Abstract
Background
Individuals with advanced gastric cancer (AGC) who present with severe peritoneal metastasis (SPM) have poor prognosis. This study aimed to evaluate efficacy and safety of second-line treatment for patients with such condition.
Methods
This retrospective study included patients receiving taxane-based second-line chemotherapy at three Japanese institutions between 2010 and 2016. Patients with AGC who present with SPM were included if they had massive ascites and/or inadequate oral intake requiring intravenous nutritional support.
Results
In this study, 43 (40%) of 108 patients had an Eastern Cooperative Oncology Group Performance Status score ≥ 2, and the median serum albumin level of the patients was 3.3 g/dL. Ramucirumab was used in combination with paclitaxel in 21 patients. The median overall survival (OS) and progression-free survival (PFS) were 5.1 and 2.8 months, respectively. Inadequate oral intake was considered a negative prognostic factor of both OS and PFS in the multivariate analysis. Three treatment-related deaths were observed, which include those attributed to febrile neutropenia, gastrointestinal perforation, and pneumonitis. Common grade ≥ 3 adverse events were neutropenia (35%), leukopenia (30%), anemia (24%), and anorexia (16%). We observed febrile neutropenia in 8% and gastrointestinal perforation in 4% of patients, and such conditions were dominantly observed in patients with inadequate oral intake.
Conclusion
Taxane-based second-line chemotherapy was effective and safe for patients with AGC who present with SPM. Attention must be provided when treating patients with inadequate oral intake as they are likely to have short prognosis and serious toxicities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is the fifth most common cancer and the third leading cause of cancer-related deaths worldwide [1]. The standard chemotherapy for advanced GC (AGC) is the combination of fluoropyrimidine and platinum, with trastuzumab if the patient with HER-2 positive GC, in the first-line setting [2,3,4] and paclitaxel plus ramucirumab in the second-line setting [5]. Although these chemotherapy treatments have survival benefits, AGC is not curable, and best supportive care (BSC) is recommended in patients with generally poor condition who cannot tolerate chemotherapy.
Peritoneal metastasis (PM) is common in individuals with AGC, and it causes serious clinical complications, such as massive ascites, bowel obstruction, jaundice, and hydronephrosis [6, 7]. These complications can rapidly worsen a patient’s general condition, making them ineligible for chemotherapy. PM is associated with poor prognosis, and the survival time of patients with severe PM (SPM) who present with massive ascites and/or bowel obstruction is extremely short even with chemotherapy [8,9,10,11]. Unfortunately, most pivotal phase III trials have not included patients with AGC who present with SPM; hence, the standard first- and second-line chemotherapy for such patients has not been established to date [2,3,4,5, 12]. Some retrospective studies have shown the efficacy and safety of fluoropyrimidine-based regimen as first-line chemotherapy for patients with AGC who present with SPM [9, 10, 13]. Recently, the first randomized phase II/III trial (JCOG1108/WJOG7312G trial: UMIN000010949) for this particular subset of AGC has been reported. In this trial, first-line 5-FU/l-leucovorin (l-LV) plus paclitaxel did not confer a significant survival benefit but might be preferred because of longer PFS and acceptable toxicity compared to 5-FU/l-LV [14].
Second-line chemotherapy for AGC is provided more frequently in Japan than in other countries, as shown by a high proportion of patients (approximately 75%–80%) receiving second-line chemotherapy in several Japanese phase III trials [2, 4, 12]. Second-line chemotherapy is effective in prolonging the survival time of patients [15]. As shown in the RAINBOW trial, the combination therapy of paclitaxel and ramucirumab, which targets vascular endothelial growth factor receptor-2, has been established as a new standard second-line treatment for AGC [5]. In patients with mild to moderate PM, the administration of paclitaxel weekly is considered a promising treatment that results in longer PFS compared with the best available 5-FU regimen in the JCOG0407 trial [16]. However, to date, there are only few data about the use of second-line chemotherapy in patients with SPM. Therefore, this study aimed to investigate the efficacy and safety of taxane-based second-line chemotherapy for patients with AGC who present with SPM.
