Abstract
Background
Small-sized HCC can be effectively cured by surgery with good clinical outcomes. A highly sensitive HCC α-fetoprotein routine test (HCC-ART) for HCC diagnosis as well as a simplied form of the HCC-ART were reported in the British Journal of Cancer. Here, we verified and studied the applicability of the HCC-ART to the detection of early-stage HCC.
Methods
341 cirrhotic patients and 318 HCC patients were included in this study. For each, the HCC-ART score was calculated, and then the sensitivity, specificity, and results of an ROC curve analysis were compared between the HCC-ART and AFP when these biomarkers were used to detect small-sized HCC.
Results
Different HCC-ART cutoffs were set for the detection of different tumor sizes. The HCC-ART (AUC = 0.871, 70% sensitivity, 97% specificity) and the simplified HCC-ART (AUC = 0.934, 82% sensitivity, 100% specificity) were found to have high predictive power when attempting to separate cirrhotic patients from those with small-sized HCC. The simplified HCC-ART score was superior to AFP for determining stages according to the early Okuda (0.950 AUC, 84% sensitivity, 99% specificity), CLIP (0.945 AUC, 84% sensitivity, 99% specificity), and BCLC (1.000 AUC, 100% sensitivity, 99% specificity) staging systems. The simplified HCC-ART score was more strongly correlated than AFP and other staging systems with HCC tumor size (P < 0.0001; r = 0.8).
Conclusion
The HCC-ART is superior to AFP for diagnosing early-stage HCC. Due to its advantages of minimal variability and a wide continuous scale for assessing HCC severity, the simplified HCC-ART has the potential to be more widely used than the original HCC-ART.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver cancer is generally associated with less-developed regions. Indeed, 83% of the estimated 782,000 new liver cancer cases that occurred worldwide in 2012 were in less-developed regions [1]. Early diagnosis is important for successful treatment by means of ablation, resection, and/or transplant [2]. While effective HCC treatment is usually curative surgery, about 80% of patients are inoperable at presentation and die early due to late diagnosis [3]. Thus, identifying effective screening strategies to detect early-stage HCC is of the utmost importance as it could result in more effective treatment and extend patient survival [4].
Although α-fetoprotein (AFP) is routinely used for screening and has been widely applied in HCC surveillance programs, it often gives normal or indeterminate results in early cancer cases. AFP is a low-sensitivity biomarker that is normal in up to 50% of patients with HCC, particularly during the early stages of the disease (HCC ≤ 3 cm) [5]. Other modalities such as ultrasonography (US) and conventional tumor markers such as α-fetoprotein-L3 (AFP-L3) and des-γ-carboxyprothrombin (DCP) are also widely used and important for HCC detection in clinical settings [6]. However, none of these modalities provides an entirely satisfactory means of detecting HCC in its early stages [7].
Recently, a clinically useful scoring system, the HCC α-fetoprotein routine test (HCC-ART), was developed for the diagnosis of patients with HCC [8]. The area under the curve, sensitivity, specificity, and accuracy of the HCC-ART for differentiating HCC from non-malignant liver cirrhosis were found to be 0.99, 97, 96, and 96%, respectively. Moreover, the HCC-ART showed absolute sensitivity and specificity (100%) when discriminating patients with HCC from those with liver fibrosis and those without fibrosis. Subsequently, a simplified version of the HCC-ART was devised in which a numerical constant and coefficients were removed from the original HCC-ART, and this simplified HCC-ART was observed to yield similar promising results to the original HCC-ART.
Because there is an urgent need to identify novel biomarkers that can be used to detect early HCC, in the large-scale study reported in the present paper, we employed HCC-ART and its simplified form to detect HCC patients with tumors of various sizes, ranging from small (≤2 cm) to very large (≥10 cm), in order to evaluate the clinical applicability of these tests to the early diagnosis and differentiation of small-sized HCC from liver cirrhosis. The widely used Okuda, CLIP, and BCLC systems were used as standard HCC staging systems, and the HCC-ART score was identified as a potential biomarker for early-stage HCC.
