Abstract
Background
Identifying lateral pelvic lymph node (LPN) metastasis in low rectal cancer is crucial before treatment. Several risk factors and prediction models for LPN metastasis have been reported. However, there is no useful tool to accurately predict LPN metastasis. Therefore, we aimed to construct a nomogram for predicting LPN metastasis in rectal cancer.
Methods
We analyzed the risk factors for potential LPN metastasis by logistic regression analysis in 705 patients who underwent primary resection of low rectal cancer. We included patients at 49 institutes of the Japan Society of Laparoscopic Colorectal Surgery between June 2010 and February 2012. Clinicopathological factors and magnetic resonance imaging findings were evaluated. The nomogram performance was assessed using the c-index and calibration plots, and the nomogram was validated using an external cohort.
Results
In the univariable logistic regression analysis, age, sex, carcinoembryonic antigen, tumor location, clinical T stage, tumor size, circumferential resection margin (CRM), extramural vascular invasion (EMVI), and the short and long axes of LPN and perirectal lymph node (PRLN) were nominated as risk factors for potential LPN metastasis. We identified a combination of the short axis of LPN, tumor location, EMVI, and short axis of PRLN as optimal for predicting potential LPN metastasis and developed a nomogram using these factors. This model had a c-index of 0.74 and was moderately calibrated and well-validated.
Conclusions
This is the first study to construct a well-validated nomogram for predicting potential LPN metastasis in rectal cancer, and its performance was high.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
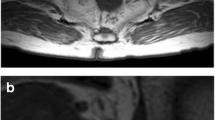
Accurate prediction of lateral pelvic lymph node (LPN) metastasis has been regarded as a critical issue for a long time with regard to rectal cancer treatment. The treatment strategy for rectal cancer significantly depends on the presence of LPN metastasis [1, 2]. Although total mesorectal excision (TME) plays a central role in the treatment strategy for locally advanced low rectal cancer, TME alone might be insufficient to prevent local recurrence [3,4,5,6]. In Japan and some other countries, lateral pelvic lymph node dissection (LPND) is often performed in addition to TME for locally advanced low rectal cancer to reduce local recurrence, according to the Japanese Society for Cancer of the Colon and Rectum guidelines [7, 8]. In contrast, neoadjuvant therapies, including radiotherapy and chemotherapy, are considered essential for the treatment of advanced low rectal cancer in Western countries [9,10,11]. However, in both Western and Asian countries, it is beneficial to predict LPN metastasis before initiating rectal cancer treatment. In addition, several risk factors for LPN metastasis, such as the short axis and shape of LPN metastasis, have been reported [11,12,13,14]. Although there are some predictive models for LPN metastasis [12,13,14,15,16], they have not been fully validated. There is currently no verified tool for predicting LPN metastasis in rectal cancer that can be easily used in daily practice. A nomogram is a graphical model, and its effectiveness in the treatment of colorectal cancer has been widely reported [17,18,19]. Therefore, this study aimed to construct a nomogram to predict LPN metastasis based on clinical and magnetic resonance imaging (MRI) findings.
Patients and methods
We conducted and described this report in accordance with the TRIPOD reporting guidelines [20].
Study setting and patients
The Japan Society of Laparoscopic Colorectal Surgery collected the clinical data of 1500 patients with clinical stage II–III low rectal cancer. These patients underwent open or laparoscopic surgery at 69 institutes participating in the Japan Society of Laparoscopic Colorectal Surgery between January 2010 and December 2011. The primary study reported short-term and mid-term outcomes [21]. The indications for neoadjuvant treatment were determined at each institution’s discretion. In addition to the data of the primary study, we collected long-term prognosis data and MRI findings. We used these data as training data after excluding the data from Kyoto University Hospital.
Eligibility
The inclusion criteria for this study were as follows: (1) clinical stage II–III low rectal cancer (tumor located below the peritoneal reflection), (2) preoperative MRI conducted (MRI after neoadjuvant therapies in patients undergoing neoadjuvant therapies), and (3) surgery with curative intent. In contrast, the exclusion criteria were as follows: (1) multiple primary cancers, (2) a history of treatment of other pelvic malignancies, and (3) patients who did not experience LPN metastasis but whose observation periods were insufficient (< 3 years). The peritoneal reflection was identified by barium or gastrografin enema and/or MRI.