Patients and methods
Patients
We retrospectively reviewed the records of patients with AGC who presented with SPM and received taxane-based second-line chemotherapy between July 2010 and June 2016 at three institutions in Japan. All patient data were extracted from a database at each center. In this study, SPM was defined as PM associated with massive ascites and/or inadequate oral intake. This definition was based on previous retrospective studies [9, 10, 13] and the JCOG1108/WJOG7312G trial [14]. Inadequate oral intake was defined as the need for intravenous nutritional support. The degree of ascites was evaluated via computed tomography and was classified as follows: none, undetectable; mild, localized to the pelvic cavity or upper abdominal cavity; moderate, inconsistent with either mild or massive ascites; and massive, extending continuously between the pelvic cavity and upper abdominal cavity. The eligibility criteria for this study were as follows: (1) histologically proven adenocarcinoma of the stomach or gastroesophageal junction, (2) with SPM during the initiation of second-line chemotherapy, (3) absence of concomitant advanced malignant disease, (4) refractory or intolerance to fluoropyrimidine (and trastuzumab if a patient has HER-2 positive disease), and (5) receiving taxane-based second-line chemotherapy after disease progression during first-line chemotherapy or recurrence within 6 months after the last adjuvant chemotherapy dose. We excluded patients with a history of taxane treatment and/or those with serious complications, such as active infection, renal failure (serum creatinine level ≥ 3.0 mg/dL), and hepatic failure or obstructive jaundice (serum total bilirubin level ≥ 2.0 mg/dL).
Assessments
We compared the degree of ascites between baseline and during treatment and determined the best responses in ascites, which were as follows: complete response (CR), the ascites completely disappeared; partial response (PR), there was a decrease by at least 1° from baseline; stable disease (SD), there was no change from baseline; progressive disease, there was an increase by at least one degree from baseline; and not evaluated, it was impossible to evaluate because fluid was drained before assessment or because there are no available records of the assessment results. We defined the response rate and disease control rate in ascites as the proportion of patients with the best CR or PR and the best CR, PR, or SD, respectively, among patients with ascites at baseline. The improvement rate of oral intake was defined as the proportion of patients whose oral intake improved and who did not require nutritional support for at least 7 days among the patients who had inadequate oral intake at baseline.
Statistical analysis
OS was defined as the time from treatment initiation to death from any cause, and PFS was defined as the time from treatment initiation to disease progression or death from any cause. Time to treatment failure (TTF) was defined as the time from the initiation of treatment to the last dose of second-line chemotherapy. Both OS and PFS were estimated using the Kaplan–Meier method. Prognostic factors were evaluated in the univariate and multivariate analyses using Cox proportional hazards models. Covariates with a p-value < 0.20 in the univariate analysis were included in the multivariate analysis. Fisher’s exact test was used for the test of independence between two categorical groups. All analyses were two-sided, and a p-value < 0.05 was considered statistically significant. All statistical analyses were performed using StatView software version 5.0 (SAS Institute, Cary, NC, the USA).
Human rights statement and informed consent
All procedures were in accordance with the ethical standards of the responsible committees on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later revisions. Informed consent for chemotherapy was obtained from all patients before treatment. This study was approved by the institutional review board of each center.
Results
Patients
In total, 115 patients with AGC who presented with SPM received taxane-based second-line chemotherapy. Seven patients (four with serum total bilirubin level ≥ 2.0 mg/dL, two with a history of receiving taxane, and one with serious infection) were excluded; thus, 108 patients were finally included. The characteristics of the patients are shown in Table 1. Forty-three (40%) patients had an Eastern Cooperative Oncology Group Performance Status (PS) score ≥ 2 (including one patient with a PS score of 3), and the median serum albumin level of the patients was 3.3 (range 1.8–4.3) g/dL. Thirty (34%) patients already had SPM before the initiation of first-line treatment. The detailed information about the number of patients receiving chemotherapy is as follows: paclitaxel (n = 80), paclitaxel plus ramucirumab (n = 21), nanoparticle albumin-bound paclitaxel (n = 3), 5-FU/l-leucovorin plus paclitaxel (n = 3), and docetaxel (n = 1). The following characteristics are more commonly observed in patients receiving paclitaxel plus ramucirumab (n = 21) than in those receiving treatment without ramucirumab (n = 87): intestinal histological type (33% vs 10%), PS score of 0 or 1 (76% vs 56%), metastatic sites ≥ 2 (81% vs 44%), and adequate oral intake (71% vs 44%). The details are shown in Online Resource 1.