Patients and methods
Patient selection
659 consecutive patients (318 patients with HCC and 341 with liver cirrhosis) who were admitted to the Tropical Medicine Unit (Mansoura University Hospitals, Mansoura, Egypt) were enrolled in this study. All of the HCC patients had chronic hepatitis C or liver cirrhosis as the underlying liver disease. The diagnosis of HCC in those patients was made according to the American Association for the Study of Liver Diseases (AASLD) practice guidelines [9]. The tumors were detected by abdominal ultrasound (US) studies and/or AFP assays (>400 U/L). Each focal lesion detected was further evaluated by multiphase spiral computed tomography (CT) or contrast-enhanced magnetic resonance imaging (MRI). The presence of enhancement in the arterial phase was considered diagnostic for HCC if the lesion was larger than 2 cm. The final diagnosis was, whenever possible, confirmed by histopathologic analysis on US-assisted fine-needle biopsy. Informed consent was obtained from each patient and the study protocols followed the ethical guidelines of the 1975 Declaration of Helsinki.
Differentiation of HCC stage
The tumor size was defined by contrast CT or MRI scan. HCC patients were divided according to tumor size into four groups: small tumor (size ≤2 cm, n = 25); medium tumor (size 3–5 cm, n = 130); large tumor (size 6–9 cm, n = 97); and very large tumor (size ≥10 cm, n = 66). The Okuda classification [10] is widely applied in HCC patients. It includes parameters related to liver functional status (albumin, ascites, bilirubin) and to the tumor stage (proportion of the area of the liver involved). All HCC patients were divided into three groups: early stage (0 points, n = 115); intermediate stage (1 or 2 points, n = 169); and advanced stage (3 or 4 points, n = 34). The Cancer of the Liver Italian Program (CLIP) score [11] was also determined. This score combines four variables and provides a seven-stage classification system. The HCC patients studied were divided into three groups: early HCC (stages 0–1, n = 100); intermediate HCC (stages 2–3, n = 175); and advanced HCC (stages ≥4, n = 43). Moreover, tumor stage was defined according to the Barcelona Clinic Liver Cancer (BCLC) staging system as either early (stage 0-A, n = 76), intermediate (stage B, n = 86), advanced (stage C, n = 76), or end-stage (stage D, n = 80).
Sample collection and laboratory tests
Fasting blood samples were collected from all patients and divided into two parts; one was collected without an anticoagulant and the second was drawn into KEDTA tubes for a complete blood count. Sera were separated and tested fresh in liver function tests using an automated biochemistry analyzer (model A15, Biosystems S.A., Barcelona, Spain). The AFP level was determined by chemiluminescence with an Immulite AFP (1000) kit (Diagnostic Products Corporation, Los Angeles, CA, USA). In addition, serologic tests were carried out for HCV using commercial ELISA kits (ETI-AB-HCVK-3 kit, Sorine Biomedica, Suluggia, Italy). Complete blood counts were performed on a KX-21 automated hematology analyzer (Sysmex Corporation, Kobe, Japan).
Statistical analysis
All statistical analyses were carried out using the Statistical Package for the Social Sciences (SPSS, SPSS Inc., Chicago, IL, USA) software, version 15.0, running in Microsoft Windows XP, as well as the GraphPad Prism package; v.5.0 (GraphPad Software, San Diego, CA, USA). Continuous variables were expressed as the mean ± SD or SEM, whereas categorical variables were expressed as numbers. ANOVA was used in cases where the Kolmogorov–Smirnov test results were not significant, while the Mann–Whitney U test was used in cases with nonparametric variables. The main endpoint was the identification of patients with hepatocellular carcinoma vs. liver cirrhosis. In secondary analyses, the accuracies of HCC-ART and AFP at discriminating HCC patients according to tumor size (small, medium, and large) were evaluated using the area under the ROC curve. The third step was to evaluate the predictive power of HCC-ART for the diagnosis of early-stage HCC in the Okuda, CLIP, and BCLC staging systems. The best cutoff values for the optimal prediction of HCC were determined from the ROC curves. In a fourth step, the correlations of HCC-ART and AFP with tumor size and different HCC classification systems were evaluated by Pearson’s correlation coefficient. A P value of <0.05 was considered statistically significant. The sensitivities and specificities of the HCC-ART and AFP were derived from a 2 × 2 contingency table.
