Abstract
Osteoporotic vertebral compression fractures of the thoracolumbar spine can progress to Kümmell’s disease, an avascular vertebral osteonecrosis. Vertebral augmentation (VA)—vertebroplasty and/or kyphoplasty—is the main treatment modality, but additional short-segment fixation (SSF) has been recommended concomitant to VA. The aim is to compare clinical and radiological outcomes of VA + SSF versus VA alone. Systematic review, including comparative articles in Kümmell’s disease, was performed. This study assessed the following outcome measurements: visual analog scale (VAS), Oswestry Disability Index (ODI), anterior vertebral height (AVH), local kyphotic angle (LKA), operative time, blood loss, length of stay, and cement leakage. Six retrospective studies were included, with 126 patients in the VA + SSF group and 152 in VA alone. Pooled analysis showed the following: VAS, non-significant difference favoring VA + SSF: MD –0.61, 95% CI (–1.44, 0.23), I2 91%, p = 0.15; ODI, non-significant difference favoring VA + SSF: MD –9.85, 95% CI (–19.63, –0.07), I2 96%, p = 0.05; AVH, VA + SSF had a non-significant difference over VA alone: MD –3.21 mm, 95% CI (–7.55, 1.14), I2 92%, p = 0.15; LKA, non-significant difference favoring VA + SSF: MD –0.85°, 95% CI (–5.10, 3.40), I2 95%, p = 0.70. There were higher operative time, blood loss, and hospital length of stay for VA + SSF (p < 0.05), but with lower cement leakage (p < 0.05). VA + SFF and VA alone are effective treatment modalities in Kümmell’s disease. VA + SSF may provide superior long-term results in clinical and radiological outcomes but required a longer length of stay.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Kümmell’s disease is defined as the presence of avascular osteonecrosis of the vertebral body, creating a pseudoarthrosis. It is well recognized as a complication of osteoporotic vertebral compression fracture (OVCF) with consequent development of spinal instability, pain, kyphosis, disability, and eventually neurological compromise [14], generally after a minor spinal trauma [12].
Treatment strategies for Kümmell’s disease may be non-operative, with pain medication and bracing [7]. However, it may need to be surgically managed when pain is refractory, there is deformity progress, or neurological deficit appears. Vertebral augmentation (VA), with percutaneous kyphoplasty (PKP) or percutaneous vertebroplasty (PVP), has successfully restored vertebral height and decreased pain in some clinical series [7, 10]. However, despite the low associated morbidity of these procedures, late-onset complications may occur, such as mechanical failure, progressive deformity, and pain [8, 22].
To improve the results of VA, some surgeons proposed adding short-segment fixation (SSF)—one level above and one level below—to improve construction strength [17]. Both surgical treatments have been considered valid options for this disease, without clear superiority of one over the other in literature [23]. Therefore, the aim of this study is to investigate the clinical and radiological outcomes of thoracolumbar Kümmell’s disease treated with VA versus VA + SSF.
Materials and methods
We performed a systematic review of the literature using PubMed, Web of Science, and Scopus databases during September 2020, to identify studies reporting the outcome of thoracolumbar Kümmell’s disease treated with VA + SSF or VA alone. The systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [15].
The following PICO acronym was used:
P (Population): adult patients with thoracolumbar Kümmell’s disease.
I (Intervention): VA + SSF.
C (Comparison): VA alone.
O (Outcome): visual analog scale (VAS), Oswestry Disability Index (ODI), anterior vertebral height (AVH), local kyphotic angle (LKA), length of surgery, blood loss, length of stay, and cement leakage.
Search strategy and inclusion and exclusion criteria
One author (J.P.C.) performed the database search and initially screened articles published from January 2010 to September 2020. The screening process of all articles was performed using titles and abstracts; the selected articles were analyzed for eligibility in full text and assessed by 2 other independent reviewers (A.G. and G.C.W.). A mismatch of one article was resolved by a third reviewer (A.F.J.), and that article was subsequently excluded. None of the authors had any conflict of interests related to this systematic review. Figure 1 shows the flow chart of the search strategy.
