Abstract
Background
We evaluated short- and long-term renal function in patients after radical cystectomy with urinary diversion and identified risk factors for the deterioration of renal function.
Methods
This retrospective study comprised 91 patients who underwent radical cystectomy and urinary diversion for bladder cancer and survived ≥3 years after surgery. The estimated glomerular filtration rate (eGFR) was calculated, and longitudinal changes of eGFR were assessed. Deterioration in renal function in early and late postoperative years was defined as a ≥25 % decrease in the eGFR from preoperative to postoperative year one, and a reduction in the eGFR of >1 mL/min/1.73 m2 annually in subsequent years, respectively. Univariate and multivariate logistic regression analyses were used to evaluate its association with clinicopathologic features.
Results
The median follow-up period after surgery was 7 years (range 3–26). The mean eGFR decreased from preoperative 65.1 to 58.9 mL/min/1.73 m2 1 year after the surgery, followed by a continuous decline of ~1.0 mL/min/1.73 m2 per year thereafter. Multivariate analyses identified ureteroenteric stricture as the sole risk factor associated with early renal function deterioration [odds ratio (OR) 4.22, p = 0.037]. Diabetes mellitus (OR 8.24, p = 0.015) and episodes of pyelonephritis (OR 4.89, p = 0.038) were independently associated with the gradual decline in the late postoperative period.
Conclusion
In cystectomy patients with urinary diversion, the rapid deterioration of renal function observed during the first year after surgery and the gradual but continuous decline in function thereafter were found to be associated with different risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical cystectomy (RC) with urinary diversion (UD) is the standard treatment for muscle-invasive and refractory superficial bladder cancer [1]. However, RC with UD is associated with significant risks of perioperative and long-term morbidity and mortality, including renal function deterioration and development of chronic kidney disease (CKD) [2, 3]. CKD is known as an established risk factor of cardiovascular events and death; therefore special attention is needed for the preservation of renal function [4, 5].
The natural history and long-term follow-up of renal function in patients treated by RC with UD have been reported [6, 7]. Several factors have been identified to be associated with the decline in renal function after RC with UD: advanced age, potential nephrotoxic chemotherapy, postoperative urinary tract obstruction, and urinary tract infection [6–10]. The postoperative deterioration of renal function appears to be biphasic: a rapid decline occurred during the first two postoperative years with a slight to moderate decrease in subsequent years [7]. However, these studies did not identify the factors associated with each phase of the decline in renal function.
We postulate that different risk factors are associated with the early and late changes in renal function. In the present study, we evaluated short- and long-term postoperative renal function, as well as investigating the risk factors for each phase of decline in renal function in patients who had undergone RC with UD.
Materials and methods
Patient selection
This study was approved by the institutional review board (#3124). Patients (n = 222) were identified who underwent radical cystectomy and urinary diversion for bladder cancer at the University of Tokyo Hospital between February 1986 and August 2011. Of these, we excluded the patients who underwent nephroureterectomy at the time of cystectomy or developed postoperative disease recurrence within 3 years, and those with insufficient data, leaving 91 patients (41 %) available for analysis.
Four different types of urinary diversion were performed in this cohort of patients: ileal conduit in 56 patients (62 %); orthotopic ileal neobladder substitution in 28 (31 %); cutaneous ureterostomy in 2 (2 %); Mainz pouch in 5 (5 %). All patients underwent RC using standard techniques, and the surgical procedure of UD has been described previously [11–15]. Medical charts were reviewed and various clinical parameters were collected: age, gender, preoperative comorbidities including chronic hypertension and diabetes mellitus, baseline and follow-up estimated glomerular filtration rate (eGFR), and receipt of perioperative chemotherapy. Chronic hypertension was defined as administration of one or more antihypertensive drugs.
Patient follow-up data and data collection
All patients were regularly followed in our department every 3 months for the first 2 years, then every 6 months up to 5 years, and annually thereafter. At each visit, routine blood tests including serum creatinine value were performed. Computed tomography was performed every 3–6 months for the first 2–3 years and annually thereafter. We focused our evaluation on postoperative complications, including mechanical urinary obstruction and pyelonephritis. Pyelonephritis was defined as hospitalization by either a febrile episode or flank pain tenderness with a positive urine culture (>105 colony-forming units) after excluding other indications for fever.
