Abstract
Background
To derive and validate a risk score for prediction of contrast-induced nephropathy (CIN) in the Chinese patients undergoing cardiac catheterization.
Methods
The hospital medical records of 3945 patients undergoing coronary angiography or percutaneous coronary intervention were reviewed. Patients were randomly assigned into two cohorts: one was for derivation of risk score (n = 2764) and another for validation (n = 1181). The CIN was defined as an increase of serum creatinine level ≥44.2 μmol/L or ≥25 % and beyond its upper limit of normal value within 72 h following the procedure. On the basis of the odds ratio obtained from multivariate logistic regression, risk score of CIN was built up. The discrimination of the risk score was assessed using the area under the receiver operating characteristic curve and the calibration was assessed using the Hosmer–Lemeshow goodness-of-fit test.
Results
The incidences of CIN in the derivation and validation cohorts were 4.6 and 4.2 %, respectively. Independent predictors included age >60 years, hypertension, acute myocardial infarction, heart failure, use of intra-aortic balloon pump, decreased glomerular filtration rate and contrast volume >100 mL. The incidence of CIN was increased with increment of risk score. Both the derivation and validation cohorts showed adequate discrimination (an area under the ROC curve, 0.76 and 0.71, respectively) and good calibration (Hosmer–Lemeshow statistic test, P = 0.50 and P = 0.54, respectively).
Conclusion
A simple risk score for prediction of CIN development after cardiac catheterization in Chinese patients was built up by this study. Use of this risk score may help clinicians to perform early preventative strategies to minimize the risk of CIN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Contrast-induced nephropathy (CIN) is an acute renal injury resulted from the renal toxicity of iodinated contrast media. Now contrast media are widely used on the world [1, 2] and CIN has become the third most common cause of hospital-acquired acute renal failure [3]. Furthermore, the development of CIN has been associated with prolonged hospitalization, increased health care costs, especially, increased in-hospital and long-term mortality [4, 5]. Once CIN occurred, treatment of CIN is rather limited and only supportive measures and dialysis can be provided. The principal method to tackle this complication is prevention. Therefore, timely risk assessment will help clinicians to focus on especially vulnerable patients and to offer a greater opportunity to implement intensive prevention strategies for these patients. So, the present study is going to derive a risk score from a Chinese cohort that could be readily applied by clinicians to predict CIN risk for the patients undergoing cardiac catheterization.
Materials and methods
Patients
All the adult patients undergoing cardiac catheterization including coronary angiography or percutaneous coronary intervention (PCI) in our hospital during 2005, 2006 and the first half of 2010 were consecutively collected. Excluded criteria were as follows: lacking sufficient inspection of serum creatinine (SCr); pre-existing end-stage renal disease requiring dialysis; other contrast exposure in the 1 week before procedure or in the 3 days after procedure; coronary artery bypass grafting in the 3 days after procedure; death in the first 24 h after procedure. In addition, patients who received intravenous hydration before and after the procedure were also excluded. In the all cases, only non-ionic low-osmolar (iopromide, iohexol) or iso-osmolar (iodixanol) contrast media were used for all the procedures. The study was approved by the Ethics Committee of Beijing Anzhen Hospital (approval number 2013012).
Definitions
Contrast-induced nephropathy was defined as an increase in SCr level ≥44.2 μmol/L or ≥25 % and simultaneously beyond the upper limit of normal value within 72 h following the intravascular administration of contrast media [6].
Hypertension was defined according to systolic/diastolic blood pressure >140/90 mmHg or patients had a history of hypertension and current use of any antihypertensive medication.
Hypotension was defined as systolic blood pressure <80 mmHg requiring inotropic support with medications or intra-aortic ballon pump (IABP).
Hear failure included advanced congestive heart failure (New York Heart Association functional class III/IV) or acute heart failure (Killip class II–IV).
Glomerular filtration rate estimating equation
Estimated glomerular filtration rate (eGFR) was calculated using the modified abbreviated MDRD equation for Chinese patients: 175 × SCr (mg/dL)−1.234 × age−0.179 (×0.79 for women) [7].