The following terms were used in the advanced search of the databases screened: (“Kümmell”[All Fields] OR “Kummell’s”[All Fields] OR “osteonecrosis”[MeSH Terms] OR “osteonecrosis”[All Fields] OR “osteonecrosis”[All Fields] OR “vertebral compression fracture”[All Fields] OR “vacuum cleft”[All Fields]) AND ((fixation OR instrumentation OR “hybrid stabilization” OR “short segment”) [All Fields] AND (augmentation OR vertebroplasty OR Kyphoplasty) [All Fields]). Records were filtered from 2010 to date, only in English literature, excluding studies related to animals and cadavers.
The inclusion criteria used were comparative case series between VA + SSF and VA alone, using pedicle screw instrumentation, either open or percutaneous, with or without inclusion of the fractured vertebra; patients with single-level osteoporotic fracture of the thoracolumbar spine in a non-acute scenario; studies analyzing patients with the diagnosis of Kümmell’s disease or delayed treatment of vertebral compression fractures after failure of medical treatment, pseudoarthrosis/nonunion, or presence of intravertebral vacuum cleft; and studies with a minimum follow-up of 6 months.
The exclusion criteria were the patients with spinal cord compression, those with neurological deficits, and studies not reporting results of both surgical techniques separately.
Evidence quality assessment and risk of bias
The risk of bias of all included studies was performed using the MINORS assessment tool [19] for non-randomized studies evaluated by two independent reviewers. Using this instrument, the quality for comparative studies according to the scores is as follows: 0–6, very low quality; 7–12, low quality; 13–18, moderate quality; and 19–24, high quality [16].
Data synthesis and statistical analysis
Data analysis and synthesis were performed using Review Manager (RevMan) (computer program) version 5.4.1, The Cochrane Collaboration, 2020. For continuous variables, the mean difference with a 95% CI was calculated, and for dichotomous outcomes, the odds ratio with a 95% CI by the Mantel–Haenszel method. For non-randomized studies, the outcomes VAS, ODI, AVH, and LKA were compared between experimental and control groups, using the change-from-baseline method, calculating mean difference change from preoperative to the final follow-up. Statistical heterogeneity among studies was evaluated using I2 test; the fixed-effect model was used if I2 < 50%, while the random-effect model was employed when I2 > 50%. A p value < 0.05 was considered significant.
Results
A total of 235 articles were found in the initial search of all three databases used. After 31 duplicated articles were removed, 204 articles were analyzed and 186 of them were excluded. A total of 18 full-text articles were analyzed by reviewers, with six studies fully included [1, 5, 6, 9, 10, 23]. The search mechanism used in the systematic review is shown in Fig. 1.
The six articles included in this systematic review are summarized in Table 1. All articles included are non-randomized retrospective studies and were consequently assessed for the level of perceived risk of bias using the MINORS assessment tool [19]; the result was five studies [5, 6, 9, 10, 23] with moderate quality and one study [1] with high quality.
Patient demographics
Patient characteristics related to age and gender are provided in all the studies included [1, 5, 6, 9, 10, 23], and bone mineral density (BMD) was analyzed in four of the six studies [1, 6, 9, 23]; all cases have a density range of osteoporosis, without significant differences between both groups. In the Chen et al. [1] study, BMD was − 3.45 in the VA group and − 2.97 in the VA + SSF group (p = NR). Regarding the Kim et al. [9] study, BMD was − 3.61 ± 0.57 in the VA group, while − 3.55 ± 0.59 in the VA + SSF group (p = NR). Huang et al. [6] reported − 3.36 ± 0.4 in the VA group and − 3.42 ± 0.4 in the VA + SSF group (p = 0.627) for BMD. Finally, Wang et al. [23] reported BMD of − 3.4 ± 0.6 in the VA group and − 3.5 ± 0.8 in the VA + SSF group (p = 0.538). Therefore, comparing these reported demographic characteristics regarding BMD, the groups are comparable and it was not a significant factor on the decision-making of type of treatment. Table 2 summarizes the demographic characteristics of patients from both groups, and a summary of the main specific outcomes extracted from the six articles included in this systematic review is shown in Table 3.
Notably, only two studies [1, 23] reported results with a clinical stage classification system of Kümmell’s disease with a similar number of treated patients according to the stages assessed with the Steel and Li classifications [1], while the study of Wang et al. [23] preferably according to the pattern of the intravertebral vacuum cleft rather than the stage of the disease and not affecting the decision on treatment modality between these two comparable groups.
