Abstract
Lynch syndrome (LS) is one of the most common genetic cancer syndromes, occurring at a rate of 1 per 250–1000 in the general population. This autosomal dominant disease is caused by a germline variant in one of the four mismatch repair genes, MSH2, MLH1, MSH6, PMS2, or the EPCAM gene. LS develops at early ages in colorectal cancer (CRC), endometrial cancer, and various other associated tumors. Accurate diagnosis of LS and utilization of various risk-reduction strategies such as surveillance, prophylactic surgery, and chemoprevention could improve clinical outcomes. The efficacy of surveillance has only been proven for CRC; however, specialists have proposed surveillance for other LS associated tumors. Universal screening for tumor tissue using microsatellite instability testing or the mismatch repair protein immunochemistry in all CRC or endometrial cancers is recommended not only as a diagnostic tool for LS, but also as a predictive, prognostic, and therapeutic marker. Next-generation sequencing methods have revealed several conditions with phenotypes similar to LS, such as Lynch-like syndrome, constitutional mismatch repair deficiency syndrome, and polymerase proofreading-associated polyposis. Distinguishing LS from these similar conditions is clinically important, since clinical management for patients differs according to the conditions. Recently, immune checkpoint inhibitors have been shown to be a promising treatment against mismatch repair-deficient (dMMR) solid tumors. The efficacy of immune-checkpoint inhibitors in LS-associated tumors has been shown to be similar to that in sporadic dMMR tumors. This review discusses current clinical topics related to LS screening, diagnosis, surveillance, and therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lynch syndrome (LS) is one of the most common genetic cancer syndromes and tends to occur in the form of various types of tumors at a young age, such as colorectal cancer (CRC) and endometrial cancer. Aldred S Warthin, M.D. first reported LS in 1913 [1], while Henry T Lynch, M.D. contributed to the concept of genetic cancer syndromes [2]. LS has a population prevalence of approximately 1 in 250–1,000 individuals [3,4,5,6] and accounts for 1–4% of all CRC cases [7,8,9]. The number of patients with LS in Japan is estimated to be more than 100,000. Recent progress in genomic medicine has led to new approaches that could be useful for the management of LS. This review describes the current clinical knowledge related to LS screening, differential diagnosis, surveillance, and therapy.
Clinical features
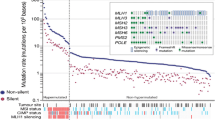
LS is an autosomal dominant disease caused by a pathogenic germline variant in a mismatch repair (MMR) gene. The causative genes are the four MMR genes MSH2, MLH1, MSH6, PMS2, and EPCAM [3, 4, 10]. EPCAM is upstream-adjacent to MSH2, and germline deletion of the 3′ end of EPCAM causes MSH2 silencing via methylation of the MSH2 promoter region [10]. The role of DNA MMR is to maintain genomic stability by correcting base mismatches and insertion–deletion mismatches that can arise during DNA replication. When the DNA MMR function is impaired, the sequence repeat number in simple repetitive sequences (microsatellites) is prone to changes. The altered number of repetitive sequences in microsatellites is termed microsatellite instability (MSI). Thus, LS-associated tumors, with variants in MMR genes, commonly show a high frequency of MSI (MSI-H) [3, 11].
Carriers of MMR gene variants are at high risk of early-onset LS-associated tumors, which include CRC, endometrial cancer (EC), gastric cancer, ovarian cancer, pancreas cancer, renal pelvic/ureteral cancer, biliary tract cancer, brain tumors, sebaceous tumors, keratoacanthoma, and small intestinal cancer [12]. In MSH2 and MLH1 gene variant carriers, the cumulative cancer risk up to age 70 years is 30–82% for CRC and 14–60% for EC [13, 14]. The risk of gastric cancer is 6–13% in Western countries [13] and 24% for Japan (up to age 60 years) [15]. The cumulative cancer risk for CRC in MSH6/PMS2 gene variant carriers is 10–22%, which is lower than that in MSH2/MLH1 variant carriers [13, 14]. Furthermore, the cumulative cancer risk for EC in MSH6 gene variant carriers is 16–71%, which is equivalent or higher than the risk for MSH2/MLH1 gene variant carriers (14–60%) [13, 14]. In addition, the cumulative risk of urinary tract cancer in MSH2/MLH1 gene variant carriers is high at 1–7% [13]. The tumor spectrum of LS has changed over time. The spectrum of LS in the family with LS first reported by Warthin included mainly gastric cancers and endometrial cancer [1]. However, follow-up reports of this family showed that in later generations, CRC was the most common tumor [2]. This change suggested that the cancer spectrum of LS is influenced by environmental factors, such as dietary and lifestyle habits, smoking, alcohol consumption, and obesity which interact with a host’s genetic factors, and may modulate the risk of developing cancer. Due to the high frequency of death due to gastric and biliary tract cancer among patients with LS in Japan, management of gastric cancer and biliary tract cancer is as important as that of CRC and EC [16] (Table 1).