Statistical analysis
The patients enrolled in the study were randomly divided into two groups, derivation group (70 % patients) and validation group (30 % patients), by a simple randomization via the software SPSS. The number of patients in derivation group could meet the requirement of the test sample size which was estimated by the following formula:
The continuous variables with normal distribution were presented as mean ± standard deviation and those with non-normal distribution as median and interquartile range. The categorical variables were presented as percentages. The comparison between two groups was performed by using the t test for normally distributed continuous variables, Wilcoxon Mann–Whitney test for non-normally distributed continuous variables and Chi-square test or Fisher exact test for categorical variables.
Variables with P < 0.2 in univariate analysis were included in multivariable steptwise logistic regression analysis until variables with a P value <0.05 remained as predictors of CIN. Based on the odds ratio, the independent predictors of CIN were assigned weighted integers. Discrimination of the risk score was assessed using the area under the receiver operating characteristic (ROC) curve. Calibration was assessed using the Hosmer–Lemeshow goodness-of-fit test and satisfied when P value was >0.05.
All the statistical analyses were performed using the software SPSS version 15.0 and statistical significance was defined as P < 0.05.
Results
Incidence of CIN and in-hospital outcome
The incidence of CIN in the total patients was 4.5 % (177/3945), and during the earlier period (2005–2006) and recently (2010) was 4.7 % (74/1584) and 4.4 % (104/2361), respectively. There was no significant difference of CIN incidence between these two periods (P > 0.05). Among these patients, there were 4.8 % (138/2846) patients with CIN in the PCI group and 3.5 % (39/1099) patients with CIN in the coronary angiography group. No significant difference in CIN incidences between these two groups was found (P = 0.07).
The patients with CIN had poor in-hospital outcome. Their hospital stay was significantly prolonged with a median of 9.0 days (interquartile range 5.0–14.0), compared with 6.0 days (4.0–9.0) in the patents without CIN (P < 0.001). Their in-hospital mortality was also significantly increased to 11.3-fold compared to that in the patients without CIN (3.4 vs 0.3 %, P < 0.001).
Baseline characteristics and univariate analysis
The demographic data, clinical data, baseline laboratory data, and cardiac catheterization procedure data of the patients in derivation cohort are shown in Table 1.
The univariate comparison of potential predictor variables between CIN and non-CIN patients in the derivation cohort is also shown in Table 1. A total of 16 variables with P < 0.2 were involved in the multivariable logistic regression model, but the data of hypoalbuminemia and left ventricular ejection fraction were excluded because their measurement data were absent in more than 10 % of study subjects.
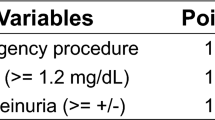
Multivariable analysis and derivation of risk score
The results of multivariable logistic regression analysis in 2671 patients, representing 96.6 % of the total patients, in the derivation cohort are shown in Table 2. Based on the odds ratio, a weighted integer score was assigned to each identified risk factor. The Youden index (sensitivity + specificity − 1) [8] was calculated, and the best cut-off in our risk score was 5 points with sensitivity of 69.3 % and specificity of 69.4 %. Moreover, the risk score was further divided into the following four groups: low risk (score 0–4, CIN incidence 1.2 %), moderate risk (score 5–8, CIN incidence 6.3 %), high risk (score 9–11, CIN incidence 16.8 %) and very high risk (score ≥12, CIN incidence 27.3 %).
The prediction score showed adequate discrimination between patients who did and did not develop CIN (an area under the ROC curve of 0.76, 95 % CI 0.72–0.80) (Fig. 1). It was well calibrated across deciles of observed and expected risks (Hosmer–Lemeshow statistic Chi-square value was 7.36, P = 0.50) (Fig. 2).
Validation of prediction score
The incidence of CIN was 6.6 % in patients with scores ≥5 points and 1.8 % in patients with <5 points. An adequate discriminative power was also demonstrated in the validation dataset with an area under the ROC curve of 0.71 (95 % CI 0.63–0.79) (Fig. 1). The results of Hosmer–Lemeshow test in the validation dataset were not statistically significant with Chi-square value 6.97, P = 0.54 (Fig. 2).