Results
Clinicopathological profiles of the patients
The clinicopathological findings (age, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), albumin, platelet count, presence of ascites, and tumor size) were evaluated (Table 1). The HCC patients were older than the cirrhotic patients. Univariate analysis of all tested variables except for ALT revealed that there was a significant difference (P < 0.05) between the HCC and liver cirrhosis patients. The original and simplified HCC-ART [8] indices for discriminating patients with HCC were calculated using the following formulae: HCC-ART score = [2.17 + [log(AFP−1) × 10 × 0.117] + AST/ALT ratio × 0.025 + age × 0.012 + alkaline phosphatase (U/L) × 0.001] − [albumin (g/L) × 0.015]; simplified HCC-ART = [age (years) × log AFP (U L−1) AAR × ALP (U L−1)]/[Alb (g−1)].
HCC-ART is superior to serum AFP for the detection of small-sized HCCs
We compared HCC-ART with AFP in terms of their ability to differentiate different tumor sizes. The values of both HCC-ART and its simplified form gradually increased as the tumor size expanded from small (≤2 cm) to very large tumors (≥10 cm) (P = 0.001 for HCC-ART, P = 0.01 for simplified HCC-ART). In contrast, AFP levels fluctuated in a nonsignificant manner as the tumor increased (P = 0.10). HCC-ART at a cutoff level of ≥2.5 detected small HCCs (≤2 cm) with a sensitivity of 70%. At the same cutoff value, HCC-ART has a specificity of 97% for separating non-neoplastic liver cirrhotic subjects from those with small HCCs. Notably, the sensitivity increased from 70% for small HCCs to 94% for medium-sized HCCs, 90% for large HCCs, and 93% for very large HCCs (Table 2).
Interestingly, the simplified HCC-ART gave superior results to the original HCC-ART when a cutoff of ≥280 was used to differentiate non-neoplastic liver cirrhotic subjects from those with small tumors (Table 2). In the same cohort of patients, AFP was less sensitive (12%) for detecting small HCC tumors (cutoff ≥400 U/L), and its expression increased with increasing tumor size. When we used a cutoff of ≥200 U/L, the sensitivity rose to 18% (not significantly different from the sensitivity obtained with a cutoff of ≥400 U/L). ROC analysis also showed that HCC-ART (AUC: 0.871) and its simplified form (AUC: 0.934) were superior to serum AFP (AUC: 0.560) for separating non-neoplastic individuals from those with small HCCs (Table 2). These results are consistent with previous reports that AFP is insensitive to small HCCs [8].
Predictive power of HCC-ART in the diagnosis of early-stage HCC according to common staging systems
As a consequence of these favorable characteristics, we further compared the diagnostic performance of HCC-ART with that of serum AFP for the diagnosis of early-stage HCC according to three commonly employed staging systems.
Okuda
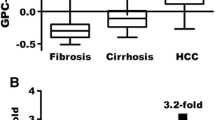
The Okuda score is used as a standard classification of HCC. In contrast to AFP, the HCC-ART score (mean ± SEM) significantly increased from stage 1 (2.7 ± 0.01) to stage 3 (3.3 ± 0.2). Similarly, the simplified HCC-ART score gradually increased (P = 0.04) with Okuda stage progression (Fig. 1a–c), although the range of simplified HCC-ART scores was wider than the corresponding range of scores for the original HCC-ART. Sensitivities to Okuda early-stage tumors were 90, 84, 42, and 52 for HCC-ART, simplified HCC-ART, AFP (≥400 U/L), and AFP (≥200 U/L), respectively.