Diagnosis
Approach for diagnosis
Since CRC and EC are the most common LS-associated tumors and develop at earlier ages, their development often can be a clue for diagnoses of LS. Traditionally, as the first step for the diagnosis of LS, clinical criteria such as the Amsterdam criteria II (Table 2) [17] or revised Bethesda guidelines (Table 3) [12] had been used for selecting individuals for further testing. However, screening by using these criteria or guidelines could miss more than one-fourth of LS cases [7]. In 2009, therefore, the Evaluation of Genomic Applications in Practice and Prevention working group recommend screening all patients with CRC using either MSI testing or immunohistochemistry (IHC) [18]. IHC can be used, as a complement to MSI testing, to evaluate the expression of the MLH1, MSH2, MSH6, and PMS2 proteins in tumor tissues [3, 9]. In LS, 90% CRC show high-frequency MSI (MSI-H) or abnormality in IHC [3, 11].
Ten to fifteen percent of all CRCs show MSI-H in Western countries [3, 13, 14], whereas, in Japan, 6–7% show MSI-H [5, 19, 20]. Tumors that show MSI-H or abnormalities in IHC for MMR proteins are called deficient MMR (dMMR). Individuals with dMMR tumor are subjected to MMR gene testing. However, dMMR is not specific for LS. Presence of dMMR, in most cases, indicates epigenetic hypermethylation of the MLH1 promoter region. To rule out sporadic MSI-H CRC, BRAF V600E testing can be used [3, 13, 14]. BRAF V600E somatic variant is observed in approximately 40% of sporadic MSI-H CRC cases [21, 22] but rarely in LS. IHC for BRAF protein expression (clone VE1) can also be used to rule out sporadic MSI-H CRC [23]. It is important to remember that the BRAF testing cannot be used for EC [24].
Nowadays, dMMR CRC screening is thought to be useful not only as a diagnostic tool for LS, but also as a predictive, prognostic, and therapeutic marker. [11, 25]; currently, many guidelines recommend universal screening for patients with CRC and/or EC [13, 14].
Given that, even universal screening would miss a small but significant minority (5–10%) of individuals with LS, and the frequency of the de novo variant in LS is low at 2.3% [26], it should be noted that recording family history is not reliable, but still an important complement to tumor testing. Additionally, because of the increased cost and heavy workloads for universal screening, genetic testing of relatives (known as cascade testing) is important for implementing the universal screening effectively.
Founder variants
More than 50 types of founder variants associated with LS have been reported worldwide [27]. In Japan, MLH1 variant (exon5 c.381–431_c.453 + 717del1221) is considered a founder variant [28, 29]. Notably, a Japanese nationwide study conducted by the Japanese Society for Cancer of the Colon and Rectum reported that large deletion or duplication was common (26.6%) in Japanese patients with LS [30] including the MLH1 founder variant. Therefore, if no pathological variant is detected using Sanger sequencing, the MLPA or other methods should be used to rule out large deletion or duplication.
Multi-gene panel testing
Conventionally, genetic testing is carried out in a step-wise manner; beginning with the most suspected gene, and if no genetic variant is detected, it proceeds to the second suspected gene. However, there are many types of tumors associated with LS, and phenotypes of LS overlap with a substantial number of other conditions and differential diagnoses. Therefore, stepwise genetic testing is too expensive and time consuming. With recent advances in NGS technology, multi-gene panel testing has been introduced since 2012 [31].
