Abstract
Background
The aim of this study was to determine whether perioperative stress hyperglycemia is correlated with surgical site infection (SSI) rates in non-diabetes mellitus (DM) patients undergoing elective colorectal resections within an SSI bundle.
Methods
American College of Surgeons National Surgical Quality Improvement Program data of patients treated at a single institution in 2006–2012 were supplemented by institutional review board-approved chart review. A multifactorial SSI bundle was implemented in 2009 without changing the preoperative 8-h nil per os, and in the absence of either a carbohydrate loading strategy or hyperglycemic management protocol. Hyperglycemia was defined as blood glucose level > 140 mg/dL. The primary endpoint was SSI defined by the Centers for Disease Control National Nosocomial Infections Surveillance.
Results
Of 690 patients included, 112 (16.2%) had pre-existing DM. Overall SSI rates were significantly higher in DM patients as compared to non-DM patients (28.7 vs. 22.3%, p = 0.042). Postoperative hyperglycemia was more frequently seen in non-DM patients (46 vs. 42.9%). The SSI bundle reduced SSI rates (17 vs. 29.3%, p < 0.001), but the rate of hyperglycemia remained unchanged for DM or non-DM patients (pre-bundle 59%; post-bundle 62%, p = 0.527). Organ/space SSI rates were higher in patients with pre- and postoperative hyperglycemia (12.6%) (p = 0.017). Overall SSI rates were higher in DM patients with hyperglycemia as compared to non-DM patients with hyperglycemia (35.6 vs. 20.8%, p = 0.002). At multivariate analysis DM, chronic steroid use, chemotherapy and SSI bundle were predictive factors for SSI.
Conclusions
This study showed that non-DM patients have a postoperative hyperglycemia rate as high as 46% in spite of the SSI bundle. A positive correlation was found between stress hyperglycemia and organ/space SSI rates regardless of the DM status. These data support the need for a strategy to prevent stress hyperglycemia in non-DM patients undergoing colorectal resections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Being the third most common nosocomial infection, surgical site infection (SSI) represents a major source of postoperative morbidity and mortality in colorectal surgery with rates as high as 30% and is responsible for annual costs of up to 10 billion dollars in the USA [1,2,3,4]. Despite the identification of SSI as a patient safety priority by the Centers for Medicaid and Medicare Services and the Joint Commission on the Accreditation of Healthcare Organizations and the development of several accountability measures (such as appropriate timing and adequate selection of antibiotics and preoperative glucose control) SSI still remains a significant burden in colorectal surgery [5]. In addition, there is controversy regarding the relative impact of stress-induced hyperglycemia in non-diabetes mellitus (DM) patients.
Stress hyperglycemia is defined as acute, transient elevations in blood glucose concentrations occurring during illness [6]. It arises as a result of a cascade of normal physiologic response to injury leading to the alteration of endogenous hormone production and metabolites, including increased serum cortisol production, insulin resistance, and subsequent hyperglycemia [7]. Stress hyperglycemia appears to be associated with increased risk of SSI in colorectal patients, especially in the absence of pre-existing DM [8, 9]. In 2003 Ljungqvist and Søreide suggested that preoperative carbohydrate loading resulted in improved insulin sensitivity for as long as 72 h postoperatively [10]. Since then a number of studies have confirmed this and other benefits associated with carbohydrate loading compared to the standard 8 h nil per os (NPO) strategy for surgical patients, however, with little mention of hyperglycemia [11, 12]. Recently, the PROCY study (comparing preoperative oral intake of 800 mL of water containing 100 g of maltodextrin to 800 mL of water) found no benefit in terms of SSI reduction (16.3 vs. 16.0%) although the rate of perioperative hyperglycemia was lower after carbohydrate loading (24.2 vs. 57.4%) [13]. Therefore, it appears that a strategy for reducing the rate of hyperglycemia below 10% may be required to impact the SSI rate.
The aim of this study was to determine whether perioperative stress hyperglycemia is correlated with SSI rates in non-DM patients undergoing elective colorectal resection within an SSI bundle.
