Abstract
Introduction
This study was to evaluate the surgical and survival effects of neoadjuvant chemotherapy (NAC) followed by radical hysterectomy (RH) for cervical cancer with stages IB2 to IIB of FIGO 2009 staging.
Methods
From February 2, 2001 to November 11, 2015, 428 patients received NAC followed by RH in a tertiary hospital, in which all the major procedures were performed by one surgeon. Surgical and survival outcomes were evaluated between the NAC and primary RH groups.
Results
A total of 279 (65.2%) patients received NAC, and the overall clinical and complete pathological response rates were 65.9% and 10.8%, respectively. Compared with primary RH patients, NAC patients had more advanced stages, higher recurrence rate, longer median duration of RH, and more median estimated blood loss. After adjusted with baseline risk factors, no significant differences in progression-free or overall survival were observed between the NAC and primary RH groups. However, the responders to NAC had better survival outcomes.
Conclusions
There were no surgical or survival benefits of NAC for patients with cervical cancer of stages IB2 to IIB except for the responders to NAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uterine cervical cancer is one of the most common global malignancies among women. In less-developed countries, cervical cancer is the leading cause of cancer death [1]. An increasing trend in incidence and mortality of cervical cancer has also been observed in China [2]. Radical hysterectomy (RH) is recommended as the primary treatment option for young patients with early stage cervical cancer (stages IA2 and IB1). While effective treatments for locally advanced cervical cancer (LACC) of stages IB2 to IIB, which have an inferior prognosis, still remain controversial. To reduce the primary tumor size [3], improve operative curability and safety, and reduce long-term complications due to radiotherapy [4], neoadjuvant chemotherapy (NAC) had been attempted for patients with LACC. Despite numerous reports guaranteeing the safety profile and effectiveness of NAC for cervical cancer, the results of randomized controlled trials [5, 6] and meta-analysis [7] suggested that NAC did not improve the survival outcomes of patients with LACC. Therefore, the applicability of NAC in LACC is debatable [8, 9], and is not recommended as general practice [10]. However, the randomized studies of NAC did not rigorously follow the uniform treatment protocols [5, 6]. Currently, no high-certainty evidence was available on the relative benefits and harms of primary radical hysterectomy versus primary chemoradiotherapy for stage IB2 cervical cancer [11]. In a phase 3 randomized controlled study, although NAC followed by chemoradiotherapy could improve disease-free survival compared with NAC followed by RH, the former had more toxicity and did not significantly improve overall survival [12]. Based on these findings, to date, there are no sufficient data to support the surgical or survival benefits of NAC followed by RH. The role of NAC in the treatment of LACC still requires more substantial evidences.
In this cohort study among Chinese patients with FIGO stage IB2 to IIB cervical cancer, we analyzed the differences in clinicopathological characteristics and surgical, survival outcomes between patients who received NAC followed by RH and those who received primary surgeries, so as to determine the impact of NAC in the treatment of LACC. All the major procedures, including resection of the parametrium and systematic lymphadenectomy, were all performed by the one surgeon.
Methods
Ethical approval and study design
This retrospective cohort study was conducted at a tertiary teaching hospital. The Institutional Review Board of the study center had approved this study. Informed consent was obtained from all individual participants before any treatment. All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
We identified all patients diagnosed with cervical cancer of stages IB2 to IIB from February 2, 2001 to November 11, 2015 through electronic medical records system. All patients were followed in outpatient clinics up to December 31, 2016. According to definitive treatment, patients were classified into NAC and primary RH groups. The primary endpoints included progression-free and overall survival (PFS and OS) between two groups, which were calculated from the date of last treatment (RH and/or adjuvant treatment) to the date of progression, death, or the last follow-up, whichever occurred first. The survival of patients with different stages and responses to NAC was also analyzed. The secondary endpoints included surgical outcomes such as estimated blood loss, transfusion volume, duration of surgery, and hospital stay.