The benefits of multi-gene panel testing include: (1) high detection rate of pathologic variants, (2) cost-effectiveness, (3) suitability for sequencing a wide area of tumor suppressor genes in which hotspots are rare, and (4) clarification of the genotype-phenotype relations. Interestingly, the phenotypes for LS and BRCA1/2-associated hereditary breast and ovarian cancer syndrome have been shown to overlap. A study investigated individuals with suspected LS by multigene panel testing and identified 114 individuals with LS and 71 with variants in other cancer predisposition genes including 15 with BRCA1 or BRCA2 [32].
In contrast, the disadvantages of multi-gene panel testing include: (1) high detection rate of variants of uncertain significance, (2) lack of clinical management guidelines for moderate and low-penetrance genes, and (3) few standard genetic counseling models for multi-gene panel testing [33].
Differential diagnosis
There are many tumors associated with LS, and phenotypes of LS commonly overlap with other conditions. Typical differential diagnoses which show nonpolyposis colon cancer are as follows.
Constitutional mismatch repair deficiency (CMMRD) syndrome
CMMRD, also called biallelic MMR deficiency, is caused by homozygous or biallelic germline variants in MMR genes. During childhood, most patients develop CMMRD related tumors. Brain tumors are the most common, followed by CRC and hematological tumors [34]. Most patients have café au lait spots on their skin resembling neurofibromatosis 1 [35]. Gastrointestinal polyposis is observed in half of the patients [36]. In LS, variants of MSH2 or MLH1 are more common than MSH6 or PMS2. In contrast, the most common MMR gene observed in CMMRD is PMS2 followed by MSH6, MLH1, and MSH2 [37]. Interestingly, a recent study reported that MSH3, which is one of MMR genes but has not been proven to cause LS, also causes CMMRD [38]. These findings suggested that biallelic variants of MSH2 or MLH1 might more likely to be embryonic lethal [39]. Currently, very intensive surveillance programs are proposed for CMMRD [39].
Sporadic MSI-H CRC
Epigenetic hypermethylation of the promoter region of the MLH1 gene is the main cause of sporadic MSI-H CRC. The clinical features of sporadic MSI-H CRC include elderly females, poorly differentiated adenocarcinoma, and right-sided colon preponderance. IHC shows absence of MLH1 protein expression. The somatic variant of BRAF V600E is observed in approximately 40% of sporadic MSI-H CRC [11], but rarely in LS.
Lynch-like syndrome
Patients with LS-associated tumors that show dMMR without hypermethylation of the MLH1 promoter in the absence of a germline variant of MMR gene or EPICAM are termed to have “Lynch-like syndrome”. Lynch-like syndrome is a heterogeneous condition and mainly caused by epigenetic bi-allelic variant of MMR genes [35, 40]. Lynch-like syndrome accounts for 18–71% of patients with dMMR LS-associated tumors without MLH1 hypermethylation. CRC or EC in Lynch-like syndrome develops at earlier ages similar to LS. [5, 40, 41].
Familial CRC type X (FCCTX)
Families that meets Amsterdam criteria I (Table 1) [42], but who lack a germline variant in an MMR gene and an MSI-H tumor, are termed to have “familial CRC type X” [3, 43]. FCCTX is a heterogeneous condition. Candidates of causative gene include BRCA2, SEMA4, NTS, RASSF9, GALNT12, KRAS, BRAF, APC, BMPR1A, and RPS20, among others [44]. FCCTX accounts for approximately 40% of cases meeting Amsterdam criteria I. The onset age of CRC in FCCTX is 7.5 years more than that in LS, with the left-sided colon accounting for 70% of CRC cases. Histologically, this type is similar to sporadic CRC. The adenoma/carcinoma ratio is high and, the rate of development of cancer from adenoma is slow compared to LS [45, 46]. The risk of developing extracolonic LS-associated cancer is not increased in patients with FCCTX [15]. For surveillance of FCCTX, colonoscopy is conducted at intervals of 3–5 years, starting 5–10 years earlier than the earliest onset age of CRC in the family [45].