Materials and methods
Study design and endpoint
This study was carried out as a retrospective cohort study of patients undergoing major colorectal surgery. National Surgical Quality Improvement Program (NSQIP) database was utilized to study demographic and perioperative variables which may be associated with surgical site infection (SSI) rates. The NSQIP participant use data files (PUF) of the patients treated in our institution from 2006 to 2012 were queried and collected as a study population which then was narrowed to those patients who had abdominal colorectal surgery. SSI was determined as the primary endpoint. Demographic and perioperative factors were collected and compared for SSI which was defined by the Centers for Disease Control (CDC) National Nosocomial Infections Surveillance System [14]. This study was designed according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [15].
Patient identification, collected data and definitions
NSQIP database was accessed and patients operated on by a single surgeon were identified using Current Procedural Terminology (CPT) codes. Collected data included demographics, such as age, gender, and body mass index (BMI); perioperative blood test values, including preoperative and postoperative blood glucose levels; date and type of procedure; wound classification; and American Society of Anesthesiologists (ASA) classification. Among comorbidities, DM was the one of interest which was defined in NSQIP as “metabolic disorder of the pancreas whereby the individual requires daily doses of exogenous parenteral insulin or a non-insulin anti-diabetic agent to prevent a hyperglycemia/metabolic acidosis” [16]. Among postoperative complications, SSI was the one of interest which consisted of superficial incisional, deep incisional, and organ/space surgical site infections. Hyperglycemia was defined as a blood glucose level of more than 140 mg/dL. Preoperative hyperglycemia was defined as a blood glucose level of more than 140 mg/dL on the morning of surgery in elective cases, and within 3 h prior to surgery in emergency cases. Postoperative hyperglycemia was defined as a blood glucose level of more than 140 mg/dL within 72 h postoperatively. SSI bundle was introduced in 2009 by our institution and consisted of pre-hospital and pre-, intra- and postoperative components, which were described in our previous study in detail (Fig. 1) [17]. Superficial SSI was defined in NSQIP as an infection that occurs within 30 days after the operation and the infection involves only skin or subcutaneous tissue of the incision; deep SSI was defined as an infection that occurs within 30 days after the operation and the infection appears to be related to the operation and infection involved deep soft tissues (e.g., fascial and muscle layers) of the incision; organ/space SSI was defined as an infection that occurs within 30 days after the operation and the infection appears to be related to the operation and the infection involves any part of the anatomy (e.g., organs or spaces), other than the incision, which was opened or manipulated during an operation [16].
Statistical analysis
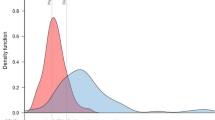
Statistical analysis was performed using SPSS software (version 18; SPSS Inc., Chicago, IL, USA). Mean and standard deviation were used as descriptive statistics for continuous variables, whereas percentage and ratio were used to express categorical variables. The data were tested for normality using normality tests (Kolmogorov–Smirnov and Shapiro–Wilk tests) and histograms. Unpaired t test and one-way ANOVA were utilized to compare independent continuous variables between two and four groups, respectively, whereas Chi-squared test and odds ratio (OR) were utilized to compare categorical variables. Multivariate logistic regression model was utilized to compare impacts of different factors on SSI rates. Statistical significance was defined as p ≤ 0.05.
Results
A total of 690 patients were included in the study and comparison of pre-SSI bundle versus post-SSI bundle patients demonstrated similar demographic characteristics (Table 1). The only significant difference between the two was a higher use of laparoscopic resection in the post-SSI bundle period (35.7% after 2009 vs. 26.1% before 2009). Implementation of the bundle significantly reduced the rate of SSI, mostly due to a reduction in superficial SSI (Table 1).
The prevalence of DM in both periods was similar (DM-15.3% vs. non-DM-17.4%), as was the rate of postoperative hyperglycemia (pre-SSI Bundle-59.4% vs. post-SSI Bundle-61.7%). As expected, the DM population had a higher BMI, ASA score, as well as mean glucose levels (Table 2). Pre- and postoperative mean glucose levels were higher in DM patients; however, the mean postoperative glucose level was above the threshold of 140 mg/dL for both DM and non-DM patients. Importantly, the incidence of postoperative hyperglycemia was similar between the DM and non-DM groups (42.9 vs. 46%).
Patients were also stratified according to perioperative blood glucose levels into four groups: pre- and postoperative normoglycemia; preoperative hyperglycemia only; postoperative hyperglycemia only; and both pre- and postoperative hyperglycemia (Table 3). The data demonstrated that total and incisional SSI rates were similar, organ/space SSI rates were higher in both pre- and postoperative hyperglycemia group (12.6%) (p = 0.017). SSI rates were also analyzed in DM hyperglycemic versus non-DM hyperglycemic patients (Table 4). Overall SSI rates were significantly higher in DM hyperglycemic patients (p = 0.002), and there was a trend toward higher superficial incisional SSI rates in this group (p = 0.078) compared to non-DM hyperglycemic patients. However, deep incisional and organ/space SSI rates did not significantly differ (Table 4).