Patients
All patients with cervical cancer of stage IB2 to IIB received RH of class III or type C of the Q–M classification [13, 14]. Detailed data were collected by searching and reviewing medical records. The inclusion criteria consisted of the following: histopathologically proven primary cervical squamous carcinoma, adenocarcinoma, or adenosquamous carcinoma; FIGO stage IB2 to IIB diagnosed by pelvic examinations of two experienced physicians of gynecologic oncology; surgical procedures belonging to RH of class III or type C with systemic lymphadenectomy; aged 18 years or older; and performance status of Eastern Cooperative Oncology Group scores 0 or 1. Patients were excluded if they had distant metastasis in presurgical imaging. Recurrence was validated by physical, imaging examination, and/or biopsy. Mortality was confirmed by reviewing medical records and interviews by telephone and/or email. As there were no patients accepted laparoscopic RH since the year of 2011, we divided the cases into two periods, i.e., before and after 2011.
Surgical and pathological evaluation
Surgical treatment consisted of laparoscopic or abdominal RH, bilateral salpingo-oophorectomy, and lymphadenectomy of the pelvic lymph nodes (PLNs) and para-aortic lymph nodes (PALNs). To preserve the ovaries of young patients, salpingectomy was undertaken along with translocation of the ovaries to the peritoneum above the level of the anterior superior spine. All the major procedures of RH (resection of parametrium and systematic lymphadenectomy) were performed by the corresponding author. The procedures of nerve-sparing RH had been described in the other study [15]. All the laparoscopies utilized the uterine manipulator. Specifically, in laparoscopic RH, the specimen of lymph nodes was placed in a sealed bags after resection, and these bags were taken out via vagina together with the uterine, fallopian tubes and ovaries. Then, a transvaginal suture was accomplished for vaginal cuff.
All specimens underwent detailed pathological examinations, including characteristics of pathological subtypes, lymph-vascular space invasion, invasion depth of the stroma, lymphatic metastasis, involvement of uterus or parametrium, and status of the incision margin. For RH performed before 2009, the staging was reviewed and redefined according to FIGO 2009 criteria [16].
NAC protocols and post-operative adjuvant therapies
The NAC protocols consisted of TC (paclitaxel 175 mg/m2, carboplatin AUC 5 on day 1 in a cycle of 21 days administered via intravenous infusion), TP (paclitaxel 175 mg/m2, cisplatin 70 mg/m2 on day 1 in a cycle of 21 days via intravenous infusion) or PF (fluorouracil 1000 mg/m2 on days 1–4, cisplatin 70 mg/m2 on day 1 in a cycle of 28 days via intravenous or transuterine arterial infusion).
Post-operative adjuvant therapies included systematic chemotherapy, radiotherapy, concurrent chemoradiotherapy, or a combination, which were provided for patients with risk factors of recurrence according to the guideline [10]. The regimens for systematic chemotherapy were similar to that for NAC. Concurrent chemoradiotherapy consisted of radiotherapy and concurrent chemotherapy of cisplatin or paclitaxel if the patient had a hypersensitivity reaction to cisplatin. Radiotherapy consisted of conventional external-beam fractionation and low-dose-rate (40–70 cGy/h) brachytherapy. For PALN metastasis, an additional and extensive radiation therapy field was applied to achieve curative treatment.
Response and toxicity evaluation of NAC
The clinical response to the NAC was assessed according to the Response Evaluation Criteria in Solid Tumors’ guidelines [17]. Target lesions of the cervical tumor were measured by preoperative imaging of magnetic resonance imaging or computed tomography rather than ultrasound, as the ultrasound could not specifically assess the residual tumor in such situations [18]. Complications related to NAC and/or RH within 3 months were reviewed according to the protocol of Obermair et al. [19] and collected from medical records as adverse events according to the Common Terminology Criteria for Adverse Events v4.03 [20].