Evaluation of renal function
The eGFR was calculated based on a formula developed by The Japanese Society of Nephrology, as follows: eGFR (mL/min/1.73 m2) = 194 × serum creatinine−1.094 × age−0.287 (×0.739, if female) [16]. We evaluated preoperative and yearly postoperative eGFR. The median serum creatinine value was used for the analyses if multiple values were available for a given time point. Early renal function deterioration was defined as a >25 % decrease in the eGFR from the preoperative to postoperative year one, and late deterioration as a reduction in the eGFR of >1 mL/min/1.73 m2 annually in subsequent years, respectively [6, 8–10, 17]. CKD stages were also used to classify renal function.
Statistical analysis
Univariate and multivariate logistic regression models were used for statistical analysis. The variables with a p value of 0.10 or less in univariate analyses were included in multivariate analyses. Statistical computations were carried out using JMP 11.0.0 (SAS Institute, Cary, NC, USA). Significance was set at P < 0.05.
Results
Patient characteristics
The clinicopathologic features of patients at the time of surgery are summarized in Table 1. The median follow-up period after RC was 7 years (range 3–26 years). The median patient age at the time of surgery was 64 years (range 39–80 years), and the gender ratio was 4:1 (male:female). Of the 91 patients, 37 (41 %) received platinum-based chemotherapy during the perioperative period. Postoperative complications included ureteroenteric stricture (n = 13, 14 %) and pyelonephritis (n = 16, 18 %).
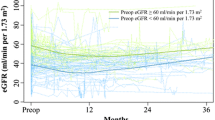
Changes in eGFR
Figure 1 shows yearly serial changes in the mean eGFR. The mean eGFR decreased from 65.1 mL/min/1.73 m2 [interquartile ratio (IQR) 56.0–75.0 mL/min/1.73 m2] preoperatively to 58.9 mL/min/1.73 m2 (IQR 50.8–70.1 mL/min/1.73 m2) 1 year after surgery. The mean eGFR consistently decreased after surgery: a rapid decline of eGFR during the first year after RC with UD (–6 mL/min/1.73 m2) and a slow continuous decrease in the subsequent years (~1 mL/min/1.73 m2 per year). Early renal function deterioration, defined as >25 % decrease of eGFR from preoperative levels to year one after RC with UD, was observed in 18 of the 91 patients (20 %). Late renal function deterioration, defined as a reduction in the eGFR of >1 mL/min/1.73 m2 annually from eGFR at 1 year after surgery, was evaluated in 44 patients, with 47 excluded due to death during the period or transfer to another hospital. Late renal function deterioration was observed in 17 of the 44 patients (39 %).
Risk factors for early renal function deterioration
The associations of clinicopathologic factors with early renal function deterioration are shown in Table 2. Ureteroenteric stricture was identified as a sole significant predictive factor of postoperative early renal impairment. Figure 2a shows the changes in eGFR during the first postoperative year in the patients with and without ureteroenteric stricture.
Changes in renal function, as measured by the estimated glomerular filtration rate, of patients with and without a ureteroenteric stricture, b diabetes mellitus, and c pyelonephritis (mean ± SE). a Ureteroenteric stricture significantly affected the early (solid line) but not the late (dashed line) renal function deterioration. On the other hand, b diabetes mellitus and c pyelonephritis were associated with the late (solid line) but not the early (dashed line) renal function deterioration
Risk factors for late renal function deterioration
The associations of clinicopathologic factors with late renal function deterioration are shown in Table 3. Different from early deterioration, diabetes mellitus and episodes of pyelonephritis were independently associated with late renal function decline. Neither perioperative chemotherapy nor chronic hypertension appeared to significantly affect renal function in this study. The choice of urinary diversion methods was also not associated with the risk of renal function decline. Figure 2b, c shows the changes in eGFR after the first postoperative year in the patients with and without diabetes mellitus and pyelonephritis, respectively.