Reasons for discontinuation of treatment
The median TTF was 2.2 months. The reasons for treatment discontinuation were as follows: disease progression [n = 90 (83%)], adverse events [n = 11 (10%)], patient refusal [n = 3 (3%)], and other reasons [n = 4 (4%)]. The adverse events leading to treatment discontinuation were peripheral neuropathy (n = 4, including three grade 3 and one grade 2 cases), gastrointestinal perforation (n = 2, including one grade 5 and one grade 3 cases), pneumonitis (n = 2, including one grade 5 and one grade 3 cases), febrile neutropenia (n = 1, grade 5 case), fatigue (n = 1, grade 2 case), and allergic reaction (n = 1, grade 3 case).
Efficacy
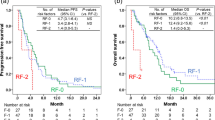
In total, 105 (97%) patients had died. The median OS and PFS were 5.1 and 2.8 months, respectively (Fig. 1a). In the analysis according to the subtype of SPM, the median OS of patients with massive ascites only, inadequate oral intake only, and both were 6.0, 4.4, and 3.2 months, respectively. The median PFS were 3.5, 2.5, and 2.1 months, respectively (Fig. 1b–c). The univariate analysis of OS identified two prognostic factors: presence of massive ascites and inadequate oral intake. The multivariate analysis showed that inadequate oral intake was the only independent prognostic factor [hazard ration (HR) = 2.41; 95% confidence interval (CI) 1.47–3.97; p < 0.01]. Similarly, in the analysis of PFS, inadequate oral intake was the only independent prognostic factor in the multivariate analysis (HR = 1.88; 95% CI 1.15–3.08; p = 0.01) (Table 2).
Kaplan–Meier analysis of overall survival (OS) and progression-free survival (PFS). a Overall survival and progression-free survival of all patients (N = 108). b Overall survival of patients with massive ascites only (N = 53), inadequate oral intake only (N = 29), and both (N = 26). c Progression-free survival of patients with massive ascites only (N = 53), inadequate oral intake only (N = 29), and both (N = 26)
The response rate and disease control rate in ascites were 27% (28/102) and 78% (80/102), respectively. The improvement rate of oral intake was 31% (17/55) (Table 3).
Safety
Data about toxicity are shown in Table 4. Three (3%) treatment-related deaths were recorded, which include those attributed to febrile neutropenia in a patient receiving paclitaxel plus ramucirumab, gastrointestinal perforation in a patient receiving paclitaxel plus ramucirumab, and pneumonitis in a patient receiving paclitaxel. In all patients, common grade ≥ 3 adverse events were neutropenia [n = 38 (35%)], leukopenia [n = 32 (30%)], anemia [n = 26 (24%)], and anorexia [n = 16 (15%)]. Febrile neutropenia occurred in nine (8%) patients, which included six patients with a PS score of 2 and seven patients whose oral intake were inadequate, and gastrointestinal perforation occurred in four (4%) patients, which included two patients with a PS score of 2 and three patients whose oral intake were inadequate. The details of each case are shown in Online Resource 2. Both febrile neutropenia and gastrointestinal perforation were more commonly observed in patients with inadequate oral intake than in those with adequate oral intake [13% (7/55) vs 4% (2/53) and 5% (3/55) vs 2% (1/53), respectively]. Meanwhile, higher incidence of febrile neutropenia and gastrointestinal perforation was not observed in patients with massive ascites, compared to those without massive ascites [5% (4/79) vs 17% (5/29) and 4% (3/79) vs 3% (1/29), respectively]. Also, both febrile neutropenia and gastrointestinal perforation were more commonly observed in patients receiving paclitaxel plus ramucirumab than in those receiving taxane only [14% (3/21) vs 7% (6/87) and 10% (2/21) vs 2% (2/87), respectively]. In patients with massive ascites, the incidence of febrile neutropenia and gastrointestinal perforation were almost similar between patients receiving paclitaxel plus ramucirumab and those receiving taxane only [6% (1/16) vs 5% (3/63), p > 0.99 and 6% (1/16) vs 3% (2/63), p = 0.50, respectively]. Meanwhile, in patients with inadequate oral intake, the incidence of febrile neutropenia tended to be higher, and that of gastrointestinal perforation was significantly higher in patients receiving paclitaxel plus ramucirumab than in those receiving taxane only [33% (2/6) vs 10% (5/49), p = 0.16 and 33% (2/6) vs 2% (1/49), p = 0.03, respectively] (Table 5). Gastrointestinal bleeding occurred only in two (2%) patients, and both patients received taxane only.