Discussion
The main finding of our study was that non-DM patients were found to have a postoperative hyperglycemia rate as high as 46% in spite of the SSI bundle. Our study also reported a positive correlation between stress hyperglycemia and organ/space SSI rates regardless of the DM status.
Recent studies reemphasized the expected impact of poorly controlled DM on SSI rates [18] and length of hospital stay [19, 20] after colorectal surgery. Conversely, the impact of perioperative stress hyperglycemia on SSI rates is not widely recognized in non-DM patients [18]. Stress-induced hyperglycemia can occur in 30–40% of surgical patients; however, the incidence depends on the degree of surgical stress [9, 21, 22]. The PROCY randomized controlled trial demonstrated that preoperative carbohydrates loading can decrease the rate of stress hyperglycemia when compared to placebo (water) (24 vs. 57%) [13]. The PROCY data, and the existing data on carbohydrate loading [23] suggest that, although a prophylaxis strategy can reduce stress hyperglycemia, all patients should be treated as there is no predictive model for who is at risk. The recent study by Keilhorn et al. [24] suggested that a lower dose of carbohydrate loading coupled with citrulline supplementation might be more effective in reducing the rate of perioperative hyperglycemia to as low as 7%. In our study, postoperative hyperglycemia occurred in 46% of non-DM patients and such rates did not change after implementation of our SSI bundle. This is likely due to the fact that we did not reduce the preoperative NPO duration of 8 h and did not use a carbohydrate loading strategy.
The concept of an SSI bundle was first introduced by the Institute for Healthcare Improvement (IHI) in 2001 and was defined as 3 or more evidence-based interventions implemented in a consistent manner with the potential to prevent SSI [25]. While specific interventions may vary in different institutions, it is the bundle approach that is expected to reduce SSI rates. A recent meta-analysis including 8515 patients found SSI rates to be significantly lower in patients complying with an SSI bundle as compared to a control group (7.0 vs. 15.1%, p = 0.0005) [26]. However, none of the cohort studies included in the abovementioned meta-analysis provided data on stress hyperglycemia. In our study, the SSI bundle significantly reduced overall and superficial incisional SSI rates (p < 0.001). However, there were no differences in postoperative hyperglycemia rates (62 vs. 59%). Several studies found a positive correlation between stress hyperglycemia and SSI rates regardless of the DM status [27,28,29]. Our study also reported a positive correlation between stress hyperglycemia and organ/space SSI rates regardless of the DM status.
The authors acknowledge that the current study has some limitations. First, the complication rates could have been underestimated since the NSQIP database only keeps records of 30-day follow-up data. Second, a retrospective single-center study might have methodological pitfalls imposed by selection bias. Further prospective studies are needed to confirm these findings.
Conclusions
This study showed that non-DM patients have a postoperative hyperglycemia rate as high as 46% in spite of the SSI bundle. A positive correlation was found between stress hyperglycemia and organ/space SSI rates regardless of the DM status. These data support the need for a strategy to prevent stress hyperglycemia in non-DM patients undergoing colorectal resections.