External validation of Mehran’s prediction score
The widely used Mehran risk score was created in 2004 based on the definition of CIN, a SCr increase of ≥0.5 mg/dL and/or ≥25 % at 48 h after intravascular administration of contrast media [9], and was consisted of 8 prediction factors, i.e., hypotension, IABP, congestive heart failure, age >75 years, anemia, diabetes mellitus, contrast volume and eGFR decease or SCr increase. The external validation of Mehran risk score was performed by us using the above definition in total 3945 patients and it achieved an area under the ROC curve of 0.57 (95 % CI 0.54–0.60), while the area under the ROC curve of the present risk score using our revised definition was 0.75 (95 % CI 0.71–0.78). In addition, the CIN incidence in patients with 0 point was 8.8 % in Mehran risk score, while zero in our score.
Discussion
In the literatures, different definitions of CIN were applied [9–15], of which the definition developed by Contrast Media Safety Committee (CMSC) of European Society of Urogenital Radiology (ESUR) in 1999 was most widely used [16]. The CIN was defined as “an impairment in renal function (an increase in SCr by more than 25 % or 44 μmol/L) occurs within 3 days following the intravascular administration of contrast medium in the absence of an alternative etiology” [16]. However, some authors and ourselves found that the criterion of relative increase in SCr might be over-sensitive, leading to an increase in the number of false-positive diagnoses, especially in the patients with normal lower level of baseline SCr [6, 13–15, 17]. The CMSC of ESUR has taken note for this issue, but so far has no mature proposals how to revise the definition, only suggesting “to wait for the possible future changes advised by nephrological experts” [13]. It has been recognized that minor changes of SCr after contrast administration are frequent but usually without any clinical relevance [17–19]. Therefore, we proposed that the diagnosis of CIN should firstly meet the ESUR criteria, and, besides this, the post-procedure SCr value also needed to exceed its upper limit of normal value [6]. The revised diagnostic criteria have been applied in our clinical practice and are particularly suitable for the patients with normal lower level of baseline SCr.
In our study, the CIN incidence was 4.5 %, which is lower than some of other studies [9–11]. In the literatures the reported incidence of CIN varies widely, which might be related to the study population who had less or more risk factors and to the CIN diagnostic criteria which were relatively stringent or loose [17]. In the present study, the renal function in a quite high proportion of patients (89.6 %) was normal or only mild damaged (i.e., eGFR ≥60 mL/min/1.73 m2), and more stringent revised ESUR criteria were used for CIN diagnosis, which might be the causes of low CIN incidence in our patients.
Because literature reported that the incidence of CIN was obviously decreased over the past years owing to promotion of technology [20], we separately collected the cases of earlier period (2005–2006) and the recent period (2010). However, no significant difference of CIN incidence between these two periods was found, so finally these two parts data were put together to analyze CIN risk factors and to derive risk score.
In our risk score, the baseline renal function was one of the strongest predictors for CIN development, which is consistent with previous studies [9–12]. The risk odds of CIN in the patients with baseline eGFR <30 mL/min/1.73 m2 were almost 6.5 times higher than that with eGFR ≥90 mL/min/1.73 m2. Because the compensatory capacity of kidney diminished in the patients with renal insufficiency, it is easier to develop acute kidney injury affected by nephrotoxic agents, including contrast media. For the similar reason, the age of >60 years was also an independent predictor of CIN, because a number of structural and functional degenerative changes in kidneys could make old persons prone to CIN [21, 22].
Our study found that hypertension was also an independent predictor of CIN, which is consistent with the result of previous study [23]. Many patients with persistent hypertension have renal pathological changes such as arteriolosclerosis, which often results in renal tissue ischemia and loss of nephrons. So, it is possible that hypertensive patients are susceptible to CIN after contrast media exposure [23].
The volume of contrast media is a main modifiable risk factor in the development of CIN. According to different sources, the relatively safe cut-off point of contrast volume varied from 70 mL up to 220 mL [24]. Our study showed that the contrast volume >100 mL was associated with a significantly higher risk of CIN and the CIN risk would be increased with the increment of contrast volume.
