Abstract
Purpose
To review data for patients with stage T4 and/or M1 lymph node (lym) esophageal cancer who have been treated with definitive chemoradiotherapy since 2000 at a high-volume center in Japan.
Patients and methods
We retrospectively reviewed all patients with T4 and/or M1 lym esophageal cancer who were treated by definitive chemoradiotherapy between 2000 and 2010. The eligibility criteria included (1) histopathologically proven esophageal cancer, (2) T4 and/or M1 lym (UICC 2002), (3) 20−79 years of age, (4) having undergone at least 1 cycle of concomitant chemotherapy, (5) having been irradiated with ≥50 Gy, and (6) having no other active malignant tumor during treatment. Toxicity was graded according to the Common Terminology Criteria for Adverse Events (CTCAE v3.0).
Results
Data from 128 patients (70 with clinical stage III, 58 with clinical stage IV) were used for analysis in this study. The median observation period for survivors was 46.3 months. The 2- and 4-year overall survival rates were 32.8 and 24.4 %, respectively. The overall survival of patients without M1 lym was significantly better than that of patients with Ml lym (4-year, 32.6 vs 11.7 %, log-rank test; p = 0.04). Overall survival in more recent patients (2006–2010) did not show improvement when compared with past patients (2000–2005). Eight patients had late toxicities of grade ≥3.
Conclusions
T4 patients without M1 lym showed a relatively good 4-year survival rate of approximately 33 %; however, the results did not show significant improvement after 2000.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, esophageal cancer is the fifth most common cause of cancer-related death for men and the eighth most common cause of cancer-related death for women [1]. In Japan, esophageal cancer causes approximately 3–4 % of cancer-related deaths. The histological background in Japan is different from the West, with >90 % of all esophageal malignancy causes being squamous cell carcinoma. Although surgery still remains a standard treatment, some recent studies revealed that results of definitive chemoradiotherapy (CRT) were almost the same as results of surgery in patients with operable esophageal cancer [2, 3], and definitive CRT has become recognized as one of the standard treatments for esophageal cancer. Results of definitive CRT have improved since the 1990s due to the establishment of concurrent chemotherapy and improvements in radiotherapy technology [4, 5]. However, results for inoperable patients with T4 and/or M1 lymph node (lym) (distant lymph node metastasis) esophageal cancer have not improved [5].
Nishimura et al. reported that the results of definitive radiotherapy for esophageal cancer were influenced by the ‘volume effect’, i.e., institutional experience [6, 7]. Our institution is one of the highest volume centers in Japan using definitive CRT for esophageal cancer.
We retrospectively reviewed data for all patients with T4 and/or M1 lym esophageal cancer who had been treated by definitive CRT between 2000 and 2010 at our institution. Our aim was to determine whether results had improved after 2005 because 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) was adopted by the national insurance program for use in esophageal cancer in Japan after 2006 and to reveal the prognostic factors for overall survival.
Materials and methods
We retrospectively reviewed data for 146 patients with T4 and/or M1 lym esophageal cancer who had been treated by definitive CRT between 2000 and 2010 at our institution, and data for 128 patients who met the eligibility criteria described below were used for analysis in this study. All patients had histologically proven squamous cell carcinoma in the esophagus, and staging was evaluated by computed tomography (CT) scans of the chest and abdomen with/without FDG-PET and esophageal ultrasound endoscopy.
Patient eligibility
Eligibility criteria included (1) histopathologically proven esophageal cancer, (2) T4 and/or M1 lym (UICC 2002), (3) 20−79 years of age, (4) having undergone at least 1 cycle of concomitant chemotherapy, (5) having been irradiated with ≥50 Gy, and (6) having no other active malignant tumor during treatment.
Treatment
Radiotherapy
A linear accelerator (4 or 10 MV) was used as the X-ray source. The target volume was localized for radiotherapy in all patients by CT planning. The daily fractional dose of radiotherapy was 1.8–2.0 Gy, administered 5 days a week, and the total dose was 50.0–70.0 Gy. Before 2005, we often used 64–70 Gy as the initial planned total dose; however, after 2005 the initial planned total dose was changed to 60 Gy. The gross tumor volume (GTV) was defined as the primary tumor and any involved nodes on CT (>1 cm on short axis). The clinical target volume for the primary lesion (CTV-p) was defined as a GTV with a 3.0-cm margin in the cranio-caudal direction and with a 0.5-cm margin in the horizontal direction. The CTVs for subclinical regional lymph nodes (CTV-s) included the bilateral supraclavicular, mediastinal and abdominal regions, except for cervical esophageal cancer. For cervical esophageal cancer without a skip lesion, CTV-s included the bilateral supraclavicular and upper mediastinal regions. Planning target volume was defined as CTV with a 0.7–1.5-cm margin.