Distribution of HCC-ART scores, simplified HCC-ART scores, and AFP values in different common HCC staging systems. In contrast to AFP, HCC-ART and simplified HCC-ART scores (mean ± SEM) increased significantly with the Okuda stage (a HCC-ART, b simplified HCC-ART, c AFP), CLIP stage (d HCC-ART, e simplified HCC-ART, f AFP), and BCLC stage (g HCC-ART, h simplified HCC-ART, i AFP) of the HCC tumor. AFP values fluctuated with HCC stage progression in a nonsignificant manner. One-way ANOVA was used to check differences between groups for statistical significance. P > 0.05 was considered to indicate a nonsignificant and P < 0.05 to indicate a significant difference
CLIP (Cancer of the Liver Italian Program score)
When CLIP was used as the standard score to define different HCC stages, HCC-ART and its simplified form increased (P < 0.0001 for HCC-ART and P = 0.02 for simplified HCC-ART) with CLIP score progression (from 0–1 to ≥4). In contrast, AFP levels fluctuated with CLIP stage progression in a nonsignificant manner (P = 0.10) (Fig. 1d–f). Sensitivities to early-stage CLIP early were 93, 84, 10, and 11 for HCC-ART, simplified HCC-ART, AFP (≥400 U/L), and AFP (≥200 U/L), respectively.
BCLC (Barcelona Clinic Liver Cancer)
Furthermore, in contrast to AFP, HCC-ART and its simplified form were able to distinguish with high statistical significance between BCLC stages ranging from early to end-stage (Fig. 1g–i). Sensitivities to early-stage BCLC were 85, 100, 8, and 8 for HCC-ART, simplified HCC-ART, AFP (≥400 U/L), and AFP (≥200 U/L), respectively (Table 3).
Overall, HCC-ART at a cutoff of ≥2.5 and simplified HCC-ART at a cutoff of ≥280 appeared to be superior, more sensitive markers than serum AFP for detecting different HCC stages (Table 3). Likewise, the diagnostic value of these formulae was high; there was a large area under the ROC curve for distinguishing early-stage tumors according to the Okuda, CLIP, and BCLC schemes (Table 3). Increased HCC-ART (r = 0.5, P < 0.0001) and simplified HCC-ART (r = 0.8, P < 0.0001) values were found to be correlated with HCC tumor size significantly better than the Okuda (r = 0.2, P = 0.03), CLIP (r = 0.2, P = 0.02), BCLC (r = 0.2, P = 0.03), and AFP (r = 0.1, P = 0.03) (Table 4).
Discussion
No treatment appears to be capable of prolonging survival in patients with large HCC tumors [12]. The conventional biomarker AFP, its glycated isoforms, and other modalities are widely used to detect HCC [5, 6]. However, their accuracy for detecting early-stage HCCs is poor [7]. So far, no reliable biomarker for detecting small HCCs has been reported; thus, novel biomarkers are urgently needed for these tumors.
Recently, an exciting study suggested that the use of a novel predictive model, the HCC-ART score, could increase the accuracy of HCC screening and surveillance [8]. In the present work, we have made significant improvements to the reliability of that model by verifying its applicability to the detection of small-sized and early-stage HCC. We found that the HCC-ART score increased significantly as tumor size increased from small to very large. For small tumors (≤2 cm), the calculated AUC values for the HCC-ART, the simplified HCC-ART, and AFP were 0.871, 0.934, and 0.560, respectively, indicating that the HCC-ART is a superior small-HCC biomarker to AFP. The sensitivities of these biomarkers to small (≤2 cm) and medium-sized (3–5 cm) HCCs were 70 and 97% for the HCC-ART, 82 and 100% for the simplified HCC-ART, and 12 and 100% for AFP, respectively. Excellent results were obtained when the HCC-ART was used to distinguish between different tumor sizes.