Statistical analysis
SPSS 22.0 (SPSS Inc., Chicago, IL, USA) was utilized for statistical analysis. The differences in epidemiological, clinical, and pathological characteristics between patients in the NAC group and patients in the primary RH group were determined by univariate analysis of Chi-square tests or Wilcoxon rank sum test. The Kaplan–Meier method and Cox proportional hazards regression models were used to determine the risk factor of survival outcomes. Pathological characteristics, post-operative complications, and post-operative adjuvant therapies were integrated as covariates. All reported significances were two tailed at a level of 0.05.
Results
Epidemiological, clinical, and pathological characteristics of patients
From February 2, 2001 to November 11, 2015, 428 eligible patients were included in the study, and 279 (65.2%) received NAC. The baseline characteristics of the patients are summarized in Table 1. Stage IB2, IIA1, IIA2, and IIB cervical cancer consisted of 272 (63.6%), 68 (15.9%), 46 (10.7%), and 42 (9.8%) patients, respectively. Squamous carcinoma, adenocarcinoma, and adenosquamous carcinoma consisted of 375 (87.6%), 39 (9.1%), and 14 (3.3%) cases, respectively. Half of the operations were performed after 2011 (221 cases, 51.6%) and by laparoscopy (54.0%). Nerve-sparing RH consisted of 115 (26.9%) cases of all surgeries.
As shown in Table 1, there were no significant differences in most of preoperative parameters between the NAC group and the RH group. However, patients in the NAC group had more advanced FIGO stages (P = 0.002), more surgeries performed before year 2011 (P < 0.001), and more post-RH radiotherapy (P = 0.003). These variates had been the adjusted factors in a Cox regression model.
Clinical and pathological response to NAC
NAC protocols consisted of TP (86 cases, 20.1%), TC (17, 4.0%) and PF (175, 40.9%), with a median number of cycles of 3 (range 2–3), 3 (range 3–3) and 2 (range 1–4), and a median duration from initiation of chemotherapy to RH of 61 (range 39–68), 64 (60–68) and 60 days (25–122), respectively. In 120 of 175 (68.6%) patients with PF protocols, chemotherapy was administered via the transuterine artery.
After NAC, complete and partial responses were observed in 25 (9.0%) and 159 (57.0%) patients, respectively. The overall response rate was 184/279 (65.9%). The TP, TC, and PF protocols had similar response rates of 71.3% (62/87), 58.8% (10/17) and 64.0% (112/175) (P = 0.412). Thirty patients (10.8%) had no residual lesion in the final pathological examinations.
Surgical and pathological outcomes
Table 1 summarizes data concerning surgical conditions and outcomes. Compared with patients in the primary RH group, patients in the NAC group had longer operative times and more estimated blood loss (P = 0.011 and 0.026, respectively). Grade 3 and 4 complications were observed in 28 (6.5%) patients. Early adverse events within 90 days after surgery occurred in 7 of 149 (4.7%) of the patients in the RH group and 21 of 279 (7.5%) of the patients in the NAC group (P = 0.309). No surgery-related mortality occurred. No significant differences were found among the pathological characteristics.
Survival outcomes
Survival data were available in 397 patients (92.8%) with a median follow-up of 41.3 months (range 6–193.5). For the whole population, 5-year and 10-year PFS were 70.0% and 60.0%, respectively; 5-year and 10-year OS were 75.0% and 65.0%, respectively. Specifically, surgical routs (laparoscopy versus open surgery) had no significant impact on the PFS or OS in Kaplan–Meier analysis (P = 0.471 and 0.098, respectively). In Cox regression models, as shown in Supplement Table 1, independent factors of recurrence and mortality included lymph node metastasis, involvement of the parametrium, post-operative complications, incision status, invasion depth of stroma, pathological subtypes, differentiation, and FIGO stages.