Post-discontinuation therapy (PDT)
In total, 28 (26%) patients received PDT. The regimens of PDT were as follows: irinotecan plus cisplatin (n = 6), irinotecan (n = 6), FOLFOX (n = 6), 5-FU/l-LV (n = 3), ramucirumab (n = 2), S-1 plus oxaliplatin (n = 1), S-1 plus cisplatin (n = 1), and others (n = 3).
Discussion
This study first investigated second-line treatment specifically for patients with AGC who presented with SPM. Herein, we reveal the efficacy and safety of taxane-based chemotherapy using real-world clinical data.
In contrast with previous clinical trials in the second-line setting, patients with SPM had a poorer general condition. The high proportion of patients with a poor PS score (≥ 2, 40%) and low serum albumin level (with a median of 3.3 g/dL) were significant characteristics, which were presented in the current study. These characteristics are similar to those of patients with AGC who presented with SPM and who received first-line chemotherapy, as reported in another retrospective study. That is, 40% had a PS score > 2, and the median serum albumin level was 3.1 g/dL in the first-line setting [13]. This may lead to poor prognosis: median OS of 5.1 months and median PFS of 2.8 months in the present study. Although this result was worse than survival times in second-line chemotherapy for generally advanced GC, with a median OS of 7.7–9.6 months and median PFS of 3.6–4.4 months [5, 16,17,18], taxane-based second-line chemotherapy may have more survival benefits than BSC in patients with SPM, considering the reported median survival time of 2.4–3.8 months in patients with AGC receiving BSC [19,20,21,22]. Importantly, we showed the difference in prognosis between the subtypes of SPM. That is, longer OS and PFS were observed in the subtype with massive ascites alone compared with the other two subtypes. Similarly, the multivariate analysis showed that inadequate oral intake was the only adverse prognostic factor of both OS and PFS. These findings indicated that patients with inadequate oral intake may have more aggressive state of disease than others; therefore, we should be cautious in terms of treatment.
The incidence of common adverse events was almost comparable to that of the effects of paclitaxel-based treatment, as reported in the RAINBOW and WJOG4007 trials in the second-line setting [5, 17]. However, febrile neutropenia and gastrointestinal perforation were more commonly observed in the present study compared to RAINBOW trial: the frequency of febrile neutropenia was 8%, 3%, and 2% in the present trial, the paclitaxel plus ramucirumab arm in RAINBOW trial, and the paclitaxel plus placebo arm in RAINBOW trial, respectively; that of gastrointestinal perforation was 4%, 3%, and 2% in the present trial, the paclitaxel plus ramucirumab arm in RAINBOW trial, and the paclitaxel plus placebo arm in RAINBOW trial, respectively. Of note, these serious toxicities were dominantly observed in patients with inadequate oral intake in the present study. In addition, a higher incidence of febrile neutropenia was observed in patients receiving paclitaxel plus ramucirumab (14%) than in patients receiving taxane only (7%). Similarly, gastrointestinal perforation was more commonly observed in patients receiving paclitaxel plus ramucirumab (10%) than in those receiving taxane only (2%). Interestingly, the higher incidence of febrile neutropenia and gastrointestinal perforation after paclitaxel plus ramucirumab compared to after taxane only was observed in the subgroup with inadequate oral intake, but not in the subgroup with massive ascites. This may be caused by patient’s poor systemic conditions, particularly in the subgroup with inadequate oral intake. Of note, approximately 33% of patients who have inadequate oral intake and who were receiving paclitaxel plus ramucirumab presented with gastrointestinal perforation. This finding indicated that gastrointestinal perforation during anti-angiogenesis treatment is significantly correlated to severe peritoneal metastasis involving in the intestinal tract stenosis. A previous report has shown that tumor infiltration in the intestinal tract and stenosis due to PM might be the risk factors of gastrointestinal perforation [23]. These findings can serve as a warning to observe caution when providing treatment with paclitaxel plus ramucirumab particularly in patients with inadequate oral intake due to SPM.