Polymerase proofreading-associated polyposis (PPAP)
PPAP is an autosomal dominant disease caused by germline variants in the proofreading (exonuclease) domains of DNA polymerases (DNA polymerase ɛ, POLE and DNA polymerase δ, POLD1) [47, 48]. Two hot spots of the gene variant have been reported (POLE p.Leu424Val and POLD1 p.Ser478Asn). Patients with germline POLE variants present oligo-adenomatous colorectal polyposis and CRC at an early age. Patients with germline POLD1 variants present EC and brain tumor as well as oligo-adenomatous colorectal polyposis and CRC at an early age. Although PPAP associated tumors show stable microsatellites, these tumors are hypermutated or ultramutated due to loss of polymerase proofreading function [49]. Therefore, PPAP associated tumors might benefit from immune-checkpoint inhibitor therapy [50].
Surveillance
The efficacy of surveillance in LS has only been demonstrated for CRC; a 3-year endoscopic surveillance was reported to reduce mortality due to CRC by 65% [51]. However, because cancers can occur over the testing interval of 3 years, colon surveillance with endoscopy should be performed from 20 to 25 years of age at intervals of 1–2 years [3, 13, 14]. Because the progression from colon adenoma to cancer in patients with LS is faster than that in the general population, adenomas regardless of their size should be removed in patients with LS [11]. Gastric surveillance with endoscopy should be performed from 30 to 35 years of age at intervals of 1–2 years. The presence of Helicobacter pylori infection should be evaluated from approximately 25 years of age, and if detected, treatment should be performed [11, 52]. Small intestinal cancer is another LS-associated cancer, and when performing gastroscopy or colonoscopy, the duodenum and ileum should be observed whenever possible. Uterine/ovary surveillance with transvaginal ultrasound, endometrial biopsy/cytology, and serum CA125 should be conducted from an age of 30–35 years at an interval of 6 months to one year. Urinary tract surveillance with urine tests/cytology should be conducted from an age of 30–35 years at intervals of 1–2 years [3, 13, 14, 52].
Risk reduction surgery
Risk reduction surgery for CRC
An extended colectomy for CRC could reduce the risk of metachronous CRC. It also makes colonoscopic surveillance of the residual colon easier [53]. Therefore, extended surgery such as total colectomy or total proctocolectomy might be a good option. However, in clinical studies, extended surgery did not show better prognosis of CRC compared to partial colectomy, and might reduce bowel function. The US Multi-Society Task Force on colorectal cancer strongly recommended extended colectomy for patients with colon cancer in LS based on moderate evidence [14], however, a European group (Mallorca group) could only provide a weak recommendation, which was based on their expert opinion [52]. Thus, at present, no consensus has been reached on whether extended surgery is better management for patients with LS.
Risk reduction surgery for EC, and ovarian cancer
It has been reported that prophylactic hysterectomy and bilateral salpingo-oophorectomy can greatly reduce the risk of EC and ovarian cancer, respectively [54]. Especially, at the time of CRC surgery, these prophylactic surgeries have been considered to be a good option. Before making a decision, both patients and surgeons should take into account the stage of CRC, age of patients, their desire to have children, menopausal status, and gene variant type, among other factors [3, 13, 14]. Notably, a recent prospective study described a good prognosis for EC (98% 10-year crude survival) or ovarian cancer (89% 10-year crude survival) in patients with LS without prophylactic surgery [55].
Chemoprevention/drug therapy
Chemoprevention of CRC
The CAPP2 trial was a randomized controlled trial of LS variant carriers that evaluated the efficacy of aspirin (600 mg/day) on CRC, extra-colonic LS-associated tumors, and colon adenoma. Long-term aspirin use (at least 2 years) significantly lowered the risk of developing CRC and extra-colonic cancers [56]. Currently, CAPP3 trial is ongoing to study the optimal dose and administration period of aspirin.
Postoperative adjuvant chemotherapy for CRC
Postoperative adjuvant chemotherapy with 5-FU did not improve prognosis in Stage II colon cancer with MSI-H [57]. In contrast, postoperative adjuvant chemotherapy with oxaliplatin improved prognosis in Stage III colon cancer with MSI-H. However, only a few studies have been conducted with a focus on patients with LS.