References
Keenan JE, Speicher PJ, Thacker JK et al (2014) The preventative surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg 149(14):1045–1052
Tanner J, Khan D, Ball J et al (2009) Post discharge surveillance to identify colorectal surgical site infection rates and costs. J Hosp Infect 72(3):242–250
Thompson KM, Oldenburg WA, Deschamps C et al (2011) Chasing zero: the drive to eliminate surgical site infections. Ann Surg 254(3):430–436 discussion 436–437
Mahmoud NN, Turpin RS, Yang G, Saunders WB (2009) Impact of surgical site infections on length of stay and costs in selected colorectal procedures. Surg Infect (Larchmt) 10(6):539–544
The Joint Commission Accountability Measure List (2015). https://www.jointcommission.org/assets/1/18/ACCOUNTABILITYMEASURESList_2014_May2015.pdf. Accessed 22 Mar 2017
Dungan KM, Braithwaite SS, Preiser JC (2009) Stress hyperglycemia. Lancet 373(9677):1798–1807
May AK, Kauffmann RM, Collier BR (2011) The place for glycemic control in the surgical patient. Surg Infect 12(5):405–418
Kwon S, Thompson R, Delinger P, Yanez D, Farrohki E, Flum D (2013) Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg 257(1):8–14
McConnell YJ, Johnson PM, Porter GA (2009) Surgical site infections following colorectal surgery in patients with diabetes: association with postoperative hyperglycemia. J Gastrointest Surg 13(3):508–515
Ljungqvist O, Søreide E (2003) Preoperative fasting. Br J Surg 90(4):400–406
Ramos M, Khalpey Z, Lipsitz S et al (2008) Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg 248(4):585–591
Hanazaki K, Maeda H, Okabayashi T (2009) Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol 15(33):4122–4125
Gianotti L, Biffi R, Sandini M et al (2007) Preoperative oral carbohydrate load versus placebo in major elective abdominal surgery (PROCY): a randomized, placebo-controlled, multicenter, phase III trial. Ann Surg. https://doi.org/10.1097/SLA.0000000000002325
Horan TC, Gaynes RP, Martone WJ et al (1992) CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 13(10):606–608
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 147(8):573–577
User Guide for the 2014 ACS NSQIP Participant Use Data File (PUF), American College of Surgeons, Chicago, IL (2014). https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2014.ashx. Accessed 22 Mar 2017
Connolly TM, Foppa C, Kazi E, Denoya PI, Bergamaschi R (2016) Impact of a surgical site infection reduction strategy after colorectal resection. Colorectal Dis 18(9):910–918
Martin ET, Kaye KS, Knott C et al (2016) Diabetes and risk of surgical site infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 37(1):88–99
Bower WF, Jin L, Underwood MJ et al (2010) Overt diabetes mellitus adversely affects surgical outcomes of noncardiovascular patients. Surgery 147(5):670–675
Ceriello A, Esposito K, Piconi L et al (2008) Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes 57(5):1349–1354
Thompson RE, Broussard EK, Flum DR, Wisse BE (2016) Perioperative glycemic control during colorectal surgery. Curr Diab Rep 16(3):32
Kiran RP, Turina M, Hammel J, Fazio V (2013) The clinical significance of an elevated postoperative glucose value in nondiabetic patients after colorectal surgery: evidence for the need for tight glucose control? Ann Surg 258(4):599–604 discussion 604–605
Vigano J, Cereda E, Caccialanza R et al (2012) Effects of preoperative oral carbohydrate supplementation on postoperative metabolic stress response of patients undergoing elective abdominal surgery. World J Surg 36(8):1738–1743
Kielhorn BA, Senagore AJ, Asgeirsson T (2017) The benefits of a low dose complex carbohydrate/citrulline electrolyte solution for preoperative carbohydrate loading: focus on glycemic variability. Am J Surg. https://doi.org/10.1016/j.amjsurg.2017.10.029
Institute for Healthcare Improvement (IHI). What is a bundle? www.ihi.org/resources/Pages/ImprovementStories/WhatIsaBundle.aspx. Accessed 29 Mar 2017
Tanner J, Padley W, Assadian O, Leaper D, Kiernan M, Edmiston C (2015) Do surgical care bundles reduce the risk of surgical site infections in patients undergoing colorectal surgery? A systematic review and cohort meta-analysis of 8515 patients. Surgery 158(1):66–77
Jackson RS, Amdur RL, White JC, Macsata RA (2012) Hyperglycemia is associated with increased risk of morbidity and mortality after colectomy for cancer. J Am Coll Surg 214(1):68–80
Ata A, Lee J, Bestle SL et al (2010) Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg 145(9):858–864
Serra-Aracil X, Garcia-Domingo MI, Pares D et al (2011) Surgical site infection in elective operations for colorectal cancer after the application of preventive measures. Arch Surg 146(5):606–612
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional review board approval was obtained prior to initiating the study.
Informed consent
Informed consents are not applicable to this study as it was a retrospective study.
Rights and permissions
About this article
Cite this article
Gachabayov, M., Senagore, A.J., Abbas, S.K. et al. Perioperative hyperglycemia: an unmet need within a surgical site infection bundle. Tech Coloproctol 22, 201–207 (2018). https://doi.org/10.1007/s10151-018-1769-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-018-1769-2