We used the patients’ data from the Kyoto University Hospital from June 2005 to December 2016 as validation datasets. Eligibility criteria were the same as those in the training dataset.
Definition of potential lateral lymph node metastasis
We set potential LPN metastasis as an outcome, which was defined as a composite event of pathological LPN metastasis in patients with LPND and postoperative recurrence in lateral regions diagnosed by image inspections regardless of LPND. There are several cases of lateral recurrence due to omission of LPND, and treating only positive pathology as an outcome for patients with LPND might be an underestimation. Therefore, we adopted a composite outcome by including patients who did not undergo LPND.
Risk factors for potential lateral pelvic lymph node metastasis
We analyzed the following risk factors: age, sex, carcinoembryonic antigen (CEA), tumor location (distance from the anal verge), and preoperative MRI findings. The MRI findings included tumor depth (clinical T stage), tumor size, circumferential resection margin (CRM), extramural vascular invasion (EMVI), and the short and long axes of the LPN and perirectal lymph node (PRLN). Since this was a retrospective study, MRI imaging conditions varied by institution and time period. MRI for the training dataset was centrally assessed by six radiologists who established a consensus about MRI assessment before the start of the study. MRI for the validation dataset was assessed by surgeons of Kyoto University Hospital. CRM and EMVI were categorized into two groups according to the Mercury study [22] and the study by Smith et al. [23], respectively. Continuous variables were categorized for practicality. For example, short axis of LPN was categorized as < 3 mm, 3–5 mm, 5–7 mm, 7–9 mm, and ≥ 9 mm. CRM was defined as positive if the distance from the tumor to the rectal fascia or puborectalis was < 1 mm or the tumor extended beyond the internal anal sphincter [22]. EMVI was defined as positive if the MRI-EMVI score was 3 or 4 and negative if the MRI-EMVI score was 0–2 [23].
Statistical analysis
A logistic regression model was used to identify the risk factors for potential LPN metastasis. Risk factors with p < 0.20 in the univariable analysis were included in the multivariable analysis. We sought to identify the best combination of risk factors based on the clinical significance, and results of the stepwise backward elimination method referred to information criteria, such as the Akaike Information Criterion and Bayesian information criterion [24]. The Akaike Information Criterion penalizes the complexity of the model by decreasing the p value threshold at which variables are dropped from the model in proportion to the number of variables selected [24]. The Bayesian information criterion confers a larger penalty for models with several parameters. A nomogram was constructed using the results of the multivariable logistic regression model.
Assessment of nomogram performance
The nomogram performance was evaluated in terms of its discrimination and calibration [20]. Discrimination was the ability to distinguish between patients with events from those without events and was evaluated by area under the curve (AUC) after plotting the receiver operating characteristic curve (ROC). Calibration referred to how well the predicted probabilities from the model were in agreement with the observed outcome frequencies in the data, and it was assessed based on the calibration plot [24].
Statistical analysis was performed using R software, version 3.6.1 [25]. Nomogram construction and validation were performed using the “rms” package. The ROC curve was plotted using “pROC” packages, and the calibration plot was plotted using “ggplot2” packages.
Results
Patients’ characteristics
Of the 1500 patients enrolled in the primary study, preoperative MRI was available for 752 patients. Forty-seven of these patients were excluded (14 were at Kyoto University Hospital, 18 had insufficient observation periods, and 15 had missing data). Subsequently, 705 patients from 49 institutes were included in this study. The flow diagram of patient selection in the training dataset is shown in Fig. 1.
Clinical characteristics of the patients enrolled in the training dataset are shown in Table 1. Among 409 patients who underwent LPND, 84 patients were diagnosed with potential LPN metastasis, including 64 patients with LPN metastasis in the pathological assessment after surgery and 20 patients experiencing long-term lateral recurrence. In addition, of 296 patients without LPND, 15 laterally recurrent cases were diagnosed as potential LPN metastasis; thus, 99 patients had a diagnosis of potential LPN metastasis. A summary of the patients’ characteristics that were excluded from the analyses is shown in Table S1.