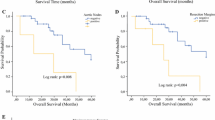
There were 91 recurrences (35.7%) and 69 deaths (27.1%) in the NAC group and 35 recurrences (24.6%) and 29 deaths (20.6%) in the RH group. The 5-year OS rates were 75.0% and 75.0% in the NAC and primary RH groups, respectively, and the 5-year PFS was 68.0% and 75.0%, respectively. The NAC group had a higher recurrence rate (P = 0.025) and fewer distant metastases (20.9% versus 45.7%, P = 0.008). As shown in Fig. 1 and Table 2, neither PFS nor OS were significantly different between the NAC and the primary RH groups with Kaplan–Meier method or after adjusting for the factors listed in Supplement Table 1. Stratified analysis according to stages of IB2 to IIB also revealed no significant differences in PFS or OS rates. Specifically, the proportion of various pathologic subtypes had no impact on these results. For patients with laparoscopies, the NAC had no significant impact on the PFS or the OS (P = 0.141 and 0.172, respectively) in Kaplan–Meier analysis. NAC had neither significant impact on the PFS or the OS (P = 0.416 and 0.271, respectively) for patients with open surgeries.
Survival outcomes of patients in the neoadjuvant chemotherapy (NAC) and primary radical hysterectomy (RH) groups using Cox regression models adjusted for clinical and pathological factors. a Progression-free survival (PFS). With the primary RH group as a reference, the odds ratio (OR) of recurrence in the NAC group was 0.8 (95% confidence interval [CI] 0.6–1.3, P = 0.522). b Overall survival (OS). With the primary RH group as a reference, the OR of mortality in the NAC group was 1.1 (95% CI 0.7–1.8, P = 0.626)
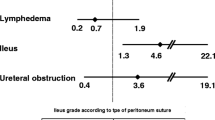
As shown in Table 3 and Fig. 2, patients with complete or partial responses following NAC had significantly better PFS and OS in the Kaplan–Meier analysis. However, after adjusting for the factors listed in Supplement Table 1, the superiority of prognosis disappeared.
Survival outcomes of patients with neoadjuvant chemotherapy (NAC) stratified according to response by the Kaplan–Meier method. The statistical data are listed in Table 3. a Progression-free survival (PFS). b Overall survival (OS)
Discussion
Our reports provided the evidences about the role of NAC in the treatment of LACC followed by radical surgeries, which were all performed by one surgeon. The surgical and survival outcomes could offer the basis of decision making for physicians and patients. As previously reported, NAC followed by radical hysterectomy was suggested as a useful strategy for patients even with non-squamous cell carcinoma of the uterine cervix [21, 22]. Trans-uterine arterial NAC may be promising for stage IB2 to IIB and IVA bulky cervical adenocarcinoma [23]. Anti-angiogenesis agents had also been attempted to be used as NAC, which could possibly improve objective response [24]. Despite these benefits provided by NAC, the survival outcomes of such intervention are still disputed. Both OS and PFS were improved with NAC for women with early stage cervical cancer or LACC in a small number of trials [25]. But for stage IB to III cervical cancer, follow-up in a long-term randomized study revealed no significant advantage in disease-free or overall survivals [26]. From the available studies, no insufficient evidences existed that hysterectomy with radiotherapy with or without chemotherapy could improves the survival of women with LACC compared with women who are treated with radiotherapy or chemoradiotherapy alone [27, 28]. In a current meta-analysis, although NAC reduced the need for adjuvant radiotherapy by decreasing tumor size and reducing lymph nodes metastasis and distant metastasis, NAC failed to improve survival when compared with primary surgical treatment in patients with FIGO stage IB1–IIA cervical cancer [7]. In our study, neither univariate nor multivariate analyses revealed any significant advantages of NAC in survival outcomes. In contrast, patients who received NAC had a higher recurrence rate, longer median duration of RH, and more median estimated blood loss, most likely due to the more advanced stages and earlier chronological years at the time of surgery (Table 1). As more NAC was utilized before 2011, the learning curves of RH could also explain its higher recurrence and poorer surgical outcomes.