Clinical outcomes
Visual analog scale
VAS was analyzed in all six studies [1, 5, 6, 9, 10, 23] included in this systematic review. Overall, all authors reported significant improvement between preoperative and postoperative VAS at the final follow-up; these results were observed in both treatment modalities without significant differences between them, except in the study of Kim et al. [9], with significant difference favoring VA + SSF (p < 0.05) (Table 4). In the pooled analysis, there was a non-significant difference favoring VA + SSF over VA alone: MD − 0.61, 95% CI (− 1.44, 0.23), I2 91%, p = 0.15 (Fig. 2a).
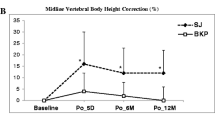
Oswestry Disability Index
ODI was measured in four studies [6, 9, 10, 23]. In general, all authors reported significant improvement between preoperative and postoperative ODI score, without significant differences between VA and VA + SSF, except for Kim et al. [9]; they reported superiority of VA + SSF over VA (p < 0.05) (Table 4). The pooled analysis showed a non-significant difference between both groups, slightly favoring VA + SSF: MD − 9.85, 95% CI (− 19.63, − 0.07), I2 96%, p = 0.05 (Fig. 2b).
Radiological outcomes
Anterior vertebral height
AVH was analyzed in three studies [1, 5, 23]; all of these showed a slightly better restoration of the VA + SSF group, without significant differences (Table 5). In pooled analysis, VA + SSF had a non-significant difference over VA alone: MD − 3.21 mm, 95% CI (− 7.55, 1.14), I2 92%, p = 0.15 (Fig. 3a).
Local kyphotic angle
LKA was measured in all studies [1, 5, 6, 9, 10, 23]. From them, three studies [8, 13, 14] reported better kyphotic angle correction with VA + SSF, two studies [6, 10] reported similar correction between both surgical treatments, and one study [5] showed better LKA restoration with VA (Table 5). There was a non-significant difference between both treatment modalities: MD − 0.85°, 95% CI (− 5.10, 3.40), I2 95%, p = 0.70 (Fig. 3b).
Other outcomes
Operative time, blood loss, and hospital length of stay
Four studies compared blood loss and operative time [1, 6, 9, 10]. Significantly higher blood loss and operative time were reported in all studies for the group VA + SSF. Hospital length of stay was mentioned in two studies [1, 6]; both authors observed significantly higher hospital stay in the VA + SSF group.
Chen et al. [1] reported minimal blood loss, mean operative time of 76 min (60–95), and mean hospital stay of 4.3 days in the VA group, while VA + SSF revealed blood loss of 245 mL, mean operative time of 128 min (95–165), and hospital stay of 7.2 days (p = NR). Kim et al. [9] reported VA + SSF estimated blood loss of 91.1 ± 15.4 mL and operative time 64.7 ± 15.4 min; both these parameters are not mentioned in the VA group. Li et al. [10] reported blood loss of 5.3 ± 3.1 mL and operative time of 43.2 ± 21.8 min in the VA group, compared with 215.0 ± 170.2 mL of blood loss and 230.6 ± 87.1 min of operative time in the VA + SSF group (p = NR). Finally, Huang et al. [6] reported the following outcomes for VA and VA + SSF, respectively: blood loss (9.9 ± 2.7 mL/214.3 ± 17.5 mL) (p < 0.05), operative time (43.1 ± 7.1 min/115.9 ± 10 min) (p < 0.05), and hospital length of stay (3.4 ± 1.2 days/7.6 ± 1.3 days) (p < 0.05). The results demonstrated lower values for the VA group in all three factors. In pooled analysis, the three outcomes—operative time, blood loss, and length of stay—showed a significant difference favoring VA alone over VA + SSF. Operative time: MD 128.46 min, 95% CI (16.20, 240.72), I2 97%, p = 0.02 (Fig. 4a); blood loss: MD 204.44 mL, 95% CI (197.92, 210.97), I2 0%, p < 0.00001 (Fig. 4b); and length of stay: MD 3.56 days, 95% CI (2.28, 4.83), I2 87%, p < 0.00001 (Fig. 4c).