In the validation dataset, 108 patients with rectal cancer were identified. Of the 108 patients, 4 without preoperative MRI data and 4 other non-recurrent cases without sufficient treatment period were excluded. Subsequently, 100 patients were enrolled in the validation dataset. The flow diagram of patient selection in the validation dataset is shown in Fig. S1. The characteristics of patients enrolled in the validation dataset are shown in Table 1 and Table S1.
Nomogram development
In the univariable logistic regression analysis, age, sex, CEA, tumor location, clinical T stage, tumor size, CRM, EMVI, and short and long axes of LPN and PRLN were found to be risk factors for potential LPN metastasis. We identified that a combination of the short axis of LPN, tumor location, EMVI, and short axis of PRLN was the most effective in predicting potential LPN metastasis based on the results of multivariable logistic regression analysis with a backward stepwise method (Table 2). We constructed a nomogram using these factors (Fig. 2).
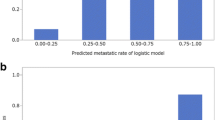
The ROC curve is shown in Fig. 3. The AUC of this nomogram was 0.74, positive predictive value was 25.4%, and negative predictive value was 93.4% (Table 3). Calibration plots are shown in Fig. 4, and the nomogram was moderately calibrated.
Nomogram validation
The ROC curve in the validation dataset is shown in Fig. S2. The AUC of the nomogram was 0.71, positive predictive value was 25.0%, and negative predictive value was 94.7% (Table 3). Calibration plots in the validation dataset are shown in Fig. S3, and the nomogram was moderately calibrated.
Discussion
In this study, the combination of the short axis of LPN, tumor location, EMVI, and the short axis of PRLN was identified to be most effective in predicting potential LPN metastasis in rectal cancer, and a nomogram was constructed using these factors. The nomogram had a high discrimination ability (AUC, 0.74) and was moderately calibrated. In addition, the nomogram was well validated in an external cohort (AUC, 0.71, moderate calibration). Evidently, neoadjuvant treatment might have had a significant impact on the diagnosis of potential LPN. We analyzed neoadjuvant treatment as a risk factor; however, it was not significant. Similarly, we created separate nomograms for those with and without neoadjuvant treatment using the same items; however, a minimal significant difference was observed (data not shown). Using this nomogram, we can determine the indications for LPND based on detailed risks rather than relying solely on size. Even if we determined not to perform LPND, screening examination intervals after surgery could be shortened based on the risk.
For an adequate treatment strategy, LPN metastasis should be diagnosed before initiating treatment. Several risk factors for LPN metastasis have been reported, such as LPN diameter, shape, and internal structures [12,13,14, 26, 27]. In particular, the short axis of LPN in MRI was reported to be the most crucial factor for predicting LPN metastasis, regardless of neoadjuvant therapies [13, 14, 26, 27]. However, the optimal cutoff value of the short axis of LPN for LPN metastasis was not sufficient to reach definitive conclusions. In addition, the diagnostic performance of MRI alone was reported to be limited [28]. Moreover, the predictive ability based on a single risk factor similarly had a limited utility. In this study, we used four risk factors, namely, the short axis of LPN, tumor location, EMVI, and short axis of PRLN, in the nomogram; in addition, the AUC of these risk factors was 0.67, 0.61, 0.57, and 0.55, respectively, all of which were lower than the AUC of the nomogram (0.74) that was constructed by the combination of these factors.
Matsuoka et al. [12] have used multiple LPN features, such as long axis, shape, and internal structure of LPN in MRI, to better predict LPN metastasis, with an AUC of 0.71. Nakanishi et al. [16] have reported that a radiomics-based prediction model was useful for predicting LPN metastasis (AUC, 0.83). Although the performance of the models was similarly high, they used data of a small number of patients from a single institution and mainly focused on imaging findings. In addition, subjective measures or special mechanics, such as LPN appearance and radiomics, were used [15, 16]. In contrast, we considered that clinicopathological factors were associated with LPN metastasis and LPN imaging. In addition, it was necessary to construct a predictive model using a large cohort for high generalizability. Thus, we considered it critical to create a predictive model using both clinicopathological factors and imaging findings by collecting data from nationwide multi-institutions.