This study had some limitations. First, this was a retrospective study. Second, the limited sample size made it challenging to obtain a clear conclusion. Thus, further studies must be conducted to validate the actual efficacy and safety of second-line chemotherapy in patients with AGC who presented with SPM in prospective clinical trials.
In conclusion, taxane-based second-line chemotherapy was effective and safe in patients with AGC who presented with SPM. Attention must be provided when treating patients with inadequate oral intake as they are likely to have poor prognosis and serious toxicities.
Abbreviations
- AGC:
-
Advanced gastric cancer
- GC:
-
Gastric cancer
- SPM:
-
Severe peritoneal metastasis
- BSC:
-
Best supportive care
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PM:
-
Peritoneal metastasis
- SPM:
-
Severe PM
- JCOG:
-
Japan clinical oncology group
- CR:
-
Complete response
- PR:
-
Partial response
- SD:
-
Stable disease
- TTF:
-
Time to treatment failure
- PDT:
-
Post-discontinuation therapy
References
International Agency for Research on Cancer. GLOBOCAN 2012: cancer incidence and mortality worldwide. https://gco.iarc.fr/. Accessed 22 Sept 2019
Koizumi W, Narahara H, Hara T et al (2008) S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol 9:215–221
Bang YJ, Van Cutsem E, Feyereislova A et al (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376:687–697
Yamada Y, Higuchi K, Nishikawa K et al (2015) Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naive patients with advanced gastric cancer. Ann Oncol 6:141–148
Wilke H, Muro K, Van Cutsem E et al (2014) Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol 15:1224–1235
Fujimura T, Ishii K, Oyama K et al (2003) A new scoring system for peritoneal metastasis in gastric cancer. Gastric Cancer 6:146–152
Wei J, Wu ND, Liu BR (2016) Regional but fatal: Intraperitoneal metastasis in gastric cancer. World J Gastroenterol 22:7478–7485
Iwasa S, Goto M, Yasui H et al (2012) Multicenter feasibility study of combination therapy with fluorouracil, leucovorin and paclitaxel (FLTAX) for peritoneal disseminated gastric cancer with massive ascites or inadequate oral intake. Jpn J Clin Oncol 42:787–793
Iwasa S, Nakajima TE, Nakamura K et al (2012) First-line fluorouracil-based chemotherapy for patients with severe peritoneal disseminated gastric cancer. Gastric Cancer 15:21–26
Hara H, Kadowaki S, Asayama M et al (2018) First-line bolus 5-fluorouracil plus leucovorin for peritoneally disseminated gastric cancer with massive ascites or inadequate oral intake. Int J Clin Oncol 23:275–280
Shitara K, Mizota A, Matsuo K et al (2013) Fluoropyrimidine plus cisplatin for patients with advanced or recurrent gastric cancer with peritoneal metastasis. Gastric Cancer 16:48–55
Boku N, Yamamoto S, Fukuda H et al (2009) Fluorouracil versus combination of irinotecan plus cisplatin versus S-1 in metastatic gastric cancer: a randomised phase 3 study. Lancet Oncol 10:1063–1069
Arai H, Iwasa S, Boku N et al (2019) Fluoropyrimidine with or without platinum as first-line chemotherapy in patients with advanced gastric cancer and severe peritoneal metastasis: a multicenter retrospective study. BMC Cancer 19:652
Nakajima TE, Yamaguchi K, Boku N et al (2020) Randomized phase II/III study of 5-fluorouracil/l-leucovorin versus 5-fluorouracil/l-leucovorin plus paclitaxel administered to patients with severe peritoneal metastases of gastric cancer (JCOG1108/WJOG7312G). Gastric Cancer. https://doi.org/10.1007/s10120-020-01043-x