After 39.6–40 Gy, radiotherapy was performed for only the primary tumor with a 3-cm cranio-caudal margin and for metastatic lymph nodes with a 1-cm circular margin avoiding the spinal cord.
Concurrent chemotherapy
All patients underwent concurrent platinum-based chemotherapy with radiotherapy as described below.
-
1.
Cisplatin (CDDP) + 5-fluorouracil (5-FU) + docetaxel (DOC): intravenous continuous infusion of 5-FU at a dose of 1,000 mg/m2/day on days 1–5 and 29–33, DOC at a dose of 50 mg/m2 on days 2 and 30, and CDDP at a dose of 60 mg/m2 on days 2 and 30.
-
2.
CDDP + 5-FU: intravenous injection of CDDP at a dose of 70 mg/m2 on days 1 and 29 and continuous infusion of 5-FU at a dose of 700 mg/m2/day on days 1–4 and 29–32.
-
3.
Nedaplatin (CDGP) + 5-FU: intravenous injection of CDGP at a dose of 70 mg/m2 on days 1 and 29 and continuous infusion of 5-FU at 500 mg/m2 on days 1–5 and 29–33.
Follow-up
Follow-up evaluations for all patients were performed every 2–3 months for the first 2 years and every 6 months thereafter by endoscopy and/or CT.
Endpoints
Endpoints of the present study were overall survival rate (OS), progression-free survival rate (PFS) and late toxicities.
Toxicity
Toxicity was graded according to the Common Terminology Criteria for Adverse Events (CTCAE v3.0). The grade was scored retrospectively based on the clinical chart. An adverse effect at >90 days after completion of CRT was defined as late toxicity.
Statistics
Statistical analysis for comparing patient characteristics between 2000–2005 and 2006–2010 was performed using the Kruskal–Wallis and Mann–Whitney test.
Survival estimates were calculated from the first day of radiotherapy using the Kaplan–Meier method, and differences were evaluated by the log-rank test. In univariate and multivariate analysis, Cox proportional hazards model was used.
Statistical significance was defined as a value of p < 0.05 in the present study. SPSS software for Windows version 20.0 was used for all calculations.
Ethics
The present study protocol was reviewed and approved by our institutional review board (2014-1-541), and written informed consent for definitive CRT was obtained from each patient before treatment.
Results
The median age of the 128 patients was 67.0 years. The characteristics of the 128 patients recruited for this retrospective study are summarized in Table 1. Primary sites were in the cervical, upper thoracic, middle thoracic, lower thoracic and abdominal esophagus in 13 patients, 31 patients, 69 patients, 14 patients and 1 patient, respectively. Clinical stages were III in 70 patients, IVa in 11 patients and IVb in 47 patients. Median total irradiation dose was 63 Gy (range 50–70 Gy). CDDP + 5-FU and CDGP + 5-FU were performed as concomitant chemotherapy with radiotherapy in 75 and 48 patients, respectively. CDDP + 5-FU + DOC was performed in 5 patients with cervical esophageal cancer. The median observation period for the survivors was 46.3 months (range 5.0–127.0).
Survival and prognostic factors
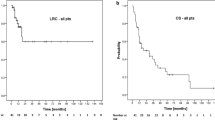
At the last observation date, there were 96 deaths including 8 intercurrent deaths. Of patients without M1 lym, 25 had recurrence or residual tumor in the irradiation field and 15 had distant metastatic recurrence. Nine patients had both locoregional recurrence of residual and distant organ metastases. Of patients with M1 lym, 23 had recurrence or residual tumor in the irradiation field and 12 had distant metastatic recurrence. Fifteen patients had both locoregional recurrence of residual and distant organ metastases. Three patients with perforation of the bronchus and two patients with perforation of the descending thoracic aorta during radiotherapy died soon after the events. These events occurred by rapid depopulation of the tumors invading the risk organs and were not considered as treatment-related toxicities. Another 4 patients had perforation of the bronchus or the mediastinum before or during treatment; however, the perforations in those patients were closed up by restarting definitive CRT after decline of fever with antibiotics and fasting. The 2- and 4-year OS rates were 32.8 % [95 % confidence interval (CI) 24.4–41.2 %] and 24.4 % (95 % CI 16.4–32.4 %), respectively (Fig. 1). The 2- and 4-year PFS rates were 20.0 % (95 % CI 12.9–27.1 %) and 14.6 % (95 % CI 8.3–20.9 %), respectively. The OS of patients without M1 lym was significantly better than that of patients with Ml lym [4-year, 32.6 % (95 % CI 20.8–44.4 %) vs 11.7 % (95 % CI 2.1–21.3 %), log-rank test; p = 0.04] (Fig. 2). The OS in recent patients (2006–2010) did not show improvement when compared with past patients (2000–2005) [4-year, 17.2 % (95 % CI 6.6–27.8 %) vs 30.5 % (95 % CI 18.5–42.5 %), log-rank test; p = 0.84] (Fig. 3). There was no significant difference in survival rate between patients who underwent FDG-PET before treatment (n = 60) and patients who did not undergo FDG-PET (n = 68) [4-year, 25.5 % (95 % CI 13.3–37.7 %) vs 23.0 % (95 % CI 12.2–33.8 %), log-rank; p = 0.35]. There was no significant difference in survival rate between patients treated with ≤60 Gy and patients treated with >60 Gy [4-year, 24.9 % (95 % CI 12.6–37.2 %) vs 23.7 % (95 % CI 17.5–29.9 %), log-rank; p = 0.55]. In multivariate analysis, only stage, which meant with or without M1 lym (hazard ratio [HR] 0.654, 95 % CI 0.433–0.987, p = 0.043) and gender (HR 2.017, 95 % CI 1.013–4.017, p = 0.046) were selected as prognostic factors of OS (Table 2).