Discussion
The maintenance of renal function is important. In the first year after RC with UD surgery for bladder cancer, renal function affects whether patients can undergo the standard cisplatin-based chemotherapy when needed. Years after surgery, the development of CKD is a risk factor for cardiovascular disease [4]. In the present study, we confirmed a biphasic deterioration of renal function after RC and UD. We elucidated the predictive factors for early and late renal function deterioration. To our knowledge, this is the first study that evaluated the impact of several parameters on the biphasic impairment of postoperative renal function.
Using univariate and multivariate analyses, we found that mechanical obstruction at ureteroenteric anastomosis was associated with a rapid eGFR decline and was predictive of early impaired renal function, while diabetes mellitus and episodes of pyelonephritis were independently associated with late development of moderate renal function deterioration. Our analyses also demonstrated that the type of urinary diversion was not associated with the postoperative decrease in eGFR. This finding is consistent with those reported in several previous studies [6, 8, 9].
The definition of renal function deterioration is debatable and heterogeneous across studies. Some groups define it as a >25 % decrease in the eGFR from baseline, regardless of the observation period [8, 10]. Others consider a decline in eGFR of >1 mL/min/1.73 m2 annually as significant [7, 9], as previous studies revealed an annual physiologic decrease in GFR of 0.58–1 mL/min/1.73 m2 per year [18–20]. Both definitions of eGFR are influenced by the length of the observation period: longer follow-up periods could result in an increase in the number of the patients with >25 % eGFR decrease, and shorter observation periods would cause inaccurate evaluation of the annual change of eGFR. With these issues in mind for the present study, we defined early renal function deterioration as a >25 % decrease in the eGFR from preoperative levels to the first postoperative year, and late renal function deterioration as a reduction in the eGFR >1 mL/min/1.73 m2 annually in subsequent years.
Our study was limited by its retrospective design and small sample size. Lack of a control cohort that did not undergo RC with UD was also a limiting factor in assessing the risk factors affecting postoperative renal function. Excluding patients lacking long-term renal function data from analysis may have introduced a selection bias. Another concern was the definition of renal function deterioration. Arguably, definitions of renal function deterioration are heterogeneous across studies. The two most widely used definitions in the literature are: annual eGFR decline of >1 mL/min/1.73 m2 and >25 % reduction from the baseline eGFR. Further investigation is needed to refine the definition of renal function deterioration after RC with UD. Currently, it is unclear to what extent creatinine and urea are reabsorbed by the ileal neobladder and ileal conduit. As the contact time of urine is longer and the reabsorbing surface is larger in an ileal neobladder than in an ileal conduit, reabsorption of creatinine may be more pronounced in patients with ileal neobladder [21]. Therefore, their eGFR could be falsely lower. Although estimation based on serum creatinine is easy and inexpensive, development of another GFR estimation would further enhance the evaluation of renal function after RC with UD.
In conclusion, the renal function of the patients with urinary diversion deteriorated rapidly during the first year after RD with UD, and gradually but continuously declined thereafter. Urinary tract obstruction induced by ureteroenteric stricture was the leading cause of rapid renal function decline after surgery, while diabetes mellitus and episodes of pyelonephritis were independently associated with the development of late renal function deterioration.