Iizumi S, Takashima A, Sakamaki K et al (2018) Survival impact of post-progression chemotherapy in advanced gastric cancer: systematic review and meta-analysis. Cancer Chemother Pharmacol 81:981–989
Nishina T, Boku N, Gotoh M et al (2016) Randomized phase II study of second-line chemotherapy with the best available 5-fluorouracil regimen versus weekly administration of paclitaxel in far advanced gastric cancer with severe peritoneal metastases refractory to 5-fluorouracil-containing regimens (JCOG0407). Gastric Cancer 19:902–910
Hironaka S, Ueda S, Yasui H et al (2013) Randomized, open-label, phase III study comparing irinotecan with paclitaxel in patients with advanced gastric cancer without severe peritoneal metastasis after failure of prior combination chemotherapy using fluoropyrimidine plus platinum: WJOG 4007 trial. J Clin Oncol 31:4438–4444
Shitara K, Takashima A, Fujitani K et al (2017) Nab-paclitaxel versus solvent-based paclitaxel in patients with previously treated advanced gastric cancer (ABSOLUTE): an open-label, randomised, non-inferiority, phase 3 trial. Lancet Gastroenterol Hepatol 2:277–287
Ford HE, Marshall A, Bridgewater JA et al (2014) Docetaxel versus active symptom control for refractory oesophagogastric adenocarcinoma (COUGAR-02): an open-label, phase 3 randomised controlled trial. Lancet Oncol 15:78–86
Fuchs CS, Tomasek J, Yong CJ et al (2014) Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet 383:31–39
Kang JH, Lee SI, Lim DH et al (2012) Salvage chemotherapy for pretreated gastric cancer: a randomized phase III trial comparing chemotherapy plus best supportive care with best supportive care alone. J Clin Oncol 30:1513–1518
Thuss-Patience PC, Kretzschmar A, Bichev D et al (2011) Survival advantage for irinotecan versus best supportive care as second-line chemotherapy in gastric cancer–a randomised phase III study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Eur J Cancer 47:2306–2314
Matsumoto H, Kawazoe A, Shimada K et al (2018) A retrospective study of the safety and efficacy of paclitaxel plus ramucirumab in patients with advanced or recurrent gastric cancer with ascites. BMC Cancer 18:120
Acknowledgments
The authors would like to thank Enago (www.enago.com) for the English language review.
Funding
We had no financial supports for this study.
Author information
Authors and Affiliations
Contributions
HA and TEN planned, designed, analyzed and drafted the manuscript. MK and TM made substantial contributions to data collection. HY and KM supported planning and drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
TM reports honoraria from Taiho, Lilly Japan, Yakult Honsha, and Sanofi. KM reports honoraria from Bristol Myers-Squibb, Taiho, and Eli Lilly, and research funding from Bristol Myers Squibb and Taiho. TEN reports honoraria from Bristol Myers-Squibb, Sawai, Nippon Kayaku, Yakult, Taiho, and Eli Lilly, and research funding Nippon Kayaku, Yakult, Taiho, and Eli Lilly. None of the remaining authors have potential conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Arai, H., Kawahira, M., Yasui, H. et al. Second-line chemotherapy using taxane in patients with advanced gastric cancer who presented with severe peritoneal metastasis: a multicenter retrospective study. Int J Clin Oncol 26, 355–363 (2021). https://doi.org/10.1007/s10147-020-01802-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01802-x