AMI was also one of risk factors in our study, which was only reported by Bouzas-Mosquera [10] in the urgent cardiac catheterization. Because of hemodynamic instability and unfeasibility of adequate prophylaxis, patients with AMI undergoing urgent PCI are prone to kidney hypoperfusion and then the development of CIN [25].
Two variables, the heart failure and use of IABP, were also strong independent predictors of CIN in our risk score. Heart failure, likely due to a reduced effective arterial blood volume and its effect to decrease GFR, enhances the likelihood of developing CIN after contrast media exposure [2]. IABP may result in the partial occlusion of the renal blood flow if it is positioned too low, which also promotes the development of CIN after contrast media exposure [9].
Many studies have shown that diabetes is a predictor of CIN [9–12, 26]. However, data from our study did not confirm these previous observations. This difference might relate to a high proportion (83 %) of patients with diabetes who had normal renal function in our study. In an earlier prospective controlled study, the risk of CIN in patients with diabetes and normal renal function was not higher than in control patients [27]. In 2006, the CIN Consensus Working Panel stated: “it is not clear whether the risk of CIN is significantly increased in patients with diabetes who do not have renal impairment” [20] and the updated CMSC of ESUR guidelines published in 2011 also hold the same opinion [13]. It needs further studies to clarify this issue.
Since 2004 several risk scores have been created for prediction of CIN [9–12, 26, 28], these risk scores were different in the research objects, CIN diagnostic criteria and assessed variables. Among these risk scores, Mehran risk score has been widely used on the world for CIN prediction, including recent application to the patients with ST-elevation myocardial infarction treated with PCI in Italy and Turkey [29, 30]. Because the Mehran risk score may be a valuable predictive tool, we chose it, as a reference, to perform an external validation in our 3945 patients. In the original validation population of Mehran risk score, the area under ROC curve was 0.67 [9], but the discriminative power of Mehran risk score in our patients was lower with an area under ROC curve of 0.57 (95 % CI 0.54–0.60), which is quite similar to the result of external validation in the Italy study, 0.57 (95 % CI 0.52–0.62) [30]. These facts suggest that a risk score tends to be more accurate in the population from which it was derived. So, it should be necessary to develop a risk score in Chinese population for prediction of CIN after cardiac catheterization.
There are several limitations in the present study. First, this is a retrospective analysis, so its inherent weakness cannot be avoided. For example, some clinical variables such as hypoalbuminemia and left ventricular ejection fraction could not be included in multivariable logistic regression analysis because these data in medical records were not complete. Second, the statistical power of this study might not be very strong because our risk score was derived and validated by a single center. For the widely application of the risk score a multicenter prospective validation is still needed. Finally, the risk score could only evaluate the short-term in-hospital CIN risk without the information of long-term outcome.
Conclusion
A simple risk score for prediction of CIN development after cardiac catheterization in Chinese patients was derived and validated by this study. Use of this risk score may help clinicians to perform early preventative strategies to minimize the risk of CIN.
References
Erselcan T, Egilmez H, Hasbek Z, et al. Contrast-induced nephropathy: controlled study by differential GFR measurement in hospitalized patients. Acta Radiol. 2012;53:228–32.
Cronin RE. Contrast-induced nephropathy: pathogenesis and prevention. Pediatr Nephrol. 2010;25:191–204.
Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–6.
Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259–64.
Lakhal K, Ehrmann S, Chaari A, et al. Acute kidney injury network definition of contrast-induced nephropathy in the critically ill: incidence and outcome. J Crit Care. 2011;26:593–9.
Li D, Gao Y, Cheng H, et al. Comparative study of diagnosis for contrast-induced nephropathy by ESUR and modified ESUR definitions. Chin J Pract Intern Med. 2011;31:938–40.
Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–44.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–5.
Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393–9.
Bouzas-Mosquera A, Vazquez-Rodriguez JM, Calvino-Santos R, et al. Contrast-induced nephropathy and acute renal failure following emergent cardiac catheterization: incidence, risk factors and prognosis. Rev Esp Cardiol. 2007;60:1026–34.