Abbreviations
- eGFR:
-
Estimated glomerular filtration rate
- RC:
-
Radical cystectomy
- UD:
-
Urinary diversion
- CKD:
-
Chronic kidney disease
References
Stamatakis L, Godoy G, Lerner SP (2012) Innovations in radical cystectomy and pelvic lymph node dissection. Semin Oncol 39:573–582. doi:10.1053/j.seminoncol.2012.08.012
Shabsigh A, Korets R, Vora KC et al (2009) Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol 55:164–174. doi:10.1016/j.eururo.2008.07.031
Shimko MS, Tollefson MK, Umbreit EC et al (2011) Long-term complications of conduit urinary diversion. J Urol 185:562–567. doi:10.1016/j.juro.2010.09.096
Go AS, Chertow GM, Fan D et al (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305. doi:10.1056/NEJMoa041031
Huang WC, Levey AS, Serio AM et al (2006) Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol 7:735–740. doi:10.1016/S1470-2045(06)70803-8
Eisenberg MS, Thompson RH, Frank I et al (2014) Long-term renal function outcomes after radical cystectomy. J Urol 191:619–625. doi:10.1016/j.juro.2013.09.011
Rouanne M, Perreaud A, Letang N et al (2015) Trends in renal function after radical cystectomy and ileal conduit diversion: new insights regarding estimated glomerular filtration rate variations. Clin Genitourin Cancer 13:e139–e144. doi:10.1016/j.clgc.2014.11.003
Nishikawa M, Miyake H, Yamashita M et al (2014) Long-term changes in renal function outcomes following radical cystectomy and urinary diversion. Int J Clin Oncol 19:1105–1111. doi:10.1007/s10147-014-0661-y
Jin X-D, Roethlisberger S, Burkhard FC et al (2012) Long-term renal function after urinary diversion by ileal conduit or orthotopic ileal bladder substitution. Eur Urol 61:491–497. doi:10.1016/j.eururo.2011.09.004
Osawa T, Shinohara N, Maruyama S et al (2013) Long-term renal function outcomes in bladder cancer after radical cystectomy. Urol J 10:784–789
Miyake H, Furukawa J, Sakai I et al (2013) Orthotopic sigmoid vs. ileal neobladders in Japanese patients: a comparative assessment of complications, functional outcomes, and quality of life. Urol Oncol 31:1155–1160. doi:10.1016/j.urolonc.2011.11.015
Kouba E, Sands M, Lentz A et al (2007) A comparison of the Bricker versus Wallace ureteroileal anastomosis in patients undergoing urinary diversion for bladder cancer. J Urol 178:945–949. doi:10.1016/j.juro.2007.05.030
Studer UE, Burkhard FC, Schumacher M et al (2006) Twenty years experience with an ileal orthotopic low pressure bladder substitute—lessons to be learned. J Urol 176:161–166. doi:10.1016/S0022-5347(06)00573-8
Hirokawa M, Iwasaki A, Yamazaki A et al (1989) Improved technique of tubeless cutaneous ureterostomy and results of permanent urinary diversion. Eur Urol 16:125–132
Thüroff JW, Alken P, Riedmiller H et al (1986) The Mainz pouch (mixed augmentation ileum and cecum) for bladder augmentation and continent diversion. J Urol 136:17–26
Matsuo S, Imai E, Horio M et al (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992. doi:10.1053/j.ajkd.2008.12.034
Harraz AM, Mosbah A, El-Assmy A et al (2014) Renal function evaluation in patients undergoing orthotopic bladder substitution: a systematic review of literature. BJU Int 114:484–495. doi:10.1111/bju.12632
Cohen E, Nardi Y, Krause I et al (2014) A longitudinal assessment of the natural rate of decline in renal function with age. J Nephrol 27:635–641. doi:10.1007/s40620-014-0077-9
Granerus G, Aurell M (1981) Reference values for 51Cr-EDTA clearance as a measure of glomerular filtration rate. Scand J Clin Lab Invest 41:611–616. doi:10.3109/00365518109090505
Fesler P, Ribstein J, du Cailar G et al (2005) Determinants of cardiorenal damage progression in normotensive and never-treated hypertensive subjects. Kidney Int 67:1974–1979. doi:10.1111/j.1523-1755.2005.00297.x
Rinnab L, Straub M, Hautmann RE et al (2005) Postoperative resorptive and excretory capacity of the ileal neobladder. BJU Int 95:1289–1292. doi:10.1111/j.1464-410X.2005.05521.x
Acknowledgments
The authors thank Dr. Pauline Lee and Dr. Makoto Suzuki for their assistance in manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Makino, K., Nakagawa, T., Kanatani, A. et al. Biphasic decline in renal function after radical cystectomy with urinary diversion. Int J Clin Oncol 22, 359–365 (2017). https://doi.org/10.1007/s10147-016-1053-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-016-1053-2