The contradiction between NAC treatment and survival outcomes has not yet been completely explained. Response to NAC could be a reasonable breakthrough point, as our study revealed responders to the NAC may have better survival outcomes. In a small phase II trial, lymph nodes metastasis before NAC and nonresponse to NAC were significant prognostic factors for IB2-to-IIIB squamous cell carcinoma of the uterine cervix with a bulky mass [29]. A larger prospective trial is needed to investigate the relationship between survivorship and response to NAC. Currently, some expert opinions about the appropriate selection of patients were available for the application of NAC: dose-dense platinum doublet neoadjuvant chemotherapy of two cycles had been suggested to evaluate the response of NAC; patients with good response could accept the third cycle of chemotherapy and following RH [30]. A surgical predicting model had also been developed for stage IB2 to IIIB patients with curative NAC and RH [31].
In our study, NAC did not appear to have advantages in promoting surgical benefits or decreasing post-operative adjuvant therapy. But the interpretation needs caution, since NAC patients had more advanced staging and earlier surgical periods. The improved experiences and skills of the surgeon would probably contribute to the discrepancy just as reported [32]. On the other hand, NAC had other surgical superiorities, such as application in fertility-sparing surgery for cervical cancer [33, 34], and for pregnant women complicated with cervical cancer [35, 36]. In our study, NAC resulted in less distant metastasis, which accorded with previously published clinical studies [37, 38] and meta-analysis [7] in patients with LACC. The reasons were little known. The systemic effects from NAC could probably explain the reduced distant metastasis. However, just as we had reported, in meta-analysis patients with NAC and primary surgery had no differences about the overall and loco-regional recurrences and progression-free survival [7]. Hence, the control of distant metastasis of NAC should be interpreted discreetly.
The 10.8% of pathological complete response rate in our study was lower than the reported 16.1–45% in two prospective phase 2 studies [39, 40]. The most possible reason is due to the retrospective study design, which was lack of uniform NAC protocols and pathological examinations. Many patients accepted radical surgeries once they achieved partial response according to the physician’s instructions, which would significantly decrease the pathological response. However, the significance of generally low pathological complete response needs exploration in studies relevant to the application of adjuvant therapy and survival outcomes.
The main strengths of our study are the relative large cohort and uniform procedures of RH performed by an experienced physician. However, as this study was a retrospective study, recall bias and selection bias are inevitable. The present study was conducted across a 15-year interval; thus, there are probably a variety of confounding biases, such as improvements in surgical equipment during this period as well as differences in personal experiences and surgical skills. In the future, prospective studies are needed to clarify the impact of these issues on outcomes, and surgeons should identify a tailored and effective treatment for LACC. The assessment of quality of life was also not included in our study. Despite the lack of survival benefits of NAC, comprehensive evaluations including short and long-term complications should be pursued to provide sufficient evidence to clarify whether this strategy can improve the quality of life or the cost-effectiveness of treatment. The impact of surgical routs on the survival of cervical cancer is another important issue. Although a randomized trial [41] and an epidemiologic study [42] suggested minimally invasive surgeries could cause significant deteriorative survival outcomes, we could not support meaningful evidences in the field of NAC, since almost all the RH were performed in recent periods and in laparoscopic routs. The learning curves of one physician would significantly distract the stratification analysis.
Conclusions
Although NAC achieved a promising response rate in patients with FIGO stage IB2-to-IIB cervical cancer, no surgical, or survival benefits were observed in this cohort study. Responders to NAC may have better PFS and OS.