Due to these favorable characteristics, the differential diagnostic accuracy of the HCC-ART for detecting early-stage HCC according to the Okuda (stage 1), CLIP (0-1), and BCLC (stage A) staging systems was assessed. Another attractive aspect of the HCC-ART is that it has a higher AUC and sensitivity than and comparable specificity to AFP for the detection of early-stage HCC (Table 3). Increased HCC-ART score was significantly correlated with HCC tumor size as well as Okuda, CLIP, and BCLC stage.
The outcomes derived from this study compared favorably with other biomarkers used for the diagnosis of early-stage HCC. For example, high serum concentrations of DCP are present in 50–60% of all HCC patients, but in only 15–30% of early-stage HCC cases [13]. AFP-L3 exhibits a sensitivity of only 35% in patients with small HCC (<2 cm) [14]. Recently, similar promising results were obtained when the biomarker Dickkopf-1 (DKK1), a secretory antagonist of the canonical Wnt signaling pathway, was employed to detect early-stage HCC (70.9% sensitivity and 90.5% specificity) [15]. However, it is unlikely that DKK1 is specific for HCC. Overexpression of DKK-1 has been reported in many malignant tissues, including breast, lung, esophageal, ovarian, and gastric cancers [16]. In contrast, our model is based on inflammatory markers, markers associated with liver fibrosis, and AFP, all of which are associated with liver cell proliferation; they reflect the disease status of the liver.
The application of a staging system is important not only for obtaining prognostic information but also in management planning. For HCC, there are many proposed staging systems [17]. The classifications most commonly used for HCC are the Okuda, CLIP, and BCLC staging systems. Although the Okuda staging system was the first classification to include both tumor parameters and liver function factors [10], its main problem is that the assessment of tumor burden is applicable only to advanced-stage tumors [18]. The most robust predictors of HCC prognosis are portal vein thrombosis, tumor size, AFP, and Child–Pugh class. Interestingly, the CLIP system, one of the most commonly used HCC-staging systems, includes all of these predictors [19]. A consensus conference, the Americas Hepato-Pancreato-Biliary Association/American Joint Committee on Cancer Conference, endorsed the use of CLIP for prognostic HCC staging because it was the only externally validated staging system [20]. The CLIP score has been well validated for the detection of HCC in Western patients. However, a CLIP score of zero is a tumor extent of less than 50% of the liver, and 50% of the liver is a fairly large tumor considering that many early-stage HCCs with nodules less than 2 cm in diameter can routinely be detected in many countries [21]. The BCLC staging for HCC is currently the only system that includes an integrated assessment of liver disease, tumor extension, and presence of constitutional symptoms, providing an indication of the first-line treatment [22]. It is based on the possibility of curative intervention, so, the BCLC staging system is actually an extension of the treatment-decision algorithm rather than a prognostic system [18]. Studies that have evaluated more than these three systems have shown that the BCLC system is the most useful [23]. We found that, among the three staging systems, the HCC-ART score showed the strongest correlation (r = 0.7, P < 0.0001) with the BCLC system. There was a strong positive correlation between the simplified HCC-ART (r = 0.8; P < 0.0001) and the tumor size in contrast to Okuda, CLIP and BCLC scores.