Toxicity
The major toxicities in the acute phase are shown in Table 3. As late toxicities, 2 patients had grade 2 hypothyroidism, 1 patient had grade 2 pleural effusion and 1 patient had a thoracic vertebral compressed fracture in the irradiated field. Furthermore, 8 patients had late toxicities of grade ≥3. Four patients had grade 3 radiation pneumonitis and 1 patient died of radiation pneumonitis. One patient showed grade 3 pleural effusion. Heart-related death occurred in 2 patients (cardiac failure and ventricular fibrillation).
Discussion
Some reports on definitive (chemo)radiotherapy, mainly from Japan, have been published. Although Higuchi et al. reported remarkably good results [8], findings from other institutions have remained unchanged [9–13] (Table 4). Our results also suggested that definitive CRT was effective and feasible. Indeed, there were 4 other patients with a perforation to the trachea, lung or mediastinum before or during treatment besides the above-mentioned 5 patients who died early with perforation. These 4 patients continued or restarted CRT after the fever declined with antibiotics and fasting and completed the treatment and the perforations were then closed up.
In Japan, FDG-PET has been used for esophageal cancer since 2005. We expected FDG-PET to improve the results by excluding small distant organ metastasis; however, an improvement in results was not achieved. The best results in previous studies were obtained by using concurrent DCF (docetaxel, cisplatin and 5-FU) with radiotherapy in patients with relatively good performance status [8]. Based on acceptable toxicities in the report [8], maybe more aggressive treatment such as that performed by Higuchi et al. should be considered for improving treatment results in patients with good performance status. Because the DCF regimen in the present study was performed in only 5 patients, the superiority of the DCF regimen over other regimens is unknown; therefore, a randomized study is necessary.
Although performance status (PS) in the recent period of 2006–2010 was significantly better, long-term OS was poorer than in 2000–2005, although the difference was not significant. In patients with stage IV, OS was significantly improved [4-year, 15.2 % (95 % CI 1.1–29.9 %) vs 4.8 % (95 % CI 0–13.8 %), log-rank; p = 0.02]. In patients with stage III, OS was poor but not significant [4-year, 19.6 % (95 % CI 3.5–35.7 %) vs 45.3 % (95 % CI 29.2–61.4 %), log-rank; p = 0.20]. The reason for the difference is unknown. Although there was a significant difference in OS between patients who underwent only the first course of concomitant chemotherapy and patients who underwent the second course of concomitant chemotherapy in stage III (p = 0.028), the rate of completion of concomitant chemotherapy in 2006–2010 was not worse than in 2000–2005 (5/30 vs 7/40).
The standard total irradiation dose worldwide is 50.4 Gy; however, in Japan, ≥60 Gy remains a standard dose except for a few institutions [6, 7, 14]. Before 2005, 64–70 Gy was often used as the initial planned total dose, but there was the impression of prolonged toxicities. However, irradiation with 60 Gy has also recently been used at our institution. Therefore, we compared the results for patients irradiated using >60 Gy with the results for patients irradiated with ≤60 Gy, but found no significant differences in OS or toxicities. One possible reason for the no difference is that some patients for whom second chemotherapy could not be performed due to decreasing PS or protracted myelosuppression were irradiated with >60 Gy despite the fact that irradiation with 60 Gy was initially planned for those patients. The median irradiation dose in patients who could not perform a second course of chemotherapy was 64 Gy, and 60 Gy in patients who could perform a second course chemotherapy, although there was no significant difference (p = 0.179, Mann–Whitney test). Furthermore, in multivariate analysis, irradiation dose was not selected as a prognostic factor of survival. Suh et al. reported that high-dose radiotherapy of ≥60 Gy with concurrent chemotherapy improved locoregional control and PFS in patients with stages II–III esophageal cancer [15]. Further prospective study is needed to determine whether 50.4, 60 Gy or higher is superior for inoperable advanced squamous cell carcinoma in the esophagus.