Abbreviations
- LACC:
-
Locally advanced cervical cancer
- NAC:
-
Neoadjuvant chemotherapy
- OS:
-
Overall survival
- PALN:
-
Para-aortic lymph nodes
- PF:
-
Fluorouracil and cisplatin
- PFS:
-
Progression-free survival
- PLN:
-
Pelvic lymph node
- RH:
-
Radical hysterectomy
- TC:
-
Paclitaxel and carboplatin
- TP:
-
Paclitaxel and cisplatin
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30. https://doi.org/10.3322/caac.21332
Chen W, Zheng R, Baade PD et al (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66:115–132. https://doi.org/10.3322/caac.21338
deSouza NM, Soutter WP, Rustin G et al (2004) Use of neoadjuvant chemotherapy prior to radical hysterectomy in cervical cancer: monitoring tumour shrinkage and molecular profile on magnetic resonance and assessment of 3-year outcome. Br J Cancer 90:2326–2331. https://doi.org/10.1038/sj.bjc.6601870
Panici PB, Bellati F, Plotti F et al (2008) Neoadjuvant chemotherapy followed by radical surgery in patients affected by vaginal carcinoma. Gynecol Oncol 111:307–311. https://doi.org/10.1016/j.ygyno.2008.07.005
Katsumata N, Yoshikawa H, Kobayashi H et al (2013) Phase III randomised controlled trial of neoadjuvant chemotherapy plus radical surgery vs radical surgery alone for stages IB2, IIA2, and IIB cervical cancer: a Japan Clinical Oncology Group trial (JCOG 0102). Br J Cancer 108:1957–1963. https://doi.org/10.1038/bjc.2013.179
Yang Z, Chen D, Zhang J et al (2016) The efficacy and safety of neoadjuvant chemotherapy in the treatment of locally advanced cervical cancer: a randomized multicenter study. Gynecol Oncol 141:231–239. https://doi.org/10.1016/j.ygyno.2015.06.027
Kim HS, Sardi JE, Katsumata N et al (2013) Efficacy of neoadjuvant chemotherapy in patients with FIGO stage IB1 to IIA cervical cancer: an international collaborative meta-analysis. Eur J Surg Oncol 39:115–124. https://doi.org/10.1016/j.ejso.2012.09.003
Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration (2010) Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: individual patient data meta-analysis. Cochrane Database Syst Rev 26:CD008285. https://doi.org/10.1002/14651858.cd008285
Minig L, Patrono MG, Romero N et al (2014) Different strategies of treatment for uterine cervical carcinoma stage IB2–IIB. World J Clin Oncol 5:86–92. https://doi.org/10.5306/wjco.v5.i2.86
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Cervical cancer. Version 2.2019—October 12, 2018. https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed 15 Dec 2018
Nama V, Angelopoulos G, Twigg J et al (2018) Type II or type III radical hysterectomy compared to chemoradiotherapy as a primary intervention for stage IB2 cervical cancer. Cochrane Database Syst Rev 10:CD011478. https://doi.org/10.1002/14651858.CD011478.pub2
Gupta S, Maheshwari A, Parab P et al (2018) Neoadjuvant chemotherapy followed by radical surgery versus concomitant chemotherapy and radiotherapy in patients with stage IB2, IIA, or IIB squamous cervical cancer: a randomized controlled trial. J Clin Oncol 36:1548–1555. https://doi.org/10.1200/JCO.2017.75.9985
Cibula D, Abu-Rustum NR, Benedetti-Panici P et al (2011) New classification system of radical hysterectomy: emphasis on a three-dimensional anatomic template for parametrial resection. Gynecol Oncol 122:264–268. https://doi.org/10.1016/j.ygyno.2011.04.029
Querleu D, Morrow CP (2008) Classification of radical hysterectomy. Lancet Oncol 9:297–303. https://doi.org/10.1016/s1470-2045(08)70074-3