To the best of our knowledge, this is the first study to develop a nomogram that predicts potential LPN metastasis in patients with low rectal cancer based on both clinicopathological factors and imaging findings. Moreover, this nomogram was internally and externally validated using different datasets. The accurate prediction of potential LPN metastasis is beneficial in developing an adequate treatment strategy and avoid unnecessary indications for invasive treatments, such as LPND and neoadjuvant chemoradiotherapy. Both treatments may reduce local recurrence; however, they could worsen short-term and long-term outcomes such as prolonged treatment time and decline in sexual and urinary functions [29,30,31].
The strength of this study lies in its use of data from institutions nationwide specialized in the treatment of rectal cancer in Japan. We included only cases with sufficient observation periods, and the only common variables across institutions where rectal cancer surgery was performed were used in this nomogram. The nomogram was validated using external data from the training dataset. Thus, we considered that this nomogram could be used widely and stably in daily clinical practice. However, this study had several limitations. Not all MRI scans were assessed by multiple radiologists. Furthermore, several patients were excluded because of missing data or insufficient observation periods. Additionally, the present study was a retrospective study, wherein characteristics of selection bias and incomplete data are inherent. Therefore, further research on prospective validation and controlled trial studies are required. These limitations could influence the prediction performance of the nomogram.
Conclusions
We constructed a nomogram to accurately predict potential LPN metastasis using the short axis of LPN, tumor location, EMVI, and the short axis of PRLN. The performance of this nomogram was high, and it was well validated.
References
Kim TH, Jeong SY, Choi DH et al (2008) Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol 15:729–737
Kim MJ, Oh JH (2018) Lateral lymph node dissection with the focus on indications, functional outcomes, and minimally invasive surgery. Ann Coloproctol 34:229–233
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Maurer CA, Renzulli P, Kull C et al (2011) The impact of the introduction of total mesorectal excision on local recurrence rate and survival in rectal cancer: long-term results. Ann Surg Oncol 18:1899–1906
Kusters M, Beets GL, van de Velde CJ et al (2009) A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg 249:229–235
Cecconello I, Araujo SE, Seid VE et al (2011) Laparoscopic total mesorectal excision: early and late results. Asian J Endosc Surg 4:99–106
Fujita S, Mizusawa J, Kanemitsu Y et al (2017) Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled. Noninferiority Trial Ann Surg 266:201–207
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Swedish Rectal Cancer Trial, Cedermark B, Dahlberg M et al (1997) Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med 336:980–987
Kapiteijn E, Marijnen CA, Nagtegaal ID et al (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646
Benson AB, Venook AP, Al-Hawary MM et al (2018) Rectal Cancer, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 16:874–901
Matsuoka H, Nakamura A, Masaki T et al (2007) Optimal diagnostic criteria for lateral pelvic lymph node metastasis in rectal carcinoma. Anticancer Res 27:3529–3533
Akiyoshi T, Matsueda K, Hiratsuka M et al (2015) Indications for lateral pelvic lymph node dissection based on magnetic resonance imaging before and after preoperative chemoradiotherapy in patients with advanced low-rectal cancer. Ann Surg Oncol 22(Suppl 3):S614–S620
Ogawa S, Hida J, Ike H et al (2016) Selection of lymph node-positive cases based on perirectal and lateral pelvic lymph nodes using magnetic resonance imaging: study of the Japanese society for cancer of the colon and rectum. Ann Surg Oncol 23:1187–1194
Chen LD, Liang JY, Wu H et al (2018) Multiparametric radiomics improve prediction of lymph node metastasis of rectal cancer compared with conventional radiomics. Life Sci 208:55–63
Nakanishi R, Akiyoshi T, Toda S et al (2020) Radiomics approach outperforms diameter criteria for predicting pathological lateral lymph node metastasis after neoadjuvant (chemo)radiotherapy in advanced low rectal cancer. Ann Surg Oncol 27(11):4273–4283
Kawai K, Sunami E, Yamaguchi H et al (2015) Nomograms for colorectal cancer: a systematic review. World J Gastroenterol 21(41):11877–11886