Chemotherapy for advanced/metastatic CRC
MSI-H CRC is reported to be more common among stage II (∼20%) than III (∼12%), and less frequent in stage IV CRC (∼4%) [58]. Efficacy of chemotherapy against metastatic dMMR CRC in patients with or without LS has not yet been clarified. Therefore, regimens for sporadic colorectal cancers are generally used for CRC in patients with LS.
Immune therapy for advanced or metastatic CRC (immune-checkpoint inhibitors) (Table 4)
The efficacy of immune-checkpoint inhibitors has been demonstrated against dMMR solid tumors. The US Food and Drug Administration (FDA) approved the use of checkpoint inhibitors in the treatment of dMMR solid tumors. PD-1 inhibitor monotherapies demonstrated no significant difference in the objective response rate for patients with or without LS: Pembrolizumab; 46 vs. 59%, and Nivolumab; 33% versus 29%, respectively [59, 60]. Combination immune therapy (Nivolumab plus Ipilimumab) demonstrated high response rates (55%) and disease control rate (80%) for ≥ 12 weeks [61].
References
Warthin AS (1913) Heredity with reference to carcinoma as shown by the study of the cases examined in the pathological laboratory of the University of Michigan, 1895–1913. Arch Int Med 12:546–555
Lynch HT, Shaw MW, Magnuson CW et al (1966) Hereditary factors in cancer. Study of two large midwestern kindreds. Arch Intern Med 117:206–212
Kohlmann W, Gruber SB (2004) Lynch syndrome. Gene Reviews. AVAILABLE via DIALOG. https://www.ncbi.nlm.nih.gov/books/NBK1211/. Accessed Apr 2018
InSiGHT (2018) Available via DIALOG. https://www.insight-group.org/. Accessed Apr 2018
Chika N, Eguchi H, Kumamoto K et al (2017) Prevalence of LS and Lynch-like syndrome among patients with colorectal cancer in a Japanese hospital-based population. Jpn J Clin Oncol 47:108–117
Jensen LH, Bojesen A, Byriel L et al (2013) Implementing population-based screening for Lynch syndrome. J Clin Oncol 31(Suppl):abstr 6600. https://meetinglibrary.asco.org/record/84519/poster. Accessed Apr 2018
Hampel H, Frankel WL, Martin E et al (2008) Feasibility of screening for LS among patients with colorectal cancer. J Clin Oncol 26:5783–5788
Moreira L, Balaguer F, Lindor N et al (2012) Identification of Lynch syndrome among patients with colorectal cancer. JAMA 308:1555–1565
Peltomäki P (2016) Update on Lynch syndrome genomics. Fam Cancer 15:385–393
Ligtenberg MJ, Kuiper RP, Chan TL et al (2009) Heritable somatic methylation and inactivation of MSH2 in families with Lynch syndrome due to deletion of the 3′ exons of TACSTD1. Nat Genet 41:112–117
Ishida H, Yamaguchi T, Tanakaya K et al (2018) Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2016 for the Clinical Practice of Hereditary Colorectal Cancer (Translated Version). J Anus Rectum Colon (JARC). http://journal-arc.jp/pdf/002s10001.pdf. Accessed Apr 2018
Umar A, Boland CR, Terdiman JP et al (2004) Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch Syndrome) and microsatellite instability. J Natl Cancer Inst 96:261–268
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN guidelines). Genetic/Familial High-Risk Assessment: Colorectal Version 3.2017. http://www.nccn.org. Accessed Feb 2018
Giardiello FM, Allen JI, Axilbund JE et al (2014) Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-Society Task Force on colorectal cancer. Gastroenterology 147:502–526
Yamaguchi T, Furukawa Y, Nakamura Y et al (2014) Comparison of clinical features between suspected familial colorectal cancer type X and LS in Japanese patients with colorectal cancer: a cross-sectional study conducted by the Japanese Society for Cancer of the Colon and Rectum. Jpn J Clin Oncol 45:153–159
Tanakaya K, Yamaguchi T, Ishikawa H et al (2016) Causes of cancer death among first-degree relatives in Japanese families with Lynch syndrome. Anticancer Res 36:1985–1989