Cement leakage
Cement leakage was analyzed in four studies [1, 6, 10, 23]. Chen et al. [1] reported cement leakage in 11 cases (4 intradiscal, 3 paravertebral, and 4 intracanal), without neurological compromise, in the VA group, whereas in the VA + SSF group, five cases of leakage were observed; one of them underwent prophylactic decompression without neurological compromise. Li et al. [10] observed two cases of cement leakage in the VA group (8%), and one case of cement leakage (4.2%) in the VA + SSF group. Huang et al. [6] showed three asymptomatic cement leakages in the VA group and three asymptomatic cement leakages in the VA + SSF group. Finally, Wang et al. [23] reported four cases of cement leakages in the VA group. The pooled analysis of cement leakage showed a non-significant difference between the groups, slightly favoring VA + SSF over VA alone: OR 0.47, 95% CI (0.20, 1.07), I2 14%, p = 0.07 (Fig. 5).
Any complication in the VA + SSF group occurred in 24 patients (19.0%), while in 23 patients (15.1%) in the VA group. The complications reported other than cement leakage in the six studies included are provided in Table 6.
Discussion
Surgical treatment of Kümmell’s disease is indicated after failure of non-operative management, and the decision-making regarding the best surgical strategy is still under debate. In our systematic review, we found six [1, 5, 6, 9, 10, 23] relevant descriptive articles comparing VA + SSF versus VA alone for the surgical treatment of Kümmell’s disease. Overall, all articles showed significant clinical improvement with both treatment modalities, with potentially better clinical and radiological results in the SSF group at the cost of a major operative time, major blood loss, and longer hospital stay [6, 9, 10, 23].
When considering radiological parameters, VA + SSF has shown better LKA correction and AVH restoration as compared to VA alone [1, 5, 9, 23]. The use of short-segment pedicle screws may allow further correction with rod maneuvers, which may explain the improvement in LKA. The rational to add SSF in VA is to avoid further collapse, delayed cement displacement, and refracture, which has been reported in some studies when patients with Kümmell’s disease were treated with VA alone [11, 20, 25]. The unique pattern of cement filling in an empty space instead of cement diffusion with trabecular bone observed in acute osteoporotic fractures has been mentioned as a possible cause of poor stability in Kümmell’s disease patients [22].
PVP and PKP alone in the surgical treatment of OVCF with intravertebral cleft have been compared, demonstrating similar results in VAS, ODI, LKA, and AVH. However, kyphoplasty was associated with lower complication rates, especially cement leakage—potentially explained by the fact that in kyphoplasty, the cement is injected with lower pression [24]. This is of paramount importance when VA alone has been chosen. Of note, both minimally invasive techniques can be associated with delayed onset cement dislodgement in the context of vacuum cleft, leading to a circumferential instrumentation as a revision surgery [3]. SSF treatment possibly reduces the rate of failure and the occurrence of this undesired complication.
Potential advantages of VA + SSF are that it can effectively shorten the entire construct [18], and biomechanically, it possibly reduces the load of dorsal implants and possibly the risk of implant failure [4]. VA alone, using PKP, can develop a new collapse of the cemented vertebrae during mid-term follow-up, being associated with the presence of an intravertebral cleft, a lack of contact between injected cement and endplates, and increased postoperative vertebral height [21]. However, a recent clinical analysis comparing PKP versus PVP + SSF found that these two surgical methods had a similar effect on improving the studied outcomes (VAS, ODI, LKA), with similar cement leakage [13].
The surgical treatment at the time of diagnosis requires to be more aggressively performed than VA alone, due to the high rate of related complications during follow-up [11, 25]. Comparing the same techniques in an acute scenario of OVCF, PVP alone is significantly associated to more fracture of the treated vertebrae and adjacent vertebras when compared to hybrid stabilization [2]. Even though the VA + SSF group had significant differences in terms of blood loss, operative time, and hospital length of stay, it was not associated with increased rates of cement leakage as was the case with the VA group.
This systematic review has some limitations that need to be addressed; on the one hand, our study included only six observational retrospective articles with a relatively small number of cases, with each of them having moderate quality of evidence. This could affect the strength of our results and, therefore, the quality of the systematic review. On the other hand, Kümmell’s disease is a relatively infrequent pathology, making it difficult to carry out larger prospective studies. Another limitation is that two studies did not report preoperative BMD [5, 6] that could influence the results due to the negative effect of osteoporosis in surgical treatment of spinal conditions, as well as only two studies [1, 23] used a clinical stage classification of the disease probably impacting the choice of treatment modality. Another limitation is related to the short time of follow-up for this pathology, requiring longer time of observation for detecting a wider spectrum of complications, and for assessing more accurately the superiority of one technique over the other. Finally, there are different procedures considered in vertebral augmentation, making the analysis more clinically heterogeneous as well as some outcomes in the pooled analysis with considerable statistical heterogeneity.