In multivariate analysis, only stage (III being better) and gender (female being better) were selected as significant prognostic factors of survival. These factors are consistent with previous reports. However, Ohtsu et al. reported that the results for patients with M1 lym were better than those for patients with T4 but without M1 lym [12]. In the present study, approximately 40 % of the patients with T4 but without M1 lym survived for >3 years, although almost all of the patients with M1 lym died within 2 years. The difference between the results of the study by Ohtsu et al. and the present study might be due to overestimation of T stage because of poor image diagnosis as their study was performed between 1992 and 1997.
Conclusions
We showed the results of definitive CRT for T4 and/or M1 lym esophageal cancer at a high-volume center after 2000 in Japan. T4 patients without M1 lym showed a relatively good 4-year survival rate of 32.6 %; however, the results did not show improvement after 2000 and FDG-PET did not improve the results.
References
Jemal A, Bray F, Center MM et al (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Ariga H, Nemoto K, Miyazaki S et al (2009) Prospective comparison of surgery alone and chemoradiotherapy with selective surgery in resectable squamous cell carcinoma of the esophagus. Int J Radiat Oncol Biol Phys 75(2):348–356
Pöttgen C, Stuschke M (2012) Radiotherapy versus surgery within multimodality protocols for esophageal cancer—a meta-analysis of the randomized trials. Cancer Treat Rev 38(6):599–604
Herskovic A, Martz K, al-Sarraf M et al (1992) Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N EngI J Med 326:1593–1598
Yamada S, Nemoto K, Ariga H et al (2012) Radiotherapy for esophageal cancer in Japan. Esophagus 9:66–74
Nishimura Y, Koike R, Ogawa K et al (2012) Clinical practice and outcome of radiotherapy for esophageal cancer between 1999 and 2003: the Japanese Radiation Oncology Study Group (JROSG) Survey. Int J Clin Oncol 17:48–54
Nishimura Y, Jingu K, Itasaka S, et al (2015 ) Clinical outcomes of radiotherapy for esophageal cancer between 2004 and 2008: the second survey of the Japanese Radiation Oncology Study Group (JROSG). Int J Clin Oncol. 2015 Jul 16. (Epub ahead of print)
Higuchi K, Komori S, Tanabe S et al (2014) Initive chemoradiation therapy with docetaxel, cisplatin, and 5-fluorouracil (DCF-R) in advanced esophageal cancer: a phase 2 trial (KDOG 0501-P2). Int J Radiat Oncol Biol Phys 89:872–879
Ishida K, Iizuka T, Ando N et al (1996) Phase II study of chemoradiotherapy for advanced squamous cell carcinoma of the thoracic esophagus: nine Japanese institutions trial. Jpn J Clin Oncol 26:310–315
Sasamoto R, Sakai K, Inakoshi H et al (2007) Long-term results of chemoradiotherapy for locally advanced esophageal cancer, using daily low-dose 5-fluorouracil and cis-diammine-dichloro-platinum (CDDP). Int J Clin Oncol 12:25–30
Kaneko K, Ito H, Konishi K et al (2003) Definitive chemoradiotherapy for patients with malignant stricture due to T3 or T4 squamous cell carcinoma of the oesophagus. Br J Cancer 88:18–24
Ohtsu A, Boku N, Muro K et al (1999) Definitive chemoradiotherapy for T4 and/or M1 lymph node squamous cell carcinoma of the esophagus. J Clin Oncol 17:2915–2921
Ishida K, Ando N, Yamamoto S et al (2004) Phase II study of cisplatin and 5-fluorouracil with concurrent radiotherapy in advanced squamous cell carcinoma of the esophagus: a Japan Esophageal Oncology Group (JEOG)/Japan Clinical Oncology Group trial (JCOG9516). Jpn J Clin Oncol 34:615–619
Kenjo M, Uno T, Murakami Y et al (2009) Radiation therapy for esophageal cancer in Japan: results of the patterns of care study 1999–2001. Int J Radiat Oncol Biol Phys 75:357–363
Suh YG, Lee IJ, Koom WS et al (2014) High-dose versus standard-dose radiotherapy with concurrent chemotherapy in stages II–III esophageal cancer. Jpn J Clin Oncol 44:534–540
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Jingu, K., Umezawa, R., Matsushita, H. et al. Chemoradiotherapy for T4 and/or M1 lymph node esophageal cancer: experience since 2000 at a high-volume center in Japan . Int J Clin Oncol 21, 276–282 (2016). https://doi.org/10.1007/s10147-015-0896-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-015-0896-2