Vasen HF, Mecklin JP, Khan PM et al (1991) The International Collaborative Group on hereditary non-polyposis colorectal cancer (ICG-HNPCC). Dis Colon Rectum 34:424–425
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group (2009) Recommendations from the EGAPP Working Group: genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives. Genet Med 11:35–41
Ishikubo T, Nishimura Y, Yamaguchi K et al (2004) The clinical features of rectal cancers with high-frequency microsatellite instability (MSI-H) in Japanese males. Cancer Lett 216:55–62
Asaka S, Arai Y, Nishimura Y et al (2009) Microsatellite instability-low colorectal cancer acquires a KRAS mutation during the progression from Dukes’ A to Dukes’ B. Carcinogenesis 30:494–499
Koinuma K, Shitoh K, Miyakura Y et al (2004) Mutations of BRAF are associated with extensive hMLH1 promoter methylation in sporadic colorectal carcinomas. Int J Cancer 108:237–242
McGivern A, Wynter CV, Whitehall VL et al (2004) Promoter hypermethylation frequency and BRAF mutations distinguish hereditary non–polyposis colon cancer from sporadic MSI-H colon cancer. Fam Cancer 3:101–110
Long GV, Wilmott JS, Capper D et al (2013) Immunohistochemistry is highly sensitive and specific for the detection of V600E BRAF mutation in melanoma. Am J Surg Pathol 37:61–65
Kawaguchi M, Yanokura M, Banno K et al (2009) Analysis of a correlation between the BRAF V600E mutation and abnormal DNA mismatch repair in patients with sporadic endometrial cancer. Int J Oncol 34:1541–1547
Le DT, Uram JN, Wang H et al (2015) PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med 372:2509–2520
Win AK, Jenkins MA, Buchanan DD et al (2011) Determining the frequency of de novo germline mutations in DNA mismatch repair genes. J Med Genet 48:530–534
Ponti G, Castellsagué E, Ruini C et al (2015) Mismatch repair genes founder mutations and cancer susceptibility in Lynch syndrome. Clin Genet 87:507–516
Sumitsuji I, Sugano K, Matsui T et al (2003) Frequent genomic disorganisation of MLH1 in hereditary non-polyposis colorectal cancer (HNPCC) screened by RT-PCR on puromycin treated samples. J Med Genet 40:e30
Utsumi M, Tanakaya K, Mushiake Y et al (2017) Metachronous colorectal carcinoma with massive submucosal invasion detected by annual surveillance in a LS patient: a case report. World J Surg Oncol 15:140
Furukawa Y (2013) Genetic changes of Japanese Lynch syndrome (in Japanese). Intestine 17:2–5
Pritchard CC, Smith C, Salipante SJ et al (2012) ColoSeq provides comprehensive lynch and polyposis syndrome mutational analysis using massively parallel sequencing. J Mol Diagn 14:357–366
Yurgelun MB, Allen B, Kaldate RR et al (2015) Identification of a variety of mutations in cancer predisposition genes in patients with suspected Lynch Syndrome. Gastroenterology 149:604–613
Bradbury AR, Patrick-Miller L, Long J et al (2015) Development of a tiered and binned genetic counseling model for informed consent in the era of multiplex testing for cancer susceptibility. Genet Med 17:485–492
Bakry D, Aronson M, Durno C et al (2014) Genetic and clinical determinants of constitutional mismatch repair deficiency syndrome: report from the constitutional mismatch repair deficiency consortium. Eur J Cancer 50:987–996
Carethers JM, Stoffel EM (2015) Lynch syndrome and Lynch syndrome mimics: The growing complex landscape of hereditary colon cancer. World J Gastroenterol 21:9253–9261
Wimmer K, Etzler J (2008) Constitutional mismatch repair-deficiency syndrome: have we so far seen only the tip of an iceberg? Hum Genet 124:105–122
Rana Q, Syngal HS (2017) Biallelic mismatch repair deficiency: management and prevention of a devastating manifestation of the Lynch syndrome. Gastroenterology 152:1254–1257
Adam R, Spier I, Zhao B et al (2016) Exome sequencing identifies biallelic MSH3 germline mutations as a recessive subtype of colorectal adenomatous polyposis. Am J Hum Genet 99:337–351