Li L, Ma S, Tan X et al (2019) The urodynamics and survival outcomes of different methods of dissecting the inferior hypogastric plexus in laparoscopic nerve-sparing radical hysterectomy of type C: a randomized controlled study. Ann Surg Oncol 26:1560. https://doi.org/10.1245/s10434-019-07228-8
Pecorelli S, Zigliani L, Odicino F (2009) Revised FIGO staging for carcinoma of the cervix. Int J Gynecol Obstet 105:107–108. https://doi.org/10.1016/j.ijgo.2009.02.009
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Testa AC, Moro F, Pasciuto T et al (2018) PRospective Imaging of CErvical cancer and neoadjuvant treatment (PRICE) study: role of ultrasound to assess residual tumor in locally advanced cervical cancer patients undergoing chemoradiation and radical surgery. Ultrasound Obstet Gynecol 52:110–118. https://doi.org/10.1002/uog.18953
Obermair A, Gebski V, Frumovitz M et al (2008) A phase III randomized clinical trial comparing laparoscopic or robotic radical hysterectomy with abdominal radical hysterectomy in patients with early stage cervical cancer. J Minim Invasive Gynecol 15:584–588. https://doi.org/10.1016/j.jmig.2008.06.013
Common Terminology Criteria for Adverse Events (CTCAE) v4.03. National Cancer Institute. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50. Accessed 15 Dec 2018
Shimada M, Nagao S, Fujiwara K et al (2016) Neoadjuvant chemotherapy with docetaxel and carboplatin followed by radical hysterectomy for stage IB2, IIA2, and IIB patients with non-squamous cell carcinoma of the uterine cervix. Int J Clin Oncol 21:1128–1135. https://doi.org/10.1007/s10147-016-1010-0
Gadducci A, Landoni F, Cosio S et al (2018) Neoadjuvant platinum-based chemotherapy followed by radical hysterectomy for stage Ib2–IIb adenocarcinoma of the uterine cervix—an Italian Multicenter Retrospective Study. Anticancer Res 38:3627–3634. https://doi.org/10.21873/anticanres.12637
Tsubamoto H, Maeda H, Kanazawa R et al (2013) Phase II trial on neoadjuvant intravenous and trans-uterine arterial chemotherapy for locally advanced bulky cervical adenocarcinoma. Gynecol Oncol 129:129–134. https://doi.org/10.1016/j.ygyno.2013.01.007
Junker P, Puppe J, Thangarajah F et al (2018) Neoadjuvant therapy of cervical carcinoma with the angiogenesis inhibitor bevacizumab: a single-centre analysis. Geburtshilfe Frauenheilkd 78:768–774. https://doi.org/10.1055/a-0641-5588
Rydzewska L, Tierney J, Vale CL et al (2012) Neoadjuvant chemotherapy plus surgery versus surgery for cervical cancer. Cochrane Database Syst Rev 12:CD007406. https://doi.org/10.1002/14651858.CD007406.pub3
Mossa B, Mossa S, Corosu L et al (2010) Follow-up in a long-term randomized trial with neoadjuvant chemotherapy for squamous cell cervical carcinoma. Eur J Gynaecol Oncol 31:497–503
Kokka F, Bryant A, Brockbank E et al (2015) Hysterectomy with radiotherapy or chemotherapy or both for women with locally advanced cervical cancer. Cochrane Database Syst Rev 4:CD010260. https://doi.org/10.1002/14651858.CD010260.pub2
Wen H, Wu X, Li Z et al (2012) A prospective randomized controlled study on multiple neoadjuvant treatments for patients with stage IB2 to IIA cervical cancer. Int J Gynecol Cancer 22:296–302. https://doi.org/10.1097/IGC.0b013e31823610a1
Shoji T, Takatori E, Furutake Y et al (2016) Phase II clinical study of neoadjuvant chemotherapy with CDDP/CPT-11 regimen in combination with radical hysterectomy for cervical cancer with a bulky mass. Int J Clin Oncol 21:1120–1127. https://doi.org/10.1007/s10147-016-1008-7
Mahmoud O, Einstein MH (2018) Which patients with cervical squamous cell carcinoma might benefit from neoadjuvant chemotherapy? J Clin Oncol 36:1543–1547. https://doi.org/10.1200/JCO.2017.77.3416