Takenaka Y, Miyoshi N, Fujino S et al (2020) Development of a novel prediction model for recurrent stage II colon cancer. Surg Today 50(4):389–395
Zhang J, Xiao L, Pu S et al (2021) Can we reliably identify the pathological outcomes of neoadjuvant chemotherapy in patients with breast cancer? Development and validation of a logistic regression nomogram based on preoperative factors. Ann Surg Oncol 28(5):2632–2645
Moons KG, Altman DG, Reitsma JB et al (2015) Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162:W1–W73
Hida K, Okamura R, Sakai Y et al (2018) Open versus laparoscopic surgery for advanced low rectal cancer: a large, multicenter, propensity score matched cohort study in Japan. Ann Surg 268:318–324
MERCURY Study Group (2006) Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ 333(7572):779
Smith NJ, Barbachano Y, Norman AR et al (2008) Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. Br J Surg 95:229–236
Sanchez-Pinto LN, Venable LR, Fahrenbach J et al (2018) Comparison of variable selection methods for clinical predictive modeling. Int J Med Inform 116:10–17
R:A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, 2018. Vienna, Austria
Matsuoka H, Masaki T, Sugiyama M et al (2007) Morphological characteristics of lateral pelvic lymph nodes in rectal carcinoma. Langenbecks Arch Surg 392:543–547
Ogura A, Konishi T, Beets GL et al (2019) Lateral nodal features on restaging magnetic resonance imaging associated with lateral local recurrence in low rectal cancer after neoadjuvant chemoradiotherapy or radiotherapy. JAMA Surg 154:e192172
Hoshino N, Murakami K, Hida K et al (2019) Diagnostic accuracy of magnetic resonance imaging and computed tomography for lateral lymph node metastasis in rectal cancer: a systematic review and meta-analysis. Int J Clin Oncol 24:46–52
Yang X, Yang S, Hu T et al (2020) What is the role of lateral lymph node dissection in rectal cancer patients with clinically suspected lateral lymph node metastasis after preoperative chemoradiotherapy? A meta-analysis and systematic review. Cancer Med 9:4477–4489
Ma P, Yuan Y, Yan P et al (2020) The efficacy and safety of lateral lymph node dissection for patients with rectal cancer: a systematic review and meta-analysis. Asian J Surg 43:891–901
Couwenberg AM, Burbach JPM, van Grevenstein WMU et al (2018) Effect of neoadjuvant therapy and rectal surgery on health-related quality of life in patients with rectal cancer during the first 2 years after diagnosis. Clin Colorectal Cancer 17:e499–e512
Acknowledgements
This study was supported by a grant from the Japanese Society of Clinical Oncology, the Japanese Foundation for Research and Promotion of Endoscopy, the Kondou Kinen Medical Foundation, and the Mitsubishi Foundation. The authors thank all institutes of The Japan Society of Laparoscopic Colorectal Surgery who have contributed to this study. The authors would also like to thank the following people for their cooperation in the assessment of MRI findings and elaborating the manuscript: S. Arizono, K. Tokunaga, S. Kohno, H. Nakai, A. Ono, T. Sato, S. Yoshida, Y. Aisu, R. Aoyama, N. Shimoike, and R. Okamura. We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
AS, KH, NH, TA, MF, TY, YS, and MW designed the study. AS, DN, IT, TT, and JW gathered data. AS, KH, NH, and DN analyzed the data and interpreted the results. All authors were involved in the draft preparation and in the review and approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
This study was supported by a grant from the Japanese Society of Clinical Oncology, the Japanese Foundation for Research and Promotion of Endoscopy, the Kondou Kinen Medical Foundation, and the Mitsubishi Foundation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10147_2022_2157_MOESM1_ESM.docx
Supplementary file1 Table S1 Patient characteristics in the training and validation datasets. Table S2 Positive and negative predictive values of the prediction model (DOCX 17 KB)
10147_2022_2157_MOESM3_ESM.tif
Supplementary file3 Fig. S2 Receiver operating characteristic curve of the nomogram in the validation dataset (TIF 85 KB)
About this article
Cite this article
Sumii, A., Hida, K., Sakai, Y. et al. Establishment and validation of a nomogram for predicting potential lateral pelvic lymph node metastasis in low rectal cancer. Int J Clin Oncol 27, 1173–1179 (2022). https://doi.org/10.1007/s10147-022-02157-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02157-1