Nevertheless, this systematic review has also some strengths: first, the assessment of outcomes in a long follow-up rather than a comparison between preoperative and postoperative outcomes; secondly, subsequent to the study design of the studies included—non-randomized—the different preoperative clinical and radiological outcomes were analyzed by arm, using the change-from-baseline, comparing the amount of improvement between experimental and control groups. Finally, it provides useful insights for a rare pathology that would be advisable when surgeons choose VA + SSF versus VA alone, using the best evidence available.
Conclusions
VA in combination with SSF or alone can effectively treat Kümmell’s disease of the thoracolumbar spine in neurological intact patients, improving outcomes of VAS, ODI, AVH, and LKA significantly. However, VA + SSF is associated with a trend to have better clinical and radiological outcomes as well as lower rates of cement leakage, but with higher operative time, blood loss, and hospital length of stay than VA alone. Further studies are needed to increase the quantity and quality of evidence regarding this controversial topic and validate the best surgical treatment for this challenging disease.
Data availability
Not applicable.
Code availability
Not applicable.
References
Chen L, Dong R, Gu Y, Feng Y (2015) Comparison between balloon Kyphoplasty and short segmental fixation combined with vertebroplasty in the treatment of Kümmell’s disease. Pain Physician 18(4):373–381
Gu YT, Zhu DH, Liu HF, Zhang F, McGuire R (2015) Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty for preventing secondary fracture after vertebroplasty. J Orthop Surg Res 10:31. https://doi.org/10.1186/s13018-015-0172-1
Ha KY, Kim YH, Yoo SR, Molon JN (2015) Bone cement dislodgement: one of complications following bone cement augmentation procedures for osteoporotic spinal fracture. Journal of Korean Neurosurgical Society 57(5):367–370. https://doi.org/10.3340/jkns.2015.57.5.367
Hartensuer R, Gehweiler D, Schulze M, Matuszewski L, Raschke MJ, Vordemvenne T (2013) Biomechanical evaluation of combined short segment fixation and augmentation of incomplete osteoporotic burst fractures. BMC Musculoskelet Disord 14:360. https://doi.org/10.1186/1471-2474-14-360
Hsieh JY, Wu CD, Wang TM, Chen HY, Farn CJ, Chen PQ (2013) Reduction of the domino effect in osteoporotic vertebral compression fractures through short-segment fixation with intravertebral expandable pillars compared to percutaneous kyphoplasty: a case control study. BMC Musculoskelet Disord 14:75. https://doi.org/10.1186/1471-2474-14-75
Huang,YS, Hao DJ, Feng H, Zhang HP, He SM, Ge CY, Niu XB (2018). Comparison of percutaneous kyphoplasty and bone cement-augmented short-segment pedicle screw fixation for management of Kümmell disease. Medical science monitor: international medical journal of experimental and clinical research, 24, 1072–1079. https://doi.org/10.12659/msm.905875
Huang Y, Peng M, He S, Tang X, Dai M, Tang C (2016) Clinical efficacy of percutaneous kyphoplasty at the hyperextension position for the treatment of osteoporotic Kümmell disease. Clinical spine surgery 29(4):161–166. https://doi.org/10.1097/BSD.0000000000000259
Jacobson RE, Palea O, Granville M (2017) Progression of vertebral compression fractures after previous vertebral augmentation: technical reasons for recurrent fractures in a previously treated vertebra. Cureus 9(10):e1776. https://doi.org/10.7759/cureus.1776
Kim HS, Heo DH (2016) Percutaneous pedicle screw fixation with polymethylmethacrylate augmentation for the treatment of thoracolumbar intravertebral pseudoarthrosis associated with Kummell’s osteonecrosis. Biomed Res Int 2016:3878063. https://doi.org/10.1155/2016/3878063
Li HK, Hao DJ, Yang JS, Huang DG, Yu CC, Zhang JN, Gao L, Li H, Qian B (2017) Percutaneous kyphoplasty versus posterior spinal fixation with vertebroplasty for treatment of Kümmell disease: a case-control study with minimal 2-year follow-up. Medicine 96(51):e9287. https://doi.org/10.1097/MD.0000000000009287