Marchetti C, De Felice F, Di Pinto A et al (2018) Survival nomograms after curative neoadjuvant chemotherapy and radical surgery for stage IB2–IIIB cervical cancer. Cancer Res Treat 50:768–776. https://doi.org/10.4143/crt.2017.141
Pergialiotis V, Rodolakis A, Christakis D et al (2013) Laparoscopically assisted vaginal radical hysterectomy: systematic review of the literature. J Minim Invasive Gynecol 20:745–753. https://doi.org/10.1016/j.jmig.2013.04.021
Bentivegna E, Maulard A, Pautier P et al (2016) Fertility results and pregnancy outcomes after conservative treatment of cervical cancer: a systematic review of the literature. Fertil Steril 106:1195–1211. https://doi.org/10.1016/j.fertnstert.2016.06.032
Plante M (2015) Bulky early-stage cervical cancer (2–4 cm lesions): upfront radical trachelectomy or neoadjuvant chemotherapy followed by fertility-preserving surgery: which is the best option? Int J Gynecol Cancer 25:722–728. https://doi.org/10.1097/IGC.0000000000000410
Li J, Wang LJ, Zhang BZ et al (2011) Neoadjuvant chemotherapy with paclitaxel plus platinum for invasive cervical cancer in pregnancy: two case report and literature review. Arch Gynecol Obstet 284:779–783. https://doi.org/10.1007/s00404-011-1943-5
Fruscio R, Villa A, Chiari S et al (2012) Delivery delay with neoadjuvant chemotherapy for cervical cancer patients during pregnancy: a series of nine cases and literature review. Gynecol Oncol 126:192–197. https://doi.org/10.1016/j.ygyno.2012.04.027
Tang J, Tang Y, Yang J et al (2012) Chemoradiation and adjuvant chemotherapy in advanced cervical adenocarcinoma. Gynecol Oncol 125:297–302. https://doi.org/10.1016/j.ygyno.2012.01.033
Lan M, Chen C, Huang Y et al (2017) Neoadjuvant chemotherapy followed by concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in nasopharyngeal carcinoma patients with cervical nodal necrosis. Sci Rep 7:42624. https://doi.org/10.1038/srep42624
Ferrandina G, Palluzzi E, Gallotta V et al (2018) Neo-adjuvant platinum-based chemotherapy followed by chemoradiation and radical surgery in locally advanced cervical cancer (Lacc) patients: a phase II study. Eur J Surg Oncol 44:1062–1068. https://doi.org/10.1016/j.ejso.2018.04.019
Ferrandina G, Corrado G, Vitrano G et al (2018) Dose-dense paclitaxel/carboplatin as neo-adjuvant chemotherapy followed by radical surgery in locally advanced cervical cancer: a prospective phase II study. Cancer Chemother Pharmacol 83:431. https://doi.org/10.1007/s00280-018-3742-1
Ramirez PT, Frumovitz M, Pareja R et al (2018) Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med 379:1895–1904. https://doi.org/10.1056/NEJMoa1806395
Melamed A, Margul DJ, Chen L et al (2018) Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med 379:1905–1914. https://doi.org/10.1056/NEJMoa1804923
Funding
This work was supported by the Chinese Academy of Medical Sciences Initiative for Innovative Medicine (no. CAMS-2017-I2M-1-002). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
LL: assistant surgeon, protocol/project development, data management, data analysis, and manuscript drafting; MW: major surgeon and manuscript editing; SM, XT, SZ: assistant surgeons and data management.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Li, L., Wu, M., Ma, S. et al. Neoadjuvant chemotherapy followed by radical hysterectomy for stage IB2-to-IIB cervical cancer: a retrospective cohort study. Int J Clin Oncol 24, 1440–1448 (2019). https://doi.org/10.1007/s10147-019-01510-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01510-1