Maioli M, Toso A, Gallopin M, et al. Preprocedural score for risk of contrast- induced nephropathy in elective coronary angiography and intervention. J Cardiovasc Med (Hagerstown). 2010;11:444–9.
Bartholomew BA, Harjai KJ, Dukkipati S, et al. Impact of nephropathy after percutaneous coronary intervention and a method for risk stratification. Am J Cardiol. 2004;93:1515–9.
Stacul F, van der Molen AJ, Reimer P, et al. Contrast induced nephropathy: updated ESUR Contrast Media Safety Committee guidelines. Eur Radiol. 2011;21:2527–41.
Reddan D, Laville M, Garovic VD. Contrast-induced nephropathy and its prevention: what do we really know from evidence-based findings? J Nephrol. 2009;22:333–51.
Waikar SS, Bonventre JV. Creatinine kinetics and the definition of acute kidney injury. J Am Soc Nephrol. 2009;20:672–9.
Morcos SK, Thomsen HS, Webb JA. Contrast-media-induced nephrotoxicity: a consensus report. Contrast Media Safety Committee, European Society of Urogenital Radiology (ESUR). Eur Radiol. 1999;9:1602–13.
Budano C, Levis M, D’Amico M, et al. Impact of contrast-induced acute kidney injury definition on clinical outcomes. Am Heart J. 2011;161:963–71.
Jabara R, Gadesam RR, Pendyala LK, et al. Impact of the definition utilized on the rate of contrast-induced nephropathy in percutaneous coronary intervention. Am J Cardiol. 2009;103:1657–62.
Toprak O. What is the best definition of contrast-induced nephropathy? Ren Fail. 2007;29:387–8.
Mccullough PA, Adam A, Becker CR, et al. Risk prediction of contrast-induced nephropathy. Am J Cardiol. 2006;98:27K–36K.
Musso CG, Liakopoulos V, Ioannidis I, et al. Acute renal failure in the elderly: particular characteristics. Int Urol Nephrol. 2006;38:787–93.
Abdel-Kader K, Palevsky PM. Acute kidney injury in the elderly. Clin Geriatr Med. 2009;25:331–58.
Conen D, Buerkle G, Perruchoud AP, et al. Hypertension is an independent risk factor for contrast nephropathy after percutaneous coronary intervention. Int J Cardiol. 2006;110:237–41.
Toprak O. Risk markers for contrast-induced nephropathy. Am J Med Sci. 2007;334:283–90.
Marenzi G, Lauri G, Assanelli E, et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2004;44:1780–5.
Brown JR, DeVries JT, Piper WD, et al. Serious renal dysfunction after percutaneous coronary interventions can be predicted. Am Heart J. 2008;155:260–6.
Parfrey PS, Griffiths SM, Barrett BJ, et al. Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both. A prospective controlled study. N Engl J Med. 1989;320:143–9.
Tziakas D, Chalikias G, Stacos D, et al. Development of an easily applicable risk score model for contrast-induced nephropathy prediction after percutaneous coronary intervention: a novel approach tailored to current practice. Int J Cardiol. 2013;163:46–55.
Sgura FA, Bertelli L, Monopoli D, et al. Mehran contrast-induced nephropathy risk score predicts short- and long-term clinical outcomes in patients with ST-elevation-myocardial infarction. Circ Cardiovasc Interv. 2010;3:491–8.
Aykan AC, Gul I, Gokdeniz T, et al. Is coronary artery disease complexity valuable in the prediction of contrast induced nephropathy besides Mehran risk score, in patients with ST elevation myocardial infarction treated with primary percutaneous coronary intervention? Heart Lung Circ. 2013;. doi:10.1016/j.hlc.2013.03.085.
Acknowledgments
We really appreciate Prof. Dong Zhao and Prof. Jing Liu for their constructive comments concerning statistical analyses.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Gao, Ym., Li, D., Cheng, H. et al. Derivation and validation of a risk score for contrast-induced nephropathy after cardiac catheterization in Chinese patients. Clin Exp Nephrol 18, 892–898 (2014). https://doi.org/10.1007/s10157-014-0942-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-014-0942-9