The HCC-ART is based on simple, noninvasive, and routinely measured biomarkers (age, AFP, aspartate aminotransferase/alanine aminotransferase ratio (AAR), alkaline phosphatase, and albumin). Oxidative DNA damage is known to contribute to the progression of chronic liver damage to HCC, and is correlated with the induction of telomerase and repair enzyme activity [24, 25]. On the other hand, these repair mechanisms, such as CuZn superoxide dismutase [26], are known to degrade with age, and the hOGG1 gene encodes a DNA glycosylase [27] that contributes to hepatocarcinogenesis in the presence of persistent oxidative damage. AFP alone cannot be considered the ideal biomarker for HCC. However, the combined detection of AFP along with other complementary serum biomarkers could improve the early diagnostic rate of HCC [28]. A higher AAR has been reported in patients with HCC compared with those with cirrhosis, likely due to an increase in cytosolic aspartate aminotransferase [29]. AAR in combination with age, AFP, albumin, and other liver-related seromarkers were recently included in predictive models for the risk of HCC [30]. Recent studies suggest that ALP could serve as an easy-to-assess biomarker that permits the early prediction of HCC recurrence after hepatectomy of large tumors [31, 32]. Liver carcinogenesis is associated with a decrease in serum albumin due to liver impairment. The level of serum human albumin is usually normal in chronic liver diseases until the onset of cirrhosis and the development of primary liver cancer.
The most robust predictors of death in HCC patients are tumor-related (e.g., AFP) and liver-related (e.g., AAR, ALP, and albumin), and these are included in the HCC-ART [19]. Thus, applying the HCC-ART may improve the prognosis of HCC. Nevertheless, in order to determine the actual prognostic value of the HCC-ART in HCC cases, further studies comparing its accuracy in a large population to other staging systems are required. Although validation studies that apply the HCC-ART in different institutions, different patient groups, and different countries are needed, we propose that the HCC-ART is a highly sensitive and specific score for differentiating small-sized and early-stage HCC from liver cirrhosis. Because it is quite easy to determine the HCC-ART score via routine laboratory tests, we strongly recommend its routine use in clinical practice. Also, because it gives similar promising results to the original HCC-ART and its advantage of minimal variability and a wide continuous scale for assessing HCC severity, the simplified HCC-ART has the potential to be even more widely used than the original HCC-ART.
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:359–386
Mustafa MG, Petersen JR, Ju H et al (2013) Biomarker discovery for early detection of hepatocellular carcinoma in hepatitis C-infected patients. Mol Cell Proteomics 12:3640–3652
Zhao C, Yan F, Wu H et al (2013) DNMT3A -448A > G polymorphism and the risk for hepatocellular carcinoma. Biomed Rep 1:664–668
El-Serag HB (2011) Hepatocellular carcinoma. N Engl J Med 365:1118–1127
Gebo KA, Chander G, Jenckes MW et al (2002) Screening tests for hepatocellular carcinoma in patients with chronic hepatitis C: a systematic review. Hepatology 36:84–92
Dohmen K, Shirahama M, Onohara S et al (2000) Differences in survival based on the type of follow-up for the detection of hepatocellular carcinoma: an analysis of 547 patients. Hepatol Res 18:110–121
Miura N, Osaki Y, Nagashima M et al (2010) A novel biomarker TERTmRNA is applicable for early detection of hepatoma. BMC Gastroenterol 10:46–57
Attallah AM, Omran MM, Attallah AA et al (2013) HCC-ART score, a simple, highly sensitive and specific test for early diagnosis of hepatocellular carcinoma: a large-scale, multicentre study. Br J Cancer 109:1657–1665
Bruix J, Sherman M (2005) Management of hepatocellular carcinoma. Hepatology 42:1208–1236
Okuda K, Ohtsuki T, Obata H et al (1985) Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Cancer 56:918–928
