate barriers to medication adherence in patients with CKD.
In conclusion, the findings showed that a low level of adherence to prescribed medication in patients with CKD seem to contribute to the progression of CKD. Younger patients were more likely to report poor medication adherence. Therefore, health care providers should acknowledge these findings and provide effective strategies for patients with CKD to help them improve their adherence.
References
Egede LE, Gebregziabher M, Echols C, Lynch CP. Longitudinal effects of medication nonadherence on glycemic control. Ann Pharmacother. 2014;48:562–70.
Elperin DT, Pelter MA, Deamer RL, Burchette RJ. A large cohort study evaluating risk factors associated with uncontrolled hypertension. J Clin Hypertens. 2014;16:149–54.
Wong MC, Tam WW, Cheung CS, Wang HH, Tong EL, Sek AC, et al. Drug adherence and the incidence of coronary heart disease-and-stroke-specific mortality among 218,047 patients newly prescribed and antihypertensive medication: a five-year cohort study. Int J Cardiol. 2013;168:928–33.
Rifkin DE, Laws MB, Rao M, Balakrishnan V, Sarnak MJ, Wilson IB. Medication adherence behavior and priorities among older adults with CKD: a semi-structured interview study. Am J Kidney Dis. 2010;56:439–46.
McKillop G, Joy J. Patients’ experience and perceptions of polypharmacy in chronic kidney disease and its impact on adherent behaviour. J Ren Care. 2013;39:200–7.
Burnier M, Pruijm M, Wuerzner G, Santschi V. Drug adherence in chronic kidney disease and dialysis. Nephrol Dial Transpl. 2015;30:39–44.
Magacho EJC, Ribeiro LC, Chaoubah A, Bastos MG. Adherence to drug therapy in kidney disease. Braz J Med Biol Res. 2011;44:258–62.
Chang TI, Desai M, Solomon DH, Winkelmayer WC. Kidney function and long-term medication adherence after myocardial infarction in the elderly. Clin J Am Soc Nephrol. 2011;6:864–9.
Schmitt KE, Edie CF, Laflam P, Simbartl LA, Thakar CV. Adherence to antihypertensive agents and blood pressure control in chronic kidney disease. Am J Nephrol. 2010;32:541–8.
Vupputuri S, Muntner P, Winkelmayer WC, Smith DH, Nichols GA. Low medication adherence is related to poor hypertension control among patients with chronic kidney disease. Circulation. 2012;125:AP097.
Muntner P, Judd SE, Krousel-Wood M, McClellan WM, Safford MM. Low medication adherence and hypertension control among adults with CKD: data from the REGARDS (reasons for geographic and racial differences in stroke) study. Am J Kidney Dis. 2010;56:447–57.
Schmid H, Hartmann B, Schiffl H. Adherence to prescribed oral medication in adult patients undergoing chronic hemodialysis: a critical review of the literature. Eur J Med Res. 2009;14:185–90.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
Praditpornsilpa K, Townamchai N, Chawatanarat T, Tiranathanagul K, Katawatin P, Susantitaphong P, et al. The need for robust validation for MDRD-based glomerular filtration rate estimation in various CKD populations. Nephrol Dial Transpl. 2011;26:2780–5.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–54.
Sakthong P, Chabunthom R, Charoenvisuthiwongs R. Psychometric properties of the Thai version of the 8-item Morisky medication adherence scale in patients with type 2 diabetes. Ann Pharmacother. 2009;43:950–7.
Tangkiatkumjai M. Herbal and dietary supplement use in Thai patients with chronic kidney disease (CKD) and their association with progression of CKD. Nottingham: Primary care, University of Nottingham; 2014.
Chonchol M, Shlipak MG, Katz R, Sarnak MJ, Newman AB, Siscovick DS, et al. Relationship of uric acid with progression of kidney disease. Am J Kidney Dis. 2007;50:239–47.
National Kidney Foundation. Stratification of risk for progression of kidney disease and development of cardiovascular disease. Am J Kidney Dis. 2002;39:S170–212.
The National Collaborating Centre for Chronic Conditions (Great Britain). Chronic kidney disease: national clinical guideline for early identification and management in adults in primary and secondary care. 1st ed. London: Royal College of Physicians; 2008.
The Nephrology Society of Thailand. Clinical practice guidelines for pre-dialysis patients in 2009. 1st ed. Bangkok: The Nephrology Society of Thailand; 2009.
National Kidney Foundation. Evaluation of laboratory measurements for clinical assessment of kidney disease. Am J Kidney Dis. 2002;39:S76–110.
Chartsrisak K, Vipattawat K, Assanatham M, Nongnuch A, Ingsathit A, Domrongkitchaiporn S, et al. Mineral metabolism and outcomes in chronic kidney disease stage 2–4 patients. BMC Nephrol. 2013;14:14.
Sagie A, Larson MG, Levy D. The natural history of borderline isolated systolic hypertension. N Engl J Med. 1993;329:1912–7.
Sarnak MJ, Astor BC. Implications of proteinuria: CKD progression and cardiovascular outcomes. Adv Chronic Kidney Dis. 2011;18:258–66.
Acknowledgments
Permission to use the 8-Item MMAS was obtained from Professor Donald E. Morisky. We would like to thank Dr. Phantipa Sakthong for the permission to use the Thai version of this questionnaire, the participants and staff of the King Chulalongkorn Memorial Hospital and HRH Princess Maha Chakri Sirindhorn Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared no competing interests.
Funding
This study was funded by the Royal Thai Government.
About this article
Cite this article
Tangkiatkumjai, M., Walker, DM., Praditpornsilpa, K. et al. Association between medication adherence and clinical outcomes in patients with chronic kidney disease: a prospective cohort study. Clin Exp Nephrol 21, 504–512 (2017). https://doi.org/10.1007/s10157-016-1312-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-016-1312-6