Li X, Lu Y, Lin X (2017) Refracture of osteoporotic vertebral body after treatment by balloon kyphoplasty: three cases report. Medicine 96(49):e8961. https://doi.org/10.1097/MD.0000000000008961
Lim J, Choi SW, Youm JY, Kwon HJ, Kim SH, Koh HS (2018) Posttraumatic delayed vertebral collapse: Kummell’s disease. Journal of Korean Neurosurgical Society 61(1):1–9. https://doi.org/10.3340/jkns.2017.0505.010
Lu W, Wang L, Xie C, Teng Z, Han G, Shi R, Liang J, Lu S (2019) Analysis of percutaneous kyphoplasty or short-segmental fixation combined with vertebroplasty in the treatment of Kummell disease. J Orthop Surg Res 14(1):311. https://doi.org/10.1186/s13018-019-1358-8
Matzaroglou C, Georgiou CS, Panagopoulos A, Assimakopoulos K, Wilke HJ, Habermann B, Panos G, Kafchitsas K (2014) Kümmell’s disease: clarifying the mechanisms and patients’ inclusion criteria. The open orthopaedics journal 8:288–297. https://doi.org/10.2174/1874325001408010288
Moher D, Liberati A, Tetzlaff J, Altman DG, & PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Öhlin A, Karlsson L, Senorski EH, Jónasson P, Ahldén M, Baranto A, Ayeni OR, Sansone M (2019) Quality assessment of prospective cohort studies evaluating arthroscopic treatment for femoroacetabular impingement syndrome: a systematic review. Orthop J Sports Med 7(5):2325967119838533. https://doi.org/10.1177/2325967119838533
Park SJ, Kim HS, Lee SK, Kim SW (2015) Bone cement-augmented percutaneous short segment fixation: an effective treatment for Kummell’s disease? Journal of Korean Neurosurgical Society 58(1):54–59. https://doi.org/10.3340/jkns.2015.58.1.54
Rajasekaran S, Kanna RM, Schnake KJ, Vaccaro AR, Schroeder GD, Sadiqi S, Oner C (2017) Osteoporotic thoracolumbar fractures-how are they different? Classification and treatment algorithm. J Orthop Trauma 31(Suppl 4):S49–S56. https://doi.org/10.1097/BOT.0000000000000949
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Wagner AL, Baskurt E (2006) Refracture with cement extrusion following percutaneous vertebroplasty of a large interbody cleft. AJNR Am J Neuroradiol 27(1):230–231
Wang C, Zhang X, Liu J, Shan Z, Li S, Zhao F (2019) Percutaneous kyphoplasty: risk factors for recollapse of cemented vertebrae. World neurosurgery 130:e307–e315. https://doi.org/10.1016/j.wneu.2019.06.071
Wang HS, Kim HS, Ju CI, Kim SW (2008) Delayed bone cement displacement following balloon kyphoplasty. Journal of Korean Neurosurgical Society 43(4):212–214. https://doi.org/10.3340/jkns.2008.43.4.212
Wang W, Liu Q, Liu WJ, Li QB, Cai L, Wang ZK (2020) Different performance of intravertebral vacuum clefts in Kümmell’s disease and relevant treatment strategies. Orthop Surg 12(1):199–209. https://doi.org/10.1111/os.12609
Wei H, Dong C, Zhu Y, Ma H (2020) Analysis of two minimally invasive procedures for osteoporotic vertebral compression fractures with intravertebral cleft: a systematic review and meta-analysis. J Orthop Surg Res 15(1):401. https://doi.org/10.1186/s13018-020-01938-6
Zhang C, Wang G, Liu X, Li Y, Sun J (2017) Failed percutaneous kyphoplasty in treatment of stage 3 Kummell disease: a case report and literature review. Medicine 96(47):e8895. https://doi.org/10.1097/MD.0000000000008895
Acknowledgements
This study was organized by the AO Spine Latin America. AO Spine is a clinical division of the AO Foundation, which is an independent medically guided not-for-profit organization. Study support was provided directly through AO Spine Latin America regarding data collection, data analysis, and proofreading.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by JPC, GCW, and AG. The first draft of the manuscript was written by JPC, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cabrera, J.P., Camino-Willhuber, G., Guiroy, A. et al. Vertebral augmentation plus short-segment fixation versus vertebral augmentation alone in Kümmell’s disease: a systematic review and meta-analysis. Neurosurg Rev 45, 1009–1018 (2022). https://doi.org/10.1007/s10143-021-01661-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01661-8