CLIP (2000) Prospective validation of the CLIP score: a new prognostic system for patients with cirrhosis and hepatocellular carcinoma. Hepatology 31:840–845
Grieco A, Pompili M, Caminiti G et al (2005) Prognostic factors for survival in patients with early-intermediate hepatocellular carcinoma undergoing non-surgical therapy: comparison of Okuda, CLIP, and BCLC staging systems in a single Italian centre. Gut 54:411–418
Weitz IC, Liebman HA (1993) Des-gamma-carboxy (abnormal) prothrombin and hepatocellular carcinoma: a critical review. Hepatology 18:990–997
Li D, Mallory T, Satomura S (2001) AFP-L3: a new generation of tumor marker for hepatocellular carcinoma. Clin Chim Acta 313:15–19
Shen Q, Fan J, Yang XR et al (2012) Serum DKK1 as a protein biomarker for the diagnosis of hepatocellular carcinoma: a large-scale, multicentre study. Lancet Oncol 13:817–826
Prieto PA, Cha CH (2013) DKK1 as a serum biomarker for hepatocellular carcinoma. Hepatobiliary Surg Nutr 2:127–128
Sirivatanauksorn Y, Tovikkai C (2011) Comparison of staging systems of hepatocellular carcinoma. HPB Surg 2011:818217
Camma C, Cabibbo G (2009) Prognostic scores for hepatocellular carcinoma: none is the winner. Liver Int 29:478–480
Tandon P, Garcia-Tsao G (2009) Prognostic indicators in hepatocellular carcinoma: a systematic review of 72 studies. Liver Int 29:502–510
Henderson JM, Sherman M, Tavill A et al (2003) AHPBA/AJCC consensus conference on staging of hepatocellular carcinoma: consensus statement. HPB Surg 5:243–250
Kudo M, Chung H, Osaki Y (2003) Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score (JIS score). J Gastroenterol 38:207–215
Maida M, Orlando E, Cammà C et al (2014) Staging systems of hepatocellular carcinoma: a review of literature. World J Gastroenterol 20:4141–4150
Giannini E, Risso D, Botta F et al (2004) Prognosis of hepatocellular carcinoma in anti-HCV positive cirrhotic patients: a single-centre comparison amongst four different staging systems. J Intern Med 255:399–408
Cardin R, Piciocchi M, Sinigaglia A et al (2012) Oxidative DNA damage correlates with cell immortalization and mir-92 expression in hepatocellular carcinoma. BMC Cancer 12:177
Cardin R, Piciocchi M, Bortolami M et al (2014) Oxidative damage in the progression of chronic liver disease to hepatocellular carcinoma: an intricate pathway. World J Gastroenterol 20:3078–3086
Elchuri S, Oberley TD, Qi W et al (2005) CuZnSOD deficiency leads to persistent and widespread oxidative damage and hepatocarcinogenesis later in life. Oncogene 24:367–380
Wang W, Dang S, Li Y et al (2013) hOGG1 Ser326Cys polymorphism and risk of hepatocellular carcinoma among East Asians: a meta-analysis. PLoS One 8:e60178
Zhao YJ, Ju Q, Li GC (2013) Tumor markers for hepatocellular carcinoma. Mol Clin Oncol 1:593–598
Lai CL, Lam KC, Wong KP et al (1981) Clinical features of hepatocellular carcinoma: review of 211 patients in Hong Kong. Cancer 47:2746–2755
Lin YJ, Lee MH, Yang HI et al (2013) Predictability of liver-related seromarkers for the risk of hepatocellular carcinoma in chronic hepatitis B patients. PLoS One 8:e61448
Kim JM, Kwon CH, Joh JW et al (2013) The effect of alkaline phosphatase and intrahepatic metastases in large hepatocellular carcinoma. World J Surg Oncol 11:40
Piras-Straub K, Khairzada K, Gerken G et al (2015) Glutamate dehydrogenase and alkaline phosphatase as very early predictors of hepatocellular carcinoma recurrence after liver transplantation. Digestion 91:117–127
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
About this article
Cite this article
Attallah, A.M., Omran, M.M., Attallah, A.A. et al. Simplified HCC-ART score for highly sensitive detection of small-sized and early-stage hepatocellular carcinoma in the widely used Okuda, CLIP, and BCLC staging systems. Int J Clin Oncol 22, 332–339 (2017). https://doi.org/10.1007/s10147-016-1066-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-016-1066-x