Durno C, Boland CR, Cohen S et al (2017) Recommendations on surveillance and management of biallelic mismatch repair deficiency (BMMRD) syndrome: a consensus statement by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2017 152:1605–1614
Rodríguez-Soler M, Pérez-Carbonell L, Guarinos C et al (2013) Risk of cancer in cases of suspected lynch syndrome without germline mutation. Gastroenterology 144:926–932
Dillon JL, Gonzalez JL, DeMars L et al (2017) Universal screening for Lynch syndrome in endometrial cancers: frequency of germline mutations and identification of patients with Lynch-like syndrome. Hum Pathol 70:121–128
Vasen HF, Watson P, Mecklin JP et al (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology 116:1453–1456
Lindor NM, Rabe K, Petersen GM et al. (2005) Lower cancer incidence in Amsterdam-I criteria families without mismatch repair deficiency: familial colorectal cancer type X. JAMA 293:1979–1985
Garre P, Martin L, Sanz J et al (2015) BRCA2 gene: a candidate for clinical testing in familial colorectal cancer type X. Clin Genet 87:582–587
Dominguez-Valentin M, Therkildsen C, Da Silva S et al (2014) Familial colorectal cancer type X: genetic profiles and phenotypic features. Mod Pathol 28:30–36
Nejadtaghi M, Jafari H, Farrohki E et al (2017) Familial Colorectal Cancer Type X (FCCTX) and the correlation with various genes-A systematic review. Curr Probl Cancer 41:388–397
Palles C, Cazier JB, Howarth KM et al (2013) Germline mutations affecting the proofreading domains of POLE and POLD1 predispose to colorectal adenomas and carcinomas. Nat Genet 45:136–144
Briggs S, Tomlinson I (2013) Germline and somatic polymerase ε and δ mutations define a new class of hypermutated colorectal and endometrial cancers. J Pathol 230:148–153
Seshagiri S (2013) The burden of faulty proofreading in colon cancer. Nat Genet 45:121–122
Bourdais R, Rousseau B, Pujals A et al (2017) Polymerase proofreading domain mutations: New opportunities for immunotherapy in hypermutated colorectal cancer beyond MMR deficiency. Crit Rev Oncol Hematol 113:242–248
Järvinen HJ, Aarnio M, Mustonen H et al (2000) Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 118:829–834
Vasen HF, Blanco I, Aktan-Collan K et al (2013) Revised guidelines for the clinical management of LS (HNPCC): recommendations by a group of European experts. Gut 62:812–823
Parry S, Win AK, Parry B, et.al (2011) Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 60:950–957
Schmeler KM, Lynch HT, Chem LM et al (2006) Prophylactic surgery to reduce the risk of gynecologic cancers in the Lynch syndrome. N Engl J Med 354:261–269
Møller P, Seppälä T, Bernstein I et al (2017) Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective Lynch syndrome database. GUT 66:464–472
Burn J, Gardes AM, Macrae F et al (2011) Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet 378:2081–2087
Sargent DJ, Marsoni S, Monges G et al (2010) Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol 28:3219–3226
Goldstein J, Tran B, Ensor J et al (2014) Multicenter retrospective analysis of metastatic colorectal cancer (CRC) with high-level microsatellite instability (MSI-H). Ann Oncol 25:1032–1038
Le DT, Durham JN, Smith KN et al (2017) Mismatch-repair deficiency predicts response of solid tumors to PD-1 blockade. Science 357:409–413
Overman MJ, McDermott R, Leach JL et al (2017) Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 18:1182–1191
Overman MJ, Lonardi S, Wong KYM et al (2018) Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal cancer. J Clin Oncol 36:773–779
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest to disclose.
About this article
Cite this article
Tanakaya, K. Current clinical topics of Lynch syndrome. Int J Clin Oncol 24, 1013–1019 (2019). https://doi.org/10.1007/s10147-018-1